Distal femoral fractures represent a problem due to their high number of complications. The aim was to compare the results, complications and stability achieved with retrograde intramedullary nailing and the angular stable plate in the treatment of distal femoral diaphyseal fractures.
Material and methodA clinical and experimental biomechanical study was carried out using finite elements. The results of the simulations allowed us to obtain the main results related to the stability of osteosynthesis. For clinical follow-up data, frequencies were used for qualitative variables, and Fisher's exact test and χ2 test were used to evaluate the significance of the different factors, with the condition of P<.05.
ResultsIn the biomechanical study, the retrograde intramedullar nails demonstrated superiority, obtaining lower values in terms of global displacement, maximum tension, torsion resistance, and bending resistance. In the clinical study, the rate of consolidation of the plates was lower than nails (77% vs. 96%, P=.02). The factor that most influenced the healing of fractures treated with plate were the central cortical thickness (P=.019). The factor that most influenced the healing of nail-treated fractures was the difference between the diameter of the medullary canal and the nail.
ConclusionsOur biomechanical study shows that both osteosynthesis provide sufficient stability, but biomechanically behaves differently. Nails provide greater overall stability being preferable the use of long nails adjusted to the diameter of the canal. Plates form less rigid osteosynthesis, with little resistance to bending.
Las fracturas de fémur distal representan un problema por su elevado número de complicaciones. El objetivo fue comparar los resultados, las complicaciones y la estabilidad conseguidos con el enclavado intramedular retrógrado y la placa de estabilidad angular en el tratamiento de las fracturas diafisarias distales de fémur.
Material y métodoSe realizó un estudio clínico y experimental biomecánico mediante elementos finitos. Los resultados de las simulaciones permitieron obtener los principales resultados relacionados con la estabilidad de la osteosíntesis. En el seguimiento clínico se utilizaron frecuencias en variables cualitativas, y la prueba exacta de Fisher y la prueba Chi cuadrado para evaluar la significación de los diferentes factores, con la condición p<0,05.
ResultadosEn el estudio biomecánico los clavos intramedulares retrógrados demostraron superioridad, obteniendo valores inferiores en cuanto a desplazamiento global, tensión máxima, resistencia a la torsión y resistencia a la flexión. En el estudio clínico la tasa de consolidación de las placas fue inferior a la de los clavos (77% vs. 96%, p=0,02). El factor que más influyó en la consolidación de las fracturas tratadas con placa fue el grosor cortical central (p=0,019). El factor que más influyó en la consolidación de las fracturas tratadas con clavo fue la diferencia entre el diámetro del canal medular y el del clavo.
ConclusionesNuestro estudio biomecánico demuestra que ambas osteosíntesis proporcionan suficiente estabilidad, pero biomecánicamente se comportan de forma diferente. Los clavos proporcionan mayor estabilidad global, siendo preferible el uso de clavos largos y ajustados al diámetro del canal. Las placas forman osteosíntesis menos rígidas, con poca resistencia a la flexión.
Distal femur fractures represent between 4% and 6%1 of femoral fractures and are a problem due to their high number of complications.2 Traditionally, they occurred in young patients due to high-energy trauma, but nowadays they are more frequent in elderly patients, who present with an osteoporotic bone,3 in addition to a large number of comorbidities which makes their treatment difficult.
Treatment options depend on the fracture pattern, the degree of comminution, the surgeon's preference, and the type of patient. The goal is to stabilise the fracture and restore the length and axis of the limb, minimising soft tissue injury as much as possible.4 Since the appearance of the dynamic condylar screw, a material specifically designed for its treatment, many materials and techniques have been described to improve fracture stabilisation and its results. Condylar plates, and more recently angular stability plates, have emerged to improve fracture stabilisation in osteoporotic bone.5
Furthermore, the appearance of the blocked intramedullary nailing (IM) in the 1970s, with excellent results in the treatment of femoral diaphyseal fractures, has led to its retrograde use in extra-articular distal fractures, also with excellent results. They offer the advantage of being performed in a closed focus, minimising soft tissue injury, and favouring the accumulation of the drilling material in the fracture site.6
Despite the different techniques, there are still a significant number of local and general complications. The choice of implant remains under debate.7,8
In clinical studies, samples may not be large enough to obtain statistically significant results due to the large number of variables to be evaluated, but they are necessary to see therapeutic trends. Computational techniques and finite element (FE) simulations are considered a useful tool to reproduce biomechanical behaviour.9 It is the clinical tendencies that set the biomechanical models to be made.
The aim of the study was to compare the biomechanical behaviour in a FE model of osteosynthesis with retrograde IM nailing and angular stability plate in three different fracture types. In addition, we evaluated the factors that influenced healing and complications.
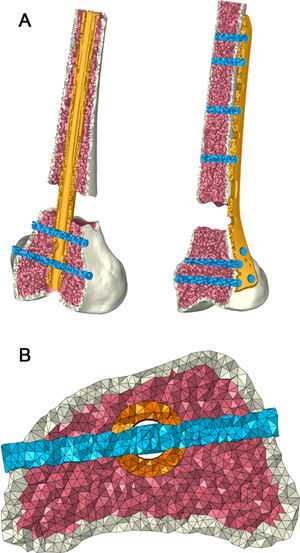
Material and methodComputational studyA three-dimensional (3D) FE model of the femur of a 55year-old male (from the project “Biomechanical and clinical study of centromedullary nailing in the treatment of diaphyseal femoral fractures”) was developed. The geometric model was obtained with the Roland3D Roland® PICZA 3D scanner (Irvine, California, USA), with a resolution of .2mm. Geometric modelling of the nail and plate was performed manually with NX-Ideas (Siemens, Plano, Texas, USA).10 The screws were geometrically modelled as cylinders of the same diameter. The different parts of the assembly were assembled to achieve a replica of the osteosynthesis as accurately as possible, performed under the supervision of a surgeon. Once this process was completed and with each part in its final position, the meshing process began.
