Tibiotalocalcaneal arthrodesis is an effective salvage procedure in cases of combined ankle and subtalar osteoarthritis as well as severe multiplanar deformities and severe joint destruction of the hindfoot. Special mention should be made of this procedure in cases of bone loss, especially from the talus, secondary to failed previous surgeries or bone infection, often being the only way to achieve a stable and painless foot and ankle. We present a case of ankle fracture in a patient with associated morbidity and multiple complications following osteosynthesis, in which tibiotalocalcaneal arthrodesis with cemented with antibiotic coated retrograde nail has achieved a satisfactory final result.
La artrodesis tibiotalocalcánea es un procedimiento de rescate efectivo en casos de artrosis combinada de tobillo y subastragalina así como en deformidades severas multiplanares y graves destrucciones articulares del retropié. Mención especial merece la indicación de este procedimiento en casos de pérdida ósea, especialmente astragalina, secundaria a cirugías previas fallidas o como secuela de infección ósea, constituyendo muchas veces la única forma de conseguir un pie plantígrado y un tobillo estable e indoloro. Presentamos un caso de fractura de tobillo en paciente con morbilidad asociada y múltiples complicaciones tras la osteosíntesis, en el que la artrodesis tibiotalocalcánea con clavo retrógrado cementado con antibiótico ha conseguido un resultado final satisfactorio.
Ankle fractures account for approximately 10–15% of total fractures, lower limb fractures being the most common.1,2 They are also the fractures most frequently treated with surgery as a result of the uniformly favourable outcomes obtained. Notwithstanding, stable fractures, or unstable fractures in patients with major comorbidities, may also be treated conservatively.3,4 With regard to complications, Spanish authors have reported that percentages range between 5% and 40% depending on the population group researched,5 and several risk factors have been identified including diabetes mellitus, peripheral neuropathy, peripheral vascular failure, a tobacco habit, alcohol abuse and the use of immunosuppresors.6–8 The most feared complications from surgery is deep infection, due to both the added morbidity and the high rise in material resource consumption with increase in costs.7
We present the case of a diabetic, kidney-diseased patient with a surgical infection secondary to open ankle fracture surgery, who was satisfactorily treated for fusion with a cemented coated retrograde ankle nail with antibiotics.
Clinical caseA female patient aged 67, diabetic with peripheral polyneuropathy and nephropathy (chronic kidney failure and in dialysis) who was admitted to our centre after suffering from an accidental fall resulting in a grade I open bimalleolar luxation fracture of the left ankle (1cm wound on medial side) Emergency antibiotic prophylaxis and surgical scrubbing were carried out followed by osteosynthesis surgery with third shank plate in peroneal malleolus, cancellous bone distal screw in tibial malleolus and peroneal tibial screw fixation, with favourable post-surgical outcome. Following the correct healing of the medial wound and absence of complications, a partial load of 20kg was permitted after 12 weeks with an orthosis brace. One week later, the patient presented at the emergency department, stating that the ankle had become red and was also painlessly deformed. An X-ray showed a loss of reduction at this stage with destruction of the articulation (Fig. 1). On suspicion of deep wound infection vs Charcot arthropathy, percutaneous biopsy was carried out, which tested positive for S. aureus in 4 samples. On diagnosis of secondary osteomyelitis, surgery was performed, which revealed the disappearance of over 50% articular cartilage and fragmentation and macroscopic signs of osteitis in peroneal malleolus. We therefore proceeded with exeresis of the malleolus, aggressive debridement and inter-positioning of the gentamycin impregnated cement spacer in the tibiotalocalcaneal articulation, to which we added 2g of vancomycin, in accordance with antibiogram results. Intravenous treatment with vancomycin was also initiated and adjusted to kidney function, for six weeks.
During evolution and on assessment by the intensive care unit the patient presented with cardiac arrest and kidney failure and was admitted to this unit for 2 weeks. Once definitive surgery had been ruled out (tibiotalar arthrodesis) due to the further complicated patient morbidity on admission, the patient was subsequently discharged with the cement spacer as definitive treatment, together with oral antibiotics (levofloxacin 500mg/24h). After six weeks, at the first consultation the patient presented with acute phase reactant normalisation and an absence of any clinical signs of infection.
