Periprosthetic fractures after primary knee arthroplasty has great importance in our environment due to the increase in their incidence and to the challenge they pose to the surgeon. Multiple factors have been associated with its production. The objective of the study was to identify the risk factors that could influence the appearance of these fractures, which of them are all modifiable and generate a probability prediction model based on these factors.
Material and methodsAnalytical, observational, retrospective, unpaired study of 38 cases of periprosthetic femoral knee fractures and 80 controls with knee prostheses. In total, 118 patients, 83 women and 35 men with a mean age of 72.49 years were included in the study. Sociodemographic data, medical history and drug consumption were collected, as well as those related to surgery. A univariate and bivariate analysis of the fracture determining factors was performed, using a logistic regression model to avoid confusion bias.
ResultsOf all the factors studied according to the logistic regression model, it was obtained that female sex (OR = 7.6), dementia (OR = 5), motor/Parkinson’s alteration (OR = 19.3) and femoral overcut Previous (OR = 8.6) were factors associated with the increased risk of this type of fractures.
ConclusionsThis work allows us to conclude that there are risk factors such as female sex, dementia and Parkinson’s that increase the probability of periprosthetic fracture that are inherent to the patient and are not modifiable. However, there is any other totally modifiable that can be avoided by being demanding and thorough in the surgical technique, such as the anterior femoral overcut.
Las fracturas periprotésicas tras artroplastia primaria de rodilla cobran gran importancia en nuestro medio debido tanto al aumento de su incidencia, como al reto que suponen para el cirujano. Múltiples factores se han asociado a su producción. El objetivo del estudio fue identificar los factores de riesgo que podían influir en la aparición de estas fracturas, cuáles de todos ellos son modificables y generar un modelo de predicción de probabilidad de las mismas en función de dichos factores.
Material y métodoEstudio analítico, observacional, retrospectivo, no pareado, de 38 casos de fracturas periprotésicas femorales de rodilla y 80 controles con prótesis de rodilla. En total, fueron incluidos en el estudio 118 pacientes, 83 mujeres y 35 hombres con una edad media de 72,49 años. Se recogieron datos sociodemográficos, antecedentes médicos y consumo de fármacos, así como los relativos a la cirugía. Se realizó un análisis uni- y bivariante de los factores determinantes de fractura, usando un modelo de regresión logística para evitar el sesgo de confusión.
ResultadosDe todos los factores estudiados según el modelo de regresión logística, se obtuvo que el sexo femenino (OR = 7,6), la demencia (OR = 5), la alteración motora/párkinson (OR = 19,3) y el sobrecorte femoral anterior (OR = 8,6) eran factores asociados al incremento de riesgo de este tipo de fracturas.
ConclusionesEste trabajo permite concluir que hay factores de riesgo, como son el sexo femenino, la demencia y el párkinson, que aumentan la probabilidad de fractura periprotésica, que son inherentes al paciente y no son modificables. Sin embargo, existe algún otro totalmente modificable que puede evitarse siendo exigente y exhaustivo en la técnica quirúrgica, como es el sobrecorte femoral anterior.
Periprosthetic knee fractures are those that occur in a patient who has undergone total knee arthroplasty (TKA), occurring less than 15 cm from the joint space or 5 cm from the stem if there is one.1 They usually occur in the context of low energy trauma in up to 94%.2 Patients’ increased life expectancy and quality of life has led to increased indications for TKA.1,3 Increased survival of the population could result in a decrease in periprosthetic bone quality1,3 and increase the incidence of periprosthetic fractures, which currently varies between .2% and 2.5%4 in the supracondylar area. These fractures are important in our setting and are currently a subject of some controversy, since they often pose a challenge for the orthopaedic surgeon as they occur in loosened implants and that complicate the surgical technique. Moreover, these are fractures that affect elderly patients in the main with high mortality5 and associated morbidity.6,7
A number of factors have been described that appear to be associated with how these fractures occur.8–10 The patient-dependent factors are advanced age, female sex8,9 and certain diseases such as rheumatoid arthritis, neurological diseases, treatment with steroids and osteoporosis.10,11 In terms of surgical factors, anterior femoral overcut, the presence of post-stabilised implants and osteolysis and/or loosening have been studied.1,4,10,11 However, these factors are reviewed in clinical series in which only a univariate analysis has been performed, which could introduce a confounding bias that would lead to overexposure of different factors.
Our objective was to identify the risk factors that could influence the onset of periprosthetic fractures, evaluating those that can be modified, and also to generate a model for predicting the probability of these fractures according to these factors.
