Women carry out a greater risk of anterior cruciate ligament (ACL) rupture. However, outcomes following ACL reconstruction remain unclear. The aim of this study was to analyse the outcomes in women following ACL reconstruction and compare these outcomes with men.
Material and methodsRetrospective study of a prospective database of patients treated with ACL reconstruction between January 2017 and December 2018. Outcome measures included Tegner activity scale, Lysholm scale, EVA scale, and IKDC evaluation form. Clinical significance was measured with minimally clinical important difference, and patient acceptable symptom state.
ResultsA total of 33 women were matched with 99 men. The mean follow-up was 36 months. Women showed significant improvement from preoperative PROs to the latest follow-up, with no differences between groups. In patients under 25 years old, there was less significant IKDC subjective score in women compared to men. There were no significant differences in frequency of patients achieving MCID and PASS in women compared with men.
ConclusionsAt 3-year following 4-strand semitendinosus-gracilis anterior ligament reconstruction, women showed significant improvements in PROs, with no differences compared to men.
Las mujeres presentan un riesgo elevado de rotura del ligamento cruzado anterior (LCA). Sin embargo, los resultados tras la cirugía reconstructiva son dispares en la literatura. El propósito de este estudio fue analizar los resultados en las mujeres tras cirugía reconstructiva del LCA, y compararlos con los resultados de los hombres.
Material y métodosEstudio retrospectivo de una base de datos prospectiva de pacientes intervenidos mediante reconstrucción anatómica semitendinoso-recto interno 4 fascículos del LCA entre enero de 2017 y diciembre de 2018. Para la valoración de los pacientes se utilizó la escala de actividad deportiva de Tegner, la escala de Lysholm, la EVA y el formulario IKDC subjetivo y objetivo. Se determinó la significación clínica con la diferencia mínima clínicamente importante y el estado de síntomas aceptable del paciente.
ResultadosSe incluyeron en el estudio 33 mujeres y 99 hombres. El seguimiento medio de los pacientes fue de 36 meses. Las puntuaciones se incrementaron significativamente en los cuestionarios de valoración funcional en las mujeres al final del seguimiento, con resultados similares a los hombres. Solo se detectó una menor puntuación media significativa en las mujeres en el cuestionario IKDC subjetivo en aquellas menores de 25 años comparadas con los hombres. El porcentaje de pacientes que alcanzaron la significación clínica fue similar entre mujeres y hombres.
ConclusionesA los 3 años de seguimiento tras la reconstrucción anatómica semitendinoso-recto interno 4 fascículos del LCA, las mujeres presentaron una mejoría con significación estadística y clínica en los cuestionarios de valoración, sin diferencias con respecto a los hombres.
The growth of women's sport is constant and the number of sports licences is increasing year after year. According to data from the National Sports Council, in the last decade the number of female sports licences has grown by 20.8%, mainly in basketball and football.1 Different factors have been described that account for a 2–9 times higher risk of anterior cruciate ligament (ACL) rupture in women compared to men.2,3 Mall et al. described an increase in the incidence of ACL rupture in women from 10.3 to 18.6 per 100,000 from 1994 to 2006 in the United States.4
Outcomes after ACL reconstructive surgery published in the literature are mixed when comparing women and men. Ageberg et al. published the results of the Swedish registry with 10,164 cases between 2005 and 2008, with significantly lower scores in women at 1 and 2 years postoperatively when compared to men.5 Ryan et al. indicated in their systematic review published in 2014 that the results are similar between women and men.6 Tan et al. published a systematic review and meta-analysis in 2015 in which they reported similar or inferior results in women, but no significant differences.7 However, the fact that there is no statistically significant difference does not guarantee that there is no clinically significant difference. Statistical significance is no more than a mathematical formula that does not reflect the patient's perception of improvement after the surgical procedure.8 Previous studies have determined clinical significance values for the Lysholm, Tegner and subjective International Knee Documentation Committee (IKDC) scales.9–11 However, few ACL reconstructive surgery studies have analysed the clinical significance of their results.12
The primary objective of this study was to evaluate functional outcomes in women after ACL reconstructive surgery and to compare these outcomes, both preoperatively and postoperatively, with those obtained by men. Secondary objectives included comparisons of demographic variables, intraoperative findings, surgical procedures, return to sporting activity and complications between women and men. Our working hypothesis was that women would not achieve similar functional outcomes when compared to men after ACL reconstructive surgery.