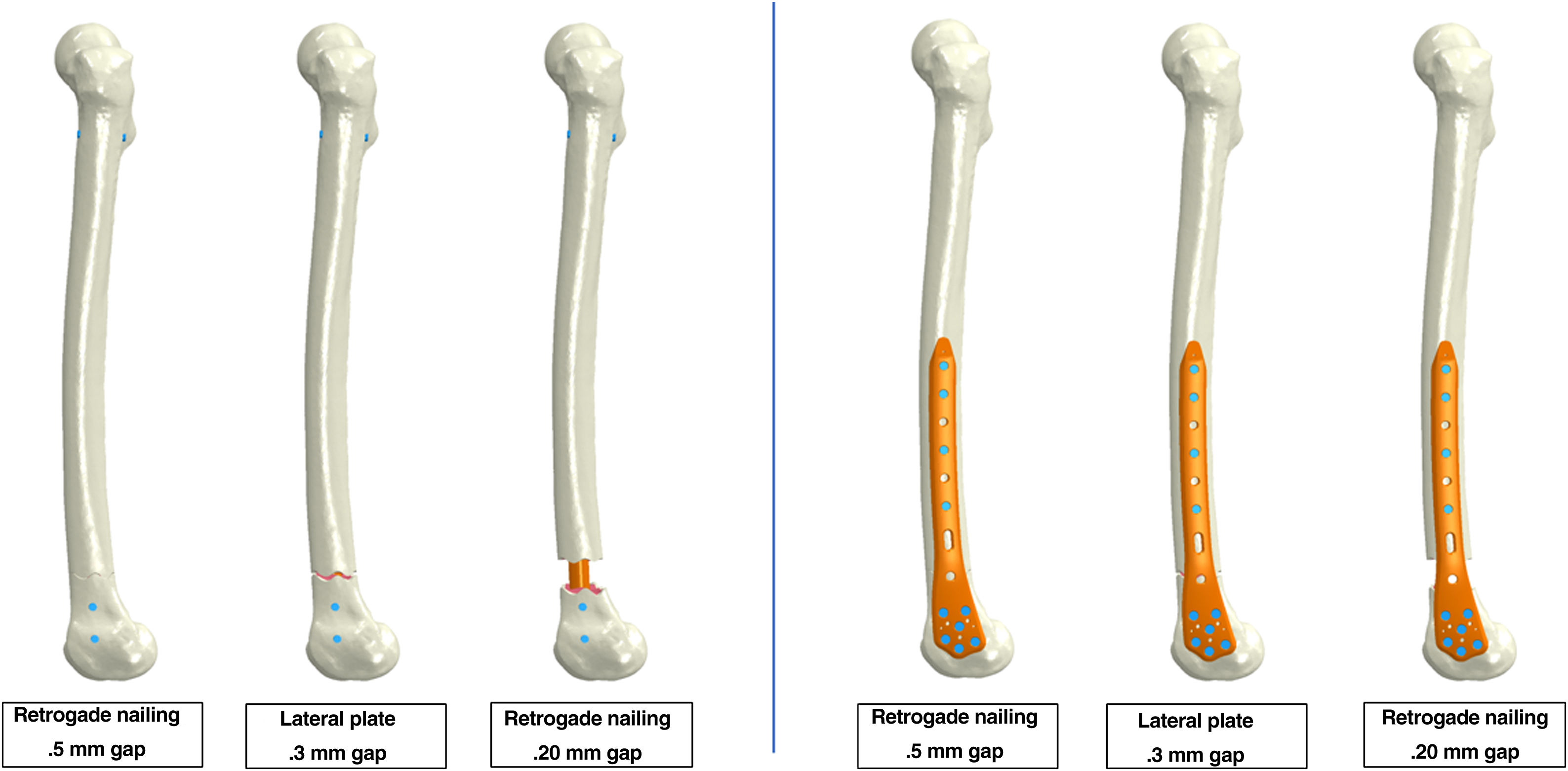
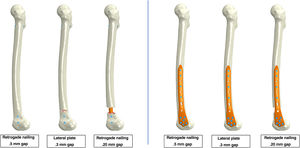
A transverse fracture was modelled in the Wiss11 zone 5, with interfragmentary distances of .5mm (considered as a non-comminuted fracture), 3mm (as the most referenced value in the literature, representing an average value of comminution) and 20mm (as an example of a comminuted fracture) (Fig. 1).
These fractures were treated with the two most widely accepted osteosynthesis models in the literature: the retrograde IM nailing and the angular stability plate. A Stryker S2/T2™ model nail (Stryker, Mahwah, New Jersey, USA) of 13mm diameter, 360mm length and 2mm thickness was used for retrograde IM nailing. The locking screws were 5mm, two proximal anteroposterior screws and two distal lateromedial screws. Three-dimensional geometric models corresponding to the nail and locking screws were generated by hand, being drawn with NX I-deas software (Siemens, Plano, Texas, USA).10 For plate osteosynthesis, the distal femur angular stability plate model LOQTEQ™ (AAP Implantate AG, Berlin, Germany) with a length of 207mm, with 4 proximal bicortical screws and 6 distal screws was used, and the same modelling process was performed.
