Diaphyseal forearm fractures in skeletally immature patients are common injuries that account for 30% of upper extremity fractures in this age group. There are cases with unstable injuries or unacceptable reductions, in which surgical resolution by reduction and stabilisation with percutaneous elastic endomedullary nailing is indicated. One of the advantages of this system is that it avoids an approach to the fracture site, allowing closed reduction in the vast majority of fractures. However, it is not always possible to achieve an acceptable closed reduction and opening of the fracture site is necessary. The aim of this study was to determine whether there are preoperative factors to predict the difficulty of performing closed reduction in these patients.
MethodsA retrospective study of skeletally immature patients with acute diaphyseal forearm fractures treated with elastic endomedullary nailing by the same paediatric surgeon was performed. The primary outcome variable was defined as the need for open reduction; considered as a direct surgical approach to the fracture site. Demographic characteristics of the included patients and radiographic characteristics of the fracture were analysed.
ResultsWe found that the median percentage of preoperative radial shortening in the closed reduction and open reduction groups was 1 and 5%, respectively; resulting in a statistically significant difference (p = 0.04).
ConclusionRadial shortening on preoperative radiographs predicts an increased risk of requiring an open reduction of the fracture (39% association); thus we understand that this variable should be considered by the general traumatologist as a prognostic factor in defining the referral of these patients.
Las fracturas diafisarias de antebrazo (FDA) en pacientes esqueléticamente inmaduros son lesiones comunes que representan el 30% de las fracturas de la extremidad superior en este grupo etario. Existen casos con lesiones inestables o reducciones inaceptables, en los cuales está indicada la resolución quirúrgica mediante la reducción y estabilización con clavos endomedulares elásticos (CEE) por vía percutánea. Una de las ventajas que ofrece este sistema es evitar un abordaje del foco de fractura, pudiendo realizar la reducción de forma cerrada en la gran mayoría de estas. Sin embargo, no siempre es posible lograr una aceptable reducción cerrada y entonces es necesaria la apertura del foco de fractura. El objetivo de este estudio fue determinar si existen factores preoperatorios para predecir la dificultad de efectuar una reducción cerrada en estos pacientes.
MétodosSe realizó un estudio retrospectivo de pacientes esqueléticamente inmaduros con FDA agudas, tratados con CEE por el mismo cirujano pediátrico. La variable de resultado primaria se definió como la necesidad de llevar a cabo una reducción abierta; considerado como un abordaje quirúrgico directo en el sitio de fractura. Se analizaron las características demográficas de los pacientes incluidos y las radiográficas de la fractura.
ResultadosEncontramos que la mediana del porcentaje del acortamiento del radio preoperatorio en los grupos de reducción cerrada y reducción abierta fue del 1 y 5%, respectivamente; resultando en una diferencia estadísticamente significativa (p = 0,04).
ConclusiónEl acortamiento del radio en las radiografías preoperatorias permite predecir un aumento del riesgo de requerir una reducción abierta de la fractura (39% de asociación); por lo cual, esta variable debe ser considerada por el traumatólogo general como un factor pronóstico para definir la derivación de estos pacientes.
Diaphyseal forearm fractures (DFF) in skeletally immature patients are common injuries that account for 30% of upper extremity fractures in this age group.1 Distribution is bi-modal, with maximum incidence in patients aged between five and nine years and between 10 and 14 years.2 Closed reduction followed by immobilisation with brachial-palmar moulded cast is currently the gold standard for the treatment of the majority of DFF,3 with excellent long-term outcomes.4,5 The relevant remodelling capacity presented by patients with open growth plates means that reductions with mild angular deformities or mild reductions may be tolerated, depending on age and fracture location.6
In DFF cases with unstable or unacceptable reductions, surgical resolution is indicated7,8 using reduction and stabilisation with percutaneous elastic endomedullary nailing (EEN).9–12 One of the advantages of this system is that it avoids fracture site approach, resulting in closed reduction in the vast majority of cases. However, an acceptable closed reduction is not always possible and opening of the fracture site is needed.2,9,12 Furthermore, numerous attempts at closed reduction may lead to undesirable complications, such as compartment syndrome, that may have devastating effects on the extremity if not diagnosed and treated in time.13,14
Up until now there have been no published works that take into account the initial radiographic displacement as a preoperative predictor for open reduction of DFF in the paediatric population. As a result, the aim of this study was to determine whether preoperative factors exist which could be analysed, to predict the difficulty in carrying out a closed reduction in skeletally immature patients with DFF, and therefore make a referral in keeping with treatment complexity.