Material and methodAnalytical, observational, retrospective, unpaired study of 38 cases (periprosthetic femoral knee fractures) and 80 controls (people who have undergone TKA without fracture). The case-control collection period was from January 2006 to October 2016 with an average time from prosthesis to fracture of 9 years.
Case/patient definition: patients admitted with a fracture around the femoral component less than 15 cm from the joint space1 in primary TKA, after low energy trauma. Patients with tibial or patella fractures (3), revision surgery (5) and interprosthetic or interimplant fractures (7) were excluded.
The controls were defined as patients who had undergone primary TKA without periprosthetic fracture. Once the cases were identified, a list of all the TKAs performed in the same study period was obtained and simple manual randomisation was applied. The sample was ordered by case history number by randomly selecting a starting point and then the direction of movement was kept constant throughout the table, in our case on the right. By agreement, the last even numbers (0, 2, 4, 6 and 8) were included in the sample and the last odd numbers (1, 3, 5, 7 and 9) were excluded from the study until the required number of controls was completed.
Sociodemographic data, age and sex, as well as weight, height and body mass index (BMI) were collected. Clinical data, such as intake of drugs associated with decreased bone mass (corticosteroids), intake of antidepressants and/or benzodiazepines, the presence of dementia, blindness, alcoholism, osteoporosis or osteopenia (taking as criteria for osteoporosis those patients who met clinical and radiological criteria in relation to previous fractures, with a bone mineral density measured by T-score in the spine, femoral neck or hip ≤1.0 and ≥2.512) or rheumatological and neurological disease (neurological diseases included those related to motor and balance disorders such as Parkinson’s disease [9], ataxia [1] or tetraparesis caused by ALS [1]).
From the point of view of surgery, we identified the presence or absence of anterior femoral overcut, the type of implant, measurement of cortical thickness and diameter of the femoral channel in mm at mid-diaphyseal level. The measurement was performed with a digital ruler provided by the image viewer software (RAIM Java 2009 _DICOM Java_ viewer) after resampling the image from a radiological mark (to scale). Presence was defined on the femoral cut in those patients in whom penetration of the implant in the anterior cortex was observed to be greater than 2 mm on the postoperative strict lateral radiography.13 The presence of osteolysis or implant loosening was also assessed, defining a loosened implant as one that presented radiological criteria of continuous osteolysis greater than 2 mm with significant alterations in alignment (greater than 3° in any projection) of the implant or associated fracture of the cement.
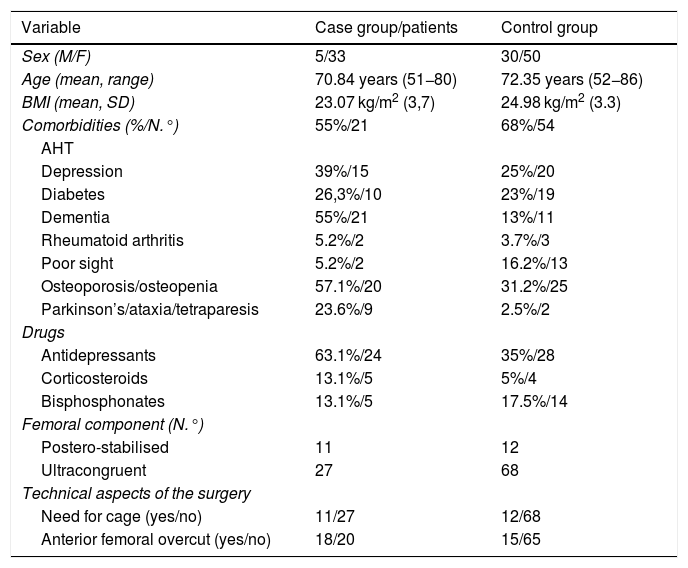
All sociodemographic parameters, comorbidities and surgical aspects can be seen in Table 1.