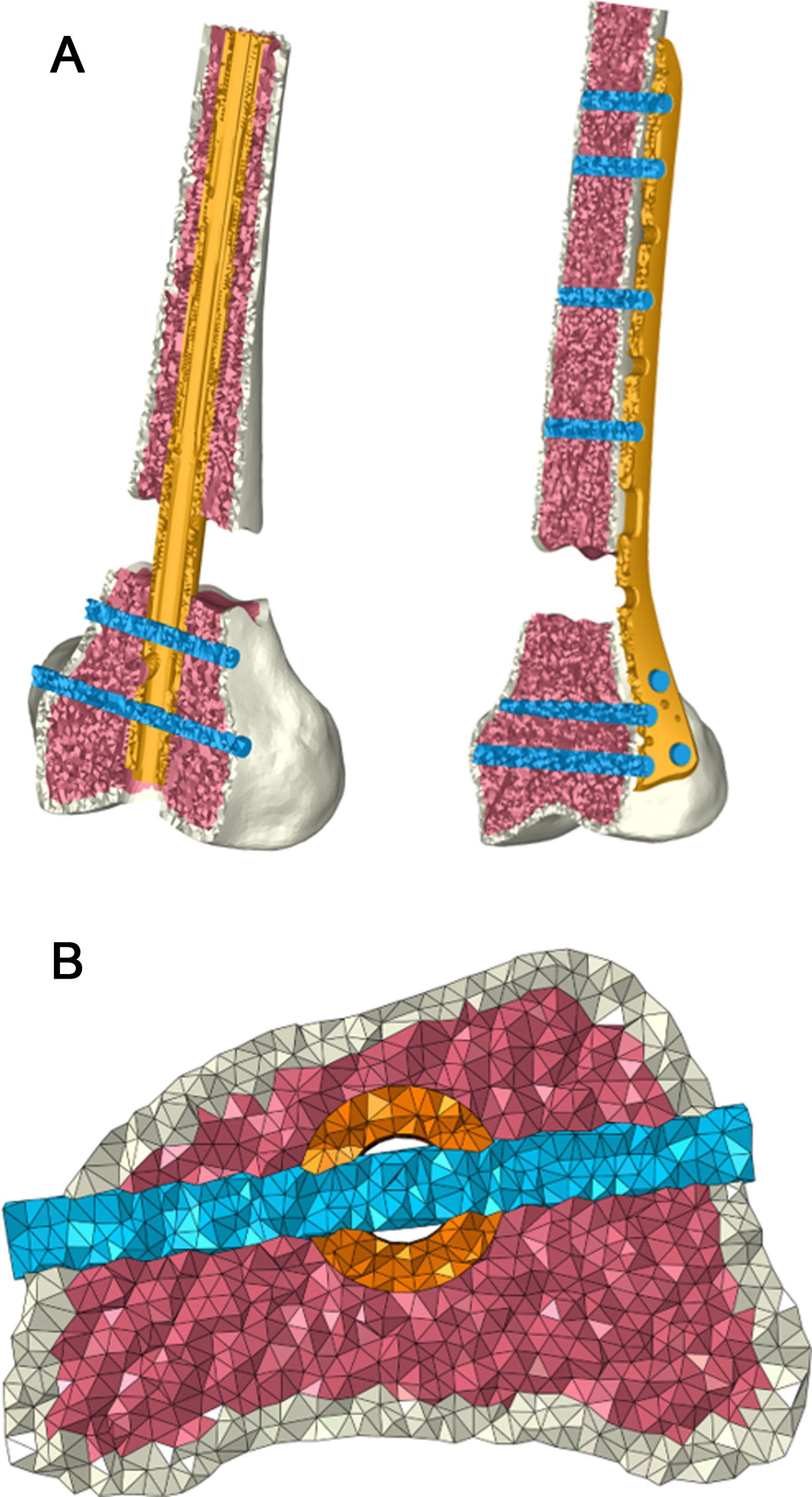
Each part of the FE model was independent, simulating the behaviour of a real osteosynthesis (Fig. 2). The mechanical properties of the different parts, their interactions and the contact conditions between them were defined.
Regarding the mechanical properties, both in the case of nails and plates, the bone was assumed to be linear elastic isotropic, with the following properties:
ECorticalbone=20,000MPa, νCorticalbone=.3; ETrabecularbone=959MPa, νTrabecularbone=.3. For nail and plate, 316 LVM (EStainlessSteel=192.360MPa, νStainlessSteel=.3) and titanium Ti–6Al–4V (ETitanium=113.760MPa, νTitanium=.34), were considered. Both materials were taken to be linearly elastic isotropic.12
As far as the interactions between the different parts of the models are concerned, the corresponding contact conditions were defined, which allow relative movements, but no interpenetrations. The value considered for the coefficient of friction between bone/nail, bone/plate, nail/screws, plate/screws and trabecular bone/screws was .15. The interaction between screws and cortical bone was considered locked, simulating the rigid joint in the thread.
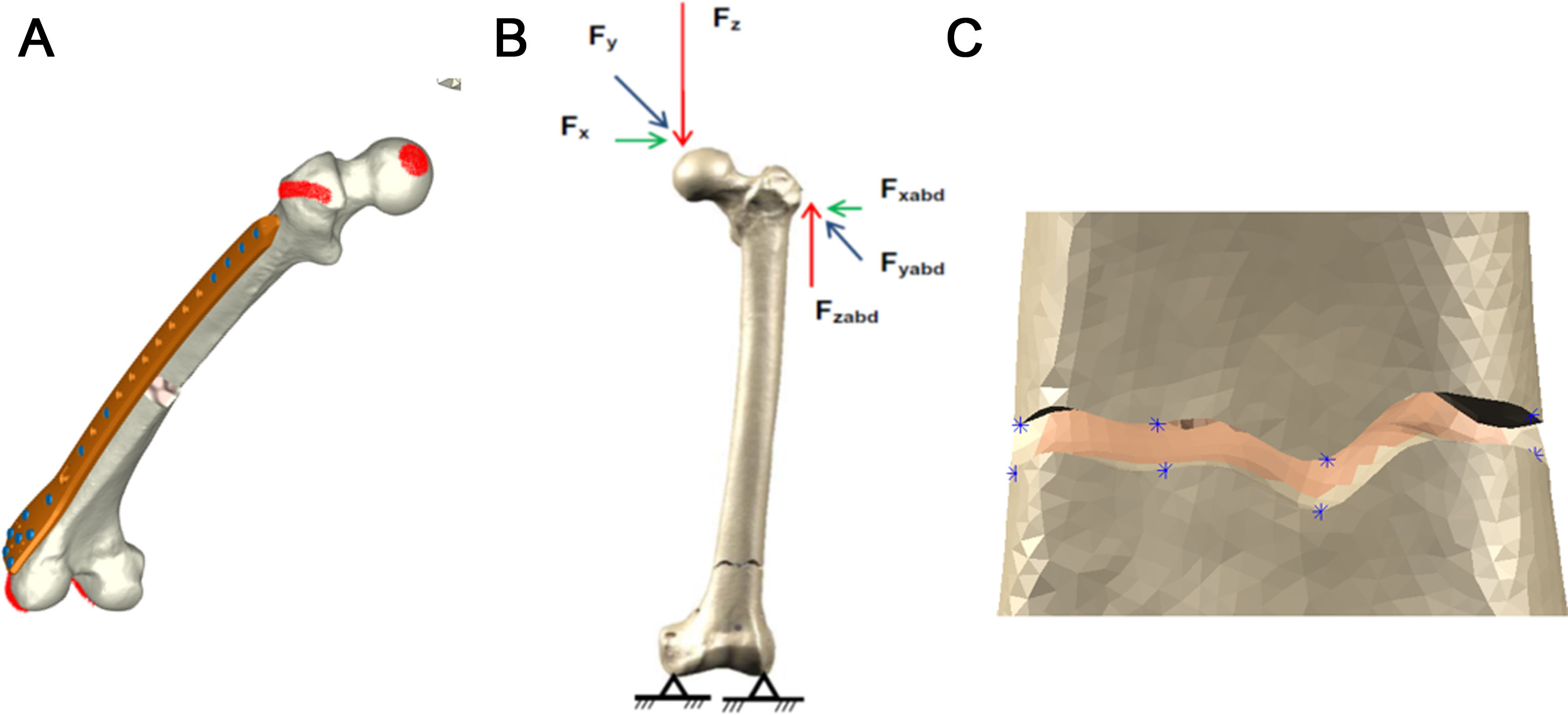
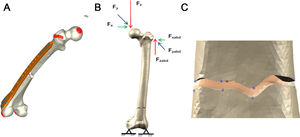
The study focused on the immediate postoperative stage, so no biological healing process was addressed. Accidental loads were considered, being a load equivalent to 10% of the physiological load in healthy models. The results were obtained by measuring the stability of the osteosynthesis (displacement at the femoral head) and the micro-movements at the fracture site, following loads from the hip applied on the femoral head and due to the abductor muscles on the greater trochanter (Fig. 3). Movement in the condylar area was blocked.13 The loading and contour conditions were entered into the respective models. The relative movements at the fracture site are processed by considering working groups of the corresponding nodes located at opposite positions (upper and lower fragment) at the fracture site.12 (Fig. 3c).
The different calculations were made using ABAQUS14 software.
Clinical studyA clinical follow-up was performed, considering a sample of 126 patients (41 males and 85 females) with mean age of 67.5years, all treated for distal femur fracture from 2010 to 2020.
