To report the result of a severe articular defect secondary to a complex open fracture of the distal humerus, using the ipsilateral radial head as a bone autograft for the trochlear region as an alternative to total arthroplasty.
Case reportWe describe a patient who suffered an open fracture of the elbow with bone loss in the distal humeral region and, after the initial stabilisation surgery, needed a reconstruction with an ipsilateral radial head autograft.
DiscussionOpen fractures of elbow are rare. When there is a severe trochlear defect, surgical options are total elbow arthroplasty, where the short and medium term results appear to be insufficient, or elbow arthrodesis. We believe that reconstruction of the defect using an ipsilateral radial head autograft is a more functional alternative than the other procedures described.
ConclusionRadial head reconstruction with ipsilateral lateral trochlear defects is a technique that, unlike fusion, preserves functionality without the problems of total elbow arthroplasty.
Presentar el resultado de la reparación de un defecto troclear severo en el codo mediante un autoinjerto óseo con la cabeza radial ipsilateral, como una alternativa a la artroplastia total.
Caso clínicoPresentamos el caso de un paciente, que sufrió una fractura abierta de codo con pérdida ósea importante en la región humeral distal, y que precisó tras la estabilización inicial una cirugía de reconstrucción mediante autoinjerto ipsilateral de cabeza radial.
DiscusiónLas fracturas abiertas de codo son infrecuentes. Cuando existe un defecto troclear severo, las alternativas quirúrgicas son la artroplastia total de codo, con unos resultados a corto y medio plazo que parecen ser insuficientes, o la artrodesis. Creemos que la reconstrucción del defecto empleando un autoinjerto de cabeza radial homolateral es una alternativa más funcional que los otros procedimientos descritos.
ConclusiónLa reconstrucción con cabeza radial ipsilateral de los defectos trocleares laterales es una técnica, que al contrario que la artrodesis, conserva la funcionalidad sin los inconvenientes de la artroplastia total de codo.
Fractures of the distal humerus in adults have an estimated incidence of 5.7 per 100,000 population per year.1 These lesions follow a bimodal age distribution, with one peak being found among men aged 12–19 years as a result of high energy trauma and another among women of advanced age with osteoporotic bones as a result of falls.2 Open fractures of the distal humerus are often a result of high energy trauma, so they generally present great comminution, severe chondral lesion and extensive soft tissue involvement, as well as concomitant injuries in the context of multiple trauma.3
A dilemma arises when young or active patients suffer a fracture in the distal humerus with severe comminution and loss of bone or skin coverage, since internal fixation becomes an almost impracticable procedure. The functional requirements and associated soft tissue injury in these patients often prevent the use of total elbow arthroplasty.4,5 The use of an ipsilateral radial head autograft to reconstruct defects of the joint portion can be an alternative to other procedures described,6 in the same way as iliac crest autografts or vascularised fibular grafts are used to reconstruct column defects.7
The aim of this work is to present the case of a multiple trauma patient with a fractured femur and compound fracture of the distal humerus, who presented a lateral trochlear defect, as well as discuss treatment options of the second lesion and propose the reconstruction of the defect with an ipsilateral radial head autograft.
Clinical caseThe Emergency Department received a 26-year-old male patient with no history of interest who, after suffering an accident whilst driving a car with his arm resting on the window, reported pain, functional disability and deformity in the left leg and elbow.
The patient was conscious and haemodynamically stable. A preoperative study was conducted, as well as a simple radiographic study of the left femur and elbow, reporting a final diagnosis of 32-B2 diaphyseal fracture of the AO classification and grade IIIB open fracture of the left humeral palette (13-C3 of AO) (Fig. 1).
Intravenous antibiotic treatment with 240mg gentamicin and 2g cefazolin was started. We then proceeded to clean and debride the elbow wound and temporarily stabilise the fractures through external fixation and transkeletal femoral traction. The patient was subsequently transferred to the intensive care unit for damage control (Fig. 1).
After 48h admission, we performed intramedullary nailing of the left femur with static locking and deferred elbow surgery until the availability of bones from the bank was confirmed, in case the use of a complete humeral palette became necessary.