Materials and methodOn approval by the hospital ethics committee a retrospective study was conducted. Data were collected from the registers in the electronic medical records. We included skeletally immature patients (14 years of age of under) with acute DFF who were candidates for surgical resolution7,8 with reduction and stabilisation with percutaneous EEN due to unstable or unacceptable reductions. All the patients were treated in our hospital between 2012 and 2017 by the same paediatric surgeon (MHP). Patients were defined as skeletally immature when there were open physes in the radiographic study in both radius and ulna. We excluded sub-acute lesions (over three weeks since the trauma), fractures with associated lesions, Galeazzi or Monteggia, and pathological fractures.
The primary variable was defined as the need for open reduction, considered as a direct surgical approach at the fracture site. Demographic characteristics such as age, gender, body mass index (BMI) and comorbidities were recorded.
Treatment protocolInitially, all patients with forearm fractures were treated by on call professionals where they were immobilised with a brachial-palmar cast. If, due to the magnitude of displacement the fracture required closed reduction, the patient was taken to surgery and this procedure was performed under general anaesthesia and radioscopic control. After this, the patients were quickly referred (within 48 h) to the paediatric surgeon for monitoring or for planning definitive treatment if satisfactory reduction had not been obtained. The definitive surgery was performed under general anaesthesia with the patient relaxed. The fracture was stabilised using EEN. The surgeon initially attempted reduction indirectly without approaching the site and threading the fracture with the EEN. If this was not achievable in the first two attempts or the soft tissues were visibly swollen, a small dorsal approach at fracture site level was chosen and reduction was achieved under direct viewing. In this case prior to approach, a haemostatic tourniquet was placed at arm level to facilitate viewing.
For analysis the patients were divided into two groups: those who required open reduction of the fracture site to achieve appropriate reduction (open reduction) and those for whom a satisfactory reduction was achieved indirectly or closed (closed reduction).
Radiological evaluationDFF were classified in keeping with the paediatric AO classification system. Preoperative radiographic evaluation was made with anteroposterior and lateral X-rays of the forearm, and were assessed blindly by three researchers. The radius and ulna were analysed separately. The radial, ulnar, dorsal and volar angulation were assessed, in coronal and sagittal planes. Interfragmentary diaphyseal overlap and bone shortening were also measured in both planes. Since we did not have witnessed radiographs to scale them to actual size, a percentage ratio was applied for the evaluation of bone shortening, which was defined by any magnitude above 1 mm of bone overlap, dividing the length of the radiographic overlap by the sum of the fragment longitude (Fig. 1).
Profile X-ray of a left forearm with diaphyseal fracture of both bones. (A) Measurement of the distal fragment length. (B) Measurement of the proximal fragment length. (C) Measurement of the overlap length of fragments A and B. The percentage ratio between the length of C over the sum of A and B must be made. If the result for the radius bone is greater than 5%, we consider that the patient would have a 39% higher risk of requiring open surgery.
