The incidence of osteoporotic vertebral fractures (OVFs) is increasing. The importance of their diagnosis and treatment lies in their frequency and the morbidity they cause in patients.
The classification proposed for OVFs by the German Society of Orthopaedics and Traumatology (DGOU) recommends surgical treatment for vertebral fractures classified as OF4. Most of these fractures will require anterior bracing as an adjunct to posterior fixation because of the significant loss of vertebral body structure.
In elderly patients, minimally invasive surgery (MIS) allows their treatment given the lesser tissue aggression and systemic repercussions. We present the results of the treatment of OF4 vertebral fractures using minimally invasive techniques in the Spine Unit of our hospital.
Material and methodsRetrospective study of 21 patients with OF4 osteoporotic fractures in the thoracolumbar transition treated in our centre. Six patients who underwent open posterolateral fusion or isolated vertebroplasty were excluded. The series consists of 15 cases (13 females and 2 males), with a mean age of 72.2, studied by computed tomography and magnetic resonance imaging. Clinical and analytical data were collected to decide the most appropriate surgical technique.
In six cases a retropleural/retroperitoneal MIS approach was performed for partial corpectomy with expandable vertebral substitute plus long posterior percutaneous fixation (technique 1). In the remaining nine cases long posterior percutaneous fixation+vertebroplasty of the fractured vertebra (technique 2).
Radiological measurements were taken pre-surgically, post-surgically, at 6 weeks and 3 months, determining the fracture angle, kyphotic deformity, compression and wedging percentage and deformation angle.
To assess functional outcome, patients completed the Oswentry Disability Index before surgery and at 3 months.
ResultsThere were no intraoperative complications of note. In the corpectomy group the mean hospital stay was 9.4 days, with a mean operative time of 250min, a postoperative haemoglobin loss of 3.3g/dL and two patients were transfused.
In the percutaneous fixation and vertebroplasty group the mean was 5.55 days, surgery time 71min and loss of 1.6g/dL haemoglobin. There was one post-surgical haematoma requiring transfusion.
None of the patients had to be reoperated during follow-up.
Radiological measurements showed adequate correction with both techniques which was maintained over time with minimal loss.
In functional outcomes assessed with the Oswentry, patients following technique 1 suffered greater worsening (15%) than those treated with technique 2 (10%).
ConclusionsIn OWF classified as OF4, percutaneous fixation associated with vertebroplasty could be an alternative to corpectomy in older patients with comorbidities, in whom functional recovery is more important than radiological correction.
The use of MIS surgery together with improvements in the prevention and treatment of osteoporosis may improve clinical outcomes in the treatment of this type of fracture.
La incidencia de las fracturas vertebrales osteoporóticas está en aumento. La importancia de su diagnóstico y tratamiento radica en su frecuencia y la morbilidad que producen en los pacientes.
En la clasificación propuesta para las fracturas vertebrales osteoporóticas por la Sociedad Alemana de Ortopedia y Traumatología (DGOU) recomienda el tratamiento quirúrgico en las fracturas vertebrales clasificadas como OF4. La mayoría de estas fracturas van a requerir un soporte anterior como complemento a la fijación posterior, por la importante pérdida de estructura del cuerpo vertebral.
En pacientes de edad avanzada, la cirugía mínimamente invasiva permite su tratamiento gracias a la menor agresión tisular y repercusión sistémica. Se presentan los resultados del tratamiento de fracturas vertebrales OF4 mediante técnicas mínimamente invasivas en la Unidad de Raquis de nuestro hospital.
Material y métodosEstudio retrospectivo de 21 pacientes con fractura osteoporótica OF4 en el tránsito toracolumbar tratados en nuestro centro. Han sido excluidos seis pacientes a los que se les realizó fusión posterolateral abierta o vertebroplastia aislada.
La serie se compone de 15 casos (13 mujeres y dos varones), con edad media de 72,2 estudiados mediante tomografía computerizada y resonancia magnética.
Se recogen datos clínicos y analíticos para decidir la técnica quirúrgica más adecuada.