Case group and control group comparison table.
| Variable | Case group/patients | Control group |
|---|---|---|
| Sex (M/F) | 5/33 | 30/50 |
| Age (mean, range) | 70.84 years (51−80) | 72.35 years (52−86) |
| BMI (mean, SD) | 23.07 kg/m2 (3,7) | 24.98 kg/m2 (3.3) |
| Comorbidities (%/N.°) | 55%/21 | 68%/54 |
| AHT | ||
| Depression | 39%/15 | 25%/20 |
| Diabetes | 26,3%/10 | 23%/19 |
| Dementia | 55%/21 | 13%/11 |
| Rheumatoid arthritis | 5.2%/2 | 3.7%/3 |
| Poor sight | 5.2%/2 | 16.2%/13 |
| Osteoporosis/osteopenia | 57.1%/20 | 31.2%/25 |
| Parkinson’s/ataxia/tetraparesis | 23.6%/9 | 2.5%/2 |
| Drugs | ||
| Antidepressants | 63.1%/24 | 35%/28 |
| Corticosteroids | 13.1%/5 | 5%/4 |
| Bisphosphonates | 13.1%/5 | 17.5%/14 |
| Femoral component (N.°) | ||
| Postero-stabilised | 11 | 12 |
| Ultracongruent | 27 | 68 |
| Technical aspects of the surgery | ||
| Need for cage (yes/no) | 11/27 | 12/68 |
| Anterior femoral overcut (yes/no) | 18/20 | 15/65 |
The prosthetic models were Nex Gen® (Zimmer) in 5 of the controls and in 9 cases, Apex® (OMNIlife science) in 35 controls and in 6 cases, Natural Knee II® (Zimmer) in 35 controls and 21 cases and Persona® (Zimmer) in 5 controls and 2 cases. The type of implant was considered according to the design of the implants, and divided into two groups, postero-stabilised models with the need for a femoral cage and models with preservation of posterior/ultracongruent cruciate.
The fractures were classified according to the criteria of Lewis and Rorabeck 14 and those of Su.10 According to Lewis and Rorabeck’s classification, the most frequent type was type II (60.5%) followed by type I (23.7%), Su’s most frequent classification was type III (39.5%).
The mean interval between replacement surgery and fracture was 108.3 months, with 94.7% of the fractures being considered late, since more than 6 months had passed since the primary surgery.
The statistical analysis was divided into two parts. On the one hand, the descriptive statistics in which proportions and means were calculated with their corresponding 95% confidence intervals. And on the other, the Pearson Chi-square test was used to contrast hypotheses in the case of qualitative variables. If not all the requirements for the application of the test were met, Yates correction or the Fisher exact test was applied. For quantitative variables, the Student’s t-test was used if they met the criteria of normality, otherwise the Mann–Whitney U test. Likewise, a binary logistic regression model was established with the aim of avoiding probable confounding bias due to the analysis of factors that could act together. SPSS v. 22.0 and a general significance level p < .05 were used.
The sample size was estimated using G * Power version 3.1.7 (Franz Faul; UniKiel, Düsseldorf, Germany) according to minimum sample size evaluation criteria, with α = .05 and β = .10 for the study factors. According to previous studies, the frequency of exposure in non-patients for the main modifiable parameters of the study (anterior femoral overcut) was 5%,12 the frequency of exposure among patients was 30%,13 for an odds ratio (OR) = 2.00, with two controls for each case we obtained a minimum necessary sample of 35 cases and 75 controls to achieve conclusions with statistical significance.
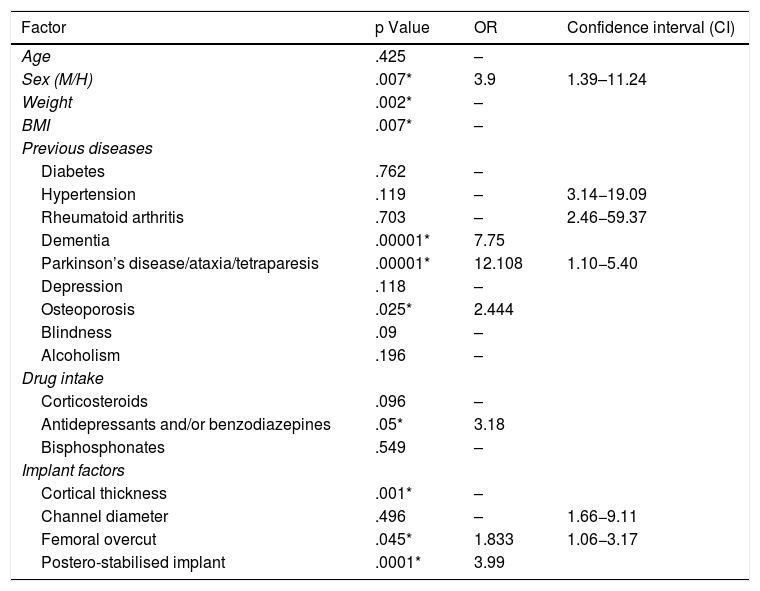
ResultsThe result of the univariate analysis is shown in Table 2. With regard to patient characteristics, female sex (p = .007), lower weight (p = .002) and lower BMI (p = .007) were identified as risk factors. In the assessment of previous diseases, we observed that osteoporosis (p = .025), dementia (p = .0000) and previous psychomotor disorder (p = .00) seemed to have an influence. From a surgical point of view, we observed that the cortical thickness was significantly lower in the fracture group (p = .0001). The presence of anterior femoral overcut (p = .001) and the need for a drawer (p = .045) also had a significant influence.