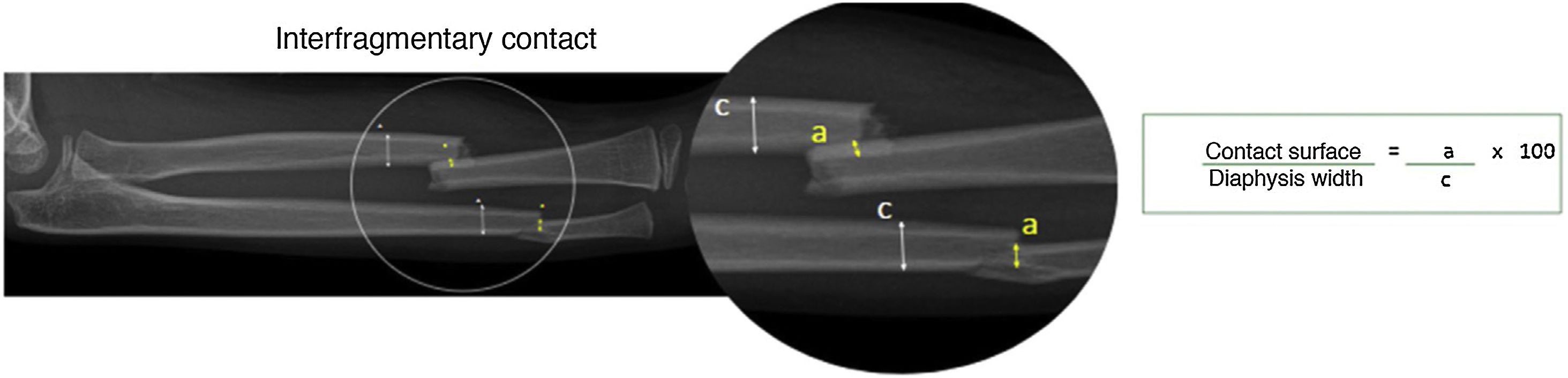
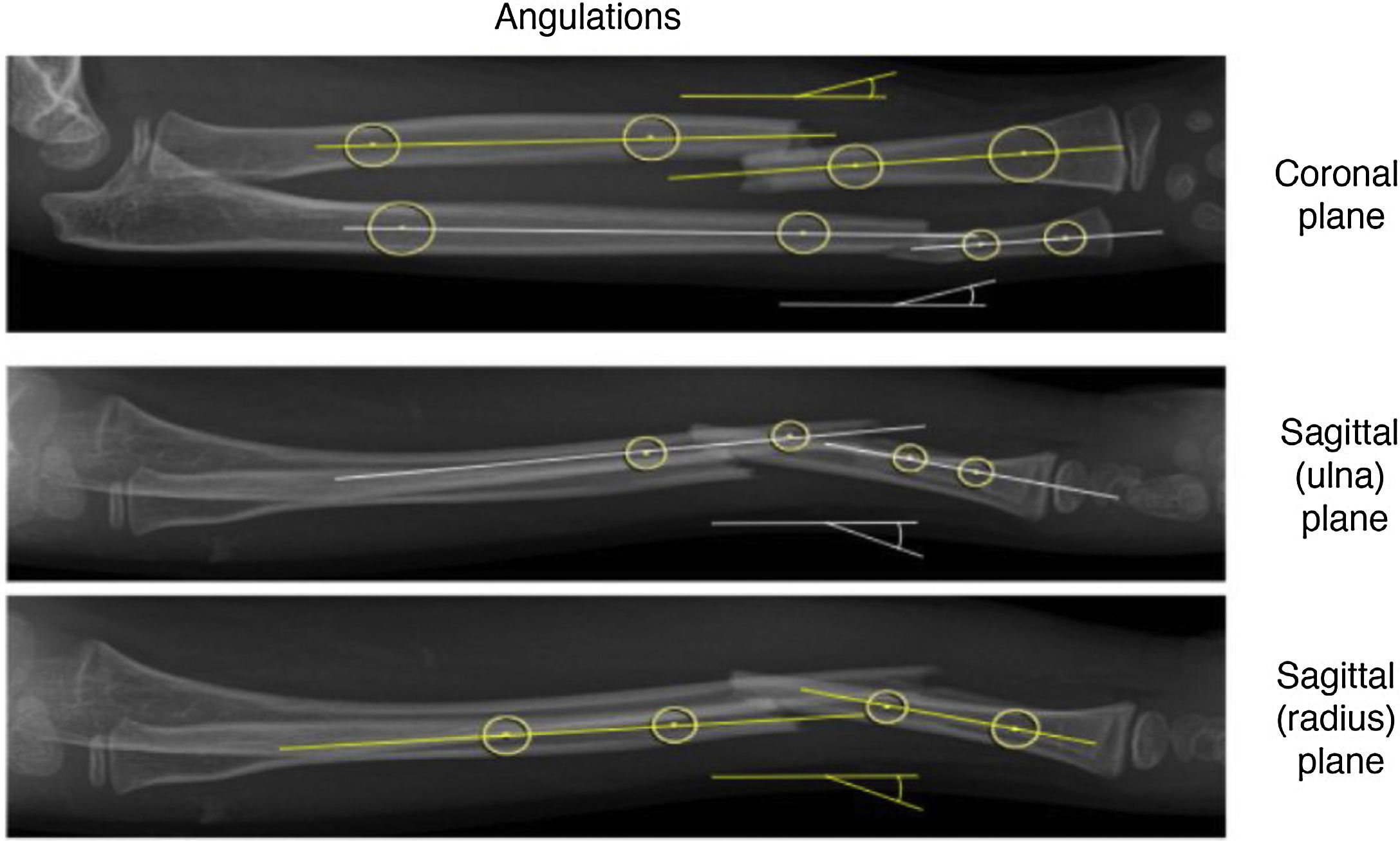
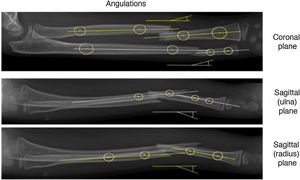
With the same anterior criteria, the interfragmentary diaphyseal overlap was defined as a percentage ratio between the diaphyseal width overlap of the fragments involved (radiographic plane that shows less overlap) (Fig. 2). The angulation degree was measured in both planes as the result of perpendicular lines through the anatomical axis of each bone fragment (Fig. 3).
Anteroposterior X-ray of a left forearm focused on the diaphyseal fracture region of both bones. (A) Measurement of the diaphyseal overlap between proximal and distal fragment. (B) Measurement of the width of intact bone diaphysis as close as possible to fracture site. The percentage ratio between A and C should be made. The result of our series showed that this measurement is not associated with significant differences that define the type of subsequent surgery.
Profile X-rays, 1 anteroposterior and 2 of a left forearm with diaphyseal fractures of both bones. The fragment angulations should be measured tracing the longitudinal axis of each proximal fragment and by measuring the angle from measurements of the longitudinal axis according to its corresponding distal fragment.
Continuous variables are presented as median with interquartile range. Categorical variables are presented as proportions. Normality was reviewed for continuous variables and the existence of extreme values for ordinal and categorical quantitative variables. The Student’s t-test was used for continuous variables. For categorical