En seis casos se realizó abordaje retropleural/retroperitoneal con cirugía mínimamente invasiva para corpectomía parcial con sustituto vertebral expansible más fijación percutánea posterior larga (técnica 1). En los nueve casos restantes fijación percutánea posterior larga + vertebroplastia de la vértebra fracturada (técnica 2).
Se han realizado mediciones radiológicas prequirúrgicas, posquirúrgicas, a las seis semanas y tres meses, determinando el ángulo fracturario, deformidad cifótica, porcentaje de compresión y de acuñamiento y ángulo de deformación.
Para valorar el resultado funcional los pacientes han respondido el Índice de Discapacidad de Oswentry antes de la intervención y a los tres meses.
ResultadosNo hubo complicaciones intraoperatorias reseñables. En el grupo de la corpectomía la media de ingreso fue de 9,4 días, con un tiempo quirúrgico medio de 250 min, una pérdida de 3,3 g/dL de hemoglobina en el postoperatorio y dos pacientes fueron transfundidos.
En el grupo de fijación percutánea y vertebroplastia la media fue de 5,55 días, tiempo de cirugía de 71 minutos y pérdida de 1,6 g/dL de hemoglobina. Hubo un hematoma posquirúrgico que requirió transfusión.
Ninguno de los pacientes ha tenido que ser reintervenido durante el seguimiento.
Las mediciones radiológicas realizadas mostraron una adecuada corrección con ambas técnicas que se mantuvo en el tiempo con una mínima pérdida.
En los resultados funcionales valorados con el Oswentry, los pacientes que siguieron la técnica 1 sufrieron mayor empeoramiento (15%) que los tratados con la técnica 2 (10%)
ConclusionesEn las fracturas vertebrales osteoporóticas clasificadas como OF4, la fijación percutánea asociada a vertebroplastia podría ser una alternativa a la corpectomía en pacientes de mayor edad y con comorbilidades, en los que prima la recuperación funcional frente a la corrección radiológica.
La utilización de cirugía mínimamente invasiva junto con mejoras en la prevención y tratamiento de la osteoporosis, pueden mejorar los resultados clínicos en el tratamiento de este tipo de fracturas.
The incidence of osteoporotic vertebral fractures (OVFs) continues to increase due to demographic changes and population ageing in the western world.1 It is important that they are diagnosed and treated because they are the most common bone fragility fractures2 and entail significant morbidity3 as they cause kyphosis of the spine from collapse and stenosis of the canal.
The sequelae of OVF seriously affect patients’ basic activities of daily living (BADL) and quality of life, and in the long term impair their walking and physical condition.4
The principles of the treatment of OVF include restoration of spinal stability, correction of the kyphotic deformity, decompression of the neural canal, and early mobilisation. Although conservative treatment has shown satisfactory clinical results, surgical management appears to provide better correction of the deformity and better long-term results.5
Surgery is demanding in elderly patients, due to ageing, associated medical comorbidities, and the increased risk of implant failure caused by osteoporosis.6
The introduction of minimally invasive surgical techniques (MIS) has made it possible to increase the indications for fixation as it achieves comparable results to open surgery, but with less surgical morbidity, as the techniques are associated with shorter surgery time, once the learning curve has been completed, less intraoperative bleeding, less muscle injury and, therefore, enable early rehabilitation.7
In 2018, the German Society for Orthopaedics and Trauma (DGOU) presented a proposal for classifying osteoporotic vertebral fractures, as they were not covered under the usual classifications (AOSpine, Denis, TLICS).8
This classification divides OVFs into 5 types (Fig. 1). It is a simple and visual organisation that allows better classification of the typical patterns of OVF. Following on from this work, they published a series of recommendations for the treatment of each type of fracture.9
Classification of osteoporotic vertebral fractures as proposed by the DGOU.8
OF4 fractures are considered fractures with loss of vertebral frame structure due to comminution, with >50% vertebral body collapse or diabolo or “pincer” type of fracture. These are unstable fractures for which surgical treatment is recommended, which can be isolated posterior fixation or, depending on the characteristics on computed tomography (CT), complemented with anterior support.
