Endomedullary nailing using the infrapatellar approach (IP) is considered the gold standard for the treatment of tibial diaphyseal fractures, however, it has been associated with greater difficulty in reduction and complications such as malalignment in procurvatum and anterior knee pain. The suprapatellar approach (SP) arises as an alternative to solve these aspects, also being associated with a shorter intraoperative time and a lower dose and fluoroscopy time.
Material and methodsRetrospective comparative study between a group of 22 fractures treated by SP approach and another of 30 fractures intervened by IP transtendinous approach. Perioperative variables were analysed, as well as clinical, radiological, and functional aspects in outpatient visits at 3, 6 and 12 months.
ResultsNo differences were found between groups in terms of intraoperative time, anemization, quality of reduction or complications during follow-up, among others. At 12 months, 12 (54.5%) SP cases and 16 (53.3%) IP presented anterior knee pain, without significant differences. In the evaluation scales, significant differences were recorded in the IKDC (International Knee Documentation Committee) in favour of the SP technique 88.45 (76.44–91.1) vs. IP 69 (49.95–80) (p=.006), with no significant differences in other functional scales analysed.
ConclusionsAccording to what has been described so far in the literature, the present study supports the tendency towards SP nailing by improving the functional results (IKDC) in the medium term compared to the traditional IP technique, without increasing complications. Likewise, surgeons perceive greater technical ease for reduction and simplicity in obtaining intraoperative radiological images.
El enclavado endomedular mediante abordaje infrapatelar (IP) se considera el gold standar del tratamiento de las fracturas diafisarias de tibia, sin embargo, se ha asociado a mayor dificultad para la reducción y complicaciones como la mala alineación en procurvatum y al dolor anterior de rodilla. El abordaje suprapatelar (SP) surge como alternativa para solventar estos aspectos, asociándose también con un menor tiempo intraoperatorio y menor dosis y tiempo de fluoroscopia.
Material y métodosEstudio retrospectivo comparativo entre un grupo de 22 fracturas intervenidas mediante abordaje SP y otro de 30 fracturas intervenidas por abordaje IP trastendinoso. Se analizaron variables perioperatorias y aspectos clínicos, radiológicos y funcionales en consulta a los tres, seis y 12 meses.
ResultadosNo se encontraron diferencias entre grupos en cuanto a tiempo intraoperatorio, anemización, calidad de la reducción o complicaciones en el seguimiento, entre otros. A los 12 meses, 12 (54,5%) casos SP y 16 (53,3%) IP presentaban dolor anterior de rodilla, sin diferencias significativas. En las escalas de evaluación, se registraron diferencias significativas en la International Knee Documentation Committee (IKDC) a favor de la técnica SP (88,45 [76,44-91,1] vs. IP 69 [49,95-80]) (p = 0,006), sin diferencias significativas en otras escalas funcionales analizadas.
ConclusionesEn consonancia con lo hasta ahora descrito en la literatura, el presente estudio apoya la tendencia hacia el enclavado SP por mejorar los resultados funcionales (IKDC) a medio plazo respecto a la técnica tradicional IP, sin aumentar las complicaciones. Asimismo se percibe por los cirujanos una mayor facilidad técnica para la reducción y sencillez en la obtención de imágenes radiológicas intraoperatorias.
Tibial diaphyseal fractures are the most frequent fractures of the long bones,1 accounting for approximately 2% of all fractures.2 Since the time of Küntscher,3 endomedullary nailing has become the gold standard in the treatment of these fractures.1,2 It has numerous advantages over other techniques, a low complication and re-intervention rate2 and it allows dynamic and minimally invasive fixation through less surgical dissection,4 respecting the soft tissue and vascular supply around the fracture, reducing infection and pseudo-arthrosis rates. It also facilitates mobilisation, rehabilitation, and early weight-bearing of the limb,1,4 reducing the patient's physical disability and stimulating osteogenesis, with high success rates in bone consolidation.5 Anterior knee pain is one of the most frequent complications related to nailing at this level. It has been described in 56%–80% of cases and is considered multifactorial in origin.6–8
An infrapatellar approach (IP), transtendinous or paratendinous, is classically used with the knee in hyperflexion.9 This technique involves difficulty in intraoperative reduction,9,10 because traction is used, and reduction needs to be performed with the knee in hyperflexion. Therefore, postoperative malalignments in valgus and procurvatum of proximal metaphyseal fractures have been described as complications associated with this approach due to the force exerted by the quadriceps on the proximal fragment11 during nailing in hyperflexion. It has also been linked to soft tissue injuries (injury to the infrapatellar nerve,6 the tendon or the surgical scar itself) as a cause of anterior knee pain.
The suprapatellar (SP) approach has been described as an alternative to the IP approach, with the main objective of facilitating the intraoperative reduction technique and optimising postoperative alignment of proximal tibial fractures. This approach allows a semi-extended position of the knee, which helps the reduction technique by neutralising the deforming forces of the quadriceps, and facilitates fluoroscopic imaging especially in the distal third of the tibia.9,12 It has also been associated with shorter operating times by providing a better entry point, lower fluoroscopy dose and time,12 and a lower rate of anterior knee pain.13,14 However, increased risk of femoropatellar joint (FP) injury10,13,15 and septic arthritis of the knee16 have been described as possible complications of this approach, as well as greater difficulty in removing material.
The aim of this study was to compare the clinical and radiographic results of the SP and IP approaches for nailing tibial diaphyseal fractures in adults at our centre.
