The purpose of this study is to analyse the indications, complications, survivorship and clinical/functional outcome of metaphyseal sleeves as a treatment option in revision total knee arthroplasty.
Material and methodA systematic review was made following the PRISMA recommendations on the use of metaphyseal sleeves for revision total knee arthroplasty. We included prospective and retrospective studies published in the last 10 years looking at implant survivorship, clinical and functional outcome with a minimum follow-up of 2 years.
ResultsThe included studies showed good both functional and clinical outcomes. The overall reoperation rate was 16.2%, with an overall survival rate of 92.2% and aseptic survivorship of 98.2%.
ConclusionsMetaphyseal sleeves are a good treatment option for this surgery, especially in AORI II or III type bone defects, achieving good intraoperative and primary stability of the implant, with good and rapid osseointegration.
El objetivo de este estudio es analizar las indicaciones, complicaciones, supervivencia y el resultado clínico y funcional de las vainas metafisarias como opción terapéutica en las revisiones de prótesis total de rodilla.
Material y métodoSe realizó una revisión sistemática siguiendo las recomendaciones PRISMA sobre el uso de vainas metafisarias para cirugía de revisión de artroplastia de rodilla. Se incluyeron estudios prospectivos y retrospectivos publicados en los últimos 10 años que analizasen la supervivencia del implante, el resultado clínico y funcional con un seguimiento mínimo de dos años.
ResultadosLos estudios incluidos mostraron buenos resultados tanto funcionales como clínicos. El porcentaje de reintervención global fue de 16,2%, con una tasa de supervivencia global de 92,2% y una supervivencia aséptica de 98,2%.
ConclusionesLas vainas metafisarias suponen una buena opción de tratamiento de esta cirugía, especialmente en defectos tipo AORI II o III consiguiendo buena estabilidad intraoperatoria y primaria del implante, con buena y rápida osteointegración.
The number of total knee arthroplasties continues to increase and, as a consequence, the incidence of revisions thereof,1 and this represents one of the most important challenges in orthopaedic surgery today.
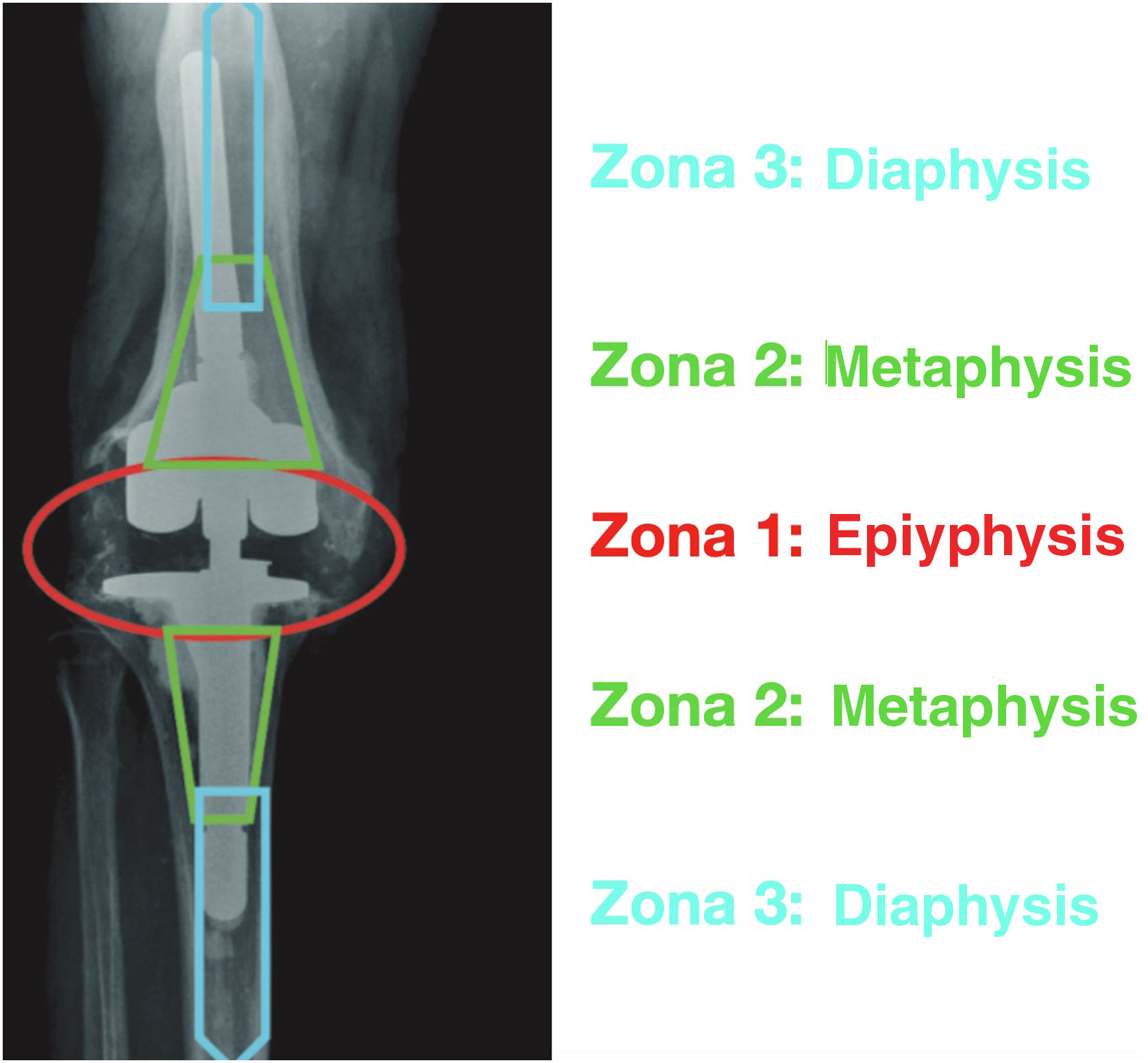
Morgan-Jones et al.,2 introduced the concept of zone fixation in knee revision surgery. They described three anatomical zones in the femur and tibia, each of which serves as support for fixation of the implant: zone 1 is the epiphysis, zone 2 is the metaphysis, and zone 3 is the diaphysis (Fig. 1). While in primary knee arthroplasty fixation depends mainly on a good articular surface without bone defect, in revisions in zone 1, this fixation is compromised and has shown a high failure rate due to defects at this level and poor vascularisation.3 Bone loss in revisions represents a significant problem in achieving a sufficiently stable interface between the implant and the bone.
