Given the boom in sports in school age, its intensity and the increase in sports in females, we are experiencing a boom in sports injuries characteristic of “adults” in growing patients, the anterior cruciate ligament being an injury with possible serious consequences.
MethodsTo show the surgical technique “without bone tunnels” by Micheli–Kocher in anterior cruciate ligament reconstruction in growing patients based on our results in 20 patients.
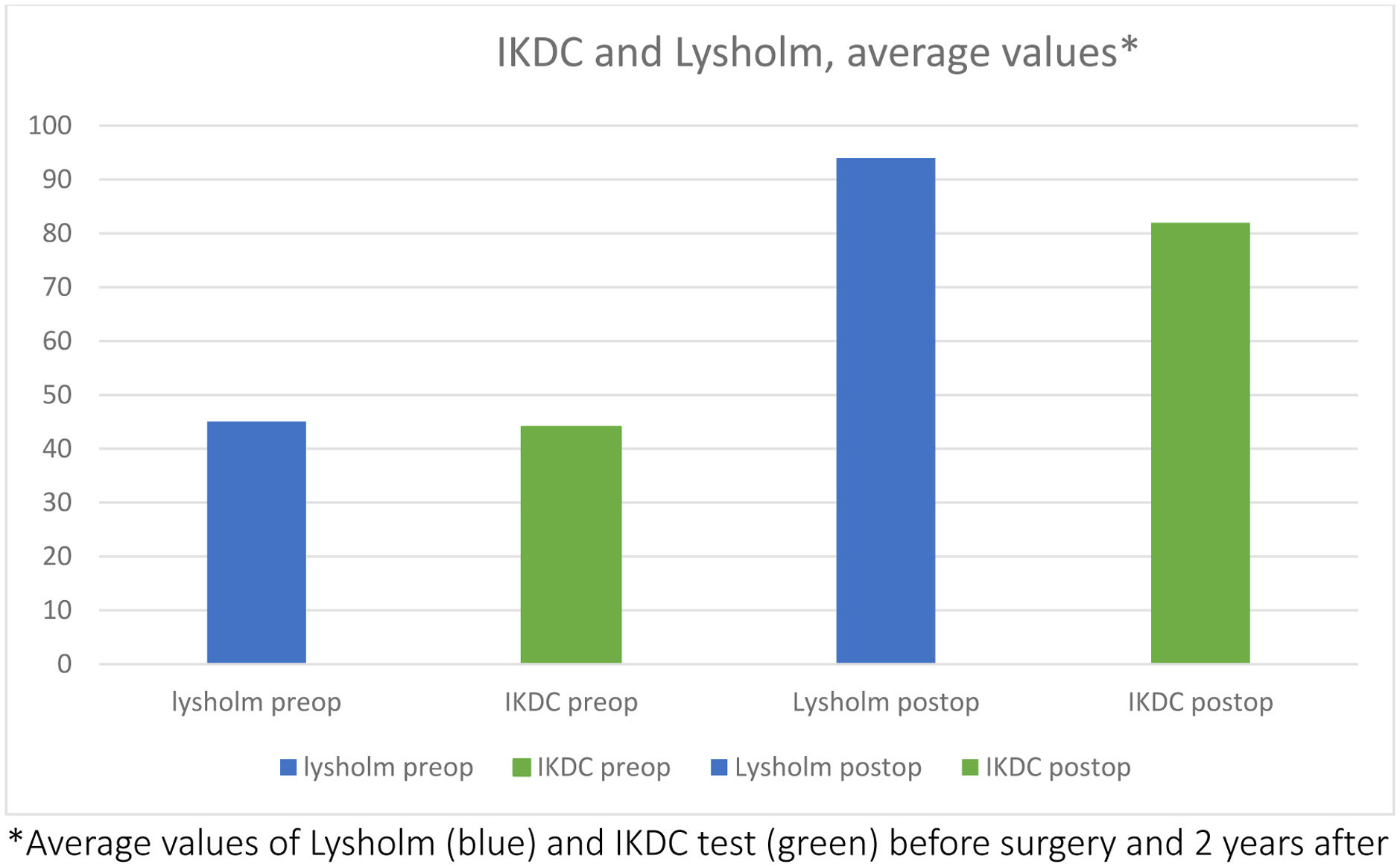
ResultsSince 2017 we have performed the technique “without bone tunnels” by Micheli–Kocher in 30 patients, 20 of whom have been followed up for more than 2 years. In our study, we have observed a return to previous sports activity in more than 90% of the patients, with only one patient undergoing reoperation due to a new rupture of the plasty. The results on the IKDC scales show an improvement in mean score from 42 points preoperatively to 84 postoperatively and on the Lysholm scale from 48 preoperatively to 94 postoperatively.