Material and methodPatient selectionFrom our prospective database of patients with ACL rupture, we selected those who met the following inclusion criteria: female sex, age over 18 and under 40 years, no previous knee surgery, surgery between 1 January 2017 and 31 December 2018, minimum follow-up of 12 months. Exclusion criteria included age younger than 18 and older than 40 years, multi-ligamentous injury, ACL rupture, previous knee surgery. For each woman included in the study, 3 men were selected by date of surgery (±3 months) and age (±3 years). All patients gave informed consent for participation in the study.
Surgical techniqueThe patients underwent surgery using the anatomical semitendinosus-rectus internus reconstruction technique with 4 fascicles, femoral anchorage with TightRope® system and interferential screw in the tibia (Arthrex, Naples, FL, USA) by the same surgical team. The presence of meniscal and cartilaginous lesions and intraoperative complications were recorded. Cartilaginous lesions were classified according to Outerbridge.13 Associated surgical techniques were meniscal suture or partial meniscectomy, debridement for low-grade cartilaginous lesion or drilling for high-grade cartilaginous lesion. In all cases, a single dose of 2g cefazolin was administered preoperatively as antibiotic prophylaxis. Aspirative drainage was not used.
Postoperative managementAntithrombotic prophylaxis with low molecular weight heparin was indicated for 30 days postoperatively. Crutch-assisted partial weight bearing was authorised at 24h post-surgery. If meniscal suturing was required, a post-surgical knee extension brace was indicated for 4 weeks.14 The rehabilitation protocol was identical for all patients and comprised several phases, with return to sport from the sixth month after surgery if the patient had a 90% symmetry index in mobility, strength and hop tests.15
EvaluationsPatients were assessed preoperatively, at 6 and 12 months and annually using the Tegner sport activity scale,16 the Lysholm scale,17 the VAS scale for pain level and the IKDC form for subjective assessment and for clinical knee assessment.18 At the end of follow-up, the number of patients who had reached clinical significance was determined by the minimum clinically important difference (MCID) for the Lysholm scale (8.9 points),9 Tegner (one point)9 and subjective IKDC (16.7 points),10 and patient acceptable symptom status (PASS) for the subjective IKDC scale (75.9 points).11
Medical and surgical complications, hospital readmissions in the first 30 days after surgery, tendon ruptures and the need for surgical reoperation were recorded.
At the end of follow-up reuptake of sport was recorded and the level of sports activity according to the Tegner scale.16
Statistical analysisStatistical analysis was performed with SPSS®, version 18.0 (SPSS Inc., Chicago, IL, USA). Values of p≤.05 were considered significant. Normality of the study variables was determined using the Kolmogorov–Smirnov test. The Student's t-test was used for comparison of continuous variables and the chi-square test for categorical variables. The relationship between continuous variables was analysed with Pearson's test. The effect size of standardised mean comparisons was calculated using Cohen's d.
The power of the study a posteriori, considering the sample size, the 95% confidence level and a difference in the mean subjective IKDC scale between women and men at the end of follow-up of 5.8 points, was 84.9%.
ResultsGeneral dataDuring the study period, 148 patients met the inclusion criteria. Of these, 33 were female and 115 were male. For each female, 3 males were selected by date of surgery (±3 months) and age (±3 years), with a final sample of 33 females and 99 males.
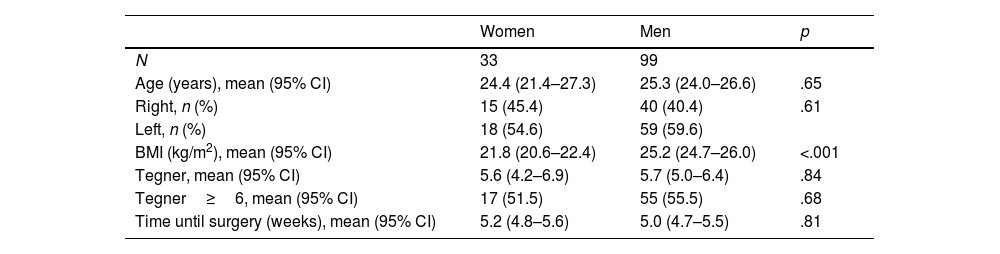
Table 1 shows the preoperative data in both groups. Significant differences were detected with respect to BMI. The most practised sport was football with 95 patients (71.9%), followed by rugby with 14 patients (10.6%), running with 13 patients (9.8%), and basketball with 10 patients (7.7%).