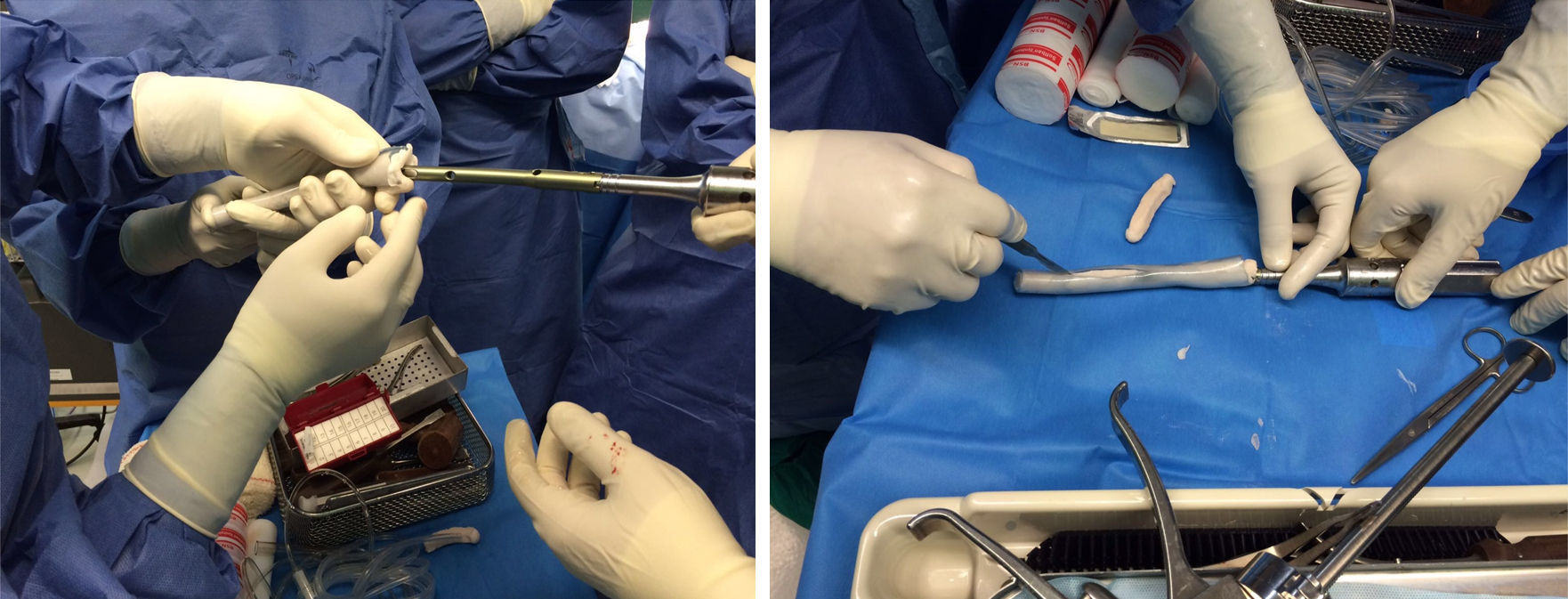
Two months after hospital discharge and again after partial load with an orthosis brace, the patient relapsed and presented with a medial ulcer with active discharge. An X-ray showed the rupture of the spacer (Fig. 2). In the light of this new situation it was suggested the patient undergo an elective below-the-knee amputation but the patient and family members rejected this. As a result, in order to stabilise the limb and treat the infection at the same time, ankle surgery with a posterior trans achilles approach was performed (due to the poor status of the soft tissues of the anterior and lateral sides of the ankle), and new debridement, with shortening of the limb and insertion of the Expert-HAN® (DePuy-Synthes, Spain) model tibiotalocalcaneal arthrodesis with cemented antibiotic-coated retrograde nail (gentamycin+vancomycin+tobramycin, see “surgical technique” section) (Fig. 3) was carried out.
After further specific intravenous treatment consisting of meropenem+linezolid, the patient evolved satisfactorily with wound healing and the disappearance of the ulcer. She was discharged with oral antibiotics (septrin Forte, one tablet every 24h). At the latest review, 9 months after surgery, the patient was asymptomatic, with acute phase reactant normalisation, wound healing and radiological evidence of tibiotalocalcaneal fusion, walking with support from a crutch, without pain, and compensating the limb shortening with a shoe implant (Fig. 4).