Fixation by knee revision surgery areas. Source: Morgan-Jones et al.2
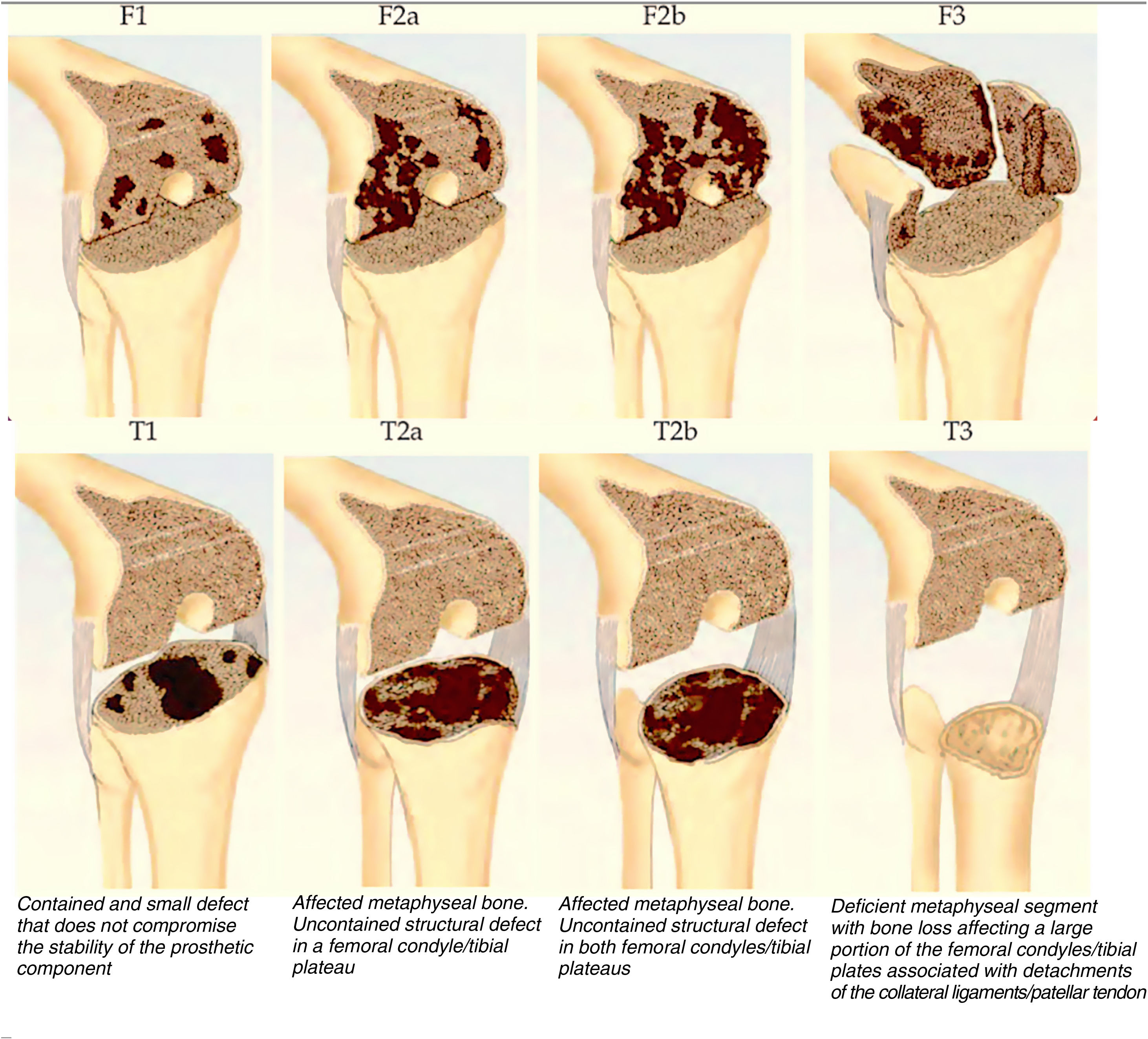
The Anderson Orthopaedic Research Institute (AORI) classification of bone loss is the most used in prosthetic revisions4 (the values of said classification are described in Fig. 2). Fixation in zone 1 is possible with conventional revision components with or without stems, only when these defects can be filled with cement or small amounts of bone graft.5 In cases of type 2 and 3 defects, additional fixation in the other areas is necessary to achieve a stable load-bearing surface and thus a good surgical result.
Anderson Orthopedic Research Institute (AORI) classification of bone defects. Source: Engh and Ammeen.4
Seeking fixation in zone 3 (diaphysis), the use of stems, both cemented and uncemented, was initially proposed, allowing the load to be transmitted to the diaphysis and combining fixation at both levels.6–9
In recent years, interest has been shown in fixation in the metaphyseal area (zone 2).10 Fixation at this level emerged as an option to avoid the aforementioned problems since it is an area with theoretically less damage and bone defect than the epiphyseal, and is also better vascularised, which represents a biological advantage with respect to the other areas for any type of fixation. Metaphyseal sleeves and trabecular metal cones emerged as an alternative for the management of these large defects in revision knee surgery.
Metaphyseal sleeves (Depuy, Warsaw [Indiana]) were introduced in the 1970s for use with hinge prostheses11 and were developed and modified until their use was enabled in semi-constrained implants, where in addition to filling bone defect, they allow fixation and immediate stability in the metaphyseal area, with bone growth and less bone resorption and stress shielding than other systems.12
Our objective is to carry out a systematic review of the literature based on the following PICO criteria:
- -
The study population (P) corresponds to all those patients undergoing revision knee arthroplasty.
- -
The intervention (I) would be those patients in whom metaphyseal fixation sleeves were used in the replacement surgery.
- -
No comparison was made (C) with other fixation systems.
- -
The results (O) to be analysed would be the indications, complications, survival of the implants and the clinical and functional result of the prosthetic revision surgery where metaphyseal sleeves were used.
A systematic review was carried out through an electronic search on the use of metaphyseal sleeves for revision knee arthroplasty surgery following the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)” recommendations.13
This review has been registered in PROSPERO (international prospective register of systematic reviews) with ID CRD42023447265.
Systematic searchThe search was carried out in December 2022 for articles published in the following databases: Medline, Web of Science, Cochrane Central Registry of Controlled Trials and Embase, between January 2010 and December 2022, using keywords in the databases mentioned: (metaphyseal[All Fields] AND sleeves[All Fields] AND («arthroplasty, replacement, knee» [MeSH Terms] OR («arthroplasty»[All Fields] AND «replacement»[All Fields] AND revision replacement, metaphyseal AND revision arthroplasty, metaphyseal AND “knee”[All Fields]) OR “knee replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “knee”[All Fields] AND “arthroplasty”[All Fields]) OR “total knee arthroplasty” [All Fields]).
The combination of free text terms and Medical Subject Headings (MeSH) in the title and abstract was used to carry out the research.
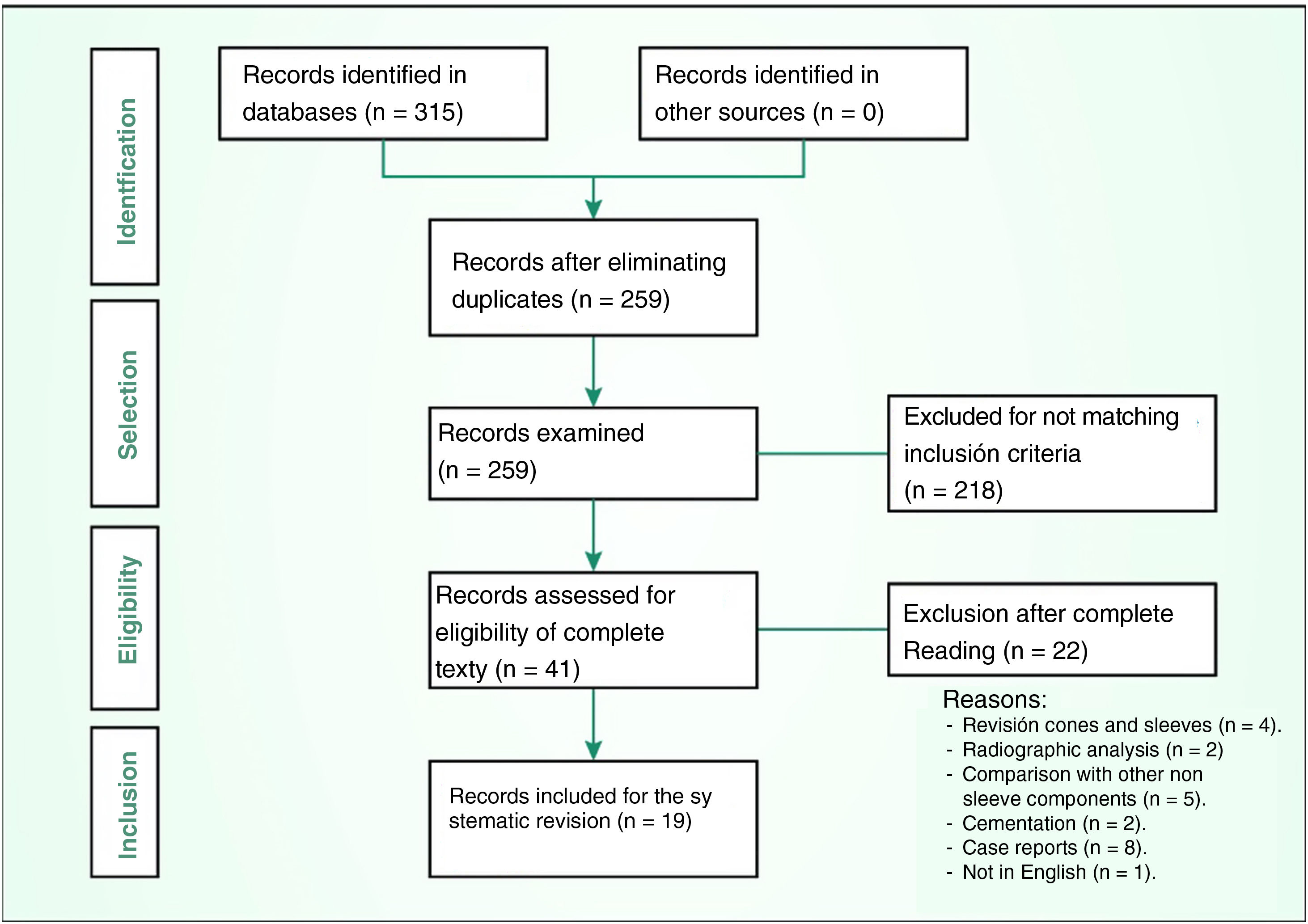
Study selectionThree authors independently reviewed all the titles of the initial search query (315 citations) and all those titles that mentioned the use of metaphyseal sleeves in knee surgery were selected, excluding 218 articles based on the abstract, since they were not articles related to the topic to be reviewed. Subsequently, all duplicate titles and articles were eliminated, leaving 42 that were selected for complete reading of the articles, which was carried out by two reviewers.