The aim of this paper is to review the preliminary results of our series of fractures treated surgically with two types of minimally invasive stabilisation including placement of anterior support.
Material and methodsWe conducted a retrospective descriptive study over one year of patients with OF4 OVFs who underwent minimally invasive surgery in our centre.
Epidemiological data, comorbidities, anaesthetic risk and presence or absence of previous diagnosis of osteoporosis were collected for each patient.
Prior to surgery all the cases underwent CT and magnetic resonance imaging (MRI). CT allows us to classify the fracture according to the OF system,8 assess risk factors for collapse, pedicle morphology, and the extent of occupation of the canal. MRI is used to assess the chronicity of the fracture, the existence of fractures at other levels, spinal cord, disc, or posterior ligament complex involvement, and to confirm the pathological aetiology.
Two minimally invasive techniques were used to treat the fractures surgically:
In younger patients with fewer comorbidities, a retropleural/retroperitoneal MIS approach is performed in lateral decubitus for partial corpectomy of the fractured vertebra and placement of an expandable vertebral replacement following the technique performed by Bordon et al.10; this approach is associated with fewer pulmonary complications compared to the classic transthoracic approach. In the same surgical procedure, the patient is transferred to the prone position for posterior percutaneous fixation two levels above and two levels below (technique 1) (Fig. 2).
68-year-old woman with L1 fracture following a fall from standing. Percutaneous T12-L2 fixation and retropleural corpectomy with vertebral replacement was decided. Preoperative CT images in sagittal and axial sections. Radiographic result with anteroposterior and lateral projections at three months post-surgery.
In older patients with a higher surgical risk, percutaneous posterior fixation in the prone position two levels above and two levels below is preferred in conjunction with vertebroplasty of the fractured vertebra (technique 2) (Fig. 3).
In the postoperative period for technique 1, the patient remains in ICU for the first 24–48h until clinically stable. Mobilisation begins 48h after removal of the urinary catheter and chest drain. In technique 2, the patient is transferred directly to the ward and starts to sit and stand the day after surgery.
Over the period studied, 21 vertebral fractures classified as OF4 were treated. Six patients were excluded from the study: three cases that were treated by open posterolateral fusion and two cases who underwent isolated vertebroplasty.
The last patient to be excluded was due to a change in indication intraoperatively. The initial indication was corpectomy and posterior percutaneous fixation (technique 1), but when the expandable vertebral replacement was placed, a vertebral plate ruptured, requiring rescue rib strut palisade graft and open posterolateral fusion to increase stability.
The radiological measurements used to assess the sagittal deformity produced by the fracture, the correction made with the surgical intervention and how it progressed over time were (Fig. 4):
- •
Fracture angle: angle between the upper plateau of the vertebra above the fracture and the lower plateau of the vertebra below the fracture.
- •
Kyphotic deformity: angle between the upper plateau of the vertebra above the fracture and the lower plateau of the vertebra below the fractured vertebra.
- •
Compression percentage (Beck's index): ratio between the height of the anterior wall of the fractured vertebra and the posterior wall of the fractured vertebra, multiplied by 100.
- •
Wedging percentage: ratio between the height of the anterior wall of the fractured vertebra and the anterior wall of the vertebra below the fracture, multiplied by 100.
- •
Deformation angle: angle formed by the intersection of the line following the posterior wall of the vertebrae above the fracture with the posterior wall line of vertebrae below the fracture.
The Oswentry Disability Index was used to assess the patients’ functional result. Radiological and functional results were obtained preoperatively and at three months.
