Correct alignment of the limb after knee replacement implantation has been a commonly pursued goal since the beginning of this procedure. The mechanical alignment aims to maintain the axis of the limb at 180º ± 3º, and for this it uses the standard instrumentation and the necessary tendon releases until achieving a symmetrical separation between femur and tibia and similar in flexion and extension. Kinematic alignment is based on the high frequency of the constitutional varus and to achieve this it is recommended to resect the damaged bone surface without altering the preoperative axis of the limb and without adding soft tissue release. There is no consensus on what type of alignment is best for the function and results of arthroplasty. It is recognized that kinematic alignment has its limitations, and it is possible that a hybrid technique such as the so-called functional alignment is the best option, but there is no uniform recommendation guideline in the literature.
Existe controversia en cuanto a la mejor técnica de alineación en las artroplastias de rodilla. La alineación mecánica persigue mantener el eje de la extremidad en 180º ± 3º, y para ello utiliza la instrumentación estándar y las liberaciones tendinosas necesarias hasta conseguir una separación simétrica entre fémur y tibia y similar en flexión y extensión. La alineación cinemática se basa en la elevada frecuencia del varo constitucional y para conseguirla se recomienda resecar la superficie ósea dañada sin alterar el eje preoperatorio de la extremidad y sin añadir liberación de partes blandas. No existe consenso sobre qué tipo de alineación es mejor para la función y resultados de la artroplastia. Se reconoce que la alineación cinemática tiene sus limitaciones; puede ser que una técnica hibrida como la denominada alineación funcional sea la más recomendable, pero no existe en la literatura una pauta uniforme de recomendación.
Nobody can doubt the excellent results which total knee arthroplasty (TKA) provides for patients requiring this procedure. Knee replacements are, in fact, considered to be one of the most common surgical interventions in reconstructive surgery. It is a technique regularly used by orthopaedic surgeons and is considered one of the healthcare procedures with the best cost-effective ratios.1 Survival of these implants is above 96% after 15 years and above 82%,2 after 25 years, which leads to the suggestion that if this occurs with arthroplasties designed 30 years ago and still using several obsolete materials, the survival of today’s models will be even higher.
However, this favourable survival is obscured by a high percentage of patients, around 20%, who continue having pain and other types of non-specific discomfort in the knee over the passage of time.3,4 A recent systematic review of the literature on this issue5 has shown that, although 71% of patients experience an improvement in symptoms after this procedure, only 22% of them classify the result as excellent. If we accept these data, then either the prosthetic models, or the surgeon’s manual or surgical techniques have not been able to reproduce the functioning of a normal knee. Despite the appearance of novel TKA designs, including new materials and biomechanical concepts, we have not been able to reduce this percentage of dissatisfied patients and it appears that neither the orthopaedic industry nor improvements in surgical technique are able to resolve this conundrum.6–9
Numerous studies are to be found in the literature which have attempted to relate this defective evolution to different variables. It has been considered that this is due to the high expectations patients attribute to this procedure, together with their increasingly younger age and the lack of preoperative information with which patients normally confront a TKA.10 However, regardless of this being possible in some circumstances, it is common in the professional practice that, having implanted an accredited TKA model with a perfect technique and with optimum radiographic postoperative findings, patients refer to uncomfortable discomfort and perceptions, of greater or lesser intensity, which force them to state that the patients say “this is not my knee”. This sensation, which is not comparable to the evolution of other implants such as hip arthroplasty, has no relationship with the surgeon’s experience or postoperative guidelines or the patient’s socio-economic level. It may be due to the actual geometry and function, to incomplete reconstruction of the ligaments or to differences between the medial and lateral side of this joint. These differences are not correctly captured in arthroplasty designs.
Certain factors directly contingent upon the surgeon, such as residual instability, poor alignment or impaired ligament balance have been held responsible for unsuitable outcomes.11 And this may be so as it is known that 50% of early TKA failures are precisely due to these defects of surgical technique.12
When searching for solutions to improve this outcome, it has been suggested that new technologies to assist the implant (from navigation to robotics), in order to better assess ligament balance (measuring and correcting the gap between femur and tibia), defining new kinematic requisites and new concepts have appeared on the correct alignment of the knee after TKA. However, to obtain a good alignment an essential requirement is to know and validate the surgical technique. This Subject for Update begins by examining some of the aspects of the surgical technique directly related with alignment, and then centres on the different systems of alignment which have been described, with particular dedication to the recently published literature.
Obtaining an effective and symmetrical joint spaceThe aim of a TKA is to achieve a well aligned and balanced knee with symmetrical ligaments structures which provide stability in the neoarticulation. However, this is not easy. It should be remembered that the knee is a relatively unstable joint which has stabilising structures that provide stability. In a normal knee the medial knee compartment is stable in flexion and in extension, the lateral compartment allows a latitude in extension, somewhat greater in flexion (3−4 mm) when compared with the medial and the femoral-tibial gap is not symmetrical either but is greater in flexion than in extension (2−3 mm). Understandably, these characteristics are difficult to reproduce in a TKA implant.
The concept of the so-called balanced knee is not clearly defined and it is manually difficult to achieve.13 This knee balance may be obtained by following 4 techniques: measured resection, gap balancing between femur and tibia, measurement of intracompartimentral pressure with new specific systems14,15 and the conventional system.16 In turn, gap measurement may be performed with the use of blocks, articulated spacers, tension systems of greater or lesser sophistication or tester components.