Articles that met the previously mentioned PICO criteria were included in the review: those patients undergoing revision knee arthroplasty (P) in which the technique employed used metaphyseal sleeves (I) and that analysed the indications, complications and the clinical and functional outcome regarding their use in knee prosthetic revision surgery (O).
All the selected articles were prospective and retrospective studies/observations that analysed the aforementioned. No records were obtained from other sources (paper journals, local repositories or web pages).
Exclusion criteriaAll those that were not written in English were excluded. Also in vitro studies, publications on surgical technique, or those that analysed the use of sleeves in primary surgery or in more specific situations such as sequelae of fractures or their implantation without a stem. All studies should have a minimum follow-up of two years, a time that the authors considered the minimum necessary to evaluate the survival of the implants and evaluate the clinical and functional improvement after arthroplasty, as considered by most scientific journals of the specialty that includes it as the minimum follow-up time to publish results of a study, and having been published in the last 10 years, a time that we consider the most relevant for our review, due to possible variations in implant design. Nineteen articles were included in the final analysis (Fig. 3).14–33
Data extractionFrom the selected articles, the following data were obtained: number of patients and knees treated, indications for revision surgery, classification and type of bone defect, age of patients and average follow-up, number of femoral and tibial sleeves implanted and level of constriction of the prosthesis.
Variables analysedRegarding the postoperative results, the number of reoperations for any cause, the number of reinterventions due to an intercurrent infectious process and the percentage of overall and aseptic survival on the analysed knees were recorded, taking into account for these indicators as the final event the prosthetic replacement due to any cause or aseptic loosening respectively. The mobility achieved and the pre- and postoperative scores on the functional scales were also analysed: Oxford Knee Score (OKS), Knee Society Score (KSS), Knee Society Function Score (KSFS) and Western Ontario and McMaster Universities Arthritis Index (WOMAC).34–36
These functional scales are based on surveys carried out on patients where questions are answered about pain, the need for drugs, the feeling of instability, the ability to carry out activities of daily living, bending down or climbing stairs, and the distance or time they are able to walk. In the case of the OKS scale, the most unfavourable result would be 0, and the most favourable 48. In the KSS and KSFS the result ranges from 0 (worst) to 100 (best). Finally, in the WOMAC the score is associated with functional status in reverse: made up of 24 questions in which patients answer 0 if they are not affected and 4 if they are very affected, so the closer the result is to 0 the better, while the worst possible is 96 points (20 points for pain, 8 for stiffness and 68 for functional capacity).
Evaluation of the risk of biasDue to the heterogeneity and variability in the data collection of the articles, the final number of patients in whom follow-up was possible in each of the articles was taken into account for the analysis, not the initial populations, and those patients with loss to follow-up were excluded as we sought to homogenise our review as much as possible.
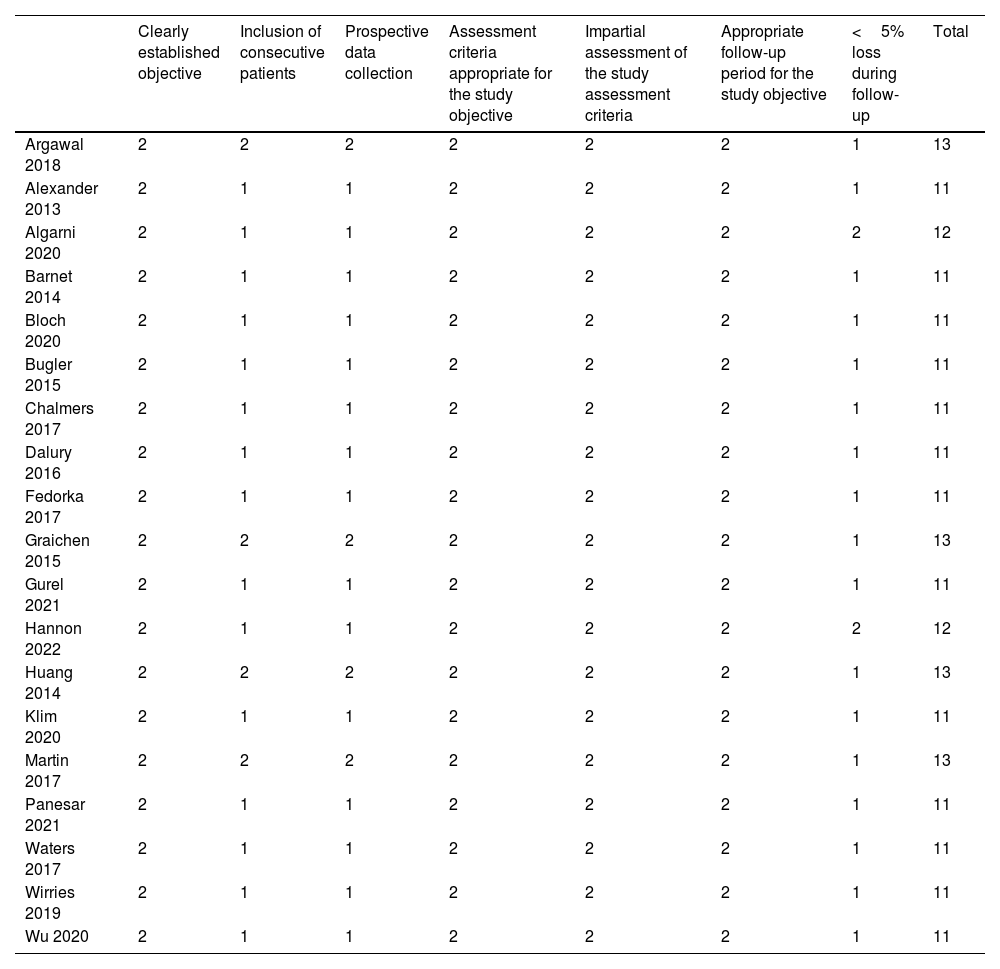
Two authors independently assessed the potential risk of bias assessed by the included studies using MINORS, a methodological index for non-randomised studies.37 Items scored 0 if not reported; 1 when reported but inadequate; and 2 when informed and appropriate. The overall ideal score was 14 for non-comparative studies. Low risk of bias was considered when the studies met all the MINORS criteria, and high risk of bias in the other studies (Table 1).
