The aim of this study is evaluate clinical and radiographic outcomes of Latitude elbow hemiarthroplasty in the treatment of articular distal humerus multifragmentary fractures in patients older than 65 years.
Material and methodsWe included those patients older than 65 years who sustained an unreconstructable articular distal humeres fracture and it was replace with a Latitude hemiarthroplasty. We excluded those with a minimum follow up less than 2 years.
The clinical outcomes were assessed with Mayo Elbow Performance Score (MEPS). Range of motion, pain, complications and elbow radiological assessments were recorded at the final follow up.
ResultsWe have found that after a mean follow-up of 5 years, the five patients included in the study have mild pain in the elbow. They have recovered a median flexion arch of 100°, with a 10° extension lag. The MEPS was considered as good in all the cases. There were not any instability or prosthesis loosening, but two patients developed a moderate proximal cubitus wear.
ConclusionLatitude elbow arthroplasty is an option in the distal articular humerus multifragmentary fractures treatment in osteoporotic and ageing patients with satisfactory results as long as the elbow ligamentous stability can be restored.
El objetivo es exponer los resultados clínicos y radiológicos del tratamiento de las fracturas de húmero distal complejas en pacientes mayores de 65 años con una hemiartroplastía de húmero distal (HHD) tipo Latitude EV.
Material y métodoSe incluyeron a pacientes mayores de 65 años en quienes se implantó una HHD tipo Latitude tras una fractura irreparable de húmero distal, excluyendo aquellas con un seguimiento menor a dos años.
Se recogieron datos sobre el dolor al final del seguimiento, empleando la escala visual analógica (EVA), el balance articular, el resultado funcional, usando la escala Mayo Elbow Performance Score y las complicaciones. También se valoró el resultado final radiológico.
ResultadosCinco pacientes fueron incluidas en el estudio, con un seguimiento medio de cinco años. Todas experimentaron un dolor considerado como leve, recuperando un arco de flexión de 100° de media y con un déficit de extensión medio de 10°. La valoración funcional se tomó como buena en todas las pacientes, presentando como complicaciones, una infección. No hubo ningún caso de inestabilidad ni de aflojamiento de la prótesis y en dos casos se produjo un desgaste moderado del cúbito.
ConclusionesLa HHD tipo Latitude EV es una opción a tener en cuenta en el tratamiento de las fracturas irreparables de húmero distal en población geriátrica con baja demanda funcional, siempre y cuando consigamos restaurar la estabilidad, reparando los ligamentos o los epicóndilos.
Although standard treatment of distal humeral fractures of the epiphysis is open reduction and internal fixation,1–4 this is quite complex and demanding surgery, further complicated in elderly patients where an osteoporotic bone makes stable osteosynthesis difficult, and this is usually combined with comminution, sometimes leading to unreconstructable fractures or repairable fractures with questionable stability.5 In these cases, due to the unsatisfactory functional results there is a tendency for total elbow replacement (TER) to be used. Several articles report a similar percentage of good or excellent outcomes, with fewer complications with joint replacement than with osteosyntheis.6,7
Even so, TER are still prone to complications8 such as loosening, polyethylene wear, instability, and also weight lifting restrictions. In order to minimise these disadvantages, distal humeral hemiarthroplasty (DHH) was developed. Although the first published article9 which refers to its use dates from 1947, it was not until 2005 when it began to be used in the treatment of unreconstructable distal humeral fractures. Adolfsson10 and Parsons11 used a Judo type prosthesis (Biomet, Warsaw, In, U.S.A.) or Sorbie-Questor (Wright Medical Technology, Arlington, TN, U.S.A.) type, respectively, to replace the distal humerus, achieving good or excellent results in 100% of their cases. We should bear in mind that both prostheses were not initially designed to be used as hemiarthroplasties.
At present, there is a convertible TER in the market, which was also designed to be able to be used as DHH: the Latitude EV (Wright Medical Technology, Arlington, TN, USA). Although the outcomes obtained in the different series published are quite satisfactory short-term,12–15 there are few articles which document their behaviour in the mid-to-long term and their repercussions on the ulna and radius.16–20
As a result the aim of this study was to evaluate medium-term results in the treatment of unreconstructable distal humeral fractures in patients over 65 years of age using a Latitude EV type DHH.