Factors listed in univariate study.
| Factor | p Value | OR | Confidence interval (CI) |
|---|---|---|---|
| Age | .425 | – | |
| Sex (M/H) | .007* | 3.9 | 1.39–11.24 |
| Weight | .002* | – | |
| BMI | .007* | – | |
| Previous diseases | |||
| Diabetes | .762 | – | |
| Hypertension | .119 | – | 3.14−19.09 |
| Rheumatoid arthritis | .703 | – | 2.46−59.37 |
| Dementia | .00001* | 7.75 | |
| Parkinson’s disease/ataxia/tetraparesis | .00001* | 12.108 | 1.10−5.40 |
| Depression | .118 | – | |
| Osteoporosis | .025* | 2.444 | |
| Blindness | .09 | – | |
| Alcoholism | .196 | – | |
| Drug intake | |||
| Corticosteroids | .096 | – | |
| Antidepressants and/or benzodiazepines | .05* | 3.18 | |
| Bisphosphonates | .549 | – | |
| Implant factors | |||
| Cortical thickness | .001* | – | |
| Channel diameter | .496 | – | 1.66−9.11 |
| Femoral overcut | .045* | 1.833 | 1.06−3.17 |
| Postero-stabilised implant | .0001* | 3.99 | |
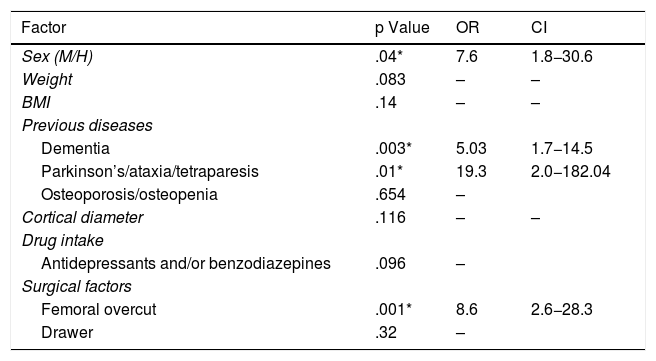
With regard to the logistic regression model, we initially used a Wald's backward regression model which determined that low BMI, osteoporosis, antidepressants, cortical thickness and postero-stabilised implants could be considered factors influenced by the others. In an introductory analysis it was found that, on removing the confounding factors, the remaining factors reached higher values in terms of periprosthetic fracture risk. According to the logistic regression model, the risk factors for periprosthetic fracture are sex, dementia, Parkinson’s disease and anterior femoral overcut. The factor with the greatest association is a history of Parkinson’s disease according to our sample (OR = 19.3; CI = 2.0–182.04; p = .01) followed by anterior femoral overcut (OR = 8.6; CI = 2.6–28.3; p = .001) and female sex (OR = 7.6; CI = 1.8–30.6; p = .04) (Table 3). Analysis of the logistic regression model could explain almost 65% of the variance (intermediate power). Of the sample, 78.8% were correctly classified with a specificity of 91.3%. This model also generates the following mathematical equation that could predict the probability of fracture (Fig. 1)
Factors listed in multivariate study.
| Factor | p Value | OR | CI |
|---|---|---|---|
| Sex (M/H) | .04* | 7.6 | 1.8−30.6 |
| Weight | .083 | – | – |
| BMI | .14 | – | – |
| Previous diseases | |||
| Dementia | .003* | 5.03 | 1.7−14.5 |
| Parkinson’s/ataxia/tetraparesis | .01* | 19.3 | 2.0−182.04 |
| Osteoporosis/osteopenia | .654 | – | |
| Cortical diameter | .116 | – | – |
| Drug intake | |||
| Antidepressants and/or benzodiazepines | .096 | – | |
| Surgical factors | |||
| Femoral overcut | .001* | 8.6 | 2.6−28.3 |
| Drawer | .32 | – | |
Female sex, neurological diseases and excessive anterior femoral cut are the factors most associated with the occurrence of periprosthetic femoral fractures.