Ninety-five patients were treated using LOQTEQ™ model distal femur angular stability plate (AAP Implantate AG, Berlin, Germany) with a series mean age of 67.52years (28–97), with 32.6% being male and 67.4% female. According to the degree of comminution, 78.9% were non-comminuted and 21.1% were comminuted. According to the type of fracture, 45.3% were transverse, 29.5% oblique and 25.3% spiroid.
Thirty-one patients were treated by Stryker S2/T2™ retrograde IM nailing (Stryker, Mahwah, New Jersey, USA) with a mean age of the series of 67.29years (17–101), 32.3% being male and 67.7% female. According to the degree of comminution, 77.4% were non-comminuted and 22.6% were comminuted. According to fracture type, 22.6% were transverse, 16.1% oblique and 61.3% spiroid. Both samples were comparable.
Exclusion criteria were skeletal immaturity, open fractures, intra-articular fractures, and patients whose follow-up could not be completed. The mean follow-up was 7years.
Factors that may affect healing and complications were evaluated, such as interfragmentary fracture distance, medullary canal diameter, cortical thickness, difference between canal and nail diameter, distance of screws to the fracture site, implant length and type of material.
Clinical healing was defined as the absence of pain at the fracture site and the visualisation of fracture callus in anteroposterior and lateral radiological projections of the femur. Delayed healing was defined by the same criteria as consolidation, but which occurred 9months or more after surgery, without the need for additional surgery (nail dynamisation is not considered surgery). And pseudarthrosis was defined by the need for subsequent surgery due to the absence of consolidation.15
The purpose of the clinical review was to mark the tendences supporting or refuting the biomechanical outcomes.
Qualitative variables were described using observed frequencies and percentages, and continuous variables were described by their means. The primary outcome was the occurrence of pseudarthrosis and complications. Fisher's exact test and the χ2 test were used to assess the significance of independent variables. Statistical data were processed with SPSS software (version 22.0, SPSS Inc, Chicago, Illinois, USA) and significance level was of p<.05.