The surgical intervention was scheduled at 2 weeks of the accident and was performed under general anaesthesia and preventive ischaemia in the left upper limb. The patient was placed in the prone position and administered grams of prophylactic cefazolin. After verifying the integrity of the medial collateral ligament, we resected the radial head and used it to rebuild the lateral trochlea (Fig. 2), inserting it between the humeral condyle and the medial hemitrochlea, with the wider area in contact with the condyle and the smaller area in contact with the hemitrochlea. Osteosynthesis was performed with 3.5mm cancellous screws, reconstructing the articular surface. Subsequently, we synthesised the fragments to the diaphysis with preformed block plates from distal humerus (DHP, Synthes®) and added an iliac crest autograft and demineralised bone matrix (DBX®) to supplement the metaphyseal defect. We anchored the radial collateral ligament to the plate using a nonabsorbable suture and, finally, closed the olecranon osteotomy with a short-loop, 7mm cancellous screw. We left an aspirative drain and immobilised the limb with a posterior splint (Fig. 2).
Top: intraoperative image of the trochlear defect with the radial head interposed between the primitive medial hemitrochlea and humeral condyle. Bottom: image of the double plate osteosynthesis. Right: image of the iliac crest autograft and demineralised bone matrix, as well as the attachment of the collateral ligament lateral to the epicondyle and plate through nonabsorbable suture.
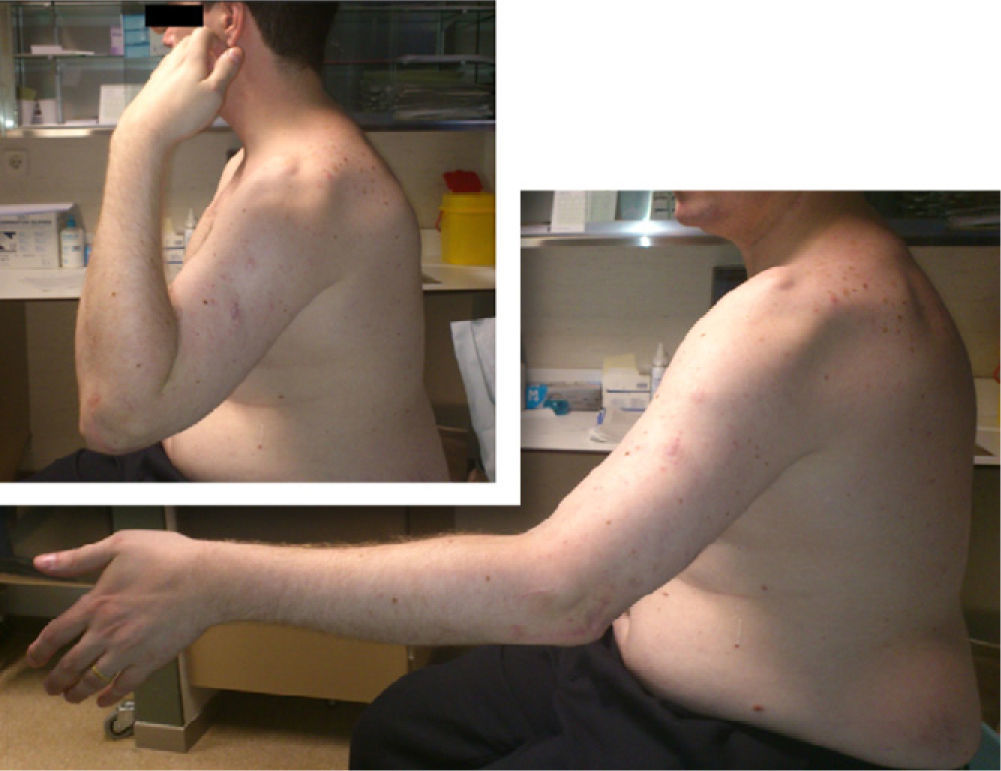
The immediate postoperative evolution was good and the patient was discharged from hospital after 20 days admission. At 3 weeks after surgery, the posterior splint was removed and the patient began passive elbow supination and flexion-extension movements. At 2 months, he was referred to the Rehabilitation Service to improve elbow joint balance, which at that time was from 20° to 60° in flexion-extension and 90° in supination (Figs. 3 and 4).