ConclusionsThe technique “without bone tunnels” by Micheli–Kocher is a technique indicated in patients under 12 years of age and Tanner stage 2 or less. It is a technique of moderate complexity with excellent results in recovery from previous sports activity and knee stability.
Dado el aumento de la práctica deportiva en edad escolar, y especialmente su intensidad y su auge en el sexo femenino, estamos viviendo un «boom» de las lesiones deportivas propias de «adultos» en pacientes en crecimiento, siendo el ligamento cruzado anterior una lesión con posibles consecuencias graves.
MétodosEstudiar nuestros resultados con la técnica quirúrgica «sin túneles óseos» de Micheli-Kocher en la reconstrucción del ligamento cruzado anterior en pacientes en crecimiento.
ResultadosDesde 2017 hemos realizado la técnica «sin túneles óseos» de Micheli-Kocher en 30 pacientes, 20 de los cuales han sido seguidos durante más de dos años. En nuestro estudio hemos observado un retorno a la actividad deportiva previa en más del 90% de los pacientes, siendo solo un paciente reintervenido por una nueva rotura de la plastia. Los resultados en las escalas IKDC muestran una mejora en la puntuación media de 42 puntos en el preoperatorio a 84 en el posoperatorio y en la escala de Lysholm de 48 en el preoperatorio a 94 en el posoperatorio.
ConclusionesLa técnica «sin túneles óseos» de Micheli-Kocher es una técnica indicada en pacientes menores de 12 años y estadio Tanner 2 o menor. Es una técnica de moderada complejidad con excelentes resultados en la recuperación de la actividad deportiva previa y la estabilidad de la rodilla.
In the last 30 years, children's sports activity has increased exponentially all over the world.1 There is a higher number of children practicing sports, and therefore an increase of training sessions and sports’ “super-specialization”, which implies that many children and adolescents engage in sport activities with a high physical demand, which is leading to a significant increase in the number of musculoskeletal injuries.2
Anterior cruciate ligament (ACL) injuries and tibial spine fractures have recently rised within the young population.3–5 ACL reconstructions in patients under 15 years of age have increased 425% between 1994 and 20066; this would explain the growing interest in clinical research on this topic, especially aimed at its prevention and treatment. Nevertheless, there are not many publications regarding these injuries in children.
In the past, this kind of injuries in patients with skeletal immaturity have been treated conservatively by modifying activity and articulated knee orthosis associated with rehabilitation treatment. This would give the child some time for skeletal maturity whilst avoiding the possibility of damage to the physis linked to classic surgical techniques. However, many studies indicate that – in patients with knee instability – the delay in surgical treatment increases the risk of associated chondral and meniscal injuries,7,8 thus worsening the functional prognosis of the knee, not only affecting the return to sports, but possibly its long-term function.
The physis of the knee plays an important role in the longitudinal growth of the lower extremity. The distal femoral physis contributes to 70% of the longitudinal growth of the femur (9mm/year), and the proximal tibial physis contributes to 60% of the growth of the tibia (6mm/year); therefore, and especially in pre-adolescent patients (Tanner stage 1–2, bone age <12 years in boys and <11 years in girls), is mandatory the use of surgical techniques that guarantee the bone tunnels will not affect the physis.
In 1976 MacIntosh9 described an extra-articular reconstruction technique using autologous iliotibial band for chronic ACL tears in adults, where the graft remains inserted in Gerdy's tubercle, passes deep to the lateral collateral ligament of the knee, and stitches back on itself. Subsequently, Micheli et al.10 described a modification of this technique for application in children and adolescents. The IT band is passed superficial to the lateral collateral ligament, and brought to an “over the top” position on the femur, through the intercondylar notch below the intermeniscal ligament, and then sutured to the periosteum of the proximal tibia and lateral femur. Although some have cited this technique as a non-anatomic reconstruction, biomechanical tests have shown complete recovery of native knee stability with low revision rates.11–14
The objective of our study is to evaluate the functional results, rate of return to sports and complications of skeletally immature patients intervened in our center following ACL rupture, employing the technique without bone tunnels described by Micheli–Kocher.