Material and methodsA retrospective case series study was designed, collecting data from patients over 65 years of age who suffered from an unreconstructable distal humeral joint fracture between the years of 2009 and 2016 and who received a Latitude type DHH implant. Those people where joint replacement was made for other non-trauma pathologies and those in follow-up for under 24 months were excluded.
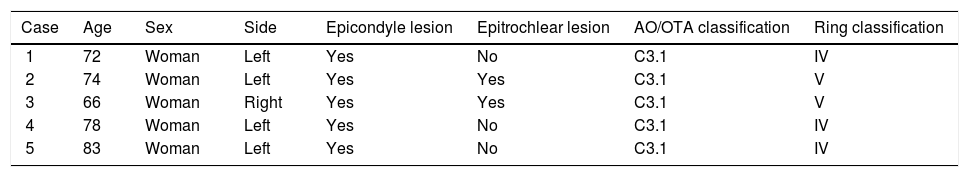
Five patients met with these criteria, all of whom were women. The mean age of patients was 74 years, with a range of between 66 and 83 years. All fractures had occurred due to low-energy trauma from a standing height fall. The upper limb affected was the left in four cases and the right in one. In all of them the distal humeral fracture was considered as C3.1, according to the classification by the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA).21 If we use the classification described by Ring,22 three cases were considered within type IV and two as type V fractures, with involvement of the medial epicondyle included. In one of the patients (case 1) the extensor mechanism of the elbow had been pulled out, with a bone fragment of 2cm in the posterior surface of the olecranon. In another case (case 3) there was an olecranon-associated fracture (Table 1). Prior to surgery computerised tomography was requested to assess the possibility of joint surface reconstruction, but the final decision to carry out distal humeral replacement was made intraoperatively when the surgeon considered the fracture unreconstructable.
Patient and lesion data.
| Case | Age | Sex | Side | Epicondyle lesion | Epitrochlear lesion | AO/OTA classification | Ring classification |
|---|---|---|---|---|---|---|---|
| 1 | 72 | Woman | Left | Yes | No | C3.1 | IV |
| 2 | 74 | Woman | Left | Yes | Yes | C3.1 | V |
| 3 | 66 | Woman | Right | Yes | Yes | C3.1 | V |
| 4 | 78 | Woman | Left | Yes | No | C3.1 | IV |
| 5 | 83 | Woman | Left | Yes | No | C3.1 | IV |
AO: Arbeitsgemeinschaft für Osteosynthesefragen; OTA: Orthopaedic Trauma Association.
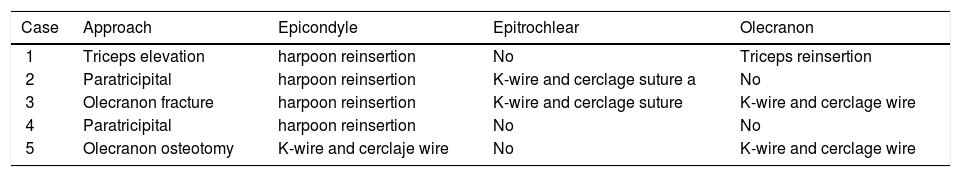
All patients received a Latitude EV type DHH in keeping with the technique described by the manufacturer. In one case, the Morrey23 approach was used, reflecting the triceps, in two cases the paratricipital approach was used and in two prostheses were implanted, through olecranon osteotomy in one and using the olecranon fracture in the other to subsequently fix it at the beginning of the tension band with two Kirschner wires (K-wires) and a cerclage wire. If there was collateral ligament or epicondyle damage, these were repaired in all women, either through reinsertion with harpoons or K-wires and cerclage wire, to achieve a stable joint. The ulnar nerve was isolated and protected throughout surgery and an anterior, subcutaneous transposition in all patients after prosthesis implantation was performed (Table 2).
