The goal of the study was to compare functional results in different treatment options in cutting-out, and analyze factors associated to failure.
Materials and methodsRetrospective cohort study in 56 patients diagnosed with cutting-out between 2000 and 2010. Groups were based on rescue treatment: arthroplasty versus alternative treatment. Demographics, fracture characteristics, osteosynthesis, tip to apex distance (TAD), follow-up, complications, and final functional capacity were analyzed.
ResultsRescue treatment: 36 (64.28%) hip replacement (arthroplasty group) and 20 (35.72%) alternative treatment preserving femoral head (alternative group). Groups were comparable on demographic parameters, fracture pattern and osteosynthesis characteristics. Radiography analysis: low inter-observer variability (k=0.83, 95% CI 0.78–0.88), mean TAD 28.66mm (arthroplasty group 32.9mm, 21.5mm control group; p=0.01), and insufficient fracture reduction 39.3% (p=0.001). Cutting-out diagnosis median was 60 days (arthroplasty group 90 days, 18 days alternative group; p=0.001). Follow-up was at least 12 months from rescue treatment. Similar complications rate was observed in both groups (p=0.16). Re-operation rate was 3.57% (11.7% arthroplasty group, alternative group 0%; p=0.01). Better final functional capacity was observed in arthroplasty group (p=0.004).
DiscussionHip arthroplasty offers better results, being considered the gold standard in geriatric patients, although re-operation rate is higher. We recommend new nailing before arthroplasty in early failure (4 weeks) in patients with femoral head integrity. An insufficient fracture reduction is the main short-term factor predicting failure; and TAD higher than 20mm is a middlelong-term one.
Comparar los resultados funcionales de las distintas opciones terapéuticas, y analizar los factores técnicos asociados al cut-out.
Material y métodoEstudio de cohortes retrospectivo de 56 pacientes diagnosticados de cut-out entre 2000-2010, divididos en dos grupos en función del tratamiento de rescate: artroplastia frente a conservar la cabeza femoral (alternativo). Se analizaron datos demográficos, características de la fractura y osteosíntesis, tip to apex distance (TAD), seguimiento, complicaciones y capacidad funcional final.
ResultadosGrupo artroplastia 36 pacientes (64,28%) y 20 (35,72%) grupo alternativo. Comparables en parámetros demográficos, comorbilidades, patrón de fractura y características de la osteosíntesis. Se observó poca variabilidad interobservador (k=0,83; IC 95%: 0,78-0,88) en el análisis radiográfico; con un TAD medio de 28,66mm (p=0,01) y un déficit de reducción en el 39,3% (p=0,001). La mediana de cut-out fue de 60 días (artroplastia 90, alternativo 18; p=0,001). Seguimiento mínimo 12 meses, con tasa de complicaciones similar en ambos grupos (p=0,16) y de reintervención del 3,57% (p=0,01). La capacidad funcional final fue mayor en el grupo de artroplastia (p=0,004).
ConclusiónEl tratamiento de rescate con artroplastia ofrece mejores resultados funcionales, considerándolo el tratamiento de elección en pacientes ancianos, aunque la tasa de reintervención es mayor. Recomendamos nuevo enclavado antes que artroplastia en los casos de cut-out temprano (<4 semanas) en aquellos casos que se mantenga la integridad de la cabeza femoral. Un déficit de reducción de la fractura es el principal factor predictor de fallo a corto plazo; un TAD por encima de 20mm lo es a medio-largo plazo.
Fractures of the proximal end of the femur are frequent pathologies which mainly affect the elderly. Due to the progressive aging of the population, this is considered as an epidemic disease which entails high morbidity, mortality and economic costs.1,2 At present, the treatment of choice is reduction and osteosynthesis, either through intramedullary nailing or a screw-sliding plate system.3–6 Disassembly of the trochanteric nailing due to cut-out effect is the most frequent complication of this treatment, with an incidence close to 4%.1,7,8
Several studies have reported that a distance between the tip of the screw and the apex of the femoral head (tip to apex distance, TAD) over 25mm is the main predictive factor of failure of the osteosynthesis,7,9,10 although most orthopedic surgeons advocate a distance under 20mm.11 There are several therapeutic options for cut-out rescue treatment,12 with some authors reporting hip arthroplasty as the treatment offering the best results in elderly patients.13
The general objective of this study was to analyze our experience with rescue surgery in patients suffering disassembly due to cut-out. The main objective was to compare the functional results obtained with hip arthroplasty compared to other alternative treatments which maintained the integrity of the femoral head. The secondary objective was to analyze technical factors associated to failure of the osteosynthesis.
