The total knee arthroplasty (TKA) has been shown to be a successful and cost-benefit procedure in terms of pain improvement in patient with symptomatic knee osteoarthritis. However, almost a 20% of the patients are not satisfied with the result of the surgery.
Material and methodWe have carried out a transversal unicentric cases controls study with clinical cases of the own hospital, obtained by a clinical records revision. A total of 160 patients with a TKA with at least 1 year of follow-up were selected. Demographic variables, functional scales (WOMAC and VAS) and rotation of the femoral component through the analysis of the images obtained by CT scan were collected.
ResultsThe total was 133 patients that was divided in two groups. A control group and pain group. The Control group was made up of 70 patients with a mean age of 69.59 years (23 men and 47 women) and the pain group was made up of 63 patients with a mean age of 69.48 years (13 men and 50 women). We didn’t find difference regarding the analysis of the rotation of the femoral component. In addition, we were not found significant differences when applying a stratification by sex. And, the analysis of the malrotation of the femoral component, previously defining limits of value rotation considered as extreme, in any of the case did not show significant differences.
ConclusionThe results of the study confirm that malrotation of the femoral component had no influence on the presence of pain at a minimum of one year of follow-up after TKA implantation.
La artroplastia total de rodilla ha demostrado ser un procedimiento exitoso y coste-efectivo en cuanto a la mejoría del dolor en pacientes con artrosis de rodilla sintomática. Sin embargo, en torno a un 20% de pacientes no está satisfecho con el resultado de la intervención.
Material y métodosRealizamos un estudio transversal de casos y controles, unicéntrico con casos hospitalarios, obtenidos mediante la revisión de historias clínicas. Se seleccionaron 160 pacientes portadores de artroplastia total de rodilla con un seguimiento mínimo de un año. Se registraron variables demográficas, escalas funcionales (WOMAC y EVA) y la rotación del componente femoral mediante análisis de imágenes obtenidas por TC.
ResultadosLa muestra final estuvo compuesta por 133 pacientes divididos en grupo control formado por 70 pacientes, con una edad media de 69,59 años (23 hombres y 47 mujeres) y grupo dolor formado por 63 pacientes, con una edad media 69,48 años (13 hombres y 50 mujeres). No encontramos diferencias en cuanto al análisis de la rotación del componente femoral. Tampoco hubo diferencias significativas al aplicar una estratificación por sexo. El análisis de la malrotación del componente femoral, definiendo unos límites de valor de rotación considerados como extremos, no mostró diferencias significativas en ninguno de los casos.
ConclusiónLos resultados del estudio confirman que la malrotación del componente femoral no tuvo influencia sobre la presencia de dolor a un mínimo de un año de seguimiento tras la implantación de una artroplastia total de rodilla.
Total knee arthroplasty (TKA) represents a major advance in the treatment of refractory chronic knee joint pain due to the significant benefits in terms of quality of life and improved functionality. Primary knee osteoarthritis is the most frequent diagnosis associated with TKA implantation. Other causes are rheumatoid arthritis, post-traumatic osteoarthritis and, less frequently, dysplasias and tumours, among others.
TKA is the procedure of choice in patients with chronic pain in whom conservative treatment has failed.1 During 2009, around 662,000 TKA were implemented, and an exponential increase of 855% has been estimated from 2012 to 2030.2
About 20% of patients are not satisfied with the result of the intervention due to the presence of pain. This percentage of dissatisfied patients remains constant despite the evolution of implants.3,4 The causes of pain are multiple. However, once the known causes that could cause it have been ruled out, we are faced with a non-negligible percentage of patients with pain of unknown origin, representing 7–11.5% of TKA revisions.2,5
Many authors have studied the influence of rotational positioning of prosthetic components as a cause of anterior knee pain. In several publications it has been shown that excessive internal rotation of the femoral and/or tibial component had an influence on the stability of the TKA, on the patellar path and, ultimately, on the pain and failure of the TKA.6–8 Excess external rotation of the femoral component has also been related to poor outcome of TKA due to the presence of flexion instability.
For this reason, we studied the influence of femoral component rotation on the aetiology of pain after TKA.
The hypothesis of our study is that malrotation of the femoral component increases the presence of pain after TKA implantation.
Material and methodsA single-centre, cross-sectional case–control study was carried out by selecting patients with implanted TKAs with a minimum follow-up of one year. Depending on the presence or absence of pain, according to pre-established criteria, the patient became part of the pain group or the control group.
The inclusion criteria for the pain group were: pain greater than 3 according to the visual analogue scale (VAS), score on the Score Modified Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)9 less than 70, having undergone surgery through the implantation of a TKA, due to femorotibial osteoarthritis.