Surgical procedures.
| Case | Approach | Epicondyle | Epitrochlear | Olecranon |
|---|---|---|---|---|
| 1 | Triceps elevation | harpoon reinsertion | No | Triceps reinsertion |
| 2 | Paratricipital | harpoon reinsertion | K-wire and cerclage suture a | No |
| 3 | Olecranon fracture | harpoon reinsertion | K-wire and cerclage suture | K-wire and cerclage wire |
| 4 | Paratricipital | harpoon reinsertion | No | No |
| 5 | Olecranon osteotomy | K-wire and cerclaje wire | No | K-wire and cerclage wire |
K-wire: Kirschner wire.
Antibiotic prophylaxis was performed with the intravenous administration of cefazolin and tobramycin, and thromboembolic prophylaxis with enoxaparin for 10 days. No prophylaxis was used against heterotopic ossifications. An articulated elbow orthesis was used postoperatively for elbowflexion and extension from the first few days, and which protected the repair of the ligaments and epicondyles for eight weeks. During this time, heavy object weight-bearing with the operated limb was restricted.
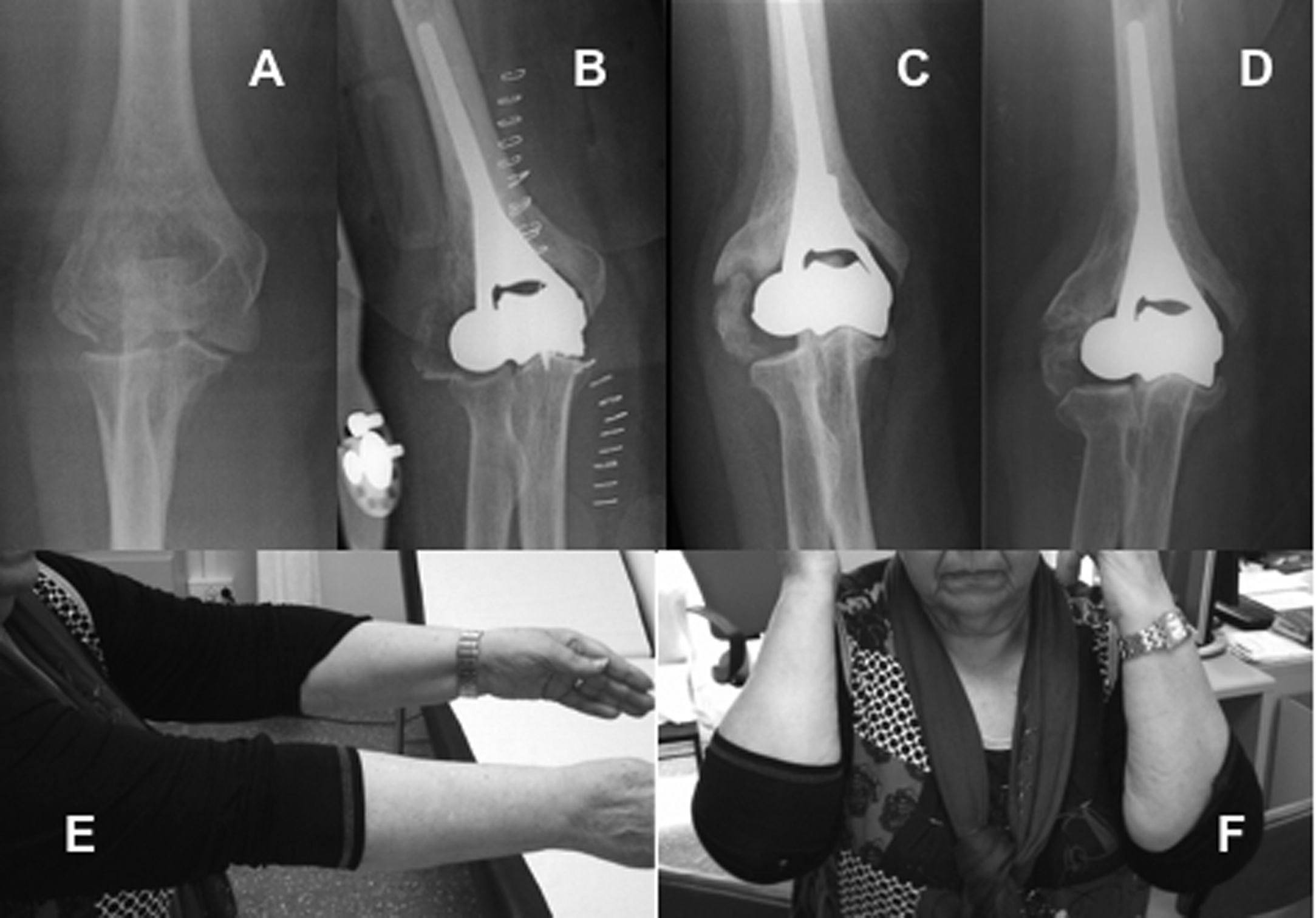
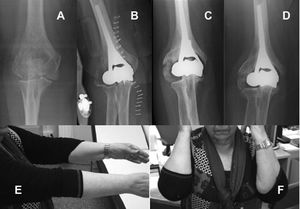
Patients were assessed at the end of follow-up both functionally and radiologically. In this visit, the presence of pain was recorded on the visual analogue scale (VAS) (considering the intensity of pain as mild between 1 and 3, moderate between 4 and 7 and severe between 8 and 10), joint balance during flexion and extension of the elbow and during pronation and supination and the Mayo Elbow Performance Score (MEPS) was used to assess functional results. The stability of the prosthesis was assessed using the varus/valgus forces with the elbow completely extended and in flexion of 30°, classifying it as grade 1 when there was a mild opening and grade 2 when joint subluxation occurred. Postoperative complications were also recorded (Figs. 1 and 2).