Preoperative data of the series.
| Women | Men | p | |
|---|---|---|---|
| N | 33 | 99 | |
| Age (years), mean (95% CI) | 24.4 (21.4–27.3) | 25.3 (24.0–26.6) | .65 |
| Right, n (%) | 15 (45.4) | 40 (40.4) | .61 |
| Left, n (%) | 18 (54.6) | 59 (59.6) | |
| BMI (kg/m2), mean (95% CI) | 21.8 (20.6–22.4) | 25.2 (24.7–26.0) | <.001 |
| Tegner, mean (95% CI) | 5.6 (4.2–6.9) | 5.7 (5.0–6.4) | .84 |
| Tegner≥6, mean (95% CI) | 17 (51.5) | 55 (55.5) | .68 |
| Time until surgery (weeks), mean (95% CI) | 5.2 (4.8–5.6) | 5.0 (4.7–5.5) | .81 |
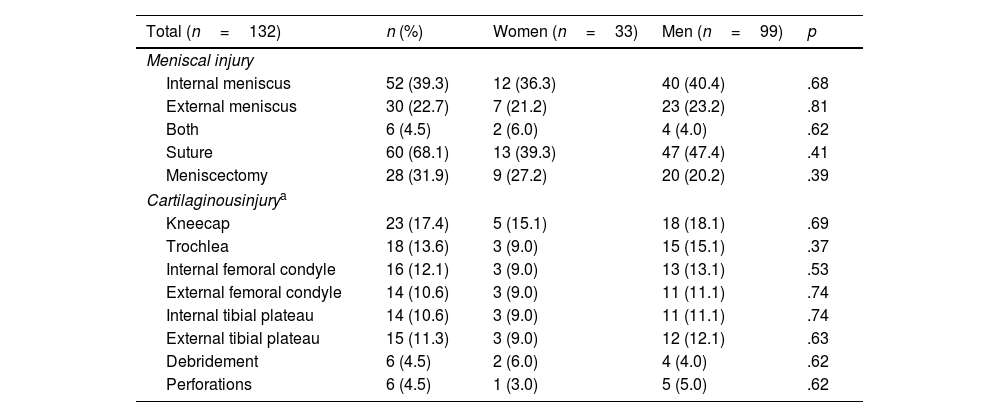
Intraoperatively meniscal injury was detected in 88 patients (66.6%) and cartilaginous injury in 52 patients (39.3%). Meniscal suturing was performed with an “all-inside” fixation system. Cartilaginous lesions were grade 1 in 81.2%. There were no significant differences in the treatment of meniscal and cartilaginous lesions (Table 2). No intraoperative complications were recorded.
Intraoperative events and procedures.
| Total (n=132) | n (%) | Women (n=33) | Men (n=99) | p |
|---|---|---|---|---|
| Meniscal injury | ||||
| Internal meniscus | 52 (39.3) | 12 (36.3) | 40 (40.4) | .68 |
| External meniscus | 30 (22.7) | 7 (21.2) | 23 (23.2) | .81 |
| Both | 6 (4.5) | 2 (6.0) | 4 (4.0) | .62 |
| Suture | 60 (68.1) | 13 (39.3) | 47 (47.4) | .41 |
| Meniscectomy | 28 (31.9) | 9 (27.2) | 20 (20.2) | .39 |
| Cartilaginousinjurya | ||||
| Kneecap | 23 (17.4) | 5 (15.1) | 18 (18.1) | .69 |
| Trochlea | 18 (13.6) | 3 (9.0) | 15 (15.1) | .37 |
| Internal femoral condyle | 16 (12.1) | 3 (9.0) | 13 (13.1) | .53 |
| External femoral condyle | 14 (10.6) | 3 (9.0) | 11 (11.1) | .74 |
| Internal tibial plateau | 14 (10.6) | 3 (9.0) | 11 (11.1) | .74 |
| External tibial plateau | 15 (11.3) | 3 (9.0) | 12 (12.1) | .63 |
| Debridement | 6 (4.5) | 2 (6.0) | 4 (4.0) | .62 |
| Perforations | 6 (4.5) | 1 (3.0) | 5 (5.0) | .62 |