Materials and methodsDesign of the studyThis was a retrospective, analytical, observational and single-center, cohort study.
Population analyzedWe included all consecutive patients with a diagnosis of cut-out who were treated at our center between January 1st 2000 and December 31st 2010. In the registry of surgical interventions of our service we identified 3105 consecutive patients intervened for pertrochanteric fracture of the femur during the studied period, of which 76 (2.45%) presented cut-out.
These patients were divided into two groups according to the treatment received: (1) the arthroplasty group included those who underwent hip arthroplasty, when the femoral head and/or the cup were significantly affected after the cut-out; (2) the alternative group included those who received a treatment which maintained the integrity of the femoral head, including extraction of the osteosynthesis material and new nailing, closed reduction and distal block or conservative treatment. A total of 48 out of the 76 patients underwent hip arthroplasty, whilst the remaining 28 underwent an alternative treatment.
We excluded from the analysis those without a full registry of clinical data (demographic data, preoperative and postoperative radiographic tests, intervention sheet) and who were not followed for a minimum period of 1 year. In total, 20 (26.3%) of the 76 patients were excluded from the analysis (12 from the arthroplasty group and eight from the alternative group). The remaining 56 patients made up the studied population, comprising of 12 males and 44 females with a mean age of 79 years (±8; range: 64–100 years).
Demographic and general parametersWe reviewed the clinical histories of patients and analyzed the following parameters: age, gender, classification of the fracture (according to the Müller AO/OTA scale),14 and comorbidities (according to the Self-Administered Comorbidity Questionnaire or SCQ).15 A total of 29 patients had fractures of the left femur, whilst the remaining 27 had fractures of the right femur. A total of nine patients (16.07%) had suffered previous fractures (vertebral, distal humeral or femoral), and 32 patients (57.14%) presented concomitant diseases (osteoporosis, renal failure, heart failure or chronic alcoholism), with no differences in the index of comorbidities according to the SCQ.
Surgical, radiographic and functional parametersWe analyzed the time until the intervention, the characteristics of the osteosynthesis (distal block, interfragmentary compression, and type of assembly), TAD,7 the existence of complications, the time until disassembly, the type of rescue treatment, the time until load and the duration of hospital stay, the follow-up period and the functional capacity at the end of the follow-up period.
All 56 patients had been initially treated by trochanteric nailing with a Gamma® (Stryker) nail: trochanteric Gamma® in 47 patients and Gamma 3® in the nine remaining patients, due to a change in the model by the purchasing department at our center. The mean time from the fracture until the intervention was 3 days (±3; range: 0–22 days).
The TAD was calculated by radiographic measurements using the following formula7: TAD=Xap*(Dreal/Dap)+Xlat*(Dreal/Dlat); where X is the distance in millimeters from the tip of the screw to the apex of the femoral head in the AP radiograph (Xap) or the lateral radiograph (Xlat), D is the diameter of the screw measured in the AP radiograph (Dap) or in the lateral radiograph (Dlat), and Dreal is the real size of the implant.
The postoperative control radiographs were examined independently by two separate researchers (FM and JLF) who assessed different aspects:
- (a)
Whether the fracture reduction was satisfactory or unsatisfactory, according to a modification of the reduction criteria described by Baumgaertner et al.7 based on the alignment and displacement of the fracture in the postoperative radiograph. It was considered satisfactory if there was neutral or slightly valgus alignment in the anteroposterior radiograph, less than 20° angulation in the axial radiograph, and a displacement of the fragments by less than 4mm. It was considered unsatisfactory if it did not fulfill all these criteria.
- (b)
Whether the entry point of the nail was correct or excentric.
- (c)
Whether there was a lesion of the calcar femorale or not.
- (d)
Whether the cephalic nail was supported by the lateral cortical or not. In cases on which there was a lack of agreement, we obtained a consensus between both examiners.