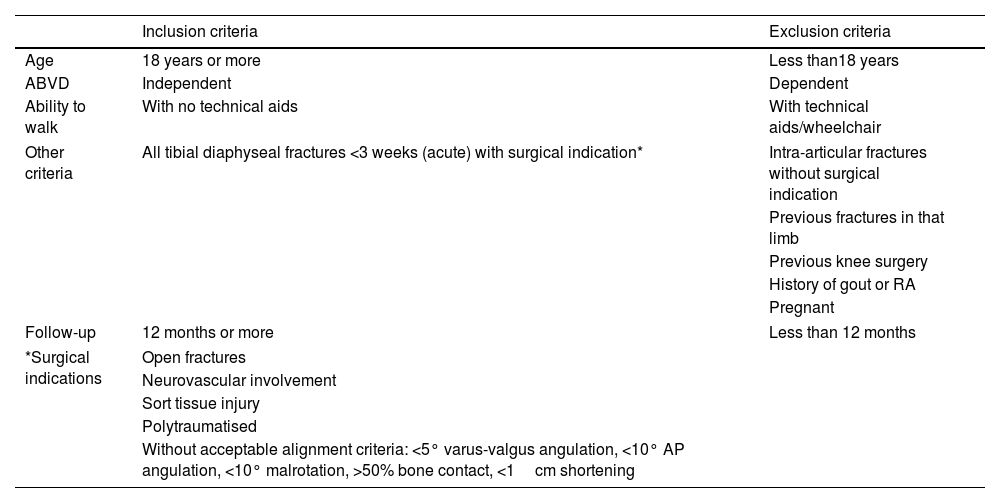
Material and methodsWe undertook a retrospective, observational comparative analytical study of patients undergoing intramedullary tibial nailing between 2015 and 2018 in a tertiary hospital: SP group versus IP control group. The patient sample was selected according to the inclusion and exclusion criteria listed in Table 1. The patients’ epidemiological variables (age and sex) and characteristics of the fractures were recorded: cause and energy of the mechanism of injury, associated injuries, laterality of the fracture. The fractures were classified according to AO/OTA Classification standards (42 A, B, C) 17 and to the Gustilo grade for open fractures.
Study inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Age | 18 years or more | Less than18 years |
| ABVD | Independent | Dependent |
| Ability to walk | With no technical aids | With technical aids/wheelchair |
| Other criteria | All tibial diaphyseal fractures <3 weeks (acute) with surgical indication* | Intra-articular fractures without surgical indication |
| Previous fractures in that limb | ||
| Previous knee surgery | ||
| History of gout or RA | ||
| Pregnant | ||
| Follow-up | 12 months or more | Less than 12 months |
| *Surgical indications | Open fractures | |
| Neurovascular involvement | ||
| Sort tissue injury | ||
| Polytraumatised | ||
| Without acceptable alignment criteria: <5° varus-valgus angulation, <10° AP angulation, <10° malrotation, >50% bone contact, <1cm shortening | ||
AP: anteroposterior; BADL: basic activities of daily living; RA: rheumatoid arthritis.
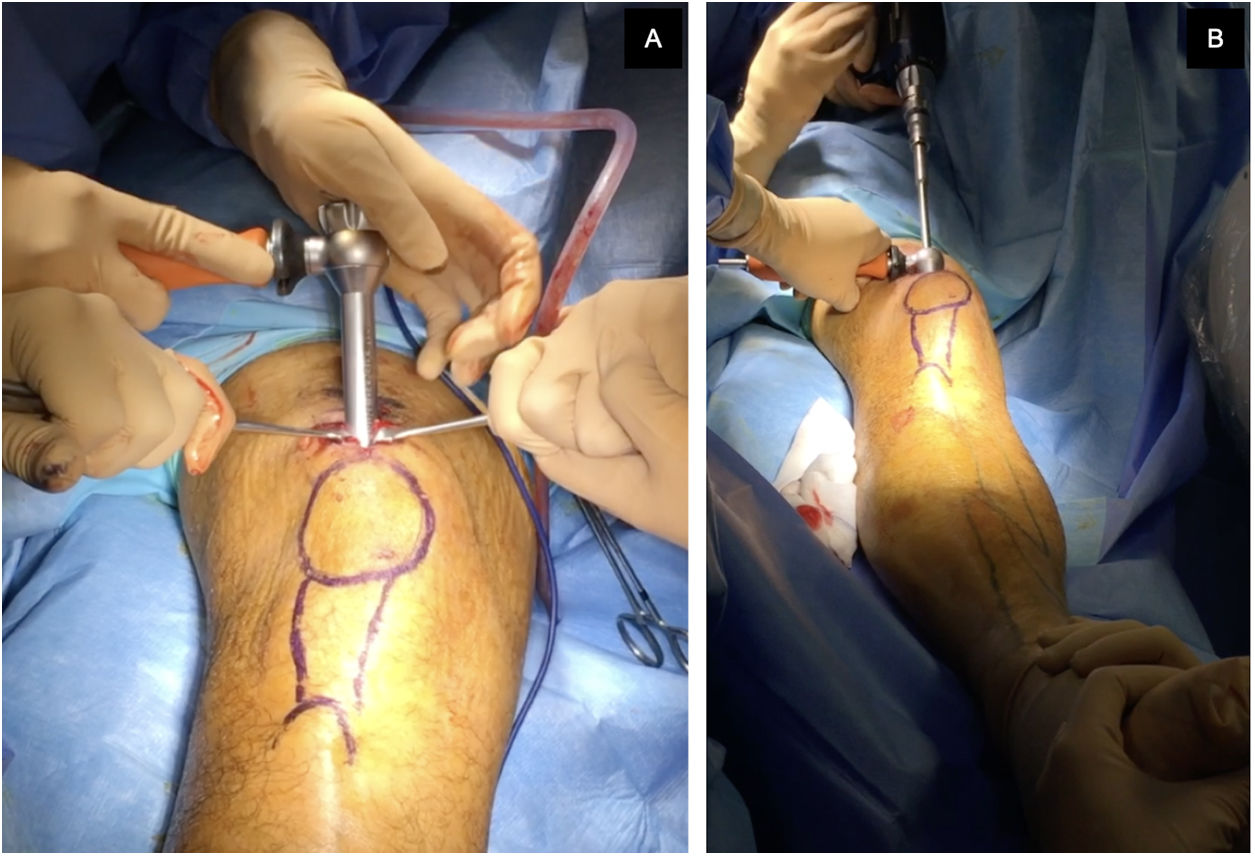
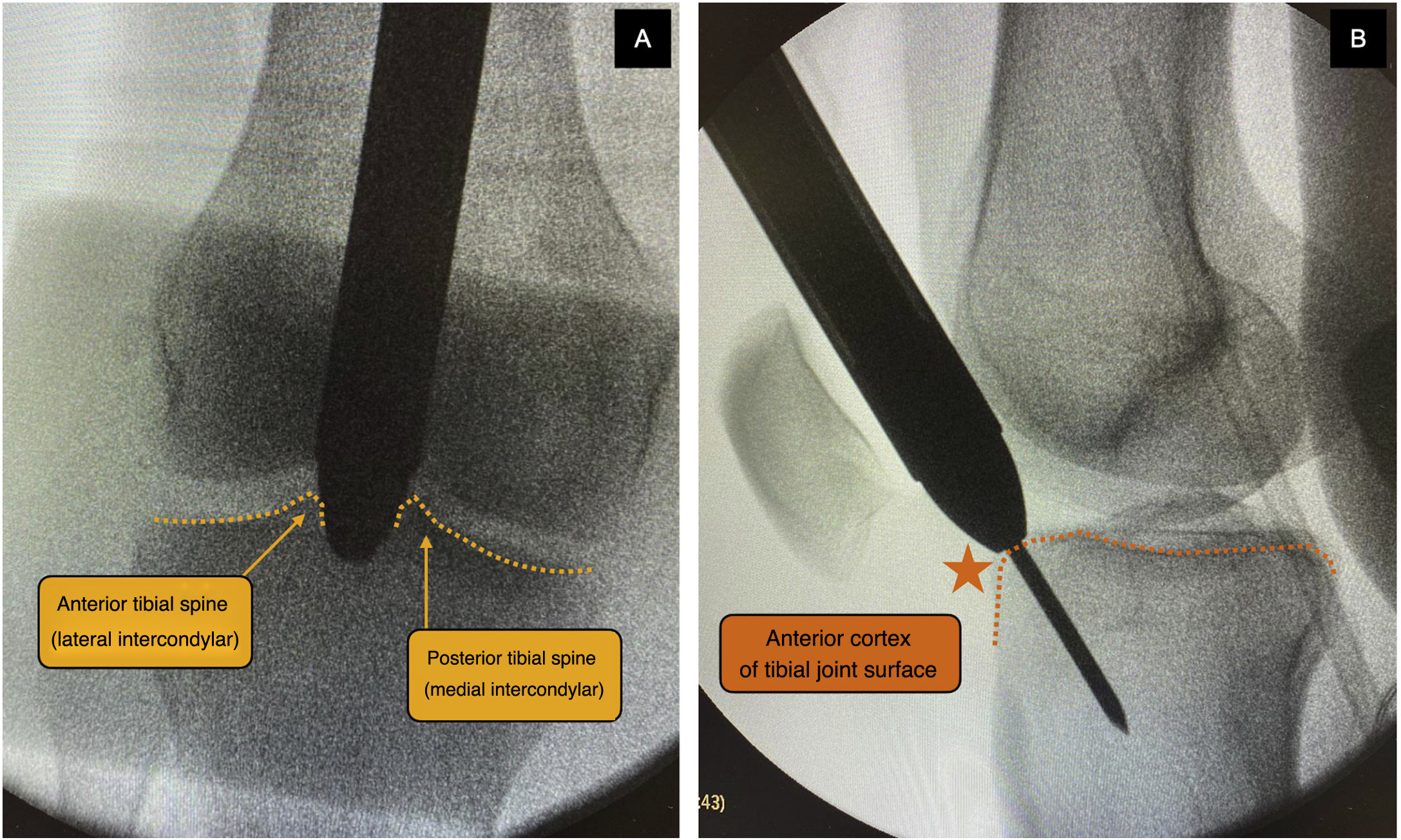