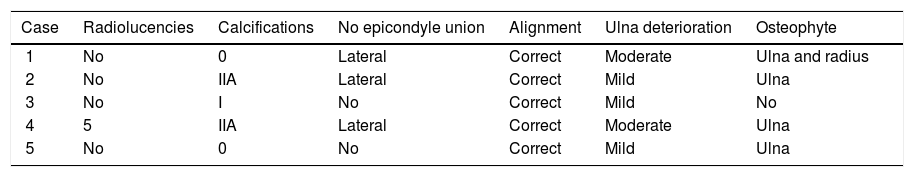
To complete radiologic evaluation, an anteroposterior and lateral X-ray of the elbow was taken at the end of follow-up, where the presence of the following was assessed:
- •
Radiolucent lines or changes in the cement around the prosthetic stem, recording size, progression and location, in keeping with the criteria described by Smith et al.,19
- •
The appearance of heterotopic calcifications, using the Hastings classification,24
- •
Consolidation of the epcondyles,
- •
Alignment of the radius to the prosthesis, searching for signs of instability, tracing the axis of the radius and assessing the cut-off point of this line in the capitellum in lateral X-rays made during and at the end of follow-up,13
- •
Alignment between the prosthesis and the ulna, searching for changes in the humeroulnar angle in anteroposterior X-rays,
- •
Wear of the ulna and proximal radius cartilage, assessing humeroulnar and humeroradial distance in anteroposterior X-rays, considering that this is mild when the distance is similar to that existing in postoperative X-rays, moderate when there is an obvious reduction and severe when there is no space between the prosthetic component and the native bone, and
- •
The appearance of osteophytes and their location.
One of the patients died two and a half years after surgery, with the other four being assessed at the end of follow-up. The MEPS was completed for the deceased with data obtained from the medical file and radiologic assessment was made from the last radiologic control performed. Mean follow-up time was five years, with a range between two and eight years.