Index of minors.
| Clearly established objective | Inclusion of consecutive patients | Prospective data collection | Assessment criteria appropriate for the study objective | Impartial assessment of the study assessment criteria | Appropriate follow-up period for the study objective | <5% loss during follow-up | Total | |
|---|---|---|---|---|---|---|---|---|
| Argawal 2018 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 13 |
| Alexander 2013 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Algarni 2020 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 12 |
| Barnet 2014 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Bloch 2020 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Bugler 2015 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Chalmers 2017 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Dalury 2016 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Fedorka 2017 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Graichen 2015 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 13 |
| Gurel 2021 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Hannon 2022 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 12 |
| Huang 2014 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 13 |
| Klim 2020 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Martin 2017 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 13 |
| Panesar 2021 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Waters 2017 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Wirries 2019 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
| Wu 2020 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 11 |
0: uninformed item; 1: informed item, but insufficient; 2: informed item and appropriate.
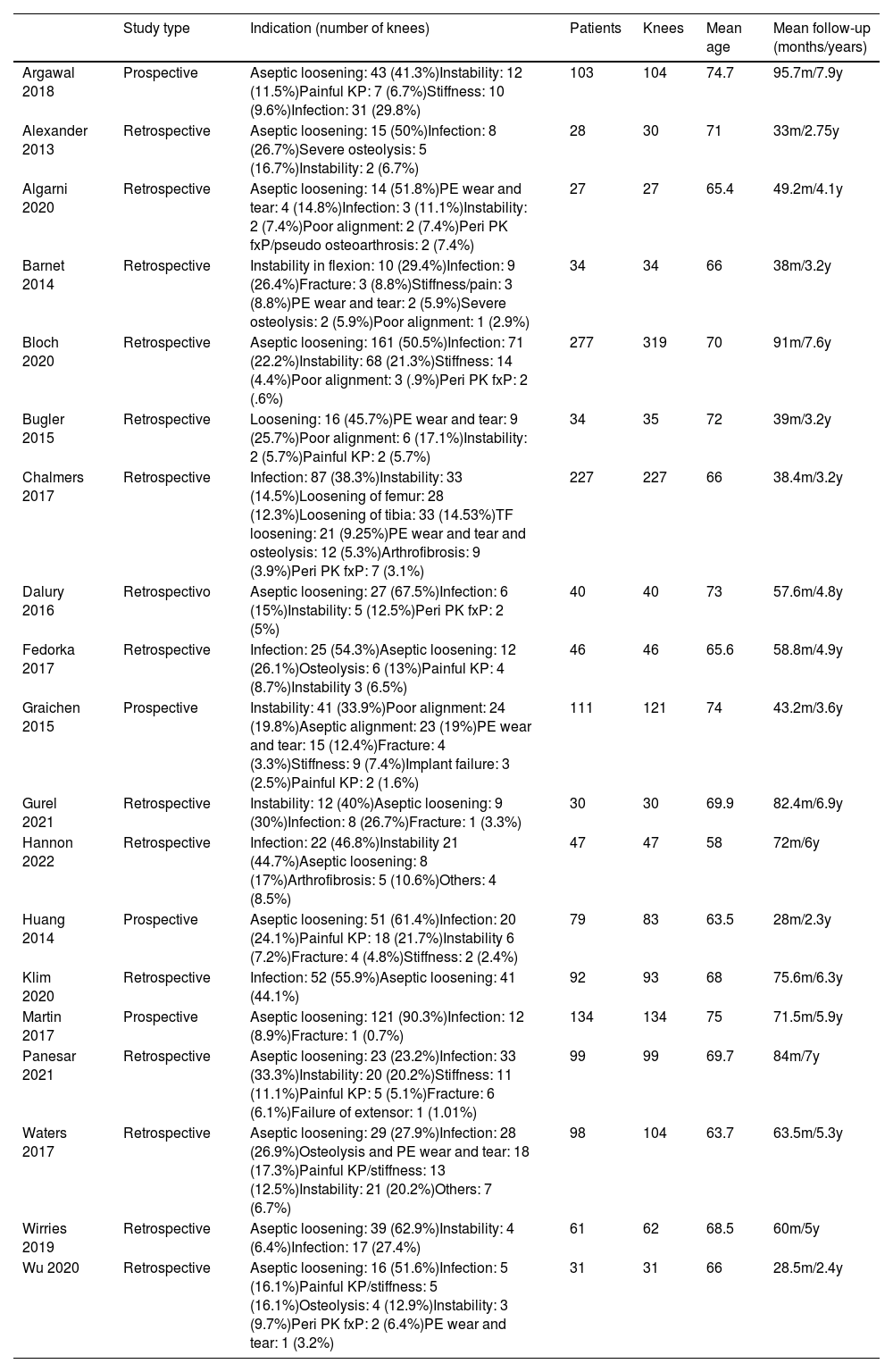
In the 19 selected articles, a total of 1666 knees in 1568 patients were analysed. Their average age was 68.4 years and the average follow-up of the articles was 58.4 months. Regarding the cause of revision surgery, 730 were indicated by aseptic loosening (43.8%) of one or several components of the prosthesis, this being the main indication for prosthetic replacement. The second most common cause was infection, with 437 prostheses revised for this reason (26.5%). 15.9% of the revisions were performed for instability (265), and the less frequent causes were painful TKA, stiffness, wear of the polyethylene insert, poor alignment, periprosthetic fracture and severe osteolysis (Table 2).
Type of study, indication, demographic data and mean follow-up.