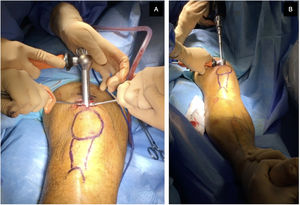
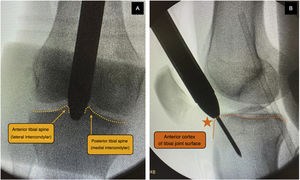
The approach was selected at the surgeon's discretion. The SP approach was used with the patient in the supine position, with the knee flexed 20°–30° on a sterile roller, through a 3–5cm skin incision from the proximal border of the patella in a cranial direction, dividing the quadriceps tendon longitudinally to access the retropatellar space, inserting a trocar (Fig. 1). The IP approach was used with the knee in about 100°–120° flexion, using a traction table for transcalcaneal traction as per the surgeon's preference (Fig. 2), making a 5cm skin incision from the inferior pole of the patella, progressing distally and slightly medially to the anterior tibial crest, crossing the patellar tendon. The entry point was the same in both approaches: medial to the lateral intercondylar tubercle (anterior tibial spine) in the coronal plane and at the anterior cortex of the joint surface; following the line of the intramedullary canal in the sagittal plane, following the indications of McConnell, Tornetta et al.,18 (Fig. 3). Closed fracture reduction was achieved by reduction manoeuvres and manual traction with no differences between groups.
Intraoperative radiological control of a patient undergoing the SP approach showing the trocar with protective cannula at the level of the patellofemoral joint and supported at the tibial entry point. (A) Medial to the lateral intercondylar tubercle (anterior tibial spine) in the coronal plane. (B) In front of the anterior articular border in the sagittal plane, following the indications of McConnell, Tornetta et al.18 This entry point was common to both types of approach.