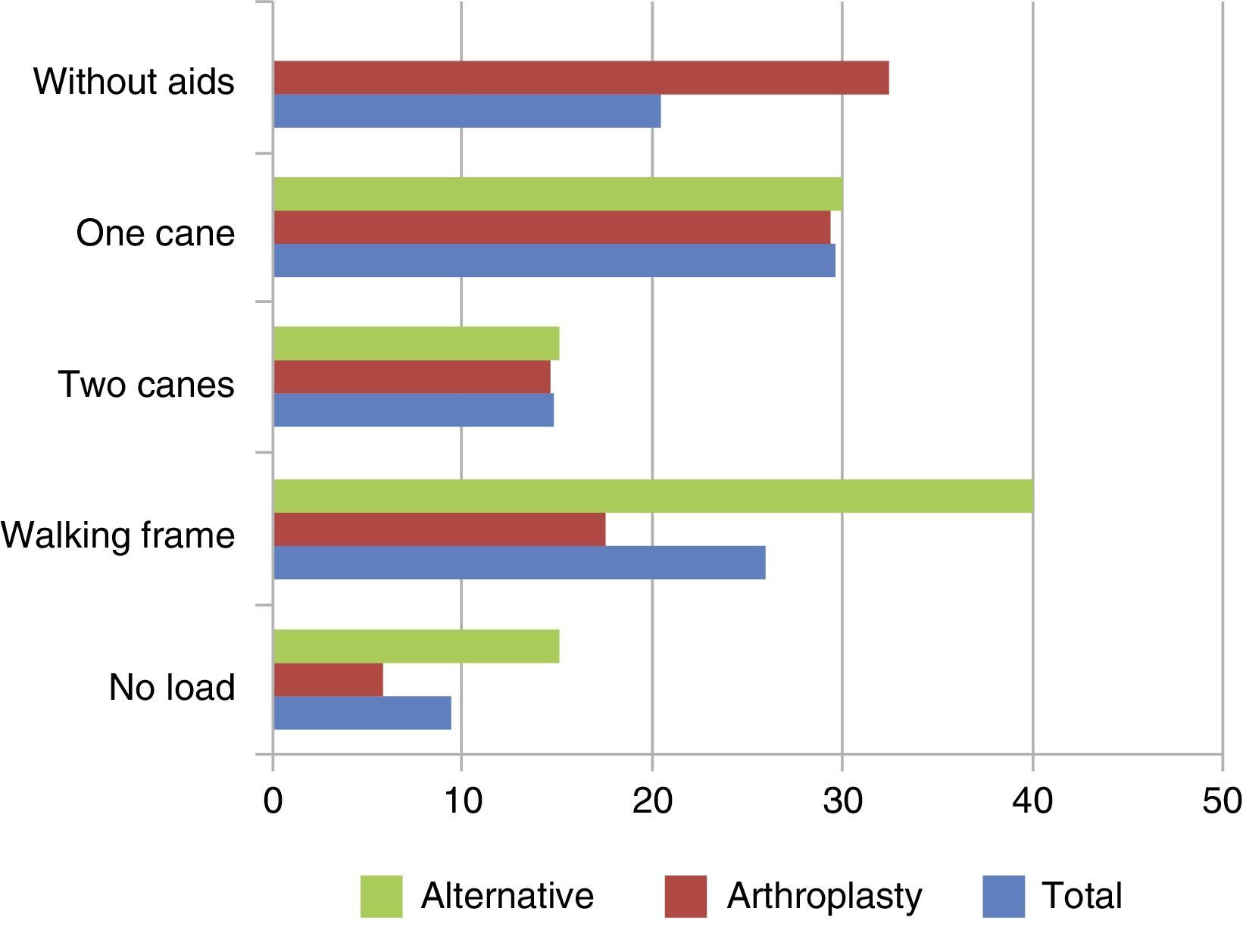
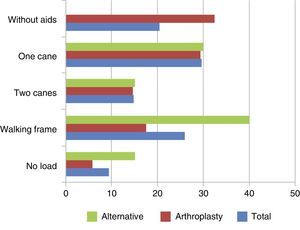
Functional capacity was assessed according to the following ordinal scale: 0 patient without load, 1 walking frame, 2 two canes, 3 one cane, 4 walking without aid.
Statistical analysisWe conducted a statistical analysis using the software package SPSS 18.0, expressing the data as: arithmetic mean (±standard deviation; range). The hypothesis contrast was carried out through the Chi-squared test, Fisher's exact test and the non-parametric Mann–Whitney U test. As multiple comparisons were carried out, we considered as statistically significant a value of P≤.01.