Given that correct positioning of the femoral component of the TKA with regards to its rotation is difficult to achieve, different surgical techniques have been devised to pursue the correct positioning of this component. This firstly enables correct patellar sliding, together with ligament stability and lastly, similar gaps in flexion and extension. The bone references used and which lead to the use of conventional instrumentation are not uniform and several are difficult to record intraoperatively. In fact, in one recent systematic review of the literature it was impossible to determine what the best references were to determine this femoral rotation.17
This difficulty and the importance of achieving a precise rotational alignment, has led to 2 alternative technique being used in the implant of a TKA18: the technique of the measured resection (MR) and the so-called tensioned gap (TG) or gap balancing technique.19
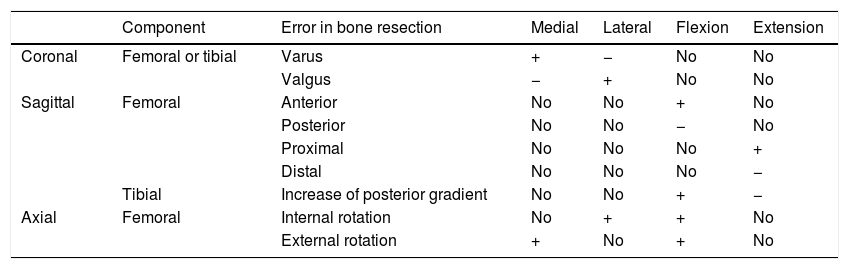
In MR anatomical references are used to position the implant. Bone cutting is performed regardless of the ligament situation and is based on the trans-epicondylar axis, the anteroposterior axis of the femur or the Whiteside axis and the posterior axis of the condyles (Fig. 1). The surgeon follows the instrumental guides, trying to make the distal and posterior femoral bone resections similar; the ligaments adapt after release of the soft tissues.20 The implant should have the same thickness as the bone resections made. If the incisions are incorrectly performed or the ligament releases are erroneous then the femoral-tibia gap will be compromised in both flexion and extension (Table 1).
Modification of joint space considering the errors committed in bone resection in a TKA.
| Component | Error in bone resection | Medial | Lateral | Flexion | Extension | |
|---|---|---|---|---|---|---|
| Coronal | Femoral or tibial | Varus | + | − | No | No |
| Valgus | − | + | No | No | ||
| Sagittal | Femoral | Anterior | No | No | + | No |
| Posterior | No | No | − | No | ||
| Proximal | No | No | No | + | ||
| Distal | No | No | No | − | ||
| Tibial | Increase of posterior gradient | No | No | + | − | |
| Axial | Femoral | Internal rotation | No | + | + | No |
| External rotation | + | No | + | No |
TKA: Total knee arthroplasty.
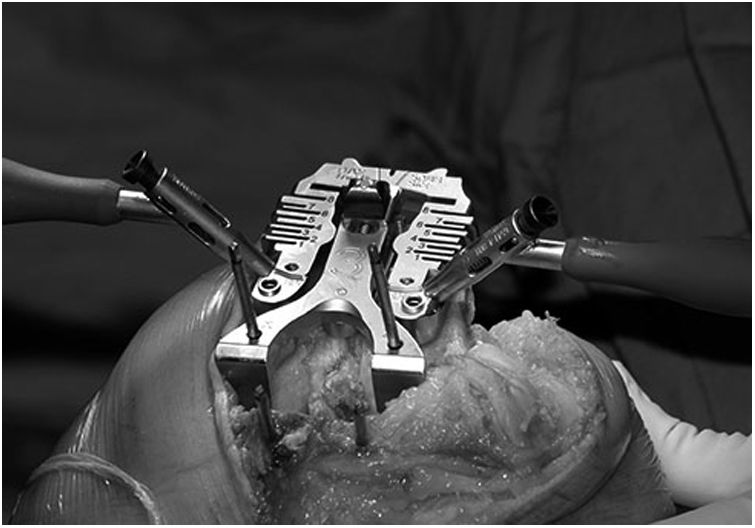
In TG, distraction systems are used to define the best position of the arthroplasty and bone cuts and ligament releases are then adapted to this (Fig. 2). The femoral component is positioned parallel to the tibial resection incision and each collateral ligament is tensed to achieve a symmetrical rectangle in flexion to 90° and in the complete extension of the knee. Depending on the technique preference of the surgeon, gap measurement and ligament releases may be initiated in flexion or extension, but always from resection of the proximal tibia. A critical moment in TG is when the tibial osteotomay is performed; a resection in varus would lead to an increase in the internal rotate of the femoral component and a resection in valgus would increase its external rotation. The integrity of the lateral ligaments is equally necessary.