variables the X2 or Fischer test were used, depending on variable distribution. Open reduction-associated risk factors were assessed with the logistical regression model. Crude and adjusted odds ratios were presented with their confidence interval and p value. We considered p values below .05 as statistically significant. All statistical analyses were performed using Stata 13 Software.
ResultsThirty-seven patients met with the inclusion criteria. Six of them were excluded from the final analysis because no preoperative radiographic assessment could be made due to incorrect radiographic technique. Thirty-one of the patients were included in the final evaluation, with a mean age of 11 years (five women). Thirteen required open reduction (OR) prior to stabilisation with EEN (OR group), whilst the remaining 18 could be treated with closed reduction (CR) (CR group). The single trace, pattern 22-A3.2 according to the AO/OTA classification was the most common, amounting to 71% of the total, with a similar distribution in both groups. Twenty-four patients presented with both bones affected, whilst in the other (seven) patients only the radius was compromised. Single bone involvement had no statistical significance towards either group.
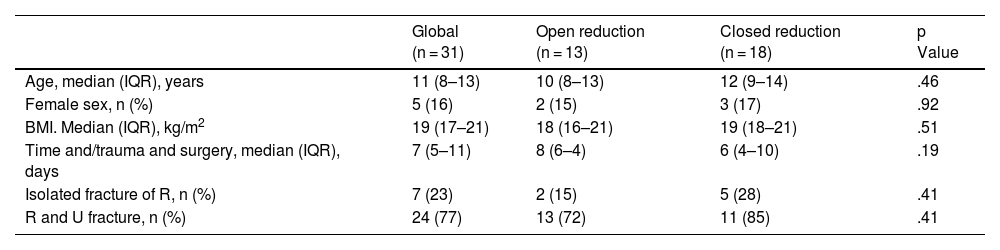
Neither did we find any statistically significant findings between the two groups with regard to age, gender, BMI or time between lesion and surgery. Only two of the patients presented with comorbidities, one with pyelonephritis and another with a respiratory sinus arrhythmia. Both only required closed reduction (Table 1).