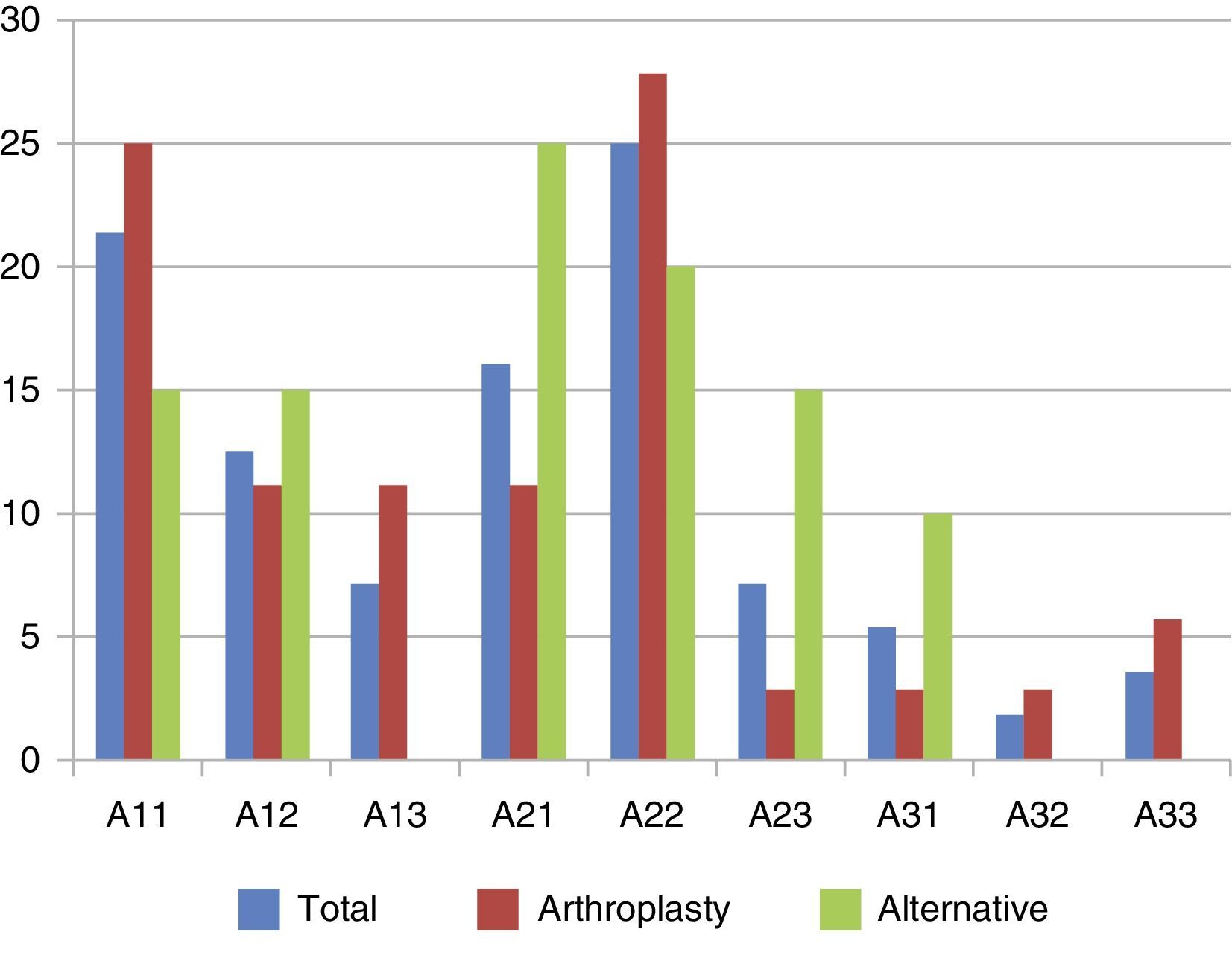
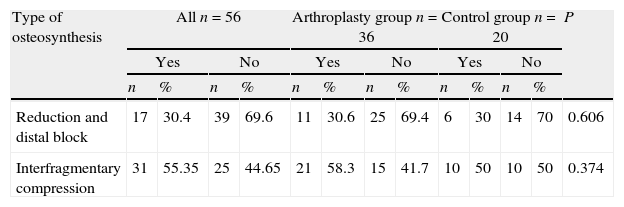
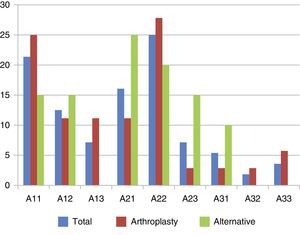
ResultsInitial treatmentBoth groups were comparable as regards their demographic and general parameters (data not shown), distribution of the fracture pattern according to the AO classification (P=0.13) (Fig. 1), characteristics of the osteosynthesis (Table 1), hospital stay and time until load.