Both techniques have their supporters and critics.21,22 Whilst MR may be safe in the majority of cases, the exclusive use of this technique may give rise to an asymmetry of the gaps already referred to, which causes instability and poor clinical outcome. The fact that the TG is less dependent on the bone anatomy has enhanced its recent recommendation.23,24
No differences have been found in the outcomes of either technique, at least in the short term.25,26 Two meta-analyses which analysed 8 articles in the first and 25 in the second revealed no differences.27,28 Each surgeon should regularly adopt the technique they find the easiest and most comfortable, although they should be aware that in some situations their practice should be modified and knowledge of both is therefore imperative. It would be correct to use both, in what has lately been called the individualised technique.29
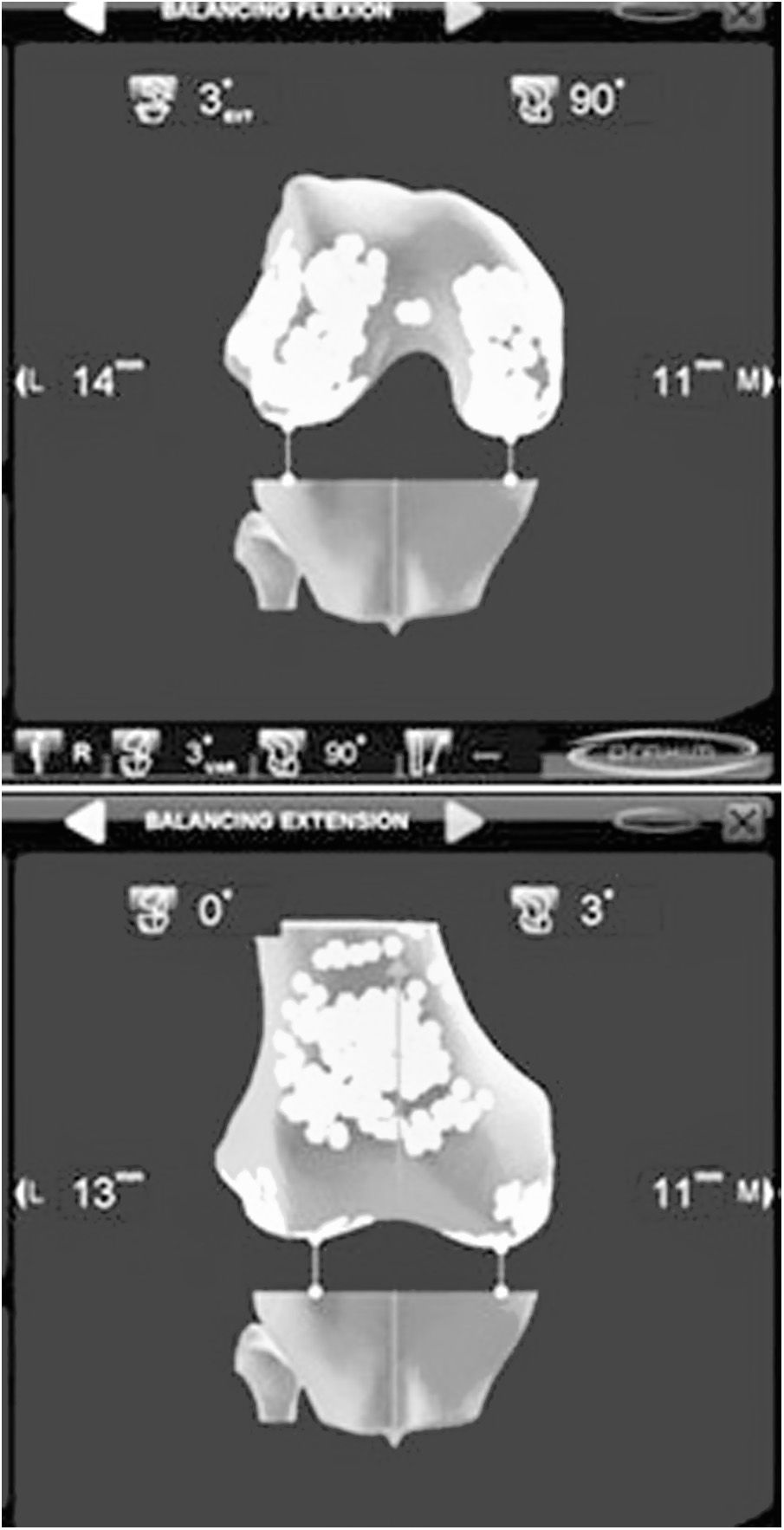
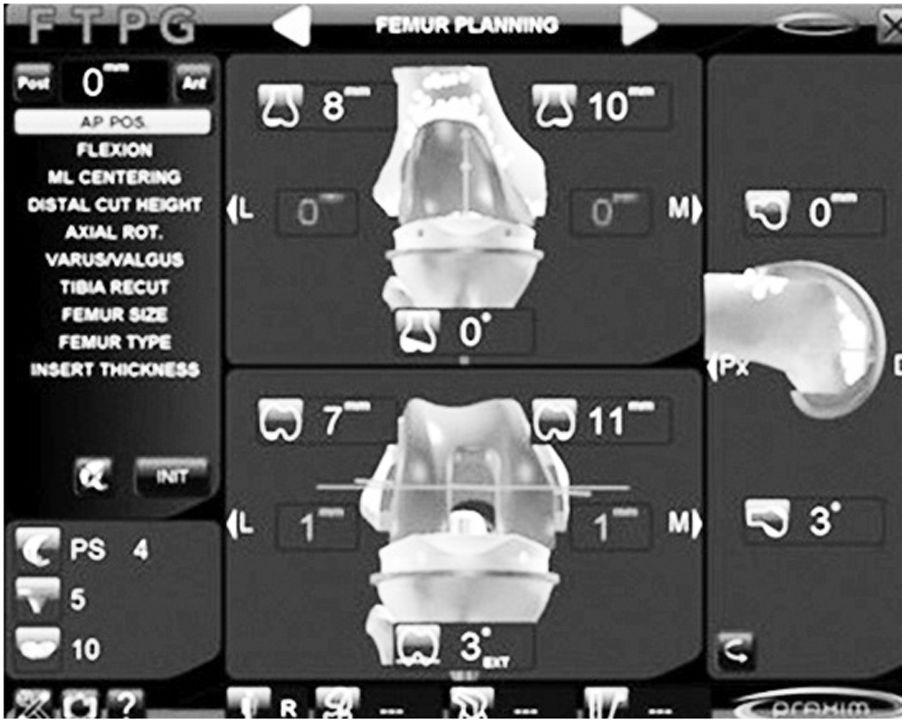
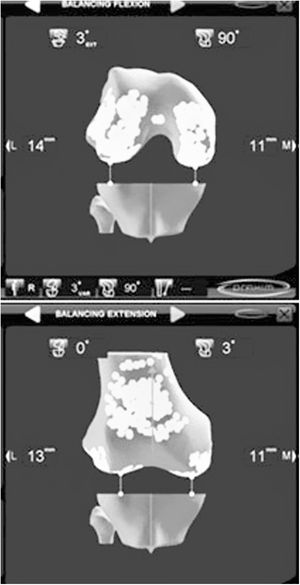
Computerised navigation in both MR and TG, has demonstrated its efficacy. Either as a learning technique, for surgical simulation or as instrumentation in the surgical technique, computerized navigation has become fully established in the TKA implant arsenal. Computerised navigation was initiated during the first years of this century as an aid for the correct resections of bones. Its usefulness in knowing the mechanical axis of the limb before and after TKA implant was the reason behind it first being used and it effectively reduced the outliers.30 With the passing of time computerised navigation has proven its true worth in the indication and evaluation of the ligament situation of the knee, to achieve a correct gap in flexion and extension and to confirm the kinematic situation of the TKA throughout the mobility arc. On offering a dynamic vision of the knee, it can orientate and then assess the technique, which could only have been done statically before, during the postoperative period. Despite the fact that in the mid to long term it has not been possible to demonstrate a clear improvement of clinical outcomes, all authors acknowledge that computerized navigation improves the position of the implants, especially in the event of previous anatomical changes and angular or rotational deformities.31,32 The outcomes of the TKA implanted with modern navigation systems is yet to be assessed in those where the treatment of soft tissues is of the utmost interest (Fig. 3). The advantages of being an individualized technique33 means that the arthroplasty may be personalised,—this specific prosthesis in this specific patient—, with confirmation of the behaviour of the ligaments throughout the whole arc of movement of the knee34–37 and confirmation of bone resections correction (Fig. 4). With the appearance of this technique and its successive optimisations, an extensive field of investigation has been initiated into the kinematics of the knee joint which may have a profound change on our future knowledge.38,39