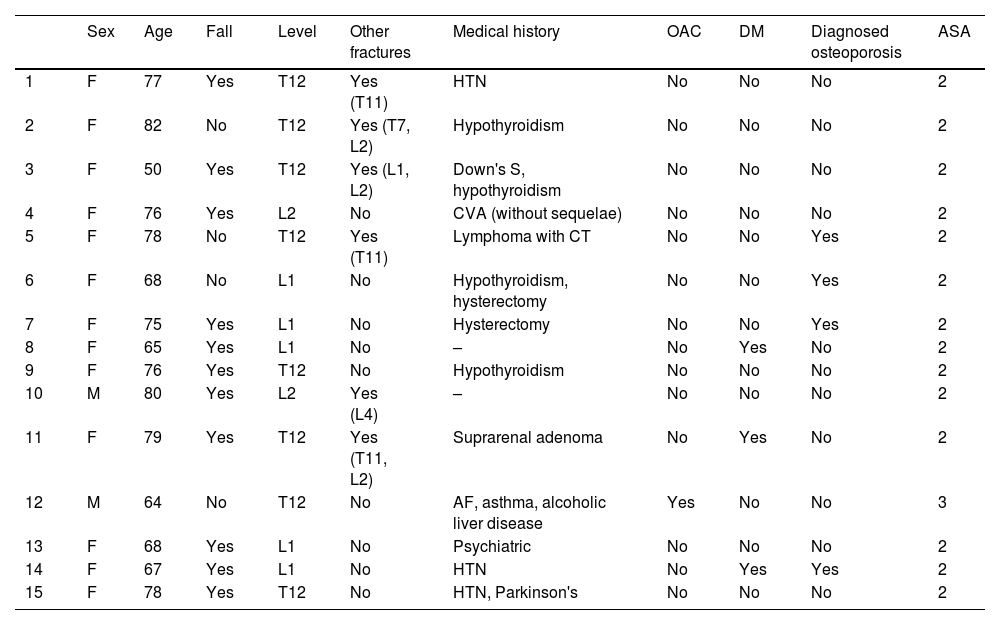
ResultsFifteen patients (13 females and two males) were included in the study, with a mean age of 72.2 years. Table 1 details the clinical and epidemiological information collected.
Patients’ clinical data. Patients treated with technique 1 shaded.
| Sex | Age | Fall | Level | Other fractures | Medical history | OAC | DM | Diagnosed osteoporosis | ASA | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 77 | Yes | T12 | Yes (T11) | HTN | No | No | No | 2 |
| 2 | F | 82 | No | T12 | Yes (T7, L2) | Hypothyroidism | No | No | No | 2 |
| 3 | F | 50 | Yes | T12 | Yes (L1, L2) | Down's S, hypothyroidism | No | No | No | 2 |
| 4 | F | 76 | Yes | L2 | No | CVA (without sequelae) | No | No | No | 2 |
| 5 | F | 78 | No | T12 | Yes (T11) | Lymphoma with CT | No | No | Yes | 2 |
| 6 | F | 68 | No | L1 | No | Hypothyroidism, hysterectomy | No | No | Yes | 2 |
| 7 | F | 75 | Yes | L1 | No | Hysterectomy | No | No | Yes | 2 |
| 8 | F | 65 | Yes | L1 | No | – | No | Yes | No | 2 |
| 9 | F | 76 | Yes | T12 | No | Hypothyroidism | No | No | No | 2 |
| 10 | M | 80 | Yes | L2 | Yes (L4) | – | No | No | No | 2 |
| 11 | F | 79 | Yes | T12 | Yes (T11, L2) | Suprarenal adenoma | No | Yes | No | 2 |
| 12 | M | 64 | No | T12 | No | AF, asthma, alcoholic liver disease | Yes | No | No | 3 |
| 13 | F | 68 | Yes | L1 | No | Psychiatric | No | No | No | 2 |
| 14 | F | 67 | Yes | L1 | No | HTN | No | Yes | Yes | 2 |
| 15 | F | 78 | Yes | T12 | No | HTN, Parkinson's | No | No | No | 2 |
AF: atrial fibrillation; CT: chemotherapy; CVA: cerebrovascular accident; DM: diabetes mellitus, F: female; HTN: hypertension; L: lumbar; M: male; OAC: oral anticoagulation; T: thoracic.