Surgical techniqueTo determine which antibiotics to use, apart from taking an additional pre-surgical culture, all positive cultures which have been presented from the beginning should be reviewed and the necessary antibiotics used to cover all germs in isolation. With regard to characteristics, it is essential that the antibiotics are not thermo-sensitive and powder form presentations are preferred over liquids. The appropriate global antibiotic recommended dose is between 3g, 6g and 8g of antibiotic for every 40g of polymethylmethacrylate, for therapeutic properties and non alteration of the cement properties.9,10 In our case we used 40g of Hi-Fatigue G Bone Cement (Zimmer®) polymethylmethacrylate which contained 0.9g of gentamycin sulphate (0.55g of gentamycin base), to which we added 2.5g of vancomycin and 1.5g of tobramycin. We carried out the preparation in a recipient firstly introducing the cement powder and then the antibiotic in powder form and we mixed it. After this we added the liquid antibiotic and lastly the cement liquid. We then mixed the solution according to the standard technique but recommendations are not to use the vacuum technique.10 The mixture was put into a sterilised silicone tube (2mm thicker than the nail to be used) using a cement gun, letting the air out initially at the opposite end of the tube and when the cement reached the end a finger was placed there to prevent it coming out (Fig. 3). We then put the nail in (connected to its insertion guide) through the silicone tube, ensuring that the nail was uniformly covered in cement and that the proximal end of connection to the nail was cement-free, and waited for it to set. The silicon was then cut length-wise with a surgical knife and the cemented nail obtained (Fig. 3). The nail locking screw guide or hands-free guide was attached, or with the help of fluoroscopy the locking holes of the nail were perforated prior to insertion. The nail was implanted in the standard manner, but bearing in mind that this was a solid nail with no possibility of a guide wire and that drilling had to be for insertion of a 2mm diameter greater than the uncemented nail. In our case the nail used was a nail with a physiological valgus angulation of 10mm diameter and 15cm in length (Expert-HAN, Depuy-Synthes®), with a 12mm diameter silicone tube light. Due to the shape of the ankle arthrodesis nail with its greater diameter in the proximal surface (12.5mm), we adapted our preparation technique by making a cut in the appropriate silicone area to allow for greater diameter and eliminating residue before drilling.
DiscussionDiabetic patients are at 4 times greater risk of suffering from complications after ankle facture osteosynthesis, especially if peripheral neuropathy is associated. Rates of amputation and worse functional medium to long term outcome are also higher for these patients.8 Osteoporosis which is often associated with these patients has led to the recommendation for “enhanced” osteosynthesis for these patients (double plate, tibial peroneal fixation, etc.) and also that discharge times be at least double that of non diabetic patients (10–12 weeks) with additional strict control of glycaemia.7,8 In our case, we fulfilled the first 2 premises, i.e. “enhanced” osteosynthesis and prolonged discharge, but due to patient characteristics (diabetic and with a kidney disease) and the fracture itself (open), there was a loss of reduction and secondary osteomyelitis.
Bone or joint infections are clinically highly demanding situations for the orthopaedic surgeon. Many of these patients are complex due to prior comorbidities and the poor state of the soft tissues, with a background of several surgical interventions and healing problems. They require a multidisciplinary approach which in all cases should include a specialist in infectious diseases since the majority of the patients require prolonged cycles of antibiotic treatment.
The main treatment objectives of local infection in the ankle are fracture stability or arthrodesis fusion, good soft tissue coverage and eradication of the germ causing the chronic infection which may endanger the viability of the limb.7,8 Aggressive debridement of all devitalised tissues, the filling in of dead spaces and good soft tissue coverage is necessary to achieve these aims, with participation from the Plastic Surgery Department. Although several surgical options are available for the treatment of the infection, no consensus of opinion has been established as to the ideal method. Regarding the local administration of antibiotics, polymethylmethacrylate balls or beads with gentamycin have been used as standard since the 1970s. In the 1980s these were replaced with antibiotic-impregnated cement spacers, which aimed at filling in the dead spaces. From the 1990s onwards the technique of cement antibiotic-coated nails was developed and even totally cemented nails (the latter being biomechanically inferior) which had satisfactory outcomes with regard to the eradication of infection.9–11 The cemented nails provide stability and release high doses of local antibiotic, with little systemic release and therefore fewer secondary effects. In the treatment of infected long bone non-union, and in cases such as the one we have described, in our centre we consider that the antibiotic-cemented nail is a useful tool for fulfilling the principles of stability of the focus and local deposit of antibiotic therapy, provided that correct prior debridement is made. These implants are becoming the technique of choice instead of external fixation since the latter may lead to greater patient malaise, lower stability of fracture and higher intolerance (superinfection of the pins).9
Specifically in the ankle and foot area, tibiotalcalcaneal fusion is a highly satisfactory salvage procedure in cases of severe joint destruction, misalignment or bone loss,11 as is the case we presented. Although numerous fixation methods have been used in this technique, the development of the so-called retrograde nail has surpassed all others due to continuous improvements in surgical and instrumental technique and the development of more anatomical designs which aid implantation. Although figures of up to 28% complications have been published, the more anatomical models, with a physiological valgus angulation, like the implant we used in this case, should theoretically lower this percentage.11
Our case is of interest not only due to the solid fusion achieved with the retrograde nail as a salvage procedure, but essentially due to the eradication of infection incorporating cement with antibiotics into the nail itself. No similar cases have been found in the published literature reviewed.
Level of evidenceLevel of evidence V.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
FinancingThe authors acknowledge that they have not received any type of financing for this work.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Herrera-Pérez M, Boluda-Mengod J, Gutierrez-Morales MJ, Pais-Brito JL. Artrodesis tibiotalocalcánea con clavo retrógrado cementado con antibiótico en rescate de osteosíntesis infectada de tobillo. Rev Esp Cir Ortop Traumatol. 2017;61:441–445.