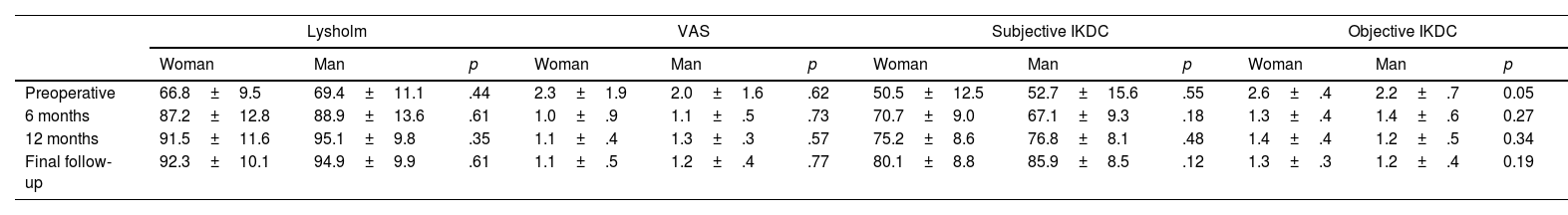
The mean follow-up of patients was 36.1 months (95% CI: 25.1–42.6). There was a significant improvement between preoperative and last revision in Lysholm scale (p=.005), subjective IKDC (p=.001) and objective IKDC (p=.002), but not with respect to VAS scale (p=.51), in both groups. No significant differences were detected between the two groups preoperatively or during follow-up (Table 3). The mean increase between preoperative and last revision was similar in both groups: Lysholm scale (21.4 in females vs. 25.7 in males; p=.25), VAS scale (−.9 in females vs. −1.3 in males; p=027), subjective IKDC scale (24.6 in females vs. 21.7 in males; p=.57). Clinical significance was also similar in both groups. MCID was achieved for the Lysholm scale in 88.9% of females versus 93.9% of males (p=.29); for the subjective IKDC scale in 95.1% of females versus 94.8% of males (p=.78); for the Tegner scale in 9.5% of females versus 10.1% of males (p=.55). With respect to the subjective PASS IKDC, 88.5% of women and 90.3% of men (p=.67) reached the indicated value of clinical significance.
Scale of functional evaluation.
| Lysholm | VAS | Subjective IKDC | Objective IKDC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Woman | Man | p | Woman | Man | p | Woman | Man | p | Woman | Man | p | |
| Preoperative | 66.8±9.5 | 69.4±11.1 | .44 | 2.3±1.9 | 2.0±1.6 | .62 | 50.5±12.5 | 52.7±15.6 | .55 | 2.6±.4 | 2.2±.7 | 0.05 |
| 6 months | 87.2±12.8 | 88.9±13.6 | .61 | 1.0±.9 | 1.1±.5 | .73 | 70.7±9.0 | 67.1±9.3 | .18 | 1.3±.4 | 1.4±.6 | 0.27 |
| 12 months | 91.5±11.6 | 95.1±9.8 | .35 | 1.1±.4 | 1.3±.3 | .57 | 75.2±8.6 | 76.8±8.1 | .48 | 1.4±.4 | 1.2±.5 | 0.34 |
| Final follow-up | 92.3±10.1 | 94.9±9.9 | .61 | 1.1±.5 | 1.2±.4 | .77 | 80.1±8.8 | 85.9±8.5 | .12 | 1.3±.3 | 1.2±.4 | 0.19 |
Figures expressed as mean±standard deviation.