| Study type | Indication (number of knees) | Patients | Knees | Mean age | Mean follow-up (months/years) | |
|---|---|---|---|---|---|---|
| Argawal 2018 | Prospective | Aseptic loosening: 43 (41.3%)Instability: 12 (11.5%)Painful KP: 7 (6.7%)Stiffness: 10 (9.6%)Infection: 31 (29.8%) | 103 | 104 | 74.7 | 95.7m/7.9y |
| Alexander 2013 | Retrospective | Aseptic loosening: 15 (50%)Infection: 8 (26.7%)Severe osteolysis: 5 (16.7%)Instability: 2 (6.7%) | 28 | 30 | 71 | 33m/2.75y |
| Algarni 2020 | Retrospective | Aseptic loosening: 14 (51.8%)PE wear and tear: 4 (14.8%)Infection: 3 (11.1%)Instability: 2 (7.4%)Poor alignment: 2 (7.4%)Peri PK fxP/pseudo osteoarthrosis: 2 (7.4%) | 27 | 27 | 65.4 | 49.2m/4.1y |
| Barnet 2014 | Retrospective | Instability in flexion: 10 (29.4%)Infection: 9 (26.4%)Fracture: 3 (8.8%)Stiffness/pain: 3 (8.8%)PE wear and tear: 2 (5.9%)Severe osteolysis: 2 (5.9%)Poor alignment: 1 (2.9%) | 34 | 34 | 66 | 38m/3.2y |
| Bloch 2020 | Retrospective | Aseptic loosening: 161 (50.5%)Infection: 71 (22.2%)Instability: 68 (21.3%)Stiffness: 14 (4.4%)Poor alignment: 3 (.9%)Peri PK fxP: 2 (.6%) | 277 | 319 | 70 | 91m/7.6y |
| Bugler 2015 | Retrospective | Loosening: 16 (45.7%)PE wear and tear: 9 (25.7%)Poor alignment: 6 (17.1%)Instability: 2 (5.7%)Painful KP: 2 (5.7%) | 34 | 35 | 72 | 39m/3.2y |
| Chalmers 2017 | Retrospective | Infection: 87 (38.3%)Instability: 33 (14.5%)Loosening of femur: 28 (12.3%)Loosening of tibia: 33 (14.53%)TF loosening: 21 (9.25%)PE wear and tear and osteolysis: 12 (5.3%)Arthrofibrosis: 9 (3.9%)Peri PK fxP: 7 (3.1%) | 227 | 227 | 66 | 38.4m/3.2y |
| Dalury 2016 | Retrospectivo | Aseptic loosening: 27 (67.5%)Infection: 6 (15%)Instability: 5 (12.5%)Peri PK fxP: 2 (5%) | 40 | 40 | 73 | 57.6m/4.8y |
| Fedorka 2017 | Retrospective | Infection: 25 (54.3%)Aseptic loosening: 12 (26.1%)Osteolysis: 6 (13%)Painful KP: 4 (8.7%)Instability 3 (6.5%) | 46 | 46 | 65.6 | 58.8m/4.9y |
| Graichen 2015 | Prospective | Instability: 41 (33.9%)Poor alignment: 24 (19.8%)Aseptic alignment: 23 (19%)PE wear and tear: 15 (12.4%)Fracture: 4 (3.3%)Stiffness: 9 (7.4%)Implant failure: 3 (2.5%)Painful KP: 2 (1.6%) | 111 | 121 | 74 | 43.2m/3.6y |
| Gurel 2021 | Retrospective | Instability: 12 (40%)Aseptic loosening: 9 (30%)Infection: 8 (26.7%)Fracture: 1 (3.3%) | 30 | 30 | 69.9 | 82.4m/6.9y |
| Hannon 2022 | Retrospective | Infection: 22 (46.8%)Instability 21 (44.7%)Aseptic loosening: 8 (17%)Arthrofibrosis: 5 (10.6%)Others: 4 (8.5%) | 47 | 47 | 58 | 72m/6y |
| Huang 2014 | Prospective | Aseptic loosening: 51 (61.4%)Infection: 20 (24.1%)Painful KP: 18 (21.7%)Instability 6 (7.2%)Fracture: 4 (4.8%)Stiffness: 2 (2.4%) | 79 | 83 | 63.5 | 28m/2.3y |
| Klim 2020 | Retrospective | Infection: 52 (55.9%)Aseptic loosening: 41 (44.1%) | 92 | 93 | 68 | 75.6m/6.3y |
| Martin 2017 | Prospective | Aseptic loosening: 121 (90.3%)Infection: 12 (8.9%)Fracture: 1 (0.7%) | 134 | 134 | 75 | 71.5m/5.9y |
| Panesar 2021 | Retrospective | Aseptic loosening: 23 (23.2%)Infection: 33 (33.3%)Instability: 20 (20.2%)Stiffness: 11 (11.1%)Painful KP: 5 (5.1%)Fracture: 6 (6.1%)Failure of extensor: 1 (1.01%) | 99 | 99 | 69.7 | 84m/7y |
| Waters 2017 | Retrospective | Aseptic loosening: 29 (27.9%)Infection: 28 (26.9%)Osteolysis and PE wear and tear: 18 (17.3%)Painful KP/stiffness: 13 (12.5%)Instability: 21 (20.2%)Others: 7 (6.7%) | 98 | 104 | 63.7 | 63.5m/5.3y |
| Wirries 2019 | Retrospective | Aseptic loosening: 39 (62.9%)Instability: 4 (6.4%)Infection: 17 (27.4%) | 61 | 62 | 68.5 | 60m/5y |
| Wu 2020 | Retrospective | Aseptic loosening: 16 (51.6%)Infection: 5 (16.1%)Painful KP/stiffness: 5 (16.1%)Osteolysis: 4 (12.9%)Instability: 3 (9.7%)Peri PK fxP: 2 (6.4%)PE wear and tear: 1 (3.2%) | 31 | 31 | 66 | 28.5m/2.4y |
KP: knee prosthesis; m: months; PE: polyethylene; Peri PK fx: periprosthetic knee fracture; TF loosening: loosening of tibia and femur; y: years.
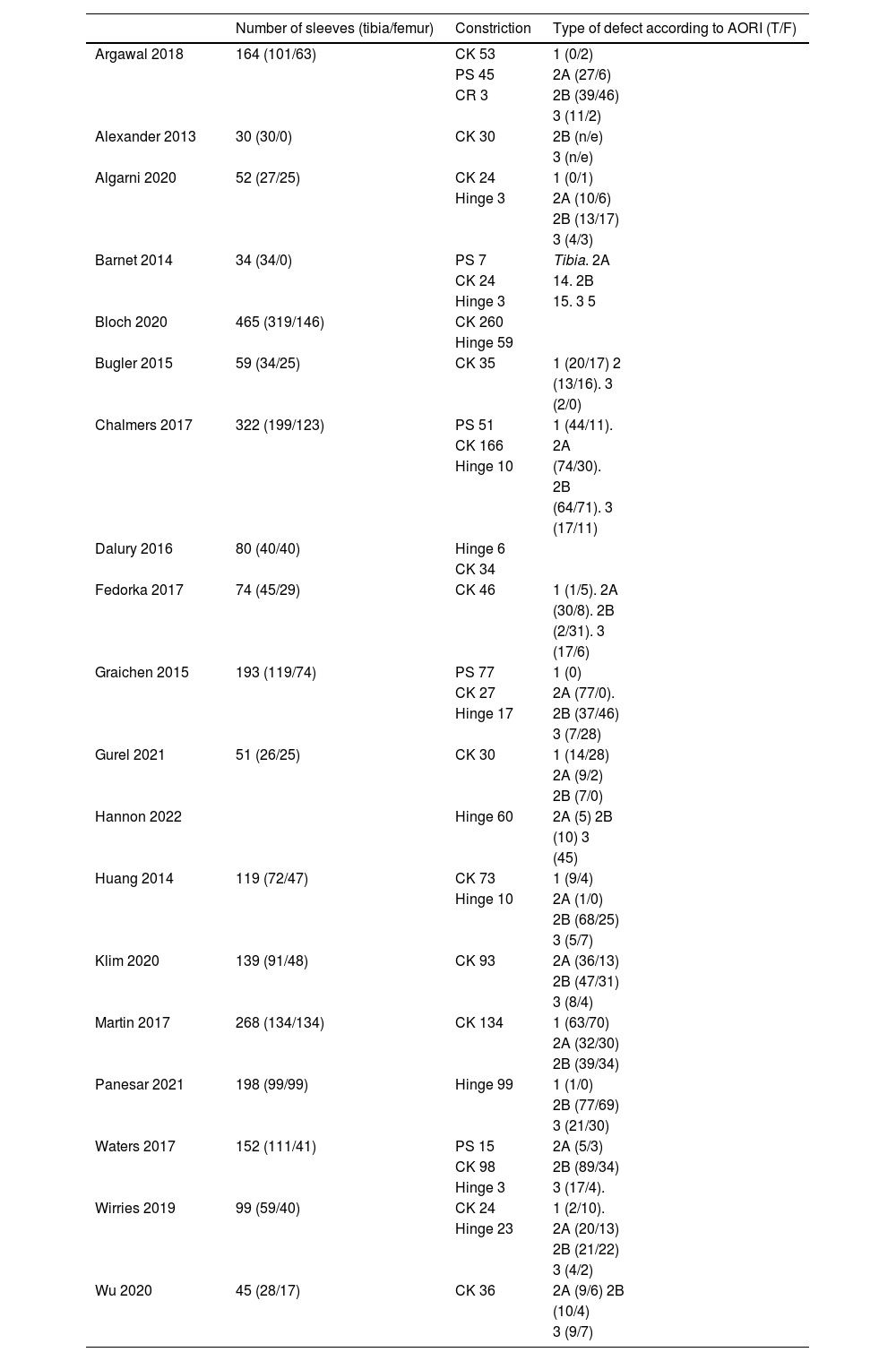
Two thousand five hundred and forty-four metaphyseal sleeves were implanted (in the articles in which the anatomical region is specified, 1568 were tibial and 976 were femoral). The bone defects identified in the revision surgery were: 296 AORI 1, 276 AORI 3 and 1463 AORI 2 type defects, these being the most frequent defects analysed in the articles (Table 3).