It has been considered that the start of the current knee arthroplasty implant technique began in the 1970’s. It has to be accepted that up until then knee prosthesis implant was pure craftsmanship. The materials and designs were rudimentary and results unsatisfactory. However, even then, great attention was given to the alignment of the implant on the resected bone structures and the resulting limb alignment so that it may be said that the history of TKA ha largely resulted from the steps in instrumental design which aimed at accurate alignment.
In those years Freeman et al.40 developed a TKA model which prioritised implant stability over anatomical function. The cross-over ligaments were resected and it could be said that it was the first TKA model with proper instrumentation, although obviously deficient. These authors had already recommended making bone cuts at 90° in coronal plane, but the absence of appropriate instrumentation almost never achieved this. Their first cases, of 69 TKA implanted between 1970 and 1972, had acceptable results, but the absence of a good alignment and the quality of the materials led to failure in the short term.
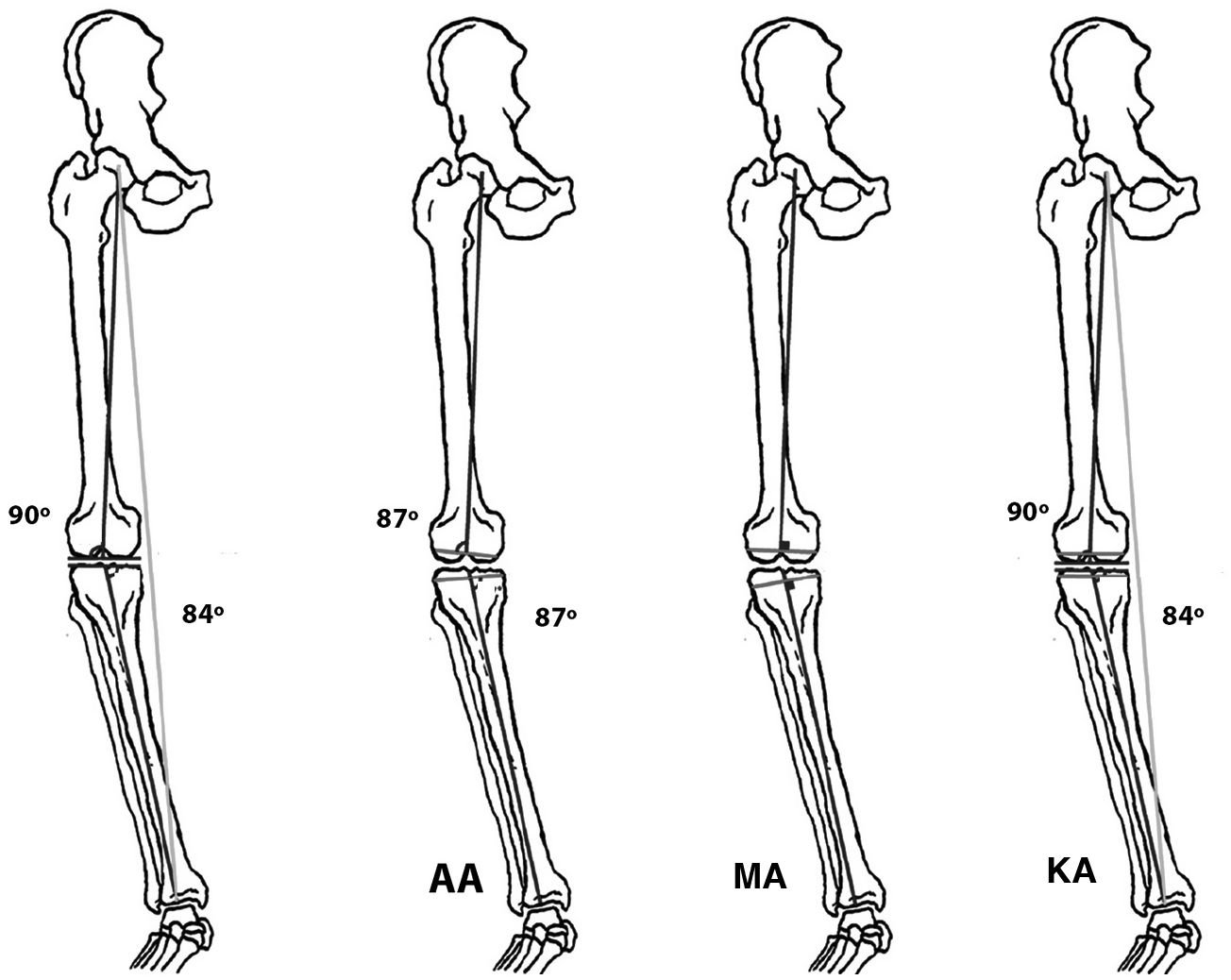
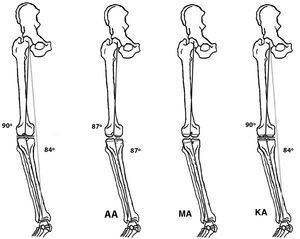
During the 1880’s Hungerford and Krackow41 developed new models of arthroplasties and introduced the concept of anatomical alignment (AA); their aim was to recreate the joint line. This alignment followed the anatomical axis of the femur and the tibia, with the recommendation to practice an oblique osteotomy with 3° of femoral valgus and 3° of tibial varus.16,42
Insall et al.43 were the first surgeons to assess the mechanical axis of the limb for the TKA implant, with their main objective being to achieve parallel and similar spaces in flexion and extension of the knee.44 They therefore aimed at a hip-knee-ankle angle of 180 ± 3° with 3° of external rotation of the femoral component. This symmetry of the loads avoided asymmetrical wear and tear of the polyethylene platform, a complication which was common and catastrophic in those days.45 The concept of the femoral head centre as reference46 and the design of the instruments which profiled the mechanical axis47 intraoperatively were undoubtedly the key to better outcomes.
Nowadays it is known that the coronal axis of the knee should maintain a valgus angulation between 3° and 7.5°. The femoral component of the TKA should be situated between 2° and 8° in coronal plane (some authors admit up to 12°48) and between 0° and 3° in the sagittal plane; in the tibia the coronal axis is positioned at 90° and the sagittal between 0° and7.° For its part the femoral and tibial component rotation should range between 2° and 5° of external rotation.49 Based on these data all available instrumentations enable bone cuts within these parameters.