In 11 cases the fracture was caused by falls from standing, and in the remaining cases it was not related to a history of trauma. Six patients presented other vertebral fractures at the time of admission: they were chronic fractures in three of the cases, and synchronous injuries in the other three. Only five patients had been previously diagnosed with osteoporosis, one of the cases with previous fractures, and the rest had no history of fracture. It was noted that most of the patients with previous fractures had not been diagnosed with osteoporosis and were not receiving treatment.
Technique 1 (corpectomy) was performed in six patients, with a mean surgery time of 250min, and a postoperative loss of 3.3g/dL haemoglobin. No serious intraoperative complications were reported. Postoperatively there were two cases of urinary tract infection and two patients had to be transfused. The mean hospital stay was nine days.
Technique 2 (vertebroplasty) was selected for the other nine cases, with a mean surgery time of 71min, and a loss of 1.6g/dL haemoglobin. No intraoperative complications were recorded. In the postoperative period, there was one case of severe subcutaneous haematoma that led to the patient becoming anaemic and requiring transfusion. In this group only two patients were transfused, and the mean hospital stay was five days.
Radiological resultsThe mean fracture angle in the corpectomy group was 29.52° preoperatively, with correction to 54° in the immediate postoperative period, 10.22° at six weeks, and 14.52 at three months. In the vertebroplasty group it was 17.2° preoperatively, with correction to 7.4° in the immediate postoperative period, 12.39° at six weeks, and 14.45° at three months (Fig. 5a).
The initial sagittal index in the corpectomy group was 17.48°, 1.22° at the immediate postoperative control, 1.12° at six weeks, and 2.12° at three months. In the vertebroplasty group the initial angulation was less, 13.83° and the correction achieved was 9° with an immediate postoperative index of 4.51°, at six weeks it remained at 4.82°, and at three months it was 5.32° (Fig. 5b).
The compression percentage or Beck's Index was 35.24% preoperatively in the corpectomy patients, and 79.88% after surgery, 71.16% at six weeks, and 62.9% at three months. In the vertebroplasty group, at the time of the fracture, the compression rate was 42%, and 69.45% after surgery. At six weeks it was 63.6%, and at three months 57.64% (Fig. 5c).
The wedging percentage showed a similar course to that of compression. In the corpectomy group the pre-surgical rate was 27%, 74.98% in the immediate post-surgical period, 69.58% at six weeks, and 68% at three months. Those who underwent vertebroplasty had a mean preoperative rate of 37.27%, after surgery the rate was 63.58%, 57% at six weeks, and 53.54% at three months (Fig. 5d).
The initial deformity angle in the corpectomy group was 22.25°, 9.62° after surgery, 11.47° at six weeks, and 16.6° at three months. In the vertebroplasty group it initially measured 17°, immediately postoperatively it was 8.81°, at six weeks it was 13.19°, and at three months 17.63° (Fig. 5e).
Functional resultsIn the group that underwent corpectomy, the Oswentry disability index prior to the vertebral fracture was 31.05%, at three months after surgery it was 46.07%. In the vertebroplasty group, the initial score was 20.06%, and at three months post-surgery it was 30.77%.
DiscussionOVFs have been treated classically with bed rest, analgesia and bracing due to the advanced age of the patients, who are often not candidates for operations that are long or involve excessive bleeding, and due to the technical difficulties in anchoring the pedicle screws because of underlying osteoporosis.11
Today's society has an increasingly ageing population with active lifestyles and high functional demands, who require better results after the treatment selected. Increasing numbers of fractures are being treated surgically due to the satisfactory results of less invasive techniques such as vertebroplasty and percutaneous fixation with screws, among others.6
The indication for percutaneous fixation with pedicle screws is supported by the fact that in comparative studies of thoracolumbar burst fractures,5 fracture fixation without posterior facet fusion had satisfactory clinical and radiological results similar to those of patients who underwent posterior fusion, with less blood loss, shorter surgery time and the ability to maintain the mobility of the segment once the instrumentation had been removed.