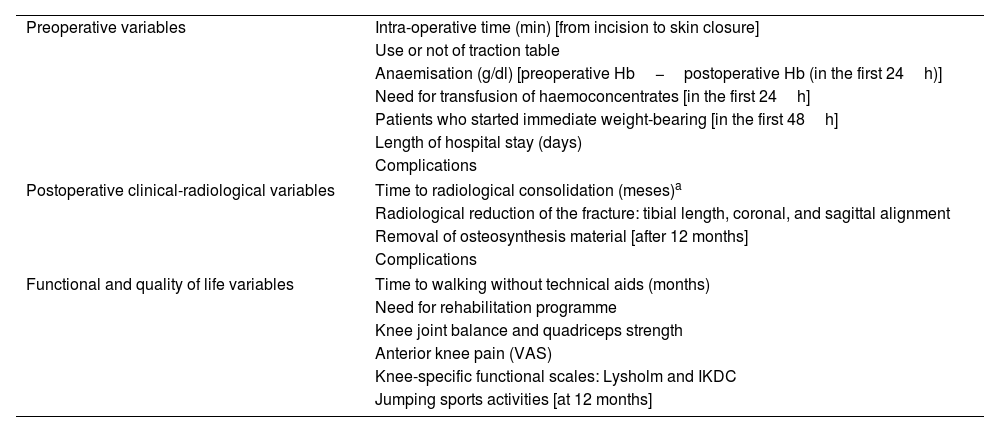
Perioperative variables during admission and clinical, radiological, and functional aspects were analysed in the clinic at 3, 6 and 12 months (Table 2). Pre- and postoperative radiological measurements were taken for study: the re-established tibial length after intramedullary nailing and postoperative alignment in the coronal and sagittal planes to assess the quality of the reduction in both groups. A subgroup analysis was also performed according to the fracture level (proximal, medial, distal, or bifocal) and type of fracture (open or closed). Knee assessment scales were used, as the fundamental difference between SP and IP nailing lies in the knee approach. The Lysholm knee score, described in 1982, is used to score patients’ subjective rating of the knee's functional ability during activities of daily living and sport, and comprises eight items: limp, support, instability, pain, locking, swelling, stair climbing, and squatting. The IKDC (International Knee Documentation Committee) scale was developed in 1987 in consensus by the American Society of Sports Medicine and the European Society of Sports Traumatology, Knee Surgery and Arthroscopy as a simple and direct questionnaire that could be easily used to assess different knee conditions, through clinical, functional and sports activity aspects with a subjective and an objective component and over 100 items.
Pre-, intra-, and postoperative variables at one, 3, 6 and 12 months.
| Preoperative variables | Intra-operative time (min) [from incision to skin closure] |
| Use or not of traction table | |
| Anaemisation (g/dl) [preoperative Hb−postoperative Hb (in the first 24h)] | |
| Need for transfusion of haemoconcentrates [in the first 24h] | |
| Patients who started immediate weight-bearing [in the first 48h] | |
| Length of hospital stay (days) | |
| Complications | |
| Postoperative clinical-radiological variables | Time to radiological consolidation (meses)a |
| Radiological reduction of the fracture: tibial length, coronal, and sagittal alignment | |
| Removal of osteosynthesis material [after 12 months] | |
| Complications | |
| Functional and quality of life variables | Time to walking without technical aids (months) |
| Need for rehabilitation programme | |
| Knee joint balance and quadriceps strength | |
| Anterior knee pain (VAS) | |
| Knee-specific functional scales: Lysholm and IKDC | |
| Jumping sports activities [at 12 months] | |
Hb: haemoglobin; IKDC: International Knee Documentation Committee Knee Form; VAS: visual analogue scale.
Consolidation was defined as callus formation in at least 3 cortices9 and pseudoarthrosis as fractures without radiological consolidation at 9 months or without radiological progression for 3 months.
We used SPSS version 2.1 (IBM Inc., Chicago, Illinois) for the statistical analysis, analysing qualitative variables using the χ2 test, Fisher's test and Likelihood Ratio test, and the Mann–Whitney test for quantitative variables. The level of statistical significance was set at p<.01. Descriptive variables for each group were reported as mean and standard deviation (SD), or median and interquartile range (IQR) for quantitative variables, and as frequencies and percentages for categorical variables.
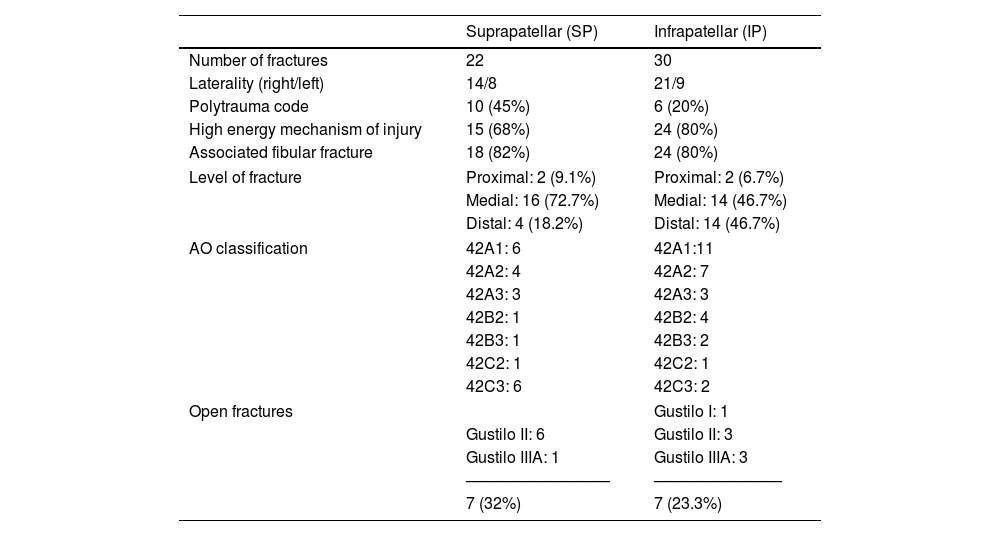
ResultsThe study included 52 patients, 35 males and 17 females with a mean age of 45 (SD 17.3) years, with 22 tibial diaphyseal fractures in the SP group and 30 in the IP group. The epidemiological data and characteristics of the fractures in each group are shown in Table 3.
Characteristics of fractures by group.