The mechanical axis has been considered the gold standard for decades and includes the axis of the complete limb from hip to ankle. It calculates simultaneously the mechanical axis of the femur forming a straight line which goes from the centre of the head of the femur and finishes in the centre of the intercondyle region and the mechanic axis of the tibia from the tibial plateau to the centre of the ankle. The joint interline is therefore kept perpendicular to the mechanical axis and parallel to the floor.
In a mechanical neutral limb the mechanical axes of the femur and the tibia form an angle of 180° as previously stated, but this axis is only neutral in a very small percentage of the population. This is why it comes into question, as we shall see later. To know this so-called mechanical alignment (MA) computerised tomography or radiography should be performed on the whole limb, including hip, knee and ankle.50 The extensive references published on TKA outcomes based on short X-rays is striking, as this suggests that neither the mechanical position of the components nor the final axis of the limb were analysed.51,52 The most that can be expected from a short X-ray which only includes the knee would be to suspect the previously defined AA. However, the anatomical axis does not predict the mechanical axis, and is therefore a useless measurement for checking the coronal or sagittal alignment of the implant.53,54 Short X-rays can only be accepted as periodic control but never for studies on TKA alignment.55,56
Conventional instrumentation for TKA implants perform the femoral cut in coronal projection with a predetermined valgus angulation related to the anatomical axis. However, no major differences were found between the anatomical axis and the femoral mechanical axis which oscillate, as previous described, between 2° and 12.5°.57 This means that the standard technique adapts the patient to the instrumentation and not the instrumentation to the patient, which would be recommendable. With no knowledge of the real and individual mechanical axis the decision regarding this angulation is subjectively that of the surgeon. Only some techniques such as the robotic and computerised navigation would enable osteotomies to be performed with exact angulations since in these techniques the mechanical axis is known through references at the centre of femoral head rotation, at the centre of the knee and at the centre of the ankle.58 Furthermore, standard instrumentation, especially when extramedullary guides are used, have their limitations and may lead to crude mistakes.59,60 However, nobody doubts that with a standard technique an accurate rectangular gap may be achieved in flexion and in extension through the orthogonal osseous resection which the said instruments provide.