Demographic and general fracture characteristics.
| Global (n = 31) | Open reduction (n = 13) | Closed reduction (n = 18) | p Value | |
|---|---|---|---|---|
| Age, median (IQR), years | 11 (8–13) | 10 (8–13) | 12 (9–14) | .46 |
| Female sex, n (%) | 5 (16) | 2 (15) | 3 (17) | .92 |
| BMI. Median (IQR), kg/m2 | 19 (17–21) | 18 (16–21) | 19 (18–21) | .51 |
| Time and/trauma and surgery, median (IQR), days | 7 (5–11) | 8 (6–4) | 6 (4–10) | .19 |
| Isolated fracture of R, n (%) | 7 (23) | 2 (15) | 5 (28) | .41 |
| R and U fracture, n (%) | 24 (77) | 13 (72) | 11 (85) | .41 |
BMI: body mass index; IQR: interquartile range; R: radius; U: ulna.
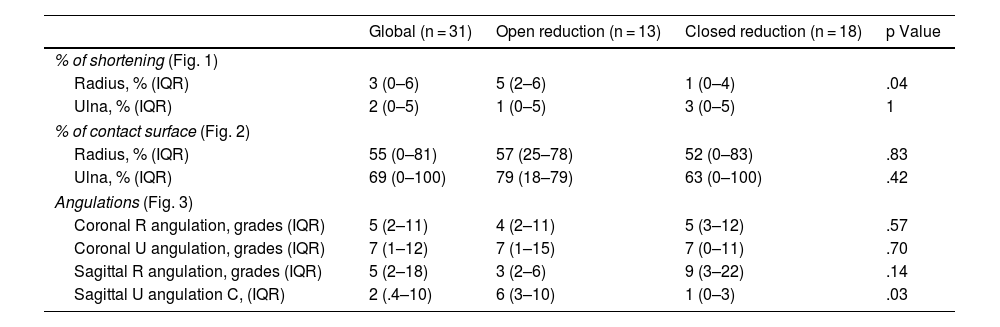
With regard to the radiographic variables analysed, we found that the median percentage of preoperative radius shortening in the CR and OR groups was 1% and 5%, respectively. This resulted in a statistically significant difference (p = .04). The other radiographic variables examined and described in the corresponding section presented with a symmetrical distribution without showing any significant differences between the two groups (Table 2).
Radiographic variables.
| Global (n = 31) | Open reduction (n = 13) | Closed reduction (n = 18) | p Value | |
|---|---|---|---|---|
| % of shortening (Fig. 1) | ||||
| Radius, % (IQR) | 3 (0–6) | 5 (2–6) | 1 (0–4) | .04 |
| Ulna, % (IQR) | 2 (0–5) | 1 (0–5) | 3 (0–5) | 1 |
| % of contact surface (Fig. 2) | ||||
| Radius, % (IQR) | 55 (0–81) | 57 (25–78) | 52 (0–83) | .83 |
| Ulna, % (IQR) | 69 (0–100) | 79 (18–79) | 63 (0–100) | .42 |
| Angulations (Fig. 3) | ||||
| Coronal R angulation, grades (IQR) | 5 (2–11) | 4 (2–11) | 5 (3–12) | .57 |
| Coronal U angulation, grades (IQR) | 7 (1–12) | 7 (1–15) | 7 (0–11) | .70 |
| Sagittal R angulation, grades (IQR) | 5 (2–18) | 3 (2–6) | 9 (3–22) | .14 |
| Sagittal U angulation C, (IQR) | 2 (.4–10) | 6 (3–10) | 1 (0–3) | .03 |
IQR: interquartile range; R: radius; U: ulna.
Bold indicates statistical significance (p < .05).