Material and methodsThis is a retrospective observational study, in which we have included all the patients operated in our center since 2016 following ACL rupture, employing techniques without bone tunnels. All the diagnosis were made by a combination of physical exam and knee MRI. All cases have been intervened by the same surgeon (J.J.L.M.).
Inclusion criteria- (1)
Tanner stage 1–2.
- (2)
Bone age of less than 12 years in boys and less than 11 years in girls (both actively practicing sports).
- (3)
Minimum postoperative follow-up of 2 years.
From 2015 to 2020, a total of 30 patients have been intervened in our center, but only 19 patients met the designated inclusion criteria; most being male patients,14 and only four female patients between ages from 7 to 12 years (mean age of 10 years).
All patients underwent preoperative IKDC and Lysholm tests, which were performed again 2 years after surgery, test was performed by the patients and their parents. All the information regarding the type of sports practiced and the pre- and postoperative sports level were registered. We also documented if there were associated intraoperative meniscal and/or chondral injuries (and the treatment performed), and the complications of the surgical treatment (infection, graft failure, arthrofibrosis, knee stiffness). All the child's parents approved the inclusion in this study and sign informed consent.
Patients were categorized and divided into several groups, as described by our co-author in another publication,15 according to the sport they practice more often:
- •
Group 1: Football.
- •
Group 2: Basketball, handball and volleyball.
- •
Group 3: Tennis, one-wall handball and padel.
- •
Group 4: Skiing and hockey.
Regarding the type of sport, most of the patients, 12 (63%) were situated in group 1 (football), followed by group 2 with 3 patients (16%), and groups 3 and 4 with two patients each.
Statistical analysis was performed using SPSS version 23.0 (IBM, New York, USA). The following variables were analyzed: age, associated meniscal injury, gender and time from injury to surgery. Chi-square test was performed for this analysis. The alpha level of statistical significance was established at p<0.05.
Surgical techniqueWe performed the anatomical reconstruction technique of the ACL without tunnels using an autologous iliotibial band, according to the technique described by Kocher et al.16 We will proceed to explain the technique in detail.
Patient is placed in supine position with ischemia cuff at the level of the proximal thigh and lateral supports (position of knee prosthesis). Initial exploratory arthroscopy is always performed to verify the ACL injury and recognize possible associated injuries at the meniscal, tibial spine or osteochondral level.
- 1.
Identification of bony prominences (Gerdy's tubercle and anterior tibial tuberosity) and femoral and tibial physis with fluoroscopy.
- 2.
6cm distal femoral lateral approach (Fig. 1A). Dissection of the iliotibial band with a width of 15mm and a length of 20cm, with subcutaneous dissection (Fig. 1B and C). The use of an open tenotome (Fig. 2A), Smillie meniscotome or mayo scissors, and a second incision of 1cm at the proximal level for its safe extraction is recommended. The graft is extracted through the lateral distal femoral incision, with dissection of the capsular area, leaving it anchored in Gerdy's tubercle (Fig. 2B).
- 3.
Preparation of the iliotibial band graft by means of high resistance suture with loop and Krakow-type stitches, leaving the graft moistened with gauze (Fig. 3).
- 4.
Arthroscopic debridement of intercondyle and dissection of the intermeniscal ligament. Introduction from the anteromedial arthroscopic portal of the Kocher forceps or large curved dissector, which is introduced through the intercondyle, passing the distal end through the posterior area of the lateral femoral condyle.
- 5.
Using the previously performed lateral approach, we begin the dissection of the posterolateral corner of the knee in the “over the top” area of the lateral femoral condyle (Fig. 4). Then, we locate the curved dissector that we have previously introduced with arthroscopic vision. Reaching this point, we are going to unite extra-articular surgery with intra-articular surgery.
- 6.
We perform the graft suture through the curved dissector previously introduced, passing the iliotibial band graft from extra to intra-articular, in an “over the top” position and emulating the native ACL, removing the iliotibial band suture through anteromedial portal.
- 7.
A 3cm incision in the area distal to the medial tibial physis is performed, with an H-shaped opening of the periosteum. Through it, subcutaneous dissection and introduction of dissection or Kocher clamp at the intra-articular level, below the intermeniscal ligament, which has been previously located by arthroscopy, monitoring this step by standard anterolateral view.
- 8.