| Suprapatellar (SP) | Infrapatellar (IP) | |
|---|---|---|
| Number of fractures | 22 | 30 |
| Laterality (right/left) | 14/8 | 21/9 |
| Polytrauma code | 10 (45%) | 6 (20%) |
| High energy mechanism of injury | 15 (68%) | 24 (80%) |
| Associated fibular fracture | 18 (82%) | 24 (80%) |
| Level of fracture | Proximal: 2 (9.1%) | Proximal: 2 (6.7%) |
| Medial: 16 (72.7%) | Medial: 14 (46.7%) | |
| Distal: 4 (18.2%) | Distal: 14 (46.7%) | |
| AO classification | 42A1: 6 | 42A1:11 |
| 42A2: 4 | 42A2: 7 | |
| 42A3: 3 | 42A3: 3 | |
| 42B2: 1 | 42B2: 4 | |
| 42B3: 1 | 42B3: 2 | |
| 42C2: 1 | 42C2: 1 | |
| 42C3: 6 | 42C3: 2 | |
| Open fractures | Gustilo I: 1 | |
| Gustilo II: 6 | Gustilo II: 3 | |
| Gustilo IIIA: 1 | Gustilo IIIA: 3 | |
| ————————— | ———————— | |
| 7 (32%) | 7 (23.3%) | |
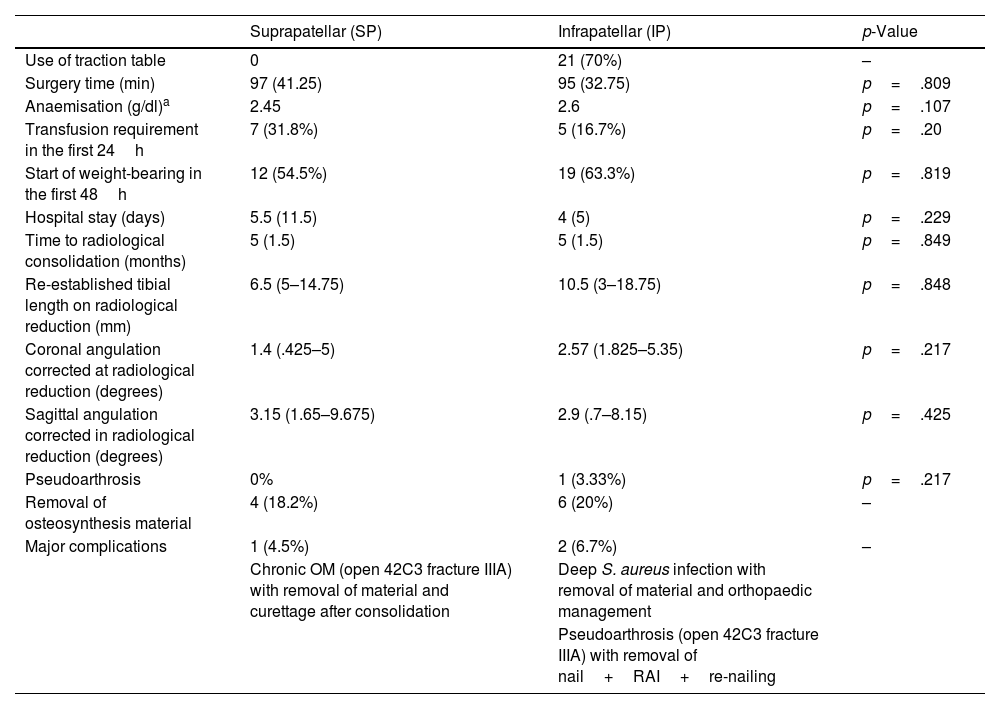
In the IP group, 21 fractures (70%) were operated on the traction table, and the orthopaedic table was used in the SP group. The intraoperative time was 97 (IQR 41.25) min in the SP group and 95 (IQR 32.75) min in the IP group, with no statistically significant differences (p=.809). Immediate weight-bearing was started within 48h postoperatively in 12 (54.5%) patients in the SP group and in 19 (63.3%) patients in the IP group, with no statistically significant differences (p=.819). Mean anaemia was 2.45g/dl and 2.6g/dl in the SP and IP groups respectively, requiring transfusion of haemoconcentrates in the first 24h in 7 SP cases (32%) and 5 IP cases (16.7%), without significant differences either in terms of mean anaemia (p=.107) or number of haemoconcentrates transfused (p=.20). There were also no significant differences in the mean hospital stay of either group: 5.5 (IQR 11.5) days mean stay in the SP group and 4 (IQR 5) days in the IP group (p=.229). No inpatient complications were recorded in either group. In the analysis of postoperative radiographs for both types of approach, no significant differences were found in terms of the quality of reduction, as measured by the restoration of tibial length and alignment in the coronal and sagittal plane. Table 4 summarises these results and other aspects of follow-up. Regarding the analysis of the quality of the radiological reduction by subgroup (fracture level and open/closed fracture) for each type of approach, only the subgroups of middle third and distal fractures could be analysed, and there were no significant differences in terms of postoperative re-established tibial length (p=.126), coronal angulation (p=.341) or sagittal angulation (p=.496).
Analysis of perioperative, radiological and complication variables.
| Suprapatellar (SP) | Infrapatellar (IP) | p-Value | |
|---|---|---|---|
| Use of traction table | 0 | 21 (70%) | – |
| Surgery time (min) | 97 (41.25) | 95 (32.75) | p=.809 |
| Anaemisation (g/dl)a | 2.45 | 2.6 | p=.107 |
| Transfusion requirement in the first 24h | 7 (31.8%) | 5 (16.7%) | p=.20 |
| Start of weight-bearing in the first 48h | 12 (54.5%) | 19 (63.3%) | p=.819 |
| Hospital stay (days) | 5.5 (11.5) | 4 (5) | p=.229 |
| Time to radiological consolidation (months) | 5 (1.5) | 5 (1.5) | p=.849 |
| Re-established tibial length on radiological reduction (mm) | 6.5 (5–14.75) | 10.5 (3–18.75) | p=.848 |
| Coronal angulation corrected at radiological reduction (degrees) | 1.4 (.425–5) | 2.57 (1.825–5.35) | p=.217 |
| Sagittal angulation corrected in radiological reduction (degrees) | 3.15 (1.65–9.675) | 2.9 (.7–8.15) | p=.425 |
| Pseudoarthrosis | 0% | 1 (3.33%) | p=.217 |
| Removal of osteosynthesis material | 4 (18.2%) | 6 (20%) | – |
| Major complications | 1 (4.5%) | 2 (6.7%) | – |
| Chronic OM (open 42C3 fracture IIIA) with removal of material and curettage after consolidation | Deep S. aureus infection with removal of material and orthopaedic management | ||
| Pseudoarthrosis (open 42C3 fracture IIIA) with removal of nail+RAI+re-nailing |
OM: osteomyelitis; RAI: reamer aspirator irrigator.
Results are shown as count and percentage or median and interquartile range.