The inclusion criteria for the control group were VAS less than or equal to 3, WOMAC9 score higher than 70, and having undergone TKA implantation for femorotibial osteoarthritis.
Exclusion criteria were defined as early postoperative complications that required reintervention, the sudden onset of pain while being asymptomatic after TKA implantation, the existence of a clinical and/or radiological suspicion of infection, aseptic loosening, prosthetic instability, fracture or patellar complications (necrosis, fracture, loosening).
Demographic and radiological variables (study with plain X-ray and a CT scan following the protocol established jointly with the radiodiagnosis service) were collected for each patient.
The measurement of rotation of the femoral component was performed using the technique described by Berger et al.10 Analysis of the rotation of the prosthetic components by CT was carried out by two independent radiologists. To analyse the concordance between the results obtained by both radiologists, we calculated the intraclass correlation coefficient.
Rotation of the femoral componentRotation of the femoral component is defined as the angle between the transepicondylar axis (TEA) and the posterior bicondylar axis. To draw the axes, an axial image of the distal femur was selected where the medial epicondylar groove was represented, if it was visible, or the central point of the medial epicondyle and the lateral epicondyle, and a line was drawn between these two selected points (which corresponds to the surgical epicondylar axis). A second line was drawn, between the posterior part of both condyles of the prosthesis, the posterior bicondylar line of the prosthesis. The angle between these two lines corresponds to the rotation of the femoral component (Fig. 1).
To identify whether the femoral component was in internal or external rotation the following was used:
- •
The posterior condylar angle measured on CT.
- •
The native medial posterior condylar angle specific to each gender. In men the mean posterior condylar angle is 3.5° (with a standard deviation [SD] of 1.2°) of internal rotation, and in women, .3° (SD 1.2°) of internal rotation.11 The femoral component was considered to be in neutral rotation when it was internally rotated 3.5° in men and .3° in women with respect to surgical TEA.
We therefore obtained two values for femoral rotation:
- •
The value measured without applying any correction, which we call femoral component (F).
- •
The value corrected by gender which we call the corrected femoral component (Fc).
Quantitative variables were described as mean, SD and range. Qualitative variables were described using frequencies.
Comparisons between quantitative variables were carried out using non-parametric tests. For the qualitative variables, Chi-square (χ2) tests were performed.
Odds ratios (OR) were calculated for both qualitative and quantitative variables.
In the variables that we consider qualitative, the following considerations were made:
- •
Femoral component: 0 was set at 0° of rotation.
- •
Corrected femoral component (Fc): 0 was set according to gender. In men it was set at 3.5° of internal rotation and in women, at .3° of internal rotation.
The other variables were considered quantitative, since they were the result of the addition or subtraction of rotation values.
The intraclass correlation coefficient (ICC) was used to analyse interobserver agreement for measurements of rotation of prosthetic components on CT.
To define the malrotation of the prosthetic components, the 10th and 90th percentiles of the different study variables of the control group were calculated and collected as extreme rotation values. Subsequently, patients who were below P10 and above P90 in both groups were evaluated.
ResultsOne hundred and sixty patients with TKA were selected from the reference population of the Parc Taulí University Hospital in Sabadell. All of them were evaluated by an expert knee surgeon who assessed whether they met the inclusion/exclusion criteria, had signed an informed consent, filled out the questionnaires (WOMAC and VAS), underwent a physical examination and were scheduled for a CT scan. Of the 160 patients selected, 13 did not meet the inclusion criteria after completing the questionnaires and 14 did not perform the CT scan. These included 3 who met the requirements for the pain group and 11 for the control group. The reasons for the losses were refusal to perform the test or failure to attend the appointment (Fig. 2).
The sample consisted of 97 women (72.9%) and 36 men (27.1%), with a mean age of 69.53years (SD 4.47 [49–84]). Sixty-eight left knees (51.1%) and 65 right knees (48.9%) were included. There were only significant differences in the VAS (p<.001) and WOMAC (p<.001) variables. The other variables did not show significant differences.
To assess interobserver agreement, the ICC was calculated, the purpose of which is to determine the degree of agreement of observations by different observers. In this study, agreement was a measure of consistency, since we did not perform a comparison with a gold standard.12
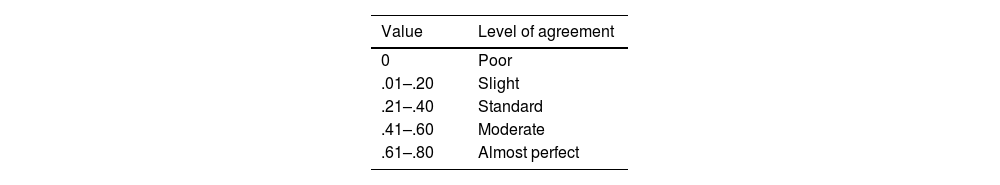
The level of agreement was measured using the Landis and Koch scale, which classifies the results as shown in Table 1.13
The ICC results were as follows: for both femoral rotation and corrected femoral rotation (Fc), the ICC was .801, with an upper limit of .728 and a lower limit of .855, reaching a substantial degree of agreement and, therefore, a strong consistency in the interobserver agreement of the different measurements.