Number and location of implants, constriction and bone defect according to AORI.
| Number of sleeves (tibia/femur) | Constriction | Type of defect according to AORI (T/F) | |
|---|---|---|---|
| Argawal 2018 | 164 (101/63) | CK 53 | 1 (0/2) |
| PS 45 | 2A (27/6) | ||
| CR 3 | 2B (39/46) | ||
| 3 (11/2) | |||
| Alexander 2013 | 30 (30/0) | CK 30 | 2B (n/e) |
| 3 (n/e) | |||
| Algarni 2020 | 52 (27/25) | CK 24 | 1 (0/1) |
| Hinge 3 | 2A (10/6) | ||
| 2B (13/17) | |||
| 3 (4/3) | |||
| Barnet 2014 | 34 (34/0) | PS 7 | Tibia. 2A |
| CK 24 | 14. 2B | ||
| Hinge 3 | 15. 3 5 | ||
| Bloch 2020 | 465 (319/146) | CK 260 | |
| Hinge 59 | |||
| Bugler 2015 | 59 (34/25) | CK 35 | 1 (20/17) 2 |
| (13/16). 3 | |||
| (2/0) | |||
| Chalmers 2017 | 322 (199/123) | PS 51 | 1 (44/11). |
| CK 166 | 2A | ||
| Hinge 10 | (74/30). | ||
| 2B | |||
| (64/71). 3 | |||
| (17/11) | |||
| Dalury 2016 | 80 (40/40) | Hinge 6 | |
| CK 34 | |||
| Fedorka 2017 | 74 (45/29) | CK 46 | 1 (1/5). 2A |
| (30/8). 2B | |||
| (2/31). 3 | |||
| (17/6) | |||
| Graichen 2015 | 193 (119/74) | PS 77 | 1 (0) |
| CK 27 | 2A (77/0). | ||
| Hinge 17 | 2B (37/46) | ||
| 3 (7/28) | |||
| Gurel 2021 | 51 (26/25) | CK 30 | 1 (14/28) |
| 2A (9/2) | |||
| 2B (7/0) | |||
| Hannon 2022 | Hinge 60 | 2A (5) 2B | |
| (10) 3 | |||
| (45) | |||
| Huang 2014 | 119 (72/47) | CK 73 | 1 (9/4) |
| Hinge 10 | 2A (1/0) | ||
| 2B (68/25) | |||
| 3 (5/7) | |||
| Klim 2020 | 139 (91/48) | CK 93 | 2A (36/13) |
| 2B (47/31) | |||
| 3 (8/4) | |||
| Martin 2017 | 268 (134/134) | CK 134 | 1 (63/70) |
| 2A (32/30) | |||
| 2B (39/34) | |||
| Panesar 2021 | 198 (99/99) | Hinge 99 | 1 (1/0) |
| 2B (77/69) | |||
| 3 (21/30) | |||
| Waters 2017 | 152 (111/41) | PS 15 | 2A (5/3) |
| CK 98 | 2B (89/34) | ||
| Hinge 3 | 3 (17/4). | ||
| Wirries 2019 | 99 (59/40) | CK 24 | 1 (2/10). |
| Hinge 23 | 2A (20/13) | ||
| 2B (21/22) | |||
| 3 (4/2) | |||
| Wu 2020 | 45 (28/17) | CK 36 | 2A (9/6) 2B |
| (10/4) | |||
| 3 (9/7) |
AORI: Anderson Orthopaedic Research Institute; CK: Condylar Constrained Knee; CR: cruciate retaining; F: femur; PS: posterior stabilised; T: tibia.
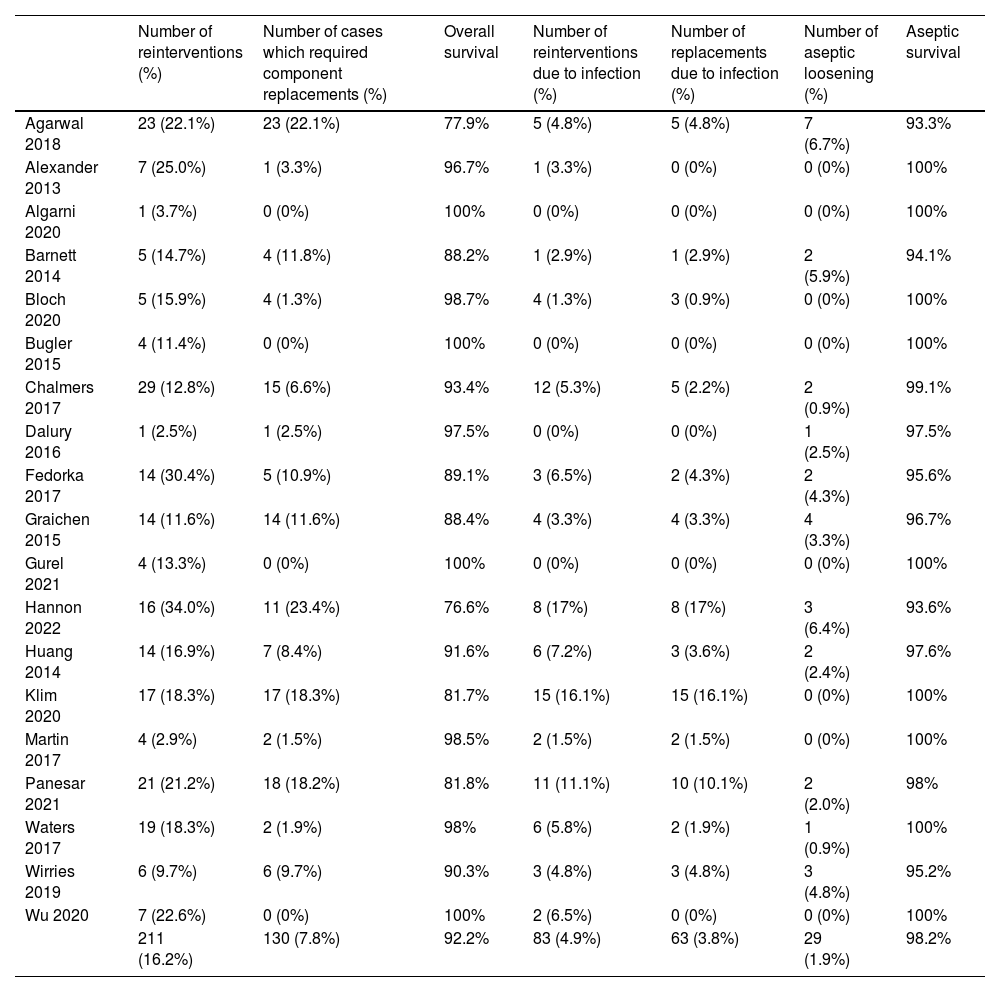
In our review, the overall reintervention percentage was 16.2% and the overall survival of the implants was 92.2%, considering any cause for their replacement. A 4.9% of reinterventions due to infectious causes and a component replacement rate for this same cause of 3.8% were observed. Regarding aseptic loosening and mechanical failure of the implant as a cause of revision, 29 cases were reported in the analysed articles, being 1.9%, assuming a survival free of aseptic loosening of 98.2% (Table 4).