All the major complications that required hospital readmission were in open fractures. One case of osteomyelitis was recorded in the SP group, which was reoperated after fracture healing, with removal of all the osteosynthesis material and curettage by reaming the medullary canal and lavage, with a good result. In the cases operated using the IP approach, 2 major complications were recorded: a deep Staphylococcus aureus infection in the operated leg in one patient that resolved after surgery and a reoperated case of pseudoarthrosis, in which fracture consolidation was achieved 5 months after the reintervention, with preserved anatomical and mechanical axis. In total, osteosynthesis material was removed in 4 (18.2%) cases in the SP group (2 due to discomfort with the material, one for fracture dynamization at 3 months and another due to an osteomyelitis complication) while 7 (23.3%) were removed in the IP group (4 due to discomfort with the material, one for fracture dynamization at 4 months and in the other 2 cases due to serious complications).
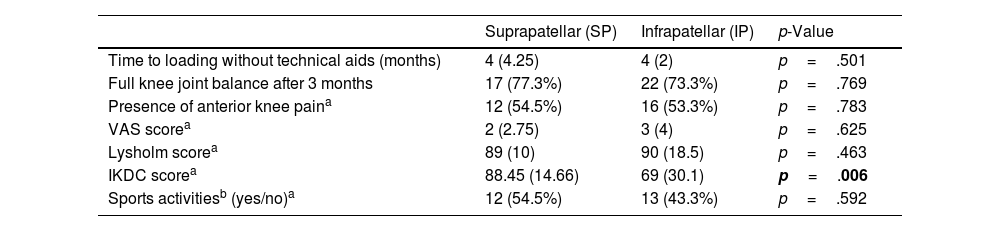
Table 5 summarises the patients’ clinical and functional progress. In both groups, the mean time to ambulation without technical aids was 4 months, and we found no significant differences, nor did we find differences in the number of patients who achieved complete joint balance at 3 months: 17 (77.3%) and 22 (73.3%) in the SP and IP groups, respectively. We questioned patients about anterior knee pain at the 12-month consultation, confirming 12 (54.5%) cases in the SP group and 16 (53.3%) in the IP group, with no significant differences.
Analysis of functional and quality of life variables during postoperative follow-up.
| Suprapatellar (SP) | Infrapatellar (IP) | p-Value | |
|---|---|---|---|
| Time to loading without technical aids (months) | 4 (4.25) | 4 (2) | p=.501 |
| Full knee joint balance after 3 months | 17 (77.3%) | 22 (73.3%) | p=.769 |
| Presence of anterior knee paina | 12 (54.5%) | 16 (53.3%) | p=.783 |
| VAS scorea | 2 (2.75) | 3 (4) | p=.625 |
| Lysholm scorea | 89 (10) | 90 (18.5) | p=.463 |
| IKDC scorea | 88.45 (14.66) | 69 (30.1) | p=.006 |
| Sports activitiesb (yes/no)a | 12 (54.5%) | 13 (43.3%) | p=.592 |
VAS: visual analogue scale; IKDC: International Knee Documentation Committee Knee Form. Results are shown as count and percentage or median and interquartile range.
In bold, the statistically significant result.
Regarding the patients’ functionality and quality of life as assessed by clinical and functional assessment scales at 12 months, significant differences (p=.006) were recorded in the IKDC knee scale, with a score of 88.45 (IQR 14.66) and 69 (IQR 30.1) in the SP and IP groups, respectively; no differences were observed in Lysholm knee or VAS score. At 12 months after surgery, approximately half the patients in the two groups (12 [54.5%] SP and 13 [43.3%] IP), were able to undertake impact sports activities (football, volleyball, tennis, basketball, etc.) with no significant differences between cases and controls (Table 5).
DiscussionOne of the main objectives in the decision to intervene in traumatology patients is to optimise their quality of life, in acute and traumatic injuries as well as chronic and degenerative injuries. The use of functionality and quality of life scales, the patients’ physical independence and sporting activities, and detecting complications and their treatment are the main factors determining patients’ residual quality after trauma and orthopaedic treatment. Current studies evaluating the outcomes of tibial diaphyseal fracture treatment focus on surgical variables and their potential complications. However, there are few studies that assess the quality of life of patients with long-term tibial diaphyseal fractures, and most of the short-term follow-up studies do not find significant results in functionality and quality of life or do not evaluate it at all. One qualifies quality of life in patients with tibial diaphyseal fractures, confirming that all patients’ quality of life improves from the beginning until one year of follow-up and that quality of life is better in patients with closed fractures of the tibia compared to those with open fractures, with statistically significant differences.19 It is essential to study factors such as functionality and personal perception of quality of life to choose the best treatment and to address controversy, such as, for example, in the type of osteosynthesis and approach in these fractures, as proposed in the present study.
Patients with limited activity and restricted quality of life after tibial intramedullary nailing are often found in clinical practice.20 Anterior knee pain is the most frequent postoperative complication following nailing, with an incidence of 10%–80%,1,2 and this most affects these patients’ quality of life. Furthermore, it is estimated that tibial diaphyseal fractures have a significant complication rate, requiring readmission to hospital for their treatment in 11.7%.21 This last figure is slightly higher than that recorded in our series, with 4.5% and 6.7% of serious complications in the SP and IP group, respectively. The high incidence of complications has a negative impact on the patient's physical and psychological condition; patients who suffer complications during the treatment of their tibial diaphyseal fracture have a statistically and clinically significant worse quality of life than those who do not have complications.19 Some of these complications occur in open fractures, in the literature 18%–24%,22,23 32% and 23.3% in the SP and IP group, respectively, in our series. All the major complications in our series occurred in open fractures.
The SP approach began to be studied when poor results with the IP approach started to be reported: high rates of malunion, postoperative malalignment, and failure of fixation of the proximal fragment in proximal diaphyseal fractures.10 Malalignment associated with the IP approach has been reported in 50%–60% of proximal third fractures and even in 24% of distal third fractures. Therefore, SP nailing has been described and successfully used10,13 with the main objective of improving alignment in proximal fragments. The semi-extended position counteracts procurvatum by minimising the deforming force of the extensor apparatus12 and also facilitates maintaining fracture reduction and improves rotation control during reaming in proximal and distal third fractures.13,15,24,25 Avilucea et al., 2016, studied this effect in distal fractures, obtaining correct alignment in 96.2% of SP and 73.9% of IP nails.24 Wang et al., 2018 and Xu et al., 2019, in their meta-analyses, identified significant results in favour of the SP approach, with better alignment in the sagittal plane1,26 and in the coronal plane.26 This position also facilitates the entry point of the nail. Eastman et al.,15 2010, conducted a cadaver study to determine the correlation between the point of entry of the nail and degrees of knee flexion, achieving a significant result especially at 30°–50° flexion, when there is greater alignment in the sagittal plane between the nail and the medullary tibia, consistent with data from other comparative studies.11 This in turn prevents mechanical conflict with the posterior cortex23 and the patella locking effect seen in the IP approach.23 Therefore, the SP approach has demonstrated significantly better surgical reductions and more precise nail entry points than the IP approach.11,26 However, in our study after postoperative radiological analysis we found no significant differences in the quality of reduction between groups.