Employing forceps, we recover the suture of the iliotibial band that we have in the anteromedial portal and it is extracted through the medial proximal tibial incision.
- 9.
The iliotibial band autograft is sutured to the intermuscular septum of the lateral femoral condyle with the knee flexed at 90° (Fig. 5).
- 10.
We then perform the tensioning of the iliotibial band and its fixation in the medial proximal tibia at 30° of flexion and external rotation of 30°. The author prefers fixation by bone harpoon but it can be done directly to the periosteum.
- 11.
Subcutaneous and cutaneous closure by means of intradermal suture of incisions and compression bandage.
- 12.
Articulated orthosis is recommended for 8 weeks with partial weight bearing and restricted mobility in 90° flexion and full extension. Protocol for strengthening, mobility and proprioceptive work similar to the usual techniques, with a return to competitive sports at 9 months.
Nineteen (89%) of the operated patients were able to return to sports. Most of them, 12 patients (63%) returned to the same sport with same pre-injury level; three of them returned to the same sport but at a lower level; four switched sports and finally two completely abandoned sports.
Regarding the time frame to return to sports, the average was 9.9 months with a narrow range (9–14 months). We did not find statistically significant differences between type of sport and return time (p 0.11).
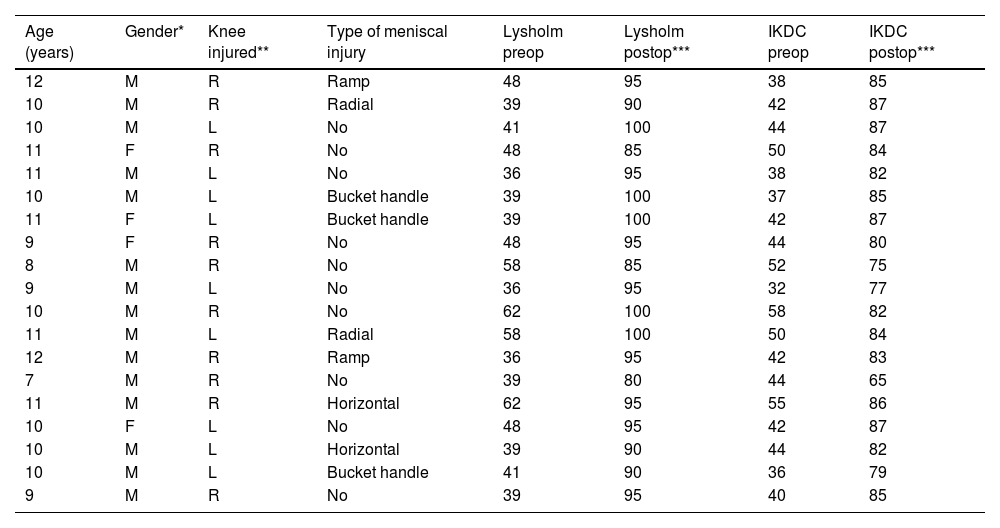
All patients were operated on following the surgical technique described. The interval, in days, between the injury and the surgical intervention was 83 days on average (25–245 days). Most of the cases required isolated ACL reconstruction (53%), the rest presented meniscal injuries that required suture. Practically half of our cases (47%) presented an associated meniscal injury (Table 1), the most common pattern being a bucket handle injury (3 of 9 cases). All of these injuries were repaired, the vast majority of cases using all-inside sutures. No case presented failure of the meniscal suture.
Patients demographic.
| Age (years) | Gender* | Knee injured** | Type of meniscal injury | Lysholm preop | Lysholm postop*** | IKDC preop | IKDC postop*** |
|---|---|---|---|---|---|---|---|
| 12 | M | R | Ramp | 48 | 95 | 38 | 85 |
| 10 | M | R | Radial | 39 | 90 | 42 | 87 |
| 10 | M | L | No | 41 | 100 | 44 | 87 |
| 11 | F | R | No | 48 | 85 | 50 | 84 |
| 11 | M | L | No | 36 | 95 | 38 | 82 |
| 10 | M | L | Bucket handle | 39 | 100 | 37 | 85 |
| 11 | F | L | Bucket handle | 39 | 100 | 42 | 87 |
| 9 | F | R | No | 48 | 95 | 44 | 80 |
| 8 | M | R | No | 58 | 85 | 52 | 75 |
| 9 | M | L | No | 36 | 95 | 32 | 77 |
| 10 | M | R | No | 62 | 100 | 58 | 82 |
| 11 | M | L | Radial | 58 | 100 | 50 | 84 |
| 12 | M | R | Ramp | 36 | 95 | 42 | 83 |
| 7 | M | R | No | 39 | 80 | 44 | 65 |
| 11 | M | R | Horizontal | 62 | 95 | 55 | 86 |
| 10 | F | L | No | 48 | 95 | 42 | 87 |
| 10 | M | L | Horizontal | 39 | 90 | 44 | 82 |
| 10 | M | L | Bucket handle | 41 | 90 | 36 | 79 |
| 9 | M | R | No | 39 | 95 | 40 | 85 |
The presence of associated meniscal injuries did not represent statistically significant differences with respect to functional results, calculated using the chi-square test (p 0.15 for Lysholm, p 0.66 for IKDC), nor in the return to sports.