Reinterventions and replacement of components for all causes, infectious cause and number and percentage of aseptic loosening+survival.
| Number of reinterventions (%) | Number of cases which required component replacements (%) | Overall survival | Number of reinterventions due to infection (%) | Number of replacements due to infection (%) | Number of aseptic loosening (%) | Aseptic survival | |
|---|---|---|---|---|---|---|---|
| Agarwal 2018 | 23 (22.1%) | 23 (22.1%) | 77.9% | 5 (4.8%) | 5 (4.8%) | 7 (6.7%) | 93.3% |
| Alexander 2013 | 7 (25.0%) | 1 (3.3%) | 96.7% | 1 (3.3%) | 0 (0%) | 0 (0%) | 100% |
| Algarni 2020 | 1 (3.7%) | 0 (0%) | 100% | 0 (0%) | 0 (0%) | 0 (0%) | 100% |
| Barnett 2014 | 5 (14.7%) | 4 (11.8%) | 88.2% | 1 (2.9%) | 1 (2.9%) | 2 (5.9%) | 94.1% |
| Bloch 2020 | 5 (15.9%) | 4 (1.3%) | 98.7% | 4 (1.3%) | 3 (0.9%) | 0 (0%) | 100% |
| Bugler 2015 | 4 (11.4%) | 0 (0%) | 100% | 0 (0%) | 0 (0%) | 0 (0%) | 100% |
| Chalmers 2017 | 29 (12.8%) | 15 (6.6%) | 93.4% | 12 (5.3%) | 5 (2.2%) | 2 (0.9%) | 99.1% |
| Dalury 2016 | 1 (2.5%) | 1 (2.5%) | 97.5% | 0 (0%) | 0 (0%) | 1 (2.5%) | 97.5% |
| Fedorka 2017 | 14 (30.4%) | 5 (10.9%) | 89.1% | 3 (6.5%) | 2 (4.3%) | 2 (4.3%) | 95.6% |
| Graichen 2015 | 14 (11.6%) | 14 (11.6%) | 88.4% | 4 (3.3%) | 4 (3.3%) | 4 (3.3%) | 96.7% |
| Gurel 2021 | 4 (13.3%) | 0 (0%) | 100% | 0 (0%) | 0 (0%) | 0 (0%) | 100% |
| Hannon 2022 | 16 (34.0%) | 11 (23.4%) | 76.6% | 8 (17%) | 8 (17%) | 3 (6.4%) | 93.6% |
| Huang 2014 | 14 (16.9%) | 7 (8.4%) | 91.6% | 6 (7.2%) | 3 (3.6%) | 2 (2.4%) | 97.6% |
| Klim 2020 | 17 (18.3%) | 17 (18.3%) | 81.7% | 15 (16.1%) | 15 (16.1%) | 0 (0%) | 100% |
| Martin 2017 | 4 (2.9%) | 2 (1.5%) | 98.5% | 2 (1.5%) | 2 (1.5%) | 0 (0%) | 100% |
| Panesar 2021 | 21 (21.2%) | 18 (18.2%) | 81.8% | 11 (11.1%) | 10 (10.1%) | 2 (2.0%) | 98% |
| Waters 2017 | 19 (18.3%) | 2 (1.9%) | 98% | 6 (5.8%) | 2 (1.9%) | 1 (0.9%) | 100% |
| Wirries 2019 | 6 (9.7%) | 6 (9.7%) | 90.3% | 3 (4.8%) | 3 (4.8%) | 3 (4.8%) | 95.2% |
| Wu 2020 | 7 (22.6%) | 0 (0%) | 100% | 2 (6.5%) | 0 (0%) | 0 (0%) | 100% |
| 211 (16.2%) | 130 (7.8%) | 92.2% | 83 (4.9%) | 63 (3.8%) | 29 (1.9%) | 98.2% |
Aseptic survival: percentage of prostheses free of replacement by aseptic loosening; overall survival: percentage of prostheses free of prosthetic replacement for any cause.
Both survivals have been calculated based on the sum in absolute numbers of the cases recorded in the articles. In the case of overall survival, the total number of replacements for any cause was 130 (7.8%) and knee prostheses free of replacement were 92.2%. Regarding aseptic survival, the total number of aseptic loosening was 29 (1.9%) and aseptic survival was 98.2%.
A maximum score on the MINORS scale was not achieved in any of the articles analysed, and none could be considered low risk; however, a score greater than or equal to 11 points was obtained in all of them (Table 1).
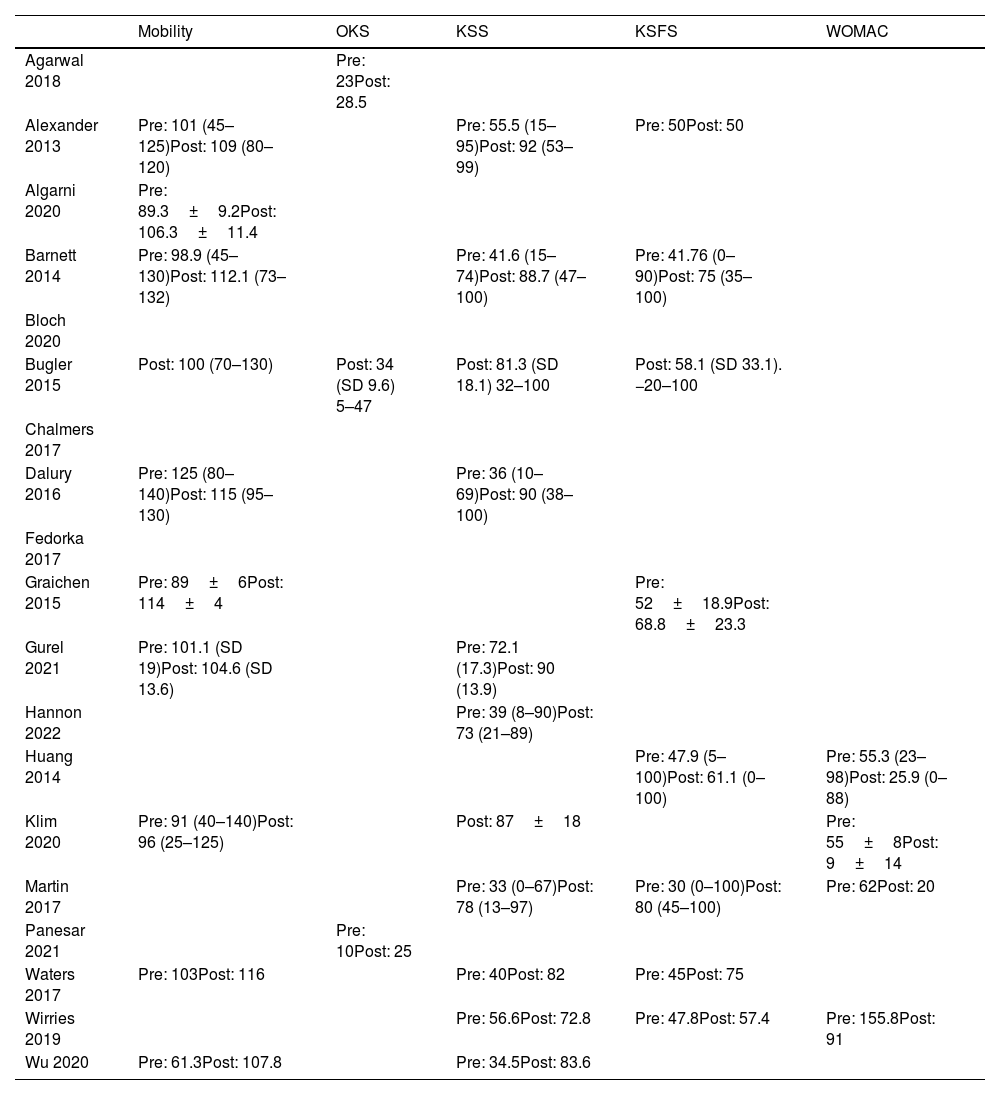
In all the articles analysed, except 4, an improvement was obtained with respect to the preoperative period in the scores of some of the functional scales analysed, with an improvement in mobility of about 13.5° (from 96.4° to 108.1°) (Table 5).