The loss of oestrogen influence after menopause, with the consequent bone loss, and a longer life expectancy make women more susceptible15 to periprosthetic fractures, making it one of the most influential factors.9,16 Less osteoblastic stimulus due to a decrease in mechanical demands on the femur associated with a lower production of certain molecules associated with the panniculus adiposus, such as estrone or leptin, means that patients with a lower fat content have lower bone mineral density, significantly increasing the risk of fractures.15 This would explain the association of low weight with the presence of fragility fractures.17,18 Obesity, as in the literature, has not been listed as a risk factor.19
In relation to clinical variables, Parkinson’s disease, other neurological/motor diseases and dementia may lead to an increased or greater risk of falls.20–22 In addition, it has been described that these patients have a lower BMI compared to controls without disease, less physical activity and muscle strength, possibly associated with malnutrition, as well as vitamin D deficiency20 and have significantly reduced bone mineral density which could favour the onset of any type of fracture.21 Osteopenia behaves as a confounder due to the characteristics of the sample as its incidence increases with age and is more frequent in women.22–24 In the literature,25 we found that rheumatoid arthritis and corticosteroid intake have been associated with a greater risk of periprosthetic fracture, unlike this study which found no association. This may be due to the low representation of these factors in the sample, less than 5% in the case of rheumatic disease and 8.6% for steroid intake.
In terms of factors arising from surgery, anterior femoral overcut is the second risk factor for periprosthetic fractures. This aspect generates controversy in the literature, since theoretical studies indicate that with cuts larger than 3 mm the torsional strength of the bone decreases from 29%26 to 39%27 and flexion strength by 18%.27–29 In the study conducted by Lesh et al.27 on 164 periprosthetic fractures of the distal femur, anterior femoral overcut was found to be present in 30% of cases. However, in other studies, such as that of Ritter et al.28 and Gujarathi et al.,29 no differences were found. Cortical thickness was significantly lower in the fracture group behaving as a risk factor. Studies have been conducted on interprosthetic fractures, where it has been observed that narrower cortices, with wider channel diameters, are associated with interprosthetic fractures.30 Postero-stabilised implants have traditionally been associated with periprosthetic fractures for two reasons.31 Firstly, because of the need to create a femoral cage and secondly due to the transmission of forces created by postero-stabilised polyethylene implants which transfer overload or increased tension in the supracondylar area. According to the results, postero-stabilised implants do not increase the risk of periprosthetic fracture by themselves, because although in the univariate study it was seen that it could be associated as a risk factor, when the logistic regression was performed it was perceived to be influenced by the rest, behaving as a confounding factor.
We recognise some limitations of the study. Firstly, it is a retrospective case-control study that is very susceptible to the introduction of bias. Secondly, the low incidence of some factors associated with fractures could affect the univariate analysis. However, it should be noted that this is a multivariate mathematical model that allows us to statistically control for confounding factors, and presents high global sensitivity (78.8%) with high specificity (91.3%), which would enable susceptible patients to be correctly identified. In addition, a sample size was selected in accordance with the study objective in terms of power and the statistical significance sought.
With these data, we can conclude that female sex, dementia, Parkinson's disease, other neurological diseases and anterior femoral overcut are the factors most associated with the onset of periprosthetic femoral knee fractures. The first four are not modifiable factors, but their being known and present in patients should set in motion a multidisciplinary plan for the control of these diseases at the time that primary knee surgery is indicated and during its follow-up. The objective would be to identify these patients using the probability prediction model (Fig. 1), in order to control and treat underlying disease, optimise them and reduce the incidence of falls, with the ultimate goal of reducing the incidence of periprosthetic fractures. A systematic review on Parkinson’s disease provides evidence for exercise-based intervention as a treatment option for the prevention of falls, not only from a clinical point of view, but also in terms of cost effectiveness.32
In addition, careful surgical technique on our part, which avoids femoral overcutting, could also help to reduce the incidence of these fractures.
Prospective and more extensive studies will be necessary to assess whether these results are reproduced in patients with the risk factors identified.
Level of evidence IV.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Redondo-Trasobares B, Torres-Campos A, Calvo-Tapies JR, Gran-Ubeira N, Blanco-Rubio N, Albareda-Albareda J. Factores de riesgo en fractura periprotésica femoral tras artroplastia sustitutiva primaria de rodilla. Rev Esp Cir Ortop Traumatol. 2020;64:258–264.