Characteristics of the previous osteosynthesis in the groups undergoing rescue with arthroplasty and alternative options.
| Type of osteosynthesis | All n=56 | Arthroplasty group n=36 | Control group n=20 | P | |||||||||
| Yes | No | Yes | No | Yes | No | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Reduction and distal block | 17 | 30.4 | 39 | 69.6 | 11 | 30.6 | 25 | 69.4 | 6 | 30 | 14 | 70 | 0.606 |
| Interfragmentary compression | 31 | 55.35 | 25 | 44.65 | 21 | 58.3 | 15 | 41.7 | 10 | 50 | 10 | 50 | 0.374 |
| Dynamic | Static | Dynamic | Static | Dynamic | Static | P | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Cephalic screw block | 33 | 58.92 | 23 | 41.18 | 18 | 50 | 18 | 50 | 15 | 75 | 5 | 25 | .61 |
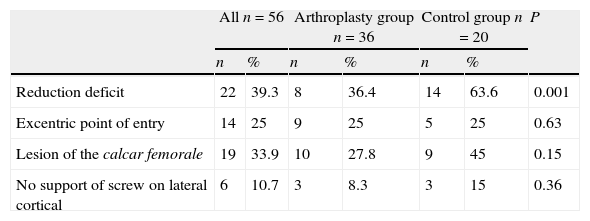
The rate of interobserver agreement in the assessment of the control radiographs by the two surgeons was good (k=0.83; 95% CI: 0.78–0.88). The percentage of fractures with a reduction deficit was significantly lower in the arthroplasty group (P=0.001). The remaining data from the control radiographs were very similar between both groups (Table 2).
Findings identified in the postoperative radiographs in the arthroplasty and alternative groups.
| All n=56 | Arthroplasty group n=36 | Control group n=20 | P | ||||
| n | % | n | % | n | % | ||
| Reduction deficit | 22 | 39.3 | 8 | 36.4 | 14 | 63.6 | 0.001 |
| Excentric point of entry | 14 | 25 | 9 | 25 | 5 | 25 | 0.63 |
| Lesion of the calcar femorale | 19 | 33.9 | 10 | 27.8 | 9 | 45 | 0.15 |
| No support of screw on lateral cortical | 6 | 10.7 | 3 | 8.3 | 3 | 15 | 0.36 |
The mean TAD in the 56 patients was 28.66mm (range: 3.9–70mm): 42 (75%) of the 56 had a TAD over 20mm and in the remaining 14 (25%) it was under 20mm. In the arthroplasty group, the mean TAD (32.9mm) was significantly higher than in the alternative group (21.5mm; P=.01).
During the hospital admission, partial load with the help of two canes was authorized in 43 patients (76.78%): 32 patients (88.9%) in the arthroplasty group and 11 patients (55%) in the control group.
Disassembly and rescue treatmentThe diagnosis of cut-out was established after a median period of 60 days (P25–P75: 20–105 days).
This period was significantly higher among patients undergoing rescue with arthroplasty (90 days, P25–P75: 62–184 days) than among those in whom the femoral head was preserved (alternative group: 8 days, P25–P75: 14–28 days) (P=.001).
A total of 36 (64.28%) patients underwent hip arthroplasty (arthroplasty group), and the remaining 20 patients (35.72%) received an alternative treatment (alternative group). A total hip arthroplasty was carried out on patients who presented radiographic involvement of the cup by the cephalic screw following cut-out (10 patients, 27.8%) and hemiarthroplasty in cases where the cup was not affected (26 patients, 72.2%), with cemented rods being used in all cases. The alternative treatment consisted in: reduction and distal block of the nailing in five patients (25%), extraction of the osteosynthesis material and new nailing in 13 patients (65%; nine patients with a short Gamma® nail and four with a long Gamma® nail), and conservative treatment by unloading in the two remaining patients (10%) due to a poor overall condition which contraindicated surgery.