At present, 2 years after injury, the patient is asymptomatic, without pain (0 in VAS), with an elbow flexion-extension from 25° to 140° and an almost complete pronation and supination. Radiographic evolution of the fracture was optimal, without signs of material mobilisation or resorption of the crest or radial grafts (Fig. 5). The joint is stable and the patient has returned to normal working activity.
DiscussionThe management of bone defects after severe open fractures of the distal humerus involves several technical difficulties. It may not be possible to obtain a proper fixation in these cases, so bone grafting should be considered as an alternative for the restoration of normal elbow anatomy.8
Various surgical approaches for the treatment of fractures in this anatomical region have been described. With the exception of those developed for the treatment of fractures of the coronoid hypophysis, all employ a posterior approach with various options through or around the triceps.
In our case we opted for olecranon osteotomy, as there are anatomical studies which demonstrate that this surgical approach provides better visualisation of the joint surface.9 We followed the basic principles of seeking anatomical joint reduction and rigid fixation with 2 plates, to obtain absolute stability. If a severe metaphyseal comminution was found, then a certain degree of shortening in the centre of the fracture was tolerable, while a proper alignment of the joint shafts and surface was maintained.10
The use of ipsilateral radial head autografts has been described, but without preservation of the humeral condyle.6 The process we employed involved reconstruction of the humeral condyle. Although this reconstruction seems to provide little benefit in the absence of the radial head, it allows the placement of a radial head implant in the event of a proximal migration of the radius or residual lateral instability of the elbow.11
The advantage of the presence of articular cartilage along the side of the radial head made it possible to restore joint congruity in the humeroulnar joint. Although the chondrocyte transplantation technique is still feasible with chondral defects smaller than that presented as long as there is adequate bone support for its implantation, the transfer of autologous osteochondral grafts has been described in the knee, ankle, shoulder and elbow joints with good results.12 We believe that chondrocytes of the radial head can remain viable if the autograft becomes consolidated with the medial trochlea and if the graft is managed with care to minimise iatrogenic cartilage lesions.13
Vascularised bone transfers are more effective than the interposition of conventional corticocancellous grafts in the management of massive bone loss (>6cm).14 They retain their blood supply and intrinsic viability, and the healing process occurs by the union of the fracture rather than its “gradual replacement”.15 As a result, graft incorporation takes place more rapidly and higher consolidation rates are anticipated.
Avascular grafts are more susceptible to infection and resorption and will probably never be replaced by histologically normal bone tissue. Acellular areas coexist with fibrous tissue, decreasing resistance.16 However, their use is simple, does not require excessive time or a complex surgical technique and they may be useful in metaphyseal defects which do not require articular cartilage. In our case we used a graft from the iliac crest in the metaphyseal area in order to encourage consolidation between the joint region and the diaphyseal region.
In our case, a vascularised bone graft would require the incorporation of cartilage and morphology similar to that of the trochlea, in order to restore joint congruity, which has not been described to date.
The option of implementing a primary total elbow arthroplasty was considered in an attempt to obtain sufficient and painless stability and function. The trochlear defect was a good reason for this indication, but the case presented several contraindications, such as a type III open fracture and being a young patient with significant functional demands.5
Elbow arthrodesis achieves a stable and painless elbow, but the resulting functional limitation is rarely accepted by patients. Interposition arthroplasty is a useful technique in young patients, especially those in whom the main complaint is stiffness after an arthropathy secondary to an inflammatory disease. However, this is a technically difficult procedure with scarcely predictable results and with a relatively high complication rate. In addition, it is not indicated in cases where there is considerable bone loss.17
We can conclude that the management of these lesions, which are fortunately rare, must be meticulous and should be performed by a specialised team. The objective of treatment must be the reconstruction of the articular surface, which will restore elbow function. The use of a radial head autograft to reconstruct the humeral trochlea followed by a stable osteosynthesis is an effective option which avoids the complications of arthrodesis and total elbow arthroplasty in young patients.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Please cite this article as: de Prado-López A, et al. Reconstrucción de defecto troclear lateral traumático con autoinjerto de cabeza radial. Rev Esp Cir Ortop Traumatol. 2012;56:323–7.