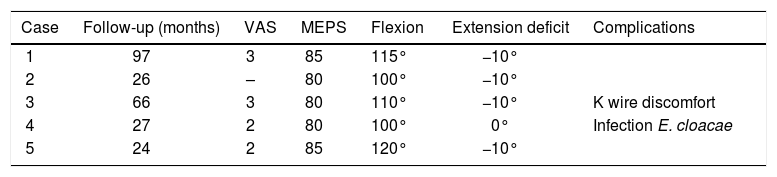
Assessing pain with the VAS, the intensity was mild in all patients. The mean flexion arc obtained was 100°, with a range between 100° and 120°. Maximum flexion reached ranged between 100° and 120°, and the maximum extension deficit was 10°. Pronation and supination was completely recovered in all cases. There was no frank instability, although in all a slight opening occurred in varus/valgus which we considered to be physiological. According to the MEPS results were classified as good in all patients (Table 3).
Functional results and complications.
| Case | Follow-up (months) | VAS | MEPS | Flexion | Extension deficit | Complications |
|---|---|---|---|---|---|---|
| 1 | 97 | 3 | 85 | 115° | −10° | |
| 2 | 26 | – | 80 | 100° | −10° | |
| 3 | 66 | 3 | 80 | 110° | −10° | K wire discomfort |
| 4 | 27 | 2 | 80 | 100° | 0° | Infection E. cloacae |
| 5 | 24 | 2 | 85 | 120° | −10° |
MEPS: Mayo Elbow Performance Score; VAS: visual analogue scale.
Regarding complications, two were recorded: one of the cases required further surgery to remove some of the K-wires which attached the olecranon fracture and lateral epicondyle, as they had moved, and in another patient a superficial Enterobacter cloacae infection occurred which was controlled and eliminated by the administration of ciprofloxacin for four weeks. None of the patients presented with ulna nerve damage.
Radiologic assessment led us to observe one case where a radiolucent line under 1mm existed in area 5 in the anteroposterior X-day at five months and this remained without changes until termination of follow-up (Table 4). In two cases there were no heterotopic calcifications, whilst in the other three minor calcifications appeared in the collateral ligaments and in two of them a larger sized calcification also presented around the anterior flap of the prosthesis which led to flexion limits. In three patients lateral epicondyle consolidation was not achieved, despite having repaired it, but in all of them alignment between the humeral component, proximal end of the ulna and radial head was maintained, with no signs of instability, both in coronal and sagittal plane.
In three cases, wear between prosthesis and bone, which was considered mild, occurred. In another two cases a reduction in space was considered moderate. In four patients an osteophyte appeared in the medial part of the coronoids and in the case with a longer follow-up also in the radial head.
DiscussionAlthough good or excellent outcomes have not been obtained in all studies published, in a large percentage of cases,12,14 expectations were to obtain between 70% and 80% of satisfactory results with the use of DHH in the treatment of both unreconstructable distal humeral fractures and to treat the faults in distal humeral fracture fixation,13,15,16,18,19,25 which we confirmed with results obtained in our patients.
Using DHH instead of TER, we sought to reduce the number of complications relating to the implant. In one of the latest reviews undertaken on the failure of the TER mechanism,8 it was commented that the percentage of loosening was approximately 4%, although no reference was made to which component had come loose or why the TER had been used. Rangarajan26 assessed loosening in TER used in the treatment of distal humeral fractures, with this complication presenting in 6% of patients. When we analysed loosening with DHH in published series, we noted that it appears in approximately 2%.25 Smith19 recorded two cases, using one Sorbie-Questor elbow, and Nestorson16 one Latitude loosening, which represents .8% of all EV latitude prostheses implanted. Unlike Kudo and Sorbie-Questor, the Latitude EV prosthesis has an anterior flap, which allows for the implantation of a bony graft, the purpose of which is to reduce the mechanical stress between the humeral component and the coat of cement, transferring the load to the distal humerus.27 This means that the risk of humeral component loosening should diminish, but in the case of the TER, the problem is transferred to the ulna component and to the interconnection system between both components. Excess load supporting the ulnar component may lead to it loosening, but another cause of this is the reaction to a foreign body which occurs when polyethylene particles are released on deterioration found in the interconnection system. Therefore, one advantage of DHH compared to TER is that by only implanting the humeral component, in theory there is less likelihood of loosening, as the risk of complications relating to the other components is reduced. As a result, we did not limit patient activities, just like in the majority of studies with DHH.11,12,16,18 Furthermore, we should recall that, in this age group, functional demand is usually lower than in a younger and more active population. These factors may also impact the fact that there are fewer periprosthetic fractures: between 2% and 3% in TER8,26 compared with two cases of Sorbie-Questor19 type DHH, one Kudo28 type and none with Latitude EV. However, this could simply be due to the lower number of DHH implants used.