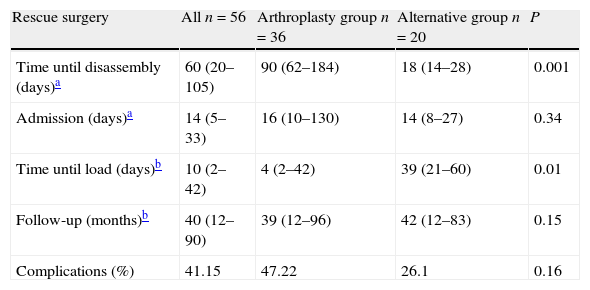
All patients were monitored for a minimum period of 12 months after the rescue surgery. The mean follow-up period and rate of complications were similar in both groups (Table 3), with significant differences in the time until load was authorized following the rescue treatment (4 days in the arthroplasty group and 30 days in the alternative group).
Hospital admissions in rescue surgery.
| Rescue surgery | All n=56 | Arthroplasty group n=36 | Alternative group n=20 | P |
| Time until disassembly (days)a | 60 (20–105) | 90 (62–184) | 18 (14–28) | 0.001 |
| Admission (days)a | 14 (5–33) | 16 (10–130) | 14 (8–27) | 0.34 |
| Time until load (days)b | 10 (2–42) | 4 (2–42) | 39 (21–60) | 0.01 |
| Follow-up (months)b | 40 (12–90) | 39 (12–96) | 42 (12–83) | 0.15 |
| Complications (%) | 41.15 | 47.22 | 26.1 | 0.16 |
During the follow-up period, 23 (41.15%) of the 56 patients presented some complication, with no significant differences being observed between both groups. In the arthroplasty group, 17 patients presented complications: dislocation (n=4), superficial infections (n=4), deep infections (n=1), supracondylar femoral fracture (n=1), cotyloiditis (or acetabular erosion) (n=1), local pain (n=2) and exitus (n=2). In the alternative group, six patients presented superficial wound infection which did not require surgical treatment.
The overall rate of reintervention following the rescue procedure was 3.57%. In the arthroplasty group, two patients required a new intervention (11.7%): 1 episode of dislocation and 1 of deep infection, which were resolved through Girdlestone-type resection arthroplasty. In contrast, there were no cases of reintervention in the alternative group (p=0.01).
At the end of the follow-up period, the functional capacity according to the ability to walk was significantly higher (p=0.004) in the arthroplasty group (Fig. 2).
DiscussionFunctional results obtained with hip arthroplasty compared to other alternative treatmentsRecovering a level of functional capacity similar to that prior to a pertrochanteric fracture continues to be a significant challenge in these patients, not only because of the initial event, but also because of the presence of disassembly, an added complication which causes a setback in the rehabilitation process.
Currently, hip arthroplasty is the most commonly used rescue treatment; however, in the only reference we found comparing functional results according to the rescue treatment employed (arthroplasty, new nailing or replacement of the nail), Chen et al.12 in their series of 432 Gamma® nailings, found no differences between the different treatment options.
The most commonly used functional scales for the hip cannot be extrapolated to patients like those in our series due to their initial deterioration. However, based on an ordinal scale according to the type of gait, with or without technical aids, our study suggests that hip arthroplasty offers better results in these patients (p=0.004). We must add that we found a difference in the time elapsed until load was authorized following the rescue treatment (4 days in the arthroplasty group vs 30 days in the alternative group), which could justify a lower initial functional recovery of patients in the control group. However, the assessment of functional capacity was carried out at the end of the follow-up period (arthroplasty 39 months, control 42 months; p=0.15) and, in our opinion, the possible initial differences due to the delay in load after the intervention should not have had an influence on the capacity to walk assessed after at least 1 year. For this reason, we believe that hip arthroplasty offers better functional results than other alternatives.