Functional result.
| Mobility | OKS | KSS | KSFS | WOMAC | |
|---|---|---|---|---|---|
| Agarwal 2018 | Pre: 23Post: 28.5 | ||||
| Alexander 2013 | Pre: 101 (45–125)Post: 109 (80–120) | Pre: 55.5 (15–95)Post: 92 (53–99) | Pre: 50Post: 50 | ||
| Algarni 2020 | Pre: 89.3±9.2Post: 106.3±11.4 | ||||
| Barnett 2014 | Pre: 98.9 (45–130)Post: 112.1 (73–132) | Pre: 41.6 (15–74)Post: 88.7 (47–100) | Pre: 41.76 (0–90)Post: 75 (35–100) | ||
| Bloch 2020 | |||||
| Bugler 2015 | Post: 100 (70–130) | Post: 34 (SD 9.6) 5–47 | Post: 81.3 (SD 18.1) 32–100 | Post: 58.1 (SD 33.1). −20–100 | |
| Chalmers 2017 | |||||
| Dalury 2016 | Pre: 125 (80–140)Post: 115 (95–130) | Pre: 36 (10–69)Post: 90 (38–100) | |||
| Fedorka 2017 | |||||
| Graichen 2015 | Pre: 89±6Post: 114±4 | Pre: 52±18.9Post: 68.8±23.3 | |||
| Gurel 2021 | Pre: 101.1 (SD 19)Post: 104.6 (SD 13.6) | Pre: 72.1 (17.3)Post: 90 (13.9) | |||
| Hannon 2022 | Pre: 39 (8–90)Post: 73 (21–89) | ||||
| Huang 2014 | Pre: 47.9 (5–100)Post: 61.1 (0–100) | Pre: 55.3 (23–98)Post: 25.9 (0–88) | |||
| Klim 2020 | Pre: 91 (40–140)Post: 96 (25–125) | Post: 87±18 | Pre: 55±8Post: 9±14 | ||
| Martin 2017 | Pre: 33 (0–67)Post: 78 (13–97) | Pre: 30 (0–100)Post: 80 (45–100) | Pre: 62Post: 20 | ||
| Panesar 2021 | Pre: 10Post: 25 | ||||
| Waters 2017 | Pre: 103Post: 116 | Pre: 40Post: 82 | Pre: 45Post: 75 | ||
| Wirries 2019 | Pre: 56.6Post: 72.8 | Pre: 47.8Post: 57.4 | Pre: 155.8Post: 91 | ||
| Wu 2020 | Pre: 61.3Post: 107.8 | Pre: 34.5Post: 83.6 |
KSFS: Knee Society Function Score; KSS: Knee Society Score; OKS: Oxford Knee Score; Post: postoperative; Pre: preoperative; WOMAC: Western Ontario and McMaster Universities Arthritis Index.
The main findings of this review are that replacement of total knee prostheses with metaphyseal sleeves is a safe option in complex cases with AORI 3 and AORI 2A or B defects, the latter being the main defects treated in the included articles. Also, that it is associated with high implant survival and a very low implant loosening rate: 1.6% in the data collected from the 19 articles. Furthermore, it presents a good functional result with improvement in the scales analysed with an average follow-up of the articles of 58.4 months (5 years).
Survival for aseptic loosening in the 19 articles varied from 93.6% analysed by Wirries et al.,25 to 100% by Algarni et al. and Martín et al.21 The good mechanical performance of this type of implant can be attributed to the high capacity of the sleeves to facilitate bone growth in the metaphysis due to their high porosity.29 Some authors even advocate a lesser relevance of fixation at the level of zone 3 (diaphysis), considering it only a guide for alignment and temporary stabilisation until the integration of the sleeves, thereby being able to reduce the length and diameter of the stems and the complications derived from this.3,7,8,10,38,39
Regarding functional results, the use of metaphyseal sleeves was also associated with good results in the articles analysed in this review. Hannon et al.18 found a statistically significant improvement in the KSS two years after the intervention, going from an average of 39, which corresponds to poor functional capacity, to an average of 73 in the postoperative period, which corresponds to good functional capacity. This functional improvement has also been analysed by different authors using different scales. Wirries et al.25 and Martin-Hernandez et al.21 also found improvement in the functional scale analysed (WOMAC) and several authors such as Gurel et al.17 or Algarni et al.28 also found statistically significant improvement in the range of mobility with the use of metaphyseal sleeves.
Despite being an effective surgery, revision surgery generally has more unfavourable results than primary knee arthroplasty. In this way, the survival of the revision implant is significantly lower than that of a primary prosthesis, which is greater than 95% at 15 years40 and in addition the mechanisms of implant failure in the case of revisions are different from those typically mentioned in the literature on primary arthroplasty. Suarez et al.41 reported a failure rate of 12%, the most frequent cause being infection (46%), aseptic loosening (19%) and instability (13%). These failures were found to be four times more likely when the cause of the primary replacement was infection and the implant survival rate they found was 82% at 12 years. Years later, Geary et al.42 analysed 1632 knees with similar results and also with infection as the main cause of failure of the revisions performed.
The data found in our systematic review are similar to those provided by other authors. Unlike other similar publications, the search was restricted to a minimum time of two years, which has been considered necessary by the authors to evaluate the survival and functional outcome of prosthetic revision knee surgery, in addition to providing new data regarding what was published on a topic that is current and that this type of implants is increasingly used for knee revision surgery. Furthermore, this review has been registered in PROSPERO, unlike the reviews published to date. Zanirato et al.,39 analysed 13 articles that included 1079 knee revision surgeries with a mean follow-up of 4 years and found an aseptic survival rate of 97.7%. In another review by Bonangiza et al.,43 in the 10 articles analysed, they found 928 knees with a mean follow-up of 45 months, of which 36 knees (4%) were reviewed for infectious reasons, finding loosening of the sleeves in five of those cases (.35%). At the same time, 27 cases (3%) were reviewed for non-infectious reasons, in which implant loosening was evident in 10 cases (aseptic loosening rate of .7%). In this case, an improvement in the final clinical result was also evident. Roach et al.44 in a systematic review that included the use of cones and sleeves, in the 12 articles selected in the case of metaphyseal sleeves, found an overall reintervention rate of 9.7% and a rate of aseptic loosening of .8%. It should be noted here that the rate of both reintervention and aseptic loosening in the case of tantalum cones was practically double that in the case of metaphyseal sleeves (18.7% and 1.7% respectively).
It is important to mention the limitations of this review: the studies collected are only in English and, furthermore, they are not long series of patients and there is great variability and heterogeneity in the data collected by each of the studies: both in population and follow-up, indications for revision, type of bone defect and measurement of functional results.
Conclusions- -
The use of metaphyseal sleeves is a safe option in complex knee revisions, especially in AORI type 2 and 3 defect.
- -
They are also associated with a very low rate of aseptic loosening, a low reintervention rate and good clinical and functional results (Table 5).
- -
Due to the heterogeneity between the studies, more and higher quality studies are needed to draw definitive conclusions.
Level of evidence II.
FundingThis research study did not receive specific support from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.