Although we eliminated the complications relating to the ulna component, the ulna may still be damaged, since the different elasticity module between the prosthetic metal and the native bone of the proximal end of the ulna and the radial head may lead to wear and loss of joint cartilage. This event has been reported in the ulna in 41% of patients who received DHH and in 11% in the radial head,29 but it is unclear whether their presence results in a poor outcome. In our series, we did not find severe clamping of the joint interline in any cases, even in the two with greater follow-up. The major problem when assessing native bone wear was how to measure it, because with radiologic projections sometimes it is difficult as they are not always well executed.15,19 Hohman14 suggested evaluation should be made using computerised tomography, but not all patients wish to undergo unjustified radiation.
Another inherent problem of DHH, which TER does not suffer from, is instability. It is well-known fact that one of the essential requirements for positioning DHH is having whole epicondyles and ligaments or the possibility of repairing them because, if not, the prosthesis would not be stable, giving rise to the loss of congruence between the prosthesis and the ulna and head of the radius and, therefore, to a poor outcome. Review of the literature reveals that this complication only appears to be recorded in one case,17 which indicates that it is one of the priorities of surgeons during intervention.29 Heijink17 states that the reason for instability is failure in repairing the external lateral ligament after its de-insertion when exposing the distal humerus and therefore recommends using an access route to preserve the origin of the ligaments. When there is epicondyle fracture, it is rare for the ligaments to be avulsed from the bone, and repair of the epicondyles should therefore re-establish stability. The size of the fragment which contains the origin of the ligament will determine the type of repair: in the case of tiny fragments, fixture may be made with transosseous suture or through the prosthesis,15 whilst if they are larger, plates, screws, K-wire or cerclage wires may be used for attachment. In the literature both Nestorson16 and Phadnis15 achieve consolidation of the epicondyles in over 90% of cases, whilst in those where this has not been achieved, there is no displacement during follow-up, similarly to the three patients in our series. This non-consolidation of the epicondyles is a radiologic finding without medical repercussions, since the minor movement generated in the focus of the non union is insufficient to give rise to a loss of ligament-stabilising function.
The series report a higher number of complications, but the rest of them have no relationship with the implant itself. They are due to the procedure itself, and include neurological lesions, particularly of the ulna nerve, superficial or deep infection, skin healing problems, failure of extensor mechanisms, heterotopic ossifications or problems relating to the osteosynthesis material. The latter begin to appear in up to 31% and 18% of treated cases,25,29 with figures similar to those obtained in open reduction and internal fixation or with TER.
We realise that the conclusions which may be gained from this small retrospective cases series are weak in validity and further studies with larger series are necessary, although this is difficult due to the low frequency of this type of fractures. Also, although in our research there are two cases with a follow-up of over five years, it is vital to confirm that results are maintained over time during long-term follow-up. The strength of this study is found in the fact that all patients were operated on by the same surgeon and the homogeneity in their selection.
ConclusionThe Latitude EV type DHH is an option to consider in the treatment of distal humeral unreconstructable fractures in the elderly population with a low functional demand, provided that we are able to restore stability repairing ligaments or epicondyles.
Level of evidenceLevel of evidence IV.
FinancingThis study did not receive any type of financing.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ricón-Recarey FJ, Lajara-Marco F, Fuentes-Díaz A, Correoso-Castellanos S. Resultados de la hemiartroplastía de húmero distal Latitude en el tratamiento de las fracturas articulares de húmero distal irreparables en mayores de 65 años. Rev Esp Cir Ortop Traumatol. 2021;65:272–278.