In the semi-extended position it is easier to perform intraoperative biplanar (anteroposterior and lateral) fluoroscopy with less manipulation and fewer attempts,12,15,26 which implies a reduction in both time and fluoroscopy dose.1,2,12,26,27 The SP approach could also reduce intraoperative times26,27; however, neither our study nor other studies looking at intraoperative time have found statistically significant differences.2,11,28 This may be due to the influence of other factors such as the skill and experience of the surgeon and the difficulty of the fracture.12 In our study, we recorded the first SP approaches performed in our centre, which may have contributed to the intraoperative time not being shorter than using the IP approach, due to the learning curve. In most of the studies,2,28 and the present study, no differences were observed in terms of patient anaemisation, or mean hospital stay. However, when reviewed by meta-analysis, some confirm significant differences in favour of the SP approach.27 As was likely, there are no differences in time to radiological consolidation either in our study or in the literature.1,2,10,28
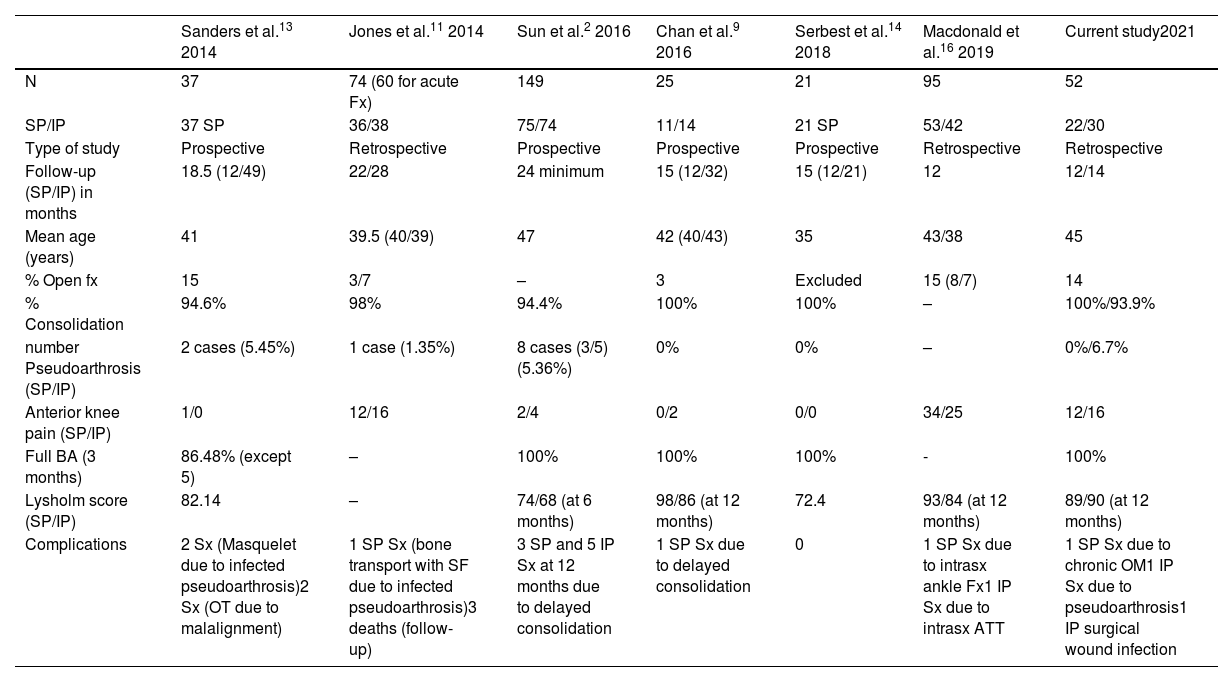
Despite the advantages associated with this approach, there is great controversy as to whether the approach10 and the advantages it provides are significant enough to implement a real change in the type of approach; therefore, in the last decade a multitude of comparative studies on the use of the SP and IP approaches have been described. Table 6 shows the most relevant data from these studies.
Summary of the most recent comparative studies between the IP and SP approaches.
| Sanders et al.13 2014 | Jones et al.11 2014 | Sun et al.2 2016 | Chan et al.9 2016 | Serbest et al.14 2018 | Macdonald et al.16 2019 | Current study2021 | |
|---|---|---|---|---|---|---|---|
| N | 37 | 74 (60 for acute Fx) | 149 | 25 | 21 | 95 | 52 |
| SP/IP | 37 SP | 36/38 | 75/74 | 11/14 | 21 SP | 53/42 | 22/30 |
| Type of study | Prospective | Retrospective | Prospective | Prospective | Prospective | Retrospective | Retrospective |
| Follow-up (SP/IP) in months | 18.5 (12/49) | 22/28 | 24 minimum | 15 (12/32) | 15 (12/21) | 12 | 12/14 |
| Mean age (years) | 41 | 39.5 (40/39) | 47 | 42 (40/43) | 35 | 43/38 | 45 |
| % Open fx | 15 | 3/7 | – | 3 | Excluded | 15 (8/7) | 14 |
| % Consolidation | 94.6% | 98% | 94.4% | 100% | 100% | – | 100%/93.9% |
| number Pseudoarthrosis (SP/IP) | 2 cases (5.45%) | 1 case (1.35%) | 8 cases (3/5) (5.36%) | 0% | 0% | – | 0%/6.7% |
| Anterior knee pain (SP/IP) | 1/0 | 12/16 | 2/4 | 0/2 | 0/0 | 34/25 | 12/16 |
| Full BA (3 months) | 86.48% (except 5) | – | 100% | 100% | 100% | - | 100% |
| Lysholm score (SP/IP) | 82.14 | – | 74/68 (at 6 months) | 98/86 (at 12 months) | 72.4 | 93/84 (at 12 months) | 89/90 (at 12 months) |
| Complications | 2 Sx (Masquelet due to infected pseudoarthrosis)2 Sx (OT due to malalignment) | 1 SP Sx (bone transport with SF due to infected pseudoarthrosis)3 deaths (follow-up) | 3 SP and 5 IP Sx at 12 months due to delayed consolidation | 1 SP Sx due to delayed consolidation | 0 | 1 SP Sx due to intrasx ankle Fx1 IP Sx due to intrasx ATT | 1 SP Sx due to chronic OM1 IP Sx due to pseudoarthrosis1 IP surgical wound infection |
ATT: anterior tibial tuberosity; Fx: fracture; Intrasx: intraoperative; IP: infrapatellar; OM: osteomyelitis; OT: osteotomy; SP: suprapatellar; Sx: surgical; TSF: Taylor spatial frame.