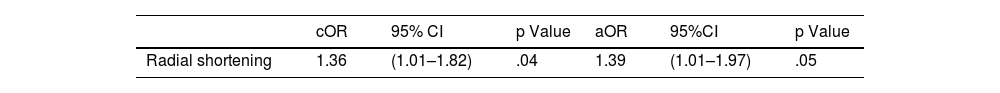
Following multivariate analysis, radius shortening remained as the only preoperative radiographic factor as a predictor of the need to perform open reduction (adjusted odd ratio = 1.39). The patients with over 5% radial shortening were associated with an increase of 39% probability of requiring an open reduction (Table 3).
Univariate and multivariate analysis for the radial shortening variable as predictor of open reduction of forearm fracture.
| cOR | 95% CI | p Value | aOR | 95%CI | p Value | |
|---|---|---|---|---|---|---|
| Radial shortening | 1.36 | (1.01–1.82) | .04 | 1.39 | (1.01–1.97) | .05 |
aOR: adjusted odds ratio; CI: confidence interval; cOR: crude odds ratio.
Bold indicates statistical significance (p < .05).
Open reduction is still the gold standard treatment for DFF among the paediatric population.3 When DFF is unstable or irreducible, one of the most commonly used therapies is reduction (closed or open depending on complexity) and stabilisation with percutaneous EEN.15 The EEN provides shorter operation times, better cosmesis and ease of osteosynthesis removal compared with plate osteosynthesis.12
However, closed reduction is not always possible as an acceptable fracture reduction. Current series show rates of open reduction of up to 60% in some studies.13,16–19 Our series presented with a rate of 41%, with the shortening of the radius the only prognostic preoperative factor for difficulty in performing closed reduction in skeletally immature patients with DFF.
In their 2017 study Makki et al.9 showed that involvement of one bone increased the risk of open reduction compared with the fracture of both. Prior to our study, this finding was the only prognostic factor for open reduction described in the medical literature. In our series, the involvement of only one bone was not a factor associated with the need for open reduction. We understand that this may have been due to the low sample size. However, we consider that the Makki study did not make a variable adjustment for confounding, which could have affected the final result.
In 2017, Lu et al.20 conducted a prospective study comprising 88 paediatric patients with DFF treated by specialised paediatric and orthopaedic surgeons. The authors found there was a significant difference between both groups in terms of open reduction rates. Although functional result and fracture consolidation were similar, in their samples, the specialised orthopaedic surgeons had a lower rate of open reduction compared to the non specialised group. To avoid a selection error, in our series, we only included procedures performed by surgeons specialising in paediatric orthopaedics with experience in treating DFF, thereby minimising possible biases related to the surgeon’s experience.
We are aware of the limitations of this study. Due to its retrospective nature, some of the X-rays examined did not present with an appropriate technique for their analysis, resulting in a considerably reduced final sample. However, although there appears to be a low number of patients, we believe it is a homogeneous cohort, treated by the same highly experienced surgeon specialising in paediatric orthopaedics and a patient series with appropriate follow-up, radiographic evaluation and statistical analysis.
Awareness of prognostic factors is highly useful when choosing treatments for a pathology. It also helps us to foresee and avoid undesirable complications during treatment. Plain, reproducible radiographic analysis, such as that of radius shortening, for which no special knowledge on fracture classifications and their subtypes is required, may be of great use to the surgeon who is assessing the X-rays of a patient with DFF. When there is significant shortening of the radius and it is possible the patent may require more complex surgery than is standard, such as open reduction and stabilisation with EEN, we believe it is of utmost importance to investigate these particular cases.
ConclusionOur results show that, in the presence of a DFF in skeletally immature patients, plain and reproducible analysis such as measuring the shortening of the radius in preoperative radiographies facilitates prediction of the increased risk of requiring open reduction of the fracture (39% of association). As a result this variable must be considered as a prognostic factor to define the referral of a patient with DFF.
Level of evidenceLevel of evidence: III.
FinancingThis study did not receive any type of financing.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Brandariz RN, Esteves TA, Cafruni VM, Abrego MO, Bosio ST, Puigdevall MH. El acortamiento del radio como factor limitante para la reducción cerrada en fracturas de antebrazo pediátrico. Rev Esp Cir Ortop Traumatol. 2022;66:16–21.