Figs. 3 and 4 show the graphic representation of the interobserver agreement measurements for the femoral component and the femoral component corrected for gender (Fc).
Table 2 shows the results of the analysis of the rotation of the prosthetic components.
Component rotation.
| Control group | Pain group | Differences (°) | p | OR (IC) | |
|---|---|---|---|---|---|
| Femoral comp. | .28° (1.97) [−5.46–4.76°] | .09° (1.80) [−3.54–4.67°] | .19 | .567 | .793 (.391–1.606) |
| Corrected femoral comp. (Fc) | −.76° (2.64) [−8.96–3.92°] | −1.23° (2.47) [−6.95–4.37°] | .47 | .289 | .658 (.330–1.310) |
Mean (SD) [range].
We can highlight a tendency towards internal rotation of the femoral component without significant differences between groups (p=.567), as well as a tendency towards external rotation of the corrected femoral component without differences between groups (p=.289). In both cases, there was a greater tendency towards external rotation in the pain group.
The OR values found for each of the variables showed that there was no relationship between the rotation of the different components and the presence of pain.
The analysis of the sample by groups showed 63.2% of femoral components in internal rotation and 36.8% in external rotation, with the tendency towards internal rotation in both groups, without significant differences (p=.519).
Regarding the femoral components corrected by gender, 54.9% were in external rotation, representing 60.3% in the pain group, with no significant differences observed between groups (p=.233).
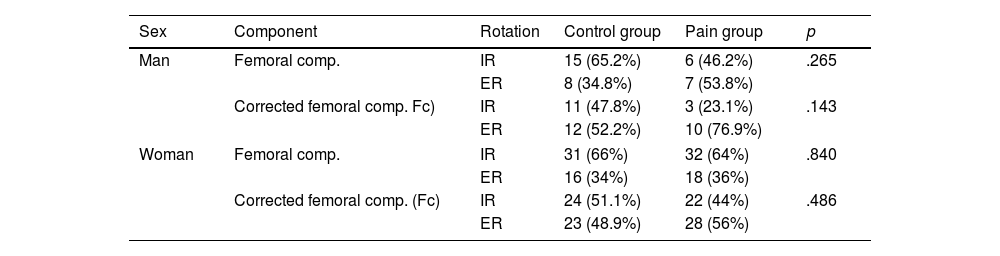
The results were analysed according to sex, with the results shown in Table 3.
Rotation of femoral component depending on gender.
| Sex | Component | Rotation | Control group | Pain group | p |
|---|---|---|---|---|---|
| Man | Femoral comp. | IR | 15 (65.2%) | 6 (46.2%) | .265 |
| ER | 8 (34.8%) | 7 (53.8%) | |||
| Corrected femoral comp. Fc) | IR | 11 (47.8%) | 3 (23.1%) | .143 | |
| ER | 12 (52.2%) | 10 (76.9%) | |||
| Woman | Femoral comp. | IR | 31 (66%) | 32 (64%) | .840 |
| ER | 16 (34%) | 18 (36%) | |||
| Corrected femoral comp. (Fc) | IR | 24 (51.1%) | 22 (44%) | .486 | |
| ER | 23 (48.9%) | 28 (56%) | |||
ER: external rotation; IR: internal rotation.
The pain group consisted of 13 men and 50 women. The control group consisted of 23 men and 47 women.
As for men, for the femoral component, 58.3% of the components were in internal rotation and 41.7% in external rotation. No significant differences were found between groups (p=.265). For the femoral component corrected for gender, 38.9% of the components were in internal rotation and 61.1% in external rotation, without finding significant differences between groups (p=.143).
As for women, for the femoral component, 64.9% of the components were in internal rotation and 35.1% in external rotation. No significant differences were found between groups (p=.840). For the femoral component corrected for gender, 47.4% of the components were in internal rotation and 52.6% in external rotation, without finding significant differences between groups (p=.486).
Malrotation of the femoral componentFor the analysis of malrotation of the femoral component, the rotation value limits that would be considered extreme were defined, calculated from the 10th and 90th percentiles for each variable in the control group. These values were used to define excess internal and external rotation in both groups.
We define excess external rotation (P10) as rotation values greater than:
- •
For the femoral component: 2.11°.
- •
For the Fc component for gender 5.01°.