Regarding functional scales, the patients had IKDC values between 36 and 62 (mean 44) and Lysholm between 36 and 62 (mean 45) before surgery. We then found a mean IKDC of 82 two years postop, and Lysholm average of 94 (Fig. 6). This difference between pre- and postoperative values is statistically significant (p<0.0164).
DiscussionOur study shows that, in expert hands, the ACL surgical reconstruction technique in patients with skeletal immaturity presents good functional results in the knee, with a high rate of return to sports with no complications in our series.
We evidenced a high rate of return to sports, specifically 17 of 19 patients (89%) returned to sports. This is a higher figure than the average of published studies that indicate a rate of return to sports in patients with open physes of 69–92%.17,18 However, these results should be carefully evaluated, since most children play different types of sports.19 Also, even the practice of a single sport in childhood has been linked to a higher incidence of injuries.
In our study we did not have any relevant post-surgical complication or ACL graft rupture. In the literature, it is generally accepted that re-rupture rates in patients with skeletal immaturity are higher than in adolescents and adults. Koch et al.20 reported 16.7% of graft failures (2/12 patients), and Cruz et al.21 in their studies of 107 patients indicated 10.7% of re-ruptures.
We should highlight that a major benefit of the technique “without bone tunnels” is that in case a re-rupture of the graft is presented and requires a new surgery, the patient's knee does not present any bone tunnel and has the possibility of taking any graft (hamstring, HTH or quadriceps) since the graft used is the iliotibial band.
It is accepted in the literature that the ACL graft failure rate is higher in children compared to adults. This happens for two reasons, the first is that isolated ACL reconstruction allows excellent stability of the knee in the sagittal plane, however does not provide as much rotational stability. The mentioned, together with the higher level of sports activity and physical demand in younger patients, could explain the rate of graft failures described in the literature.22
We can conclude that the time frame to return to sports should be indicated with great caution. Gokeler et al.22 determined that at 9 months postop, 75% of patients still present biomechanical deficiencies in the operated knee. Geffroy et al.23 reported 9% of graft failures, all of them happening after returning to contact sports within a year of surgery; therefore, this author recommends that patients with open physes should return to sports after 14 months postop.
In our study, the average time to return to sports is almost 10 months; perhaps this is one of the reasons that explains not having graft failures, the second being that our study handles a smaller number of cases.18
According to a recent meta-analysis,24 most studies on this subject – mainly IKDC (51% of studies), Lysholm (46%) and Tegner (37%) – use similar scales to those used in adults to measure knee function. They are the same scales that we have used in our study. We consider this a limitation and suggest that future studies should employ specific tests for children. In the literature25 we have only found three main ones: Pedi-IKDC, KOOS-Child, and ek HSS Pedi-FABS, which at the time of starting data collection for our study were still in the validation process and therefore were not used in our research.
ConclusionsThe “without bone tunnels” technique by Micheli–Kocher is indicated for patients under 12 years of age and in Tanner stage of 2 or less. It is a technique of moderate complexity with excellent results that provides knee stability and high rates of successful return to sports.
Level of evidenceLevel IV (case series).
Ethical approvalThis study was performed in line with the principles of the Declaration of Helsinki. This is an retrospective observational study, no ethical approval was required.
FundingThe authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Consent to participate and publishInformed consent was obtained from all individual participants included in the study, they accept his clinical information could be used for research. All patients agreed and sign voluntarily.
Conflict of interestOn behalf of all authors, the corresponding author states that there is no conflict of interest.
Availability of data and materialsYes, on electronic repository.