But the MA obtained with conventional instrumentation also has other disadvantages. This type of alignment is exclusively static, while resting, so we do not know what this means kinematically. Also, we now assume that uniform tension is required from the soft tissues around the knee both in flexion and in extension. This is the concept of “soft tissue balancing”. It is important to know that positioning of the TKA components affects the tensions in the soft tissues and that this is even more important for achieving a perfect MA. This concept has its origin in the so-called Gap Balancing (GB) technique already defined in this Update, where after performing femoral resection the lateral and medial soft tissues are released until a uniform separation is achieved between femur and tibia in both flexion and extension.
Transcendence of neutral alignment. Constitutional varusAs previously mentioned, implant misalignment, is a known cause of TKA failure which leads to further revision surgery or at least poor clinical functional outcomes.61,62
So that the TKA implantation may be considered technically correct, the alignment of the limb should be achieved in 6 dimensions.63 The first 3 are defined statically in coronal, sagittal and axial plane. The fourth dimension refers to the proximal-distal positioning of the implant. Also, these dimensions have to reflect the appropriate kinematics, both with weight-bearing and without, and lastly all construction must be stable over time, which is expressed as longevity.
The good alignment of each prosthetic component in 3 planes—coronal, sagittal and axial—was up until some years ago a globally accepted requirement. It was considered that static alignment, following the mechanical axis, was paramount. This concept, as we shall see, has recently been under debate and doubts regarding its true relevance have been raised.64
Although 10 years ago studies appeared which aimed at reducing the direct relationship between defective alignment and aseptic failures65 it was the study by Parratte et al. in 201066 which in a surprising way showed that obtaining a neutral postoperative mechanical axis, i.e. ±3°, was not linked to greater implant survival. These authors reviewed the outcomes of 400 cemented TKA implanted over 15 years ago. They compared 292 with an accurate mechanical axis to 106 which presented with errors in the same. From the first group they had surgically reviewed 15.4% and from the second 13%. According to these authors their results would not indicate that achieving accurate alignment was trivial but that also other factors played a part in the failure of TKA and these could be even more important. Following this premonitory study, different authors67–69 have repeated the same outcomes in contrast to others49,70 which continue insisting in neutral alignment being essential. This controversy still remains today, although it is necessary to highlight several facts. Firstly it would be clarified that in the studies where good TKA outcomes are shown with defects of alignment, this misalignment is highly limited, of only a few degrees and that, in sum, the actual authors conclude that it is not only the defects of alignment that are responsible for the failures of these implants, which is true and mostly accepted.71,72 It is known that several factors, such as exaggerated postoperative alignment in varus,73–75 a high body mass index76 or excessive preoperative deformity77,78 are responsible factors for a lower TKA survival. Something similar occurs with the rotation of the femoral component; minor variations do not change medical outcomes79,80 which is what invariably happens when there is an exaggerated malposition of this component.81
Historically, as previously stated, the coronal mechanical axis was considered necessary to be in 0 ± 3° and TKA results have been published with this condition and even considering this alignment as a predictive value of outcomes.82 However, the “native” axis of the knee is almost never this. For some groups the so-called “constitutional varus” must be reproduced after implant of a TKA and this does not appear to lead to poorer outcomes.3
In the native knee, the surface of the tibia has approximately 3° varus (from 1° to 5°) and the femur 3° of valgus (from 0° to 4°) unlike the ideal mechanical axis, accepting an oblique intertline when standing which in turn becomes a parallel line when walking and balancing the limb on the support of one leg.
The so-called “constitutional varus” is very common as a trigger of osteoarthritis of the knee and in fact a major proportion of the population (over 30% of men and 17% of women) have a constitutional varus above 3°. For some authors this suggests maintaining this varus after TKA and not pursuing a neutral mechanical axis at all costs.83 In these cases to achieve an accurate MA different surgical manoeuvres and releases of soft tissue are required. It is true that recovery up to a neutral alignment cannot be considered “natural” and may in fact lead to high ligament tension.29
Following these events, it must be acknowledged that what was considered an accepted truth regarding the imperative need to achieve neutral MA has been changed. Some authors84 even found better functional results when a residual varus was maintained in implanted TKA in patients with varus osteoarthritis, although correct patient selection had to always be respected, as we shall later analyse.85
One survey comprising 300 surgeons from 32 countries some years ago86 revealed that the majority were inclined towards natural alignment, although they recognised that a slight varus was acceptable in patients with a constitutional varus. For all surveys the aim of this procedure was to achieve a joint interline parallel with the floor and a weight-bearing line which crossed over the centre of the arthroplasty.
Kinematic alignment as a copy of mechanical alignmentThese concepts largely belong to those who defend kinematic alignment (KA), also called constitutional alignment, which has introduced controversies in a chapter which was considered closed: the desired natural alignment of the implant.
KA was first recommended by Howell et al. in 200687 and aims to reconstruct the limb axis prior to the TKA implant, defined as the “pre arthritic” axis. These authors and later advocates of this type of alignment consider that the reconstruction of the limb axis must follow the native axis, which in many cases is different from the neutral axis pursued by the MA. By doing this soft tissue releases would be avoided as no disequilibrium would be created and no asymmetry of the femoral-tibial gap. This is achieved by undertaking symmetrical resections of the femoral condyles and of the medial and lateral tibial plateaus, with the actual wear and tear from the osetoarthrosis being repaired. To perform this alignment computerized navigation may be used with individualized templates or with manual instrumentations helped by calibrators to execute and measure the bone resection. The greatest complication related to this technique is precisely that, that the tibial and femoral cuts are not accurately performed.