Controversial disadvantages of the SP approach include intra-articular knee injury, anterior knee pain, difficulty of material removal, and the risk of complications such as septic knee arthritis.10 Potential complications of the SP technique are weakness of the quadriceps after opening, arthrofibrosis of the knee, irritation of the femoropatellar cartilage (FP), and even the appearance of free bodies due to intra-articular invasion. Regarding FP damage, Gelbke et al., 2010 concluded that there is no risk to the cartilage surface during SP nailing29; and some authors claim that, since the SP approach facilitates the entry point, this damage would be less. In addition, the use of specific trocar systems with protectors that attach to the patellofemoral surface further decreases the possibility of FP injury.10,29 Cadaveric and pre- and postoperative arthroscopy studies have been performed to assess FP cartilage damage, and patients undergoing the SP approach have been assessed radiologically and by MRI, but in most cases the findings have not been clinically related,2,13 or have been minimal.14 Comparing the two approaches, no significant differences in FP joint damage have been found in most comparative studies.9,10,23,27 Therefore, there is insufficient evidence in the literature on FP damage with the SP approach, nor are there long-term studies to demonstrate this.
Anterior knee pain is considered multifactorial in origin: damage to the tibial articular surface with point of entry28 or soft tissue injury (Hoffa's fat necrosis),23 all more frequent during the IP approach, and the hyperflexed knee position during IP nailing.13 It is also present after SP nailing and has therefore been linked to intra-articular damage to the knee, mainly at the FP joint. There are also other causes irrespective of the approach, such as possible irritant effects of the intramedullary nail itself,15 or muscle-ligament injury associated with trauma at knee level. On comparing anterior knee pain in both types of approach, most studies have found no significant differences,9,11,13 as in our study (p=.783). However, recent meta-analyses do conclude that there is less anterior knee pain associated with the SP approach.1,2,25–27 This could be related to the advantages of this approach: greater protection of the infrapatellar nerve and patellar tendon, less damage to the tibial surface and meniscal and ligament insertion zones as the entry point is more precisely located, and the use of protective sleeves for the intra-articular guidance system.
Likewise, anterior knee pain can lead to physical disability as it is related to a loss of joint balance. In our study, we found no significant differences in terms of knee joint balance, full mobility being achieved in the first months preoperatively (70% at 3 months) thanks to early mobilisation of the limb. Most of the literature finds no significant differences in this regard for either approach, nor differences between the operated knee and the contralateral knee.2,9,10,13,27 In cases of loss of joint balance, this does not correlate with functional limitations as almost all patients are able to kneel.10
Therefore, although anterior knee pain is common, it does not generally correlate with an associated functional deficit as functional scales such as the Lysholm scale show good or very good overall scores at one year follow-up. Statistically significant differences in favour of the SP approach at 12-month follow-up in Lysholm score have been reported in the literature.2,27,28 In our study, there were no significant differences on this scale, although mean Lysholm scores of 90 out of 100 were found, corresponding to “very good” on the Lysholm scale, in line with previous studies.10 However, we also evaluated patients using the IKDC knee scale, which yielded significant results in favour of the SP approach: with a mean score at 12 months of 88.45 (76.44–91.1), and 69 (49.95–80) out of 100 points, for the SP and IP approaches respectively. We found no other comparative study that has used this scale during follow-up; however, it is a scale that is used frequently scale to assess knee injuries.
Only half the patients are able to perform impact sports activities one year following surgery, both in our study (54.5% and 43.3% in the SP and IP group respectively) and in previous studies.10 This has a negative impact on the quality of life of many patients, as most are young and active, with a mean age of 45 years in our study. Prior to the current work, we found only one study in the literature on the quality of life20 of patients operated for tibial diaphyseal fractures by long-term endomedullary nailing, which did not specify the type of approach. In that study, 8 years after surgery, 60% of patients experienced limitations in sports, 58% had restrictions in quality of life, and 44% had a higher incidence of knee pain compared to a reference population; most evident among younger patients.20
In terms of serious complications such as pseudarthrosis, osteomyelitis, heterotopic ossifications, embolisms, there are no significant differences between SP and IP nailing in the literature,1,2,10,11,25,27,28 or in our study. The SP approach has been associated with an increased risk of septic arthritis of the knee, especially in open fractures.16,25 In closed fractures there appears to be no significantly increased risk of septic knee arthritis with SP nailing,30 as in the present work, where no such complication was reported. The removal of the implant after osteosynthesis using the SP approach to the tibia is an unresolved problem to date; in our study, 3 pins were removed and extracted via the anterior, supra-, or infrapatellar approach without complications. The opinion of some authors is that it is no more complicated than in the IP approach,25 while others resort to making another incision, at the infrapatellar level, to remove it.23
This study has some limitations, mainly the small sample size, which makes it difficult to achieve statistical significance. And the retrospective nature of the study prevented analysis of some interesting aspects mentioned in this discussion, such as fluoroscopy time and dose, time in patient positioning, and preoperative results of functional scales. It would also be interesting to perform an imaging test to assess the status of the patellofemoral joint and correlate clinical and radiological findings.
In conclusion, the present study reinforces the current trend in trauma units to use SP nailing due to its numerous advantages over the traditional IP technique, through the statistically significant improvement in functional outcomes (IKDC) in the medium term, without increasing the complication rate. Surgeons also perceive that the reduction technique is easier to perform, and it is simpler to position the patient and obtain intraoperative radiological images.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.