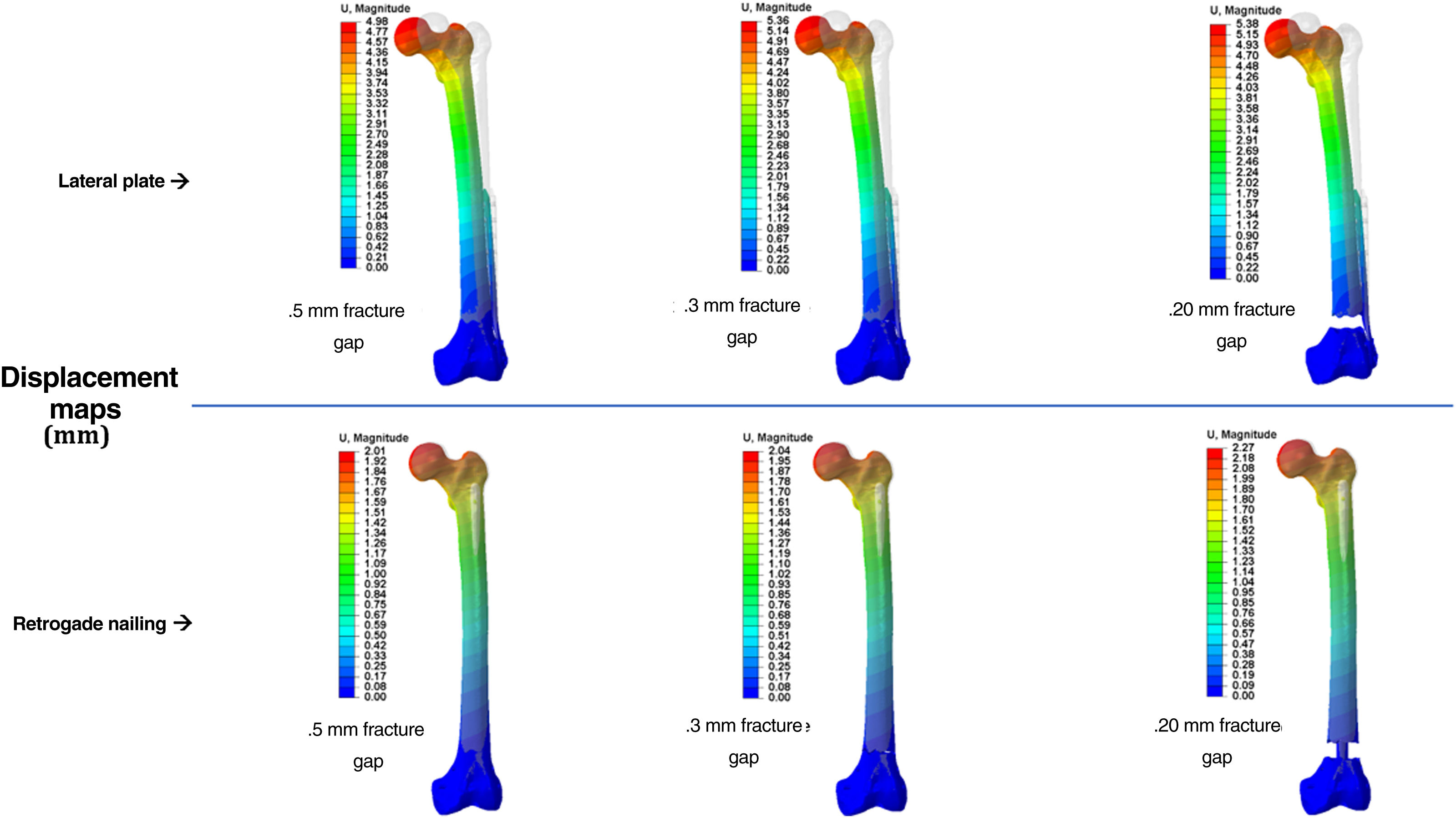
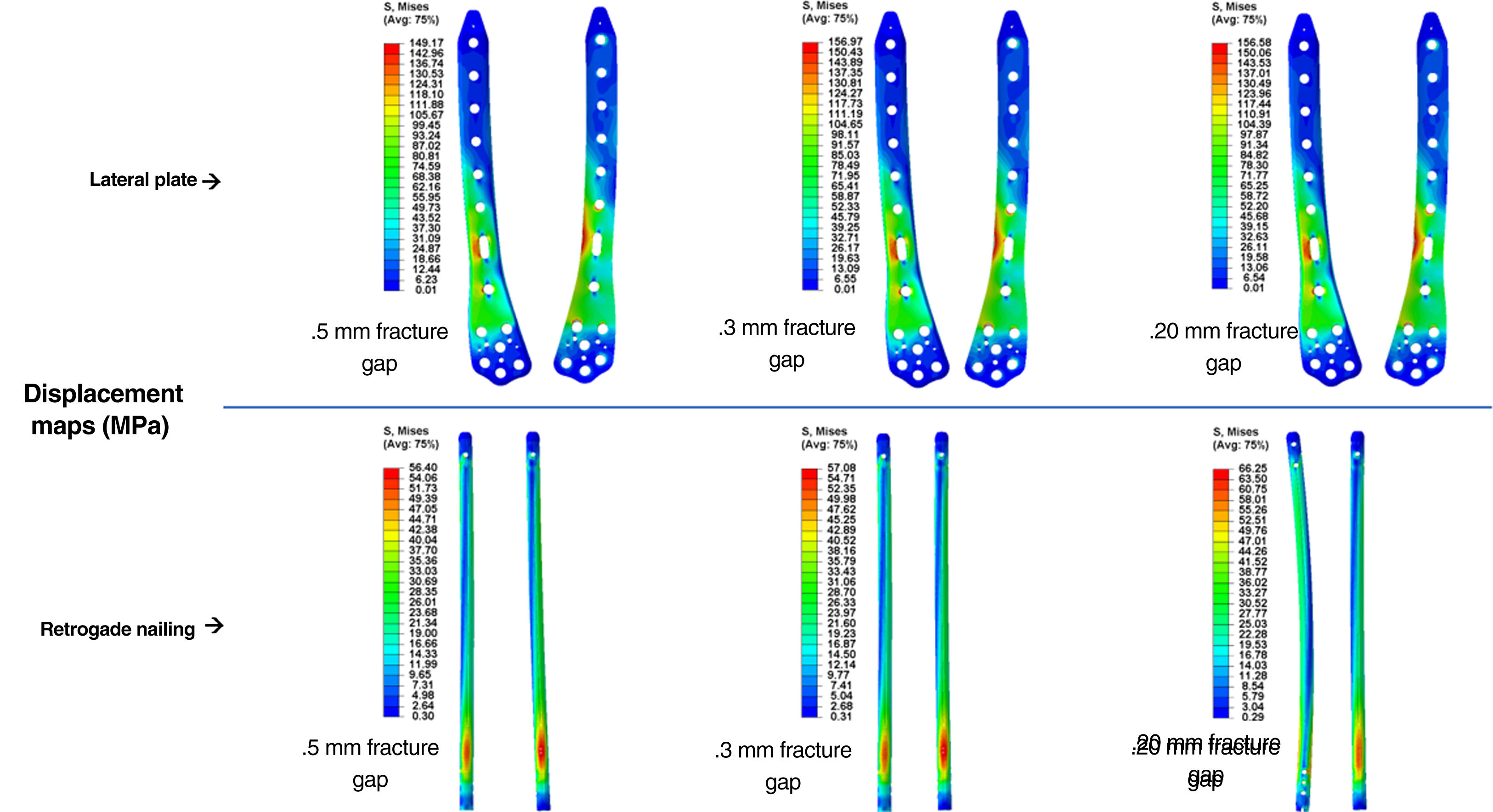
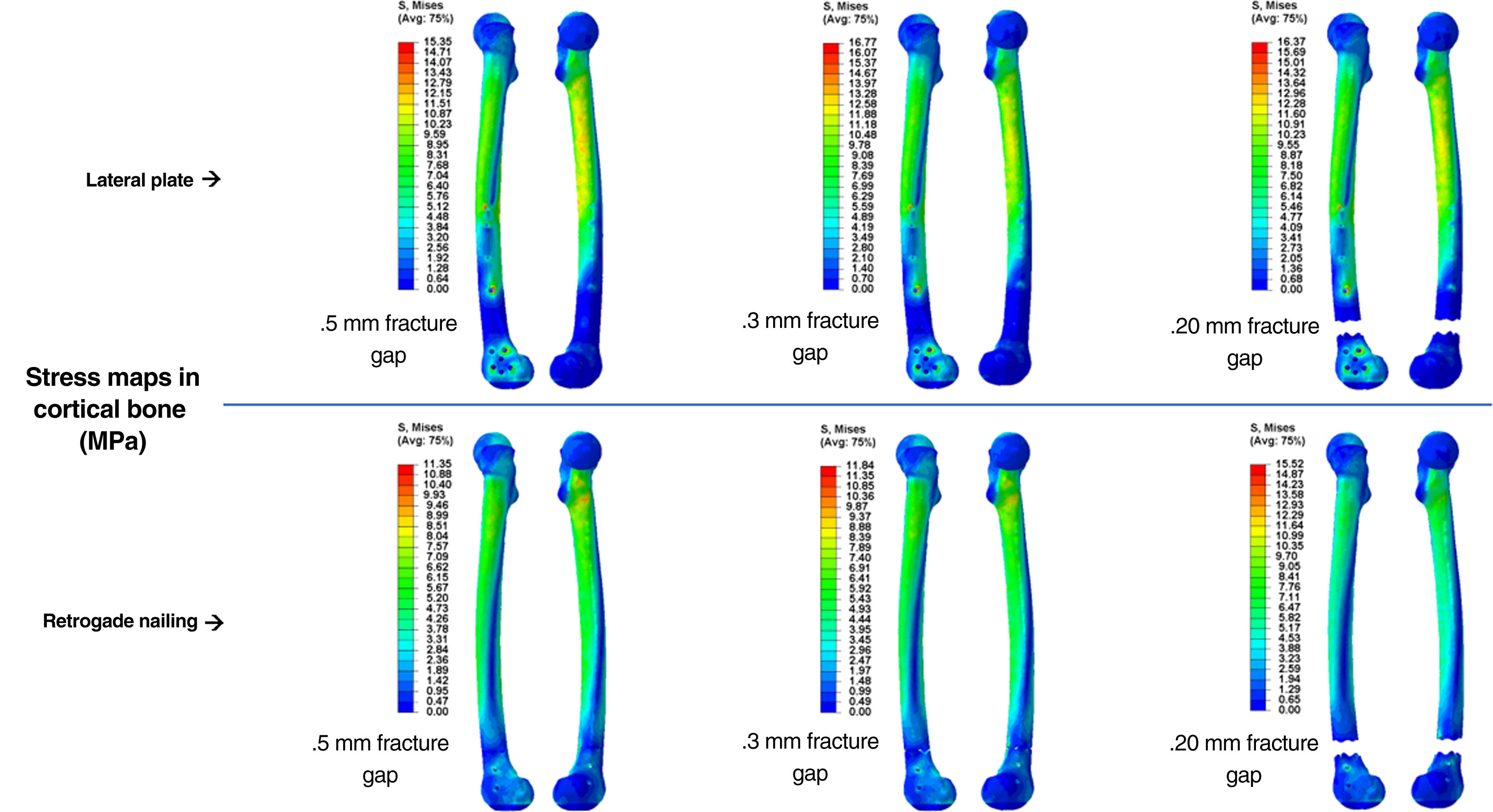
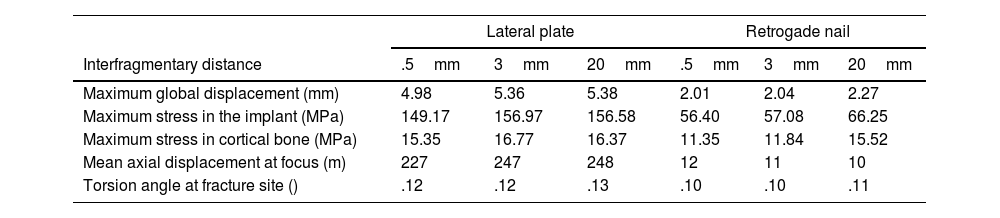
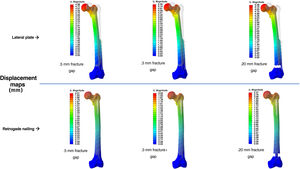
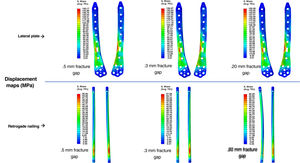
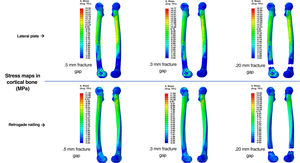
ResultsComputational studyTable 1 shows the values analysed comparing osteosynthesis with plate versus retrograde nailing, for the three interfragmentary fracture distances. We observed that with the plate the maximum global displacement increased by 148%, 136% and 137%, respectively: a displacement about 2.5 times higher than the average (Fig. 4). As for the maximum stress measured in the implant, in the plate it increased by 164%, 175% and 136%, respectively: 2.6 times higher maximum stresses in the plate than in the nail (Fig. 5). The maximum stress measured in the cortical bone increased in the plate by 35%, 42% and 5%, respectively (Fig. 6). The mean axial displacement measured at the fracture site increased by 1.789%, 2.072% and 2.258%, respectively. The mean displacement was about 20 times higher in the plate compared to the nail, with the bending strength being the parameter with the most differences between the two. The angle of rotation at the fracture site increased by 19%, 19% and 16%, respectively, making torsional strength the most similar parameter between the two.