The aim, which is in common with other types of alignment, would be to achieve less pain and better functioning of the new joint. Its defenders insist that this techique attempts to restore the 3 axes of the knee: the trans-epicondylar axis, through which the tibia is flexioned on the femur located in the centre of a circle on the femoral condyles; the transverse axis of the femur on which the patella slides in flexion and the extension of the knee and the longitudinal axis of the tibia with which the tibia rotates internally and externally on the femur.42
The 3 principles of the KA are therefore to restore the joint surfaces of the femur and the tibia, restore the native alignment of the knee and restore the original mobility of this joint.29 KA seeks to position the implant by recreating the previous anatomy of the knee and thus avoid releases of the soft tissues and improve the ligament balance due to the fact that the implant location would be closer to the individual anatomy of the patient. To sum up, whilst in the MA the knee adapts to the TKA, in the KA the TKA adapts to the previous situation of the knee (Fig. 5). KA could be likened to surface replacement hip arthroplasty, where the surgeon only removes the surface of the joint structure and instead implants the prosthesis, restoring the pre-arthritic alignment of the knee, without corrections in the bone plane.45 In keeping with these concepts new arthroplasty models were designed and a anon-going commercial dispute has arisen which encourages possible biases in results. Also, KA benefits from better and more long-lasting materials such as the new polyethylenes; complications of this type derived from poor mechanical alignment are not such a determining feature as they were some years ago.88
KA indications are not perfectly defined; not all patients have a neutral alignment in the native knee, and not all patients have a constitutional varus.89 The ideal indication would be patients where the tibial and femoral cuts may be made whilst remaining within ±5° of the mechanical axis and the hip-knee-ankle axis within ±3°. These conditions are called the “safe zone”. It is precisely due to the fact the KA advocates recognise that it is not useful in all cases, that the term restricted kinematic alignment (rKA) was coined.
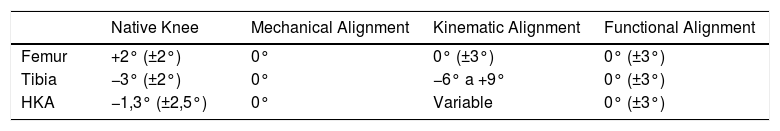
Even more recently functional alignment (FA) has been described16 which, similarly to rKA, uses intraoperative imaging with computerised navigation to make the implant adapt in flexion and extension and equalise the joint gap (Table 2). For Oussedik et al.,90 the MA ignores the soft tissues and concentrates only on obtaining a parallel interline to the floor, whilst the KA forgets about the mechanical environment. The FA is defined as the hybrid technique between both, which is based on the kinematic view of the knee using navigation. Manually the knee is strengthened in varus or valgus to correct the deformity. This means that the navigation system finds the size of the potential gaps, both in extension and in flexion. It firstly confirms the thickness of the resection and the width of the joint spaces. Once the osteyphytes have been resected the limb alignment is assessed intraoperatively, enabling a correction in the coronal plane under computer navigated vision. Both static alignment in extension and the dynamics throughout the length of the whole arc of movement are assessed.
Recommended angle in the different types of alignment (permitted interval between brackets).
| Native Knee | Mechanical Alignment | Kinematic Alignment | Functional Alignment | |
|---|---|---|---|---|
| Femur | +2° (±2°) | 0° | 0° (±3°) | 0° (±3°) |
| Tibia | −3° (±2°) | 0° | −6° a +9° | 0° (±3°) |
| HKA | −1,3° (±2,5°) | 0° | Variable | 0° (±3°) |
HKA: Hip-knee angle.
There is currently profound controversy in the literature between the defenders of MA and KA. For the former, the patient’s anatomy must be adapted to the arthroplasty implants and for the latter the positioning of the implants must be adapted to the individual knee anatomy. When extreme anatomic situations exist this is not possible, in which case kinematic alignment has its limitations, as previously described.
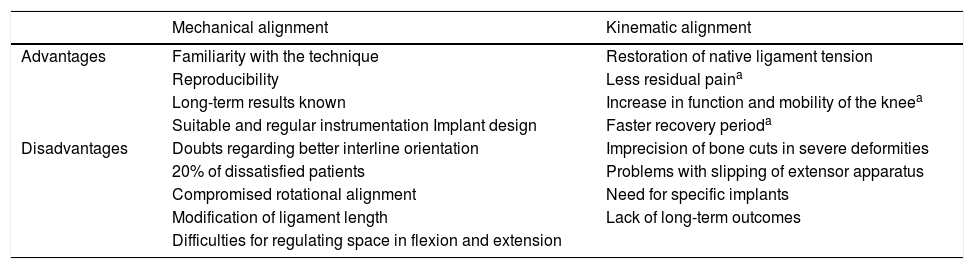
Advantages of KA referred to in the literature are less bone resection and less need for tendon releases.91 In contrast, detractors of KA fault the asymmetry of the weight bearing when walking, the need to use specific instrumentation with navigation or individual incision templates to obtain correct alignment, difficulties in patellar sliding and the impossible restoration of alignment when there are major varus-valgus deformities.92 (Table 3).