In spite of the advantages which arthroplasty could offer, we must not forget the importance of preserving the femoral head. Therefore, we believe that in cases suffering early cut-out we should attempt to preserve the femoral head and carry out a new reduction and nailing, taking into account the general condition and functional demands of each patient. We must also highlight that we found no significant differences between both groups regarding their rates of complications (p=0.16), but the rate of reintervention was higher with arthroplasty (p=0.01). In our cohort, the rate of reintervention reached 11.7%, which was lower than that reported by other authors. In their series of 1533 pertrochanteric fractures with a 3.3% incidence of cut-out, Mokka et al.16 described a rate of reinterventions of 20% among patients treated with hip arthroplasty, with dislocation being the most common complication. Likewise, in their revision of treatment with arthroplasty following failure of the osteosynthesis, Castillón et al.17 presented a series in which 4 out 17 (23.5%) patients required revision surgery, with infection being the main cause.
Radiographic study of technical factors associated to failure of the osteosynthesisA TAD above 20mm is considered as the main predictive factor of failure of the osteosynthesis.10,11 In our study we found a TAD close to 20mm in the alternative group, and, although this is correct from quantitative standpoint, not only was cut-out observed but it also took place earlier than in the arthroplasty group, with a median close to 3 weeks in the control group compared to 3 months in the arthroplasty group (p=0.001). Thus, we believe that TAD is a quantitative measurement which does not seem to explain the onset of this complication by itself.
In our opinion, among other factors with an influence on the onset of cut-out,11 correct reduction of the fracture is the main one, as 63.6% of our patients in the alternative group presented a deficit in the reduction on postoperative radiographs (p=0.01) and no differences were observed in the fracture pattern according to the AO classification between both groups (p=0.13). According to de Bruijn et al.18 based on his series of 290 patients and an incidence of cut-out of 7%, fractures classified as A3 had a risk of cut-out 14 times higher in the short term due to a more unstable pattern and difficulty for their reduction. Nevertheless, in our study we did not find differences between groups related to the fracture pattern. Other works offer data supporting the importance of a correct reduction of the fracture in order to prevent this complication, including Baumgaertner et al.7 who, in a series of 198 patients, conducted a classification of the quality of fracture reduction (good, acceptable and poor), and found percentages of 46% good, 39% acceptable and 15% poor, along with an incidence of cut-out of 8%, mainly in the group with poor reductions. Based on this classification, de Bruijn et al.18 advocated that a poor reduction increases the risk of suffering cut-out by up to five times, thus considering it as one of the main predictive factors of failure.
According to Xu et al.19 the percentage of complications in the first year does not seem to be related to the type of implant. This conclusion can also be observed in the series by Vaquero et al.20 with an incidence of cut-out under 1%. The low incidence in these two works could be related to a good reduction of the fracture, which in both cases was considered as anatomical in over 90% of patients. Based on our experience, we believe that a deficit in reduction of the fracture could explain why cut-out appeared earlier in the alternative group. Furthermore, the moment of onset of disassembly could be a conditioning factor for surgeons to carry out an alternative rescue treatment in cases of early cut-out (less than 4 weeks), compared to treatment with arthroplasty.
The main limitation of our study was the high percentage of patients excluded from the analysis (26.3%), due to the high preoperative mortality rate in this pathology, as well as the incomplete registration of some of the medical histories analyzed. Other limitations of this study are the size of the population analyzed and the fact of comparing the arthroplasty group with treatments which preserved the femoral head, which were heterogeneous in therapeutic options. We attempted to compensate the subjective component of an assessment of the deficit in fracture reduction by having the radiographs examined by two independent researchers, obtaining a good interobserver agreement coefficient.
ConclusionAs conclusion of this work, we believe that rescue with arthroplasty is the treatment of choice in elderly patients, as it offers better functional results compared to other alternatives, although the rate of reinterventions is also higher. Therefore, in cases of early cut-out (<4 weeks) of the osteosynthesis in which the integrity of the femoral head is maintained, we recommend attempting a new nailing before proceeding with the arthroplasty. From the results of our study, we can deduce that a deficit in fracture reduction is the main factor associated to short-term failure, whilst a TAD over 20mm predicts medium- and long-term failure.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Cuervas-Mons M, Mora F, López Fernández J, Chana F, Vaquero J. Desmontaje por efecto cut-out en el enclavado de fracturas pertrocantéreas de fémur: ¿cuál es el tratamiento de rescate de elección? Rev Esp Cir Ortop Traumatol. 2014;58:357–363.