Vertebroplasty has been widely used to treat osteoporotic vertebral compression fractures due to its rapid pain relief, but it is not without problems such as loss of vertebral height with worsening regional kyphosis, neurological compression caused by cement leakage and secondary fractures.11 Kim et al. note in their series that progressive loss of vertebral height after vertebroplasty is inevitable despite good initial results.12
Both techniques can be used in isolation or in combination in the same patient. Li et al. compared a series of patients with osteoporotic fractures treated with isolated vertebroplasty with another series of patients with vertebroplasty and subsequent percutaneous fixation, observing similar clinical-radiological results at up to three months of follow-up, with a significantly higher rate of complications in the percutaneous fixation group. However, at six months, the patients with isolated vertebroplasty had significant loss of height and increased kyphosis, and were less satisfied with the surgical outcome.13
Fractures classified as OF4 generally require solid anterior support to avoid the residual kyphosis described in vertebroplasty series. Despite the fewer complications observed with the MIS retropleural approach,10 an alternative is required to avoid surgical morbidity of corpectomy in older patients with more comorbidities.
In our series, patients treated with vertebroplasty, and percutaneous screws (technique 1) had 50% less bleeding on average, much less need for transfusion and shorter surgery time. These differences are explained by the greater technical complexity of corpectomy. Hospital stay was also shorter, and therefore vertebral body filling with cement may be a less harmful alternative for patients with OF4 fractures and comorbidities, or very old patients with potentially higher surgical risk.
The mean age of our patients was 72.2 years, older than that of most of the literature consulted, and 90% of the patients were female. This high female representation is common in most studies and reflects the higher incidence of osteoporosis in the elderly female population compared to men.
The radiological measurements used show that the patients who underwent technique 1 had a greater initial deformity as measured by both the kyphotic angle and compression percentage. Therefore, in our series, a greater kyphotic angle or a lower compression percentage seems to be radiological determining factors in indicating a corpectomy.
The mean correction in the immediate postoperative period was slightly higher with technique 1. We agree with other authors that corpectomy results in better biomechanical restoration of the spine.14
In both groups, the correction was maintained at six weeks with minimal loss of correction. And at three months, which is the last assessment in this study, the corrections were maintained with satisfactory results in both groups. This suggests that both alternatives can be valid in the treatment of OF4 fractures.
In terms of functional outcomes, the ODI does not reflect subjectively observed results. The corpectomy group had a higher initial value than the vertebroplasty group (31.05% compared to 20.06%). This is due to the presence in the group who underwent the first technique of a patient with Down's syndrome who already had severe previous disability. Given that this is a very small group of patients (six), such a disparate result increases the mean altering the absolute results.
The 15% worsening after surgery with technique 1 and 10% worsening after technique 2 may reflect that the patient is still in recovery given the series’ poor outcomes. The Food and Drug Administration considers that clinical change starts at a difference of 15 points after spinal surgery.15
The radiological results, shorter hospital stay and less bleeding support technique 2 for OF4 fractures in older patients or those with major comorbidities, over technique 1, because they produce a similar correction with less surgical morbidity. Our series is limited by the number of cases and progression time.
We should highlight that only four patients in the series were previously diagnosed and treated for osteoporosis, and in three cases there was a previous vertebral fracture, two of whom had not received any preventive treatment, which is evidence of the under-diagnosis and under-treatment of this disease. Clearly there is a need for improvement in the management and follow-up of patients with osteoporosis.11
After an exhaustive review of the literature, we did not find many publications on MIS treatment in osteoporotic vertebral fractures, and we found very little use of the OF classification8 compared to the AO classification of traumatic fractures.16 This review of our cases is the start of a line of work for the development of a prospective multicentre study of minimally invasive treatment of osteoporotic fractures.
ConclusionIn OVFs classified as OF4 that require anterior support, percutaneous fixation associated with vertebroplasty could be an alternative to corpectomy in older patients with many comorbidities, for whom functional recovery is more important than meticulous correction of radiological parameters.
We believe that the use of MIS in these patients, together with improvements in the prevention and treatment of osteoporosis, will improve the clinical results in the treatment of this type of fracture.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Presented as a poster at the 35th Conference of the Spanish Spine Society (GEER), which was held virtually on 3, 4 and 5 June 2021.