Advantages and disadvantages of mechanical and kinematic alignment.
| Mechanical alignment | Kinematic alignment | |
|---|---|---|
| Advantages | Familiarity with the technique | Restoration of native ligament tension |
| Reproducibility | Less residual paina | |
| Long-term results known | Increase in function and mobility of the kneea | |
| Suitable and regular instrumentation Implant design | Faster recovery perioda | |
| Disadvantages | Doubts regarding better interline orientation | Imprecision of bone cuts in severe deformities |
| 20% of dissatisfied patients | Problems with slipping of extensor apparatus | |
| Compromised rotational alignment | Need for specific implants | |
| Modification of ligament length | Lack of long-term outcomes | |
| Difficulties for regulating space in flexion and extension |
Source: modified Mercury et al.22
The latter difficulty as already been the cause of the already referred to RKA.93 In some patient’s recreation of the native knee may have negative consequences for the mechanics and wear of the TKA components. A safe range is proposed in these cases, as already stated.94
Many reports have been published comparing MA and KA both regarding knee function and clinical evolution and the failure of both. The first study was published by Nogler et al.,95 in 2012 with cadavers. Later TKA studies attributed KA with better gait,96–98 although others did not find there to be any major differences between KA and MA.99–104 For its part, RKA showed better results than MA, but with a one-year follow-up.105
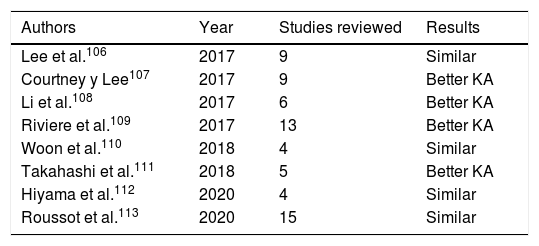
In an attempt to clarify this discrepancy in the literature, during recent years several meta-analyses and systematic reviews have been published comparing MA and KA (Table 4). In 2017, Lee et al.106 published a systematic review comparing both types of alignment. They analysed 9 studies with clinical and radiographic results of patients with KA and MA. With a 2-year follow-up the KA offered better or equal results to the MA. Another systematic review also from that year showed better results for KA.107 Li et al.,108 published a meta-analysis that same year which included 6 articles with 561 patients and with a follow-up of between 6 and 34 months. The functional results and the flexion of the knee were higher with KA, but only with consideration of short-term follow-ups. Also, in 2017 Riviere et al.109 published a systematic review on 13 studies with the same results and a similar follow-up time. A meta-analysis of Woon et al., in 2018110 assessed 4 articles, with no differences being appreciated in the two alignment systems, but also in the short term. In the study by Takahashi et al.,111 better results were revealed for KA, whilst for Hiyama et al.112 in a more recent review the results were similar. Another systematic review which had already analysed 15 articles published between 2012 and 2020113 they concluded that, after analysis of the literature, the KA had equivalent results to the MA without an increase in the failures, considering this as “convincing evidence”.
Systematic reviews and meta-analysis comparing outcomes between MA and KA.
| Authors | Year | Studies reviewed | Results |
|---|---|---|---|
| Lee et al.106 | 2017 | 9 | Similar |
| Courtney y Lee107 | 2017 | 9 | Better KA |
| Li et al.108 | 2017 | 6 | Better KA |
| Riviere et al.109 | 2017 | 13 | Better KA |
| Woon et al.110 | 2018 | 4 | Similar |
| Takahashi et al.111 | 2018 | 5 | Better KA |
| Hiyama et al.112 | 2020 | 4 | Similar |
| Roussot et al.113 | 2020 | 15 | Similar |
KA: Kinematic alignment; MA: Mechanical alignment.
Whilst attempting to summarise the literature by comparing both types of alignment it may be said that in the short term MA and KA clinical outcomes are similar, and they even show there is a positive difference for KA. Certainly the fact that commercial interests govern some studies undermines their results and long-term assessment for this type of alignment is lacking. It is suspicious that the meta-analyses have largely been performed by the KA advocates. Whilst for MA the known results have a long-term follow-up and were designed by authors from different origins, for KA follow-up is short and it is not known how a larger follow-up will impact results.114 It is possible that the provision of new technologies115 may be able to clarity what the best system of alignment is. Meanwhile, achieving a neutral alignment should be the aim for TKA implants.
ConclusionsOn consideration of the knowledge we currently possess, we cannot recommend the rigorous use of one type of alignment or another. The achievement of the mechanical axis has over the years been shown to be an aim of TKA instrumentation. The results achieved long term with this technique are known and have positioned TKA as a successful procedure. Achieving a balance of symmetrical loads has prevented the wear of the components and their collapse. Whilst attempting to reduce the percentage of patients who are not completely satisfied after TKA, and considering the frequency of constitutional varus, other alignments systems have been created in recent years. The KA pursues the positioning of arthroplasty without modifying the preoperative axis of the limb as superficialisation, without intervening on the ligaments. Comparison of results between both alignment methods cannot be seriously performed because of the difference in follow-up periods of the case studies. Recently described functional alignment is a hybrid technique between MA and KA. It is possible that functional alignment is key to obtaining better results, but literature is scarce and requires the support from techniques which ensure the correction of the bone resections. We cannot state that the implant of a TKA has stopped being a bone technique to become a soft tissue procedure, but at least it should be recognised that ligament releases are as essential as bone resections. A surgeon may know and correctly carry out both bone resections and soft tissue releases to achieve a stable and kinematically adjusted knee.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Hernández-Vaquero D. La alineación de la artroplastia de rodilla. Antiguos mitos y nuevas controversias. Rev Esp Cir Ortop Traumatol. 2021;65:386–397.