We define excess internal rotation (P90) as rotation values greater than:
- •
For the femoral component: 2.65°.
- •
For the Fc component for gender: 2.29°.
The results are presented in Table 4. No significant differences were observed in any case. For the rotation of the femoral component and the femoral component corrected for gender (Fc), no significant differences were observed. There were more patients in the control group of the Fc component with excess external rotation, although the difference was not statistically significant (p=.253).
Femoral components with excess rotation in both groups.
| Control group | Pain group | p | |
|---|---|---|---|
| n=70 | n=63 | ||
| Fem rotation | |||
| Excess>2.11° ER | 7 (10.0%) | 8 (46.2%) | .623 |
| Excess>2.65° IR | 6 (8.6%) | 5 (7.9%) | .894 |
| Fem rotation C (Fc) | |||
| Excess>5.01° ER | 7 (10.0%) | 3 (4.8%) | .253 |
| Excess>2.29° IR | 7 (10.0%) | 5 (7.9%) | .678 |
ER: external rotation; IR: internal rotation.
Rotation of prosthetic components has been studied as a cause of TKA failure without reaching a consensus regarding the degree of involvement in the pathogenesis of pain. For several authors, internal rotation of the components has been associated with worse functional results, pain and, finally, failure of TKA.6,14,15 Other authors, such as Becker et al.,16,17 have found no correlation between the rotation of the femoral component and clinical results.
In the interobserver correlation study carried out to assess the level of consistency of the study, we obtained a substantial degree of agreement (ICC: .801) in the femoral measurements according to the Landis and Koch scale.18 With the same measurement protocol, Konigsberg et al.19 obtained a regular interobserver variability for the femur (.39). Hirschman et al.20 found moderately reliable results for the measurement of femoral component rotation in 2D-CT (ICC: .29) compared to the results obtained with 3D-CT (ICC: .91), recommending its use to reduce variability in measurements.
Although later studies, such as those by Yoshioka et al.21 or Gryphon et al.,22,23 have not been able to confirm the existence of a difference between sexes in terms of the value of the posterior condylar angle, we decided to analyse the results according to the two methods of interpretation with the aim of assessing whether there were differences between both methods in terms of the relationship between rotation of the femoral component and pain. The application of the correction for gender resulted in a greater number of men having the femoral component in external rotation (61.8%). In the female sex, the neutrality value did not have the same influence, being very close to 0°.
Regarding the rotation of the femoral component, we found no relationship between its positioning and the presence of pain, regardless of whether or not the gender correction described by Berger was taken into account. Our results are similar to those of Becker et al.,16 who did not find a correlation between the positioning of the femoral component and the results of TKA. They only showed worse results in the “physical function” subcategory of the WOMAC and worse results related to increased internal rotation, but without clinical repercussions. Young et al.17 also found no correlation between pain and rotation of the prosthetic components. Several studies have shown that deviating excessively from the TEA when placing the femoral component could cause different complications.24,25
Excess external rotation of the femoral component should be considered as a poor prognostic factor. In their study, Chen et al.26 showed that both internal and external malrotation of the femoral component could have an impact on the peak forces in both compartments: 5° of internal rotation could cause an increase in peak femorotibial pressure of 17% in the medial compartment. In turn, external rotation increased the peak pressure above 35% in the lateral compartment and reduced patella-femoral tension.27 According to Verlinden et al.,28 malrotation of the femoral component has shown an alteration in the contact area and contact pressure at the FP level: 5° of internal or external rotation reduced the contact area by more than 15% and increased the pressure by FP contact by 20%. In our study we did not assess contact forces based on prosthetic positioning.
The study by Rienmüller et al,29 with their study of between 6° of external rotation and 15° of internal rotation, revealed a great natural variability in the rotation of the femoral component, with numerous factors that determine its correct positioning, without observing differences in objective and subjective results.
ConclusionAccording to the results of our study, malrotation of the femoral component would have no influence on the presence of pain at a minimum of one year of follow-up after the implantation of a total knee arthroplasty. We did not find significant differences between groups or according to sex. We also did not find significant differences in patients with excess internal or external rotation of the femoral component.
Level of evidenceLevel of evidence iii.
FundingThis study was partially funded by the Sociedad Española de Cirugía Ortopédica y Traumatología (SECOT) and by the Sociedad Española de Rodilla (SEROD).
Conflict of interestsThe authors have no conflict of interests to declare with respect to this manuscript.
Ethical disclosuresThis is a study on the influence of femoral component rotation on the aetiology of pain after total knee replacement with a minimum follow-up of one year. Patients were informed of the implications of the study prior to obtaining informed consent.
Authorisation was obtained from the ethics committee of our hospital, dated 22 November 2018 and reference 2018/631.