Results of the variables analysed comparing osteosynthesis with plate versus retrograde nailing.
| Lateral plate | Retrogade nail | |||||
|---|---|---|---|---|---|---|
| Interfragmentary distance | .5mm | 3mm | 20mm | .5mm | 3mm | 20mm |
| Maximum global displacement (mm) | 4.98 | 5.36 | 5.38 | 2.01 | 2.04 | 2.27 |
| Maximum stress in the implant (MPa) | 149.17 | 156.97 | 156.58 | 56.40 | 57.08 | 66.25 |
| Maximum stress in cortical bone (MPa) | 15.35 | 16.77 | 16.37 | 11.35 | 11.84 | 15.52 |
| Mean axial displacement at focus (m) | 227 | 247 | 248 | 12 | 11 | 10 |
| Torsion angle at fracture site () | .12 | .12 | .13 | .10 | .10 | .11 |
The consolidation rate for plates was 77%, compared to 96% for nails (p=.02). As for the mean time to consolidation, no differences were found (p=.41): that of the plates was 5.75months and that of the nails, 5.08months.
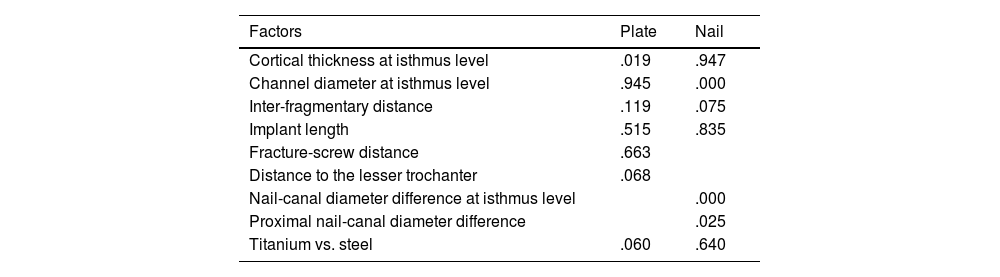
The factors impacting consolidation were studied (Table 2).
Results of the statistical analysis on different factors affecting consolidation (p-values).
| Factors | Plate | Nail |
|---|---|---|
| Cortical thickness at isthmus level | .019 | .947 |
| Channel diameter at isthmus level | .945 | .000 |
| Inter-fragmentary distance | .119 | .075 |
| Implant length | .515 | .835 |
| Fracture-screw distance | .663 | |
| Distance to the lesser trochanter | .068 | |
| Nail-canal diameter difference at isthmus level | .000 | |
| Proximal nail-canal diameter difference | .025 | |
| Titanium vs. steel | .060 | .640 |
In fractures treated with plates, we observed that cortical thickness at the isthmus influenced healing (p=.019). Greater thicknesses obtained better consolidation rates, this difference being statistically significant. Regarding the distance from the end of the plate to the lesser trochanter, we observed that plates whose mean distance to the lesser trochanter was 8cm had better consolidation rates compared to those whose mean distance was 12cm (p=.068). Another factor we studied was the distance between the fracture site and the most distal proximal screw: the greater the distance from the screw to the fracture site, the better the healing rates were, although these differences were not statistically significant (p=.663). And in terms of material, we observed that titanium had better healing rates than steel, although the difference was not significant (p=.06).
In nail-treated fractures we observed that the ratio between the diameter of the medullary canal and the nail, both proximally and centrally, influenced healing (p=.025 and p=.000, respectively). The more adjusted, the better the consolidation rates were. Regarding the interfragmentary distance of the fracture, we observed that the higher the value, the worse the healing, although this difference was not statistically significant (p=.075).
The complication rate of the plates was 16% and that of the nails was 17% (p=.52). Complications of plates were material breakage (5), peri-plate fracture (3), failure of osteosynthesis (3) and death (1). Complications of nails were death (3), periclavicular fracture (1) and infection (1).
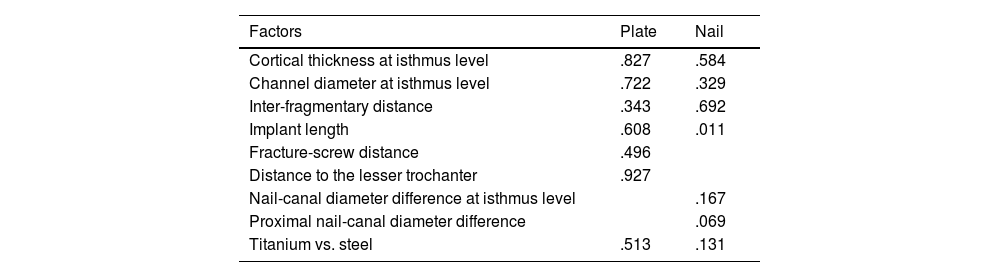
The factors influencing the complications were studied (Table 3).
Results of the statistical analysis on different factors affecting complications (p-values).
| Factors | Plate | Nail |
|---|---|---|
| Cortical thickness at isthmus level | .827 | .584 |
| Channel diameter at isthmus level | .722 | .329 |
| Inter-fragmentary distance | .343 | .692 |
| Implant length | .608 | .011 |
| Fracture-screw distance | .496 | |
| Distance to the lesser trochanter | .927 | |
| Nail-canal diameter difference at isthmus level | .167 | |
| Proximal nail-canal diameter difference | .069 | |
| Titanium vs. steel | .513 | .131 |
In fractures treated with plates, none of the factors studied influenced the occurrence of complications.
In nail-treated fractures, we observed that nail length influenced the occurrence of complications (p=.011). Shorter nail lengths increased the rate of complications (periclavicular fractures).
DiscussionThe choice of the appropriate implant is one of the key factors in achieving adequate stabilisation and load distribution in the bone, with the aim of achieving correct healing and avoiding complications.16
Analysis of the results of the FE models shows that both osteosyntheses provide sufficient stability in the treatment of distal femoral fractures, but biomechanically they behaved differently. The retrograde IM nails demonstrated their superiority, with lower values for maximum global displacement, maximum stress in both implant and cortical bone, mean axial displacement measured at the fracture site and rotation angle at the fracture site. The nails were 20 times superior in flexural strength. However, regarding torsional strength almost no differences were found.
To our knowledge, none of the published papers using FE have comparatively studied the full biomechanical behaviour of the angular stability plate and the retrograde IM nail, in distal femoral diaphyseal fractures, simulating different types of comminution at the fracture site. Work using the FE has focused on the retrograde IM nail. They have studied its biomechanical behaviour17 and stress values according to the number of locking screws and according to the material (steel or titanium). Most of the published biomechanical studies comparing the retrograde IM nail with angular stability plates have used synthetic bone7 or cadaveric models.18,19 Bliemel et al.18 performed an experimental biomechanical study with human bones comparing the stability achieved with both treatments and were unable to reach definitive conclusions on the superiority of either technique. Başcı et al.,19 however, also performed an experimental biomechanical study on cadavers and found greater stability in axial loading in those treated with retrograde IM nailing, as we observed in our study. They also observed that the plates had greater resistance to torsion, unlike our study, but this was the parameter in which both types of osteosynthesis behaved more similarly.
In relation to consolidation, we have observed very different rates between angular stability plate osteosynthesis and retrograde IM nailing. Rodriguez et al.20 studied the results and complications of more than 200 patients treated with an angular stability plate, finding 13% pseudarthrosis, a lower percentage than that found in our sample. However, in the literature, the series show very variable ranges of consolidation, between 71% and 93%.21 Jankowski et al.22 performed a systematic review of databases from the last ten years, finding a mean rate of consolidation with retrograde IM nailing of 93.9%, similar to our sample. Consolidation times were akin to those reported in the literature, around 20weeks, with no differences between the two osteosyntheses.22
In relation to complications, no differences were observed. Griffin et al.23 performed a meta-analysis including seven studies, with a total of 444 patients, finding no statistically significant differences in complications between the two treatments.
In the study of osteosyntheses performed with angular stability plates, clinically we observed that one of the most important factors for consolidation was the cortical thickness at the isthmus level (p=.019). This factor is related to the patient's bone mineral density, so it is difficult to prevent its influence on the consolidation process. There are studies that defend the influence of this factor in the development of hip fracture24 and in interprosthetic fractures.25
Other important factors, although not statistically significant, were the distance from the end of the plate to the lesser trochanter (p=.068), the distance between the fracture site and the most distal proximal screw (p=.663) and the material (p=.06). Rodriguez et al.20 concluded that the most important factor was the material: titanium plates had higher consolidation rates. However, steel plates, short and with all screws implanted, gave great rigidity to the fracture site, favouring consolidation failure. The same results were observed in different studies,26 although the results are always debated, since, although a more elastic assembly, i.e. long plates with screws away from the fracture site, seem biomechanically better for achieving consolidation, consolidation failure still sometimes occurs. In these cases, the treatment consists of making the assembly more rigid, including, according to some authors, implanting an accessory plate medially.27
In the study of osteosyntheses performed with retrograde IM nailing, clinically we observed that one of the most important factors for consolidation was the relationship between the diameter of the medullary canal and the nail, both proximally and centrally (p=.025; p=.000). Several studies on reaming have been published.16 Reaming the canal prior to nail insertion allows proper shaping of the medullary canal, facilitating the use of larger diameter nails, providing more stable osteosyntheses. Its importance in consolidation lies in the mechanical behaviour of the osteosynthesis. The forces applied to the femoral head are transferred to the nail through the contact surface in the medullary canal. The lesser the contact, the greater the overall instability. Good contact between the nail and the canal causes the forces to be evenly distributed, promoting stability and consolidation.28
Insufficient reduction or the presence of space at the fracture site has also been associated with non-union.29 We observed that the greater the distance, the worse the healing rate. Analysing the results of the FE models, it has been found that increasing the interfragmentary distance leads to an increase in the overall instability of the osteosynthesis.
In terms of complications, clinically we observed that the most important factor was nail length. Chantarapanich et al.30 performed a biomechanical FE study of retrograde IM nailing in distal femoral fractures and observed that there is an influence on the stability achieved depending on the length of the nail and the location of the locks, and very little depending on the manufactured material.
We acknowledge that there are some limitations to the study. In biomechanical studies, it is the mechanics which count, the biological part being very difficult to simulate, so that the application of the results to human clinical practice may have certain limitations and must be corroborated with the clinical trends observed. However, biomechanical studies are necessary, because to obtain decisive clinical results, a large number of patients would be necessary, which are not available in normal clinical practice due to the great individual variability and the decrease in the incidence of this type of fracture.
These findings have been produced using a single model of osteosynthesis with nail and plate, a study which has certain limitations, especially regarding osteosynthesis with plate, where the number of variables (length of the plate, number of screws and their proximity to the focus) is much greater than the variables of the nail, which are limited to length and diameter.
The aim of plate osteosynthesis is to achieve sufficient fracture stability, but with a certain point of elasticity. This can be achieved by increasing the number of proximal screws or by bringing them closer to the fracture site. And this is the problem: the biologically most suitable stiffness–elasticity for fracture healing is unknown.
ConclusionsIn conclusion, our biomechanical study demonstrates that both osteosyntheses provide sufficient stability in the treatment of distal femoral fractures, although their behaviour is different. Intramedullary nails provide greater overall stability and achieve a more uniform stress distribution. They stand out for their axial stability, due to their high resistance to bending and compression, as they are located closer to the axis of load, with the use of long nails (up to the lesser trochanter) and adjusted to the diameter of the canal being the preferred choice. As for the lateral plates, they form less rigid osteosynthesis, with little resistance to bending, which generates large axial displacements compared to the intramedullary nail. However, rotational stability is very similar between both types of osteosynthesis.
Level of evidenceLevel of evidence iii.
FundingThe authors declare that they received external funding from the SECOT Foundation for this study. Grant “Proyectos de Iniciación a la Investigación Fundación SECOT”, 2019 (SECOT Foundation Research Initiation Projects, 2019).
Conflict of interestsThe authors have no conflict of interests to declare regarding the study findings.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.