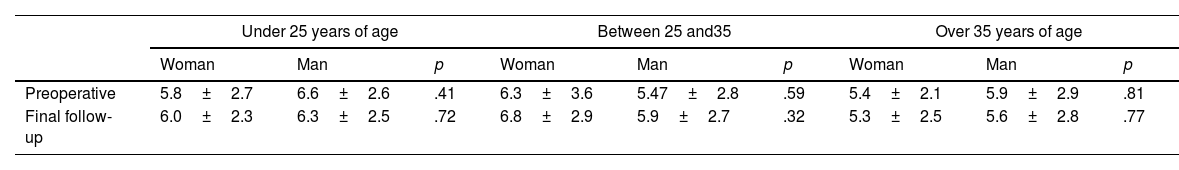
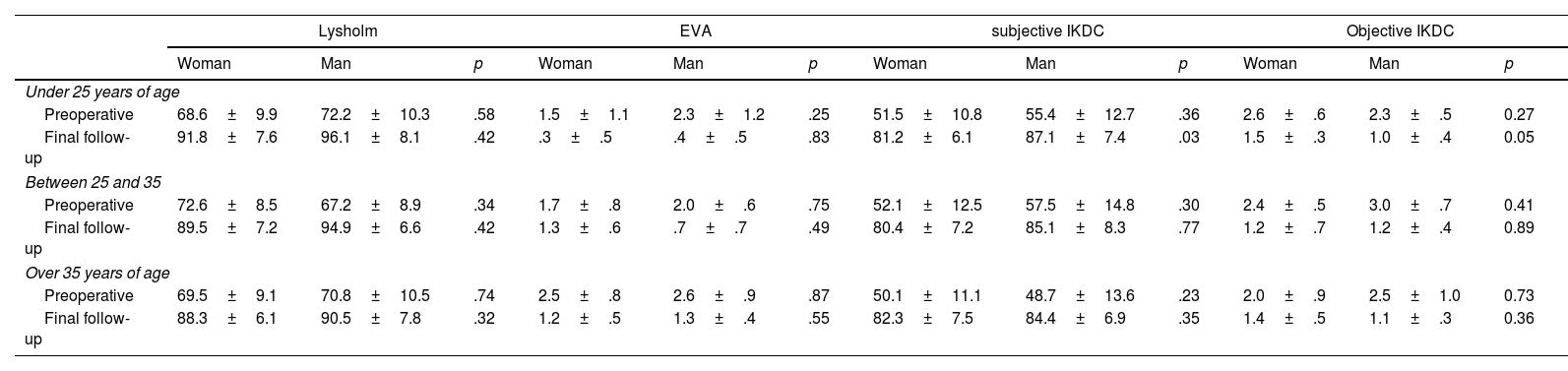
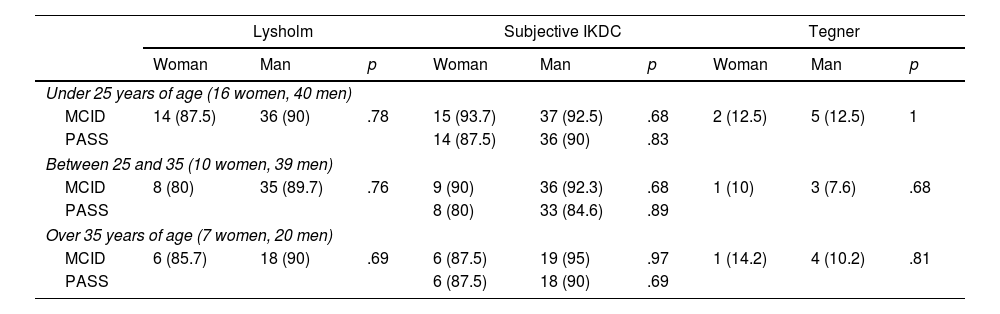
To determine whether age was a bias in the results obtained, an analysis of the rating scales was performed by dividing the patients into under 25 years (16 women and 40 men), between 25 and 35 years (10 women and 39 men) and over 35 years (7 women and 20 men). The level of sport activity preoperatively and at the end of follow-up was similar between women and men in the 3 age groups (Table 4). Significantly lower scores on the subjective IKDC scale at the end of follow-up were detected in the group of women younger than 25 years compared to men, with a Cohen effect size d=.77 (Table 5). However, there was no significant difference in the percentage of patients reaching clinical significance between women and men in the 3 age groups (Table 6).
Level of sporting activity according to age group.
| Under 25 years of age | Between 25 and35 | Over 35 years of age | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Woman | Man | p | Woman | Man | p | Woman | Man | p | |
| Preoperative | 5.8±2.7 | 6.6±2.6 | .41 | 6.3±3.6 | 5.47±2.8 | .59 | 5.4±2.1 | 5.9±2.9 | .81 |
| Final follow-up | 6.0±2.3 | 6.3±2.5 | .72 | 6.8±2.9 | 5.9±2.7 | .32 | 5.3±2.5 | 5.6±2.8 | .77 |
Figures expressed as mean±standard deviation.
Functional assessment scales.
| Lysholm | EVA | subjective IKDC | Objective IKDC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Woman | Man | p | Woman | Man | p | Woman | Man | p | Woman | Man | p | |
| Under 25 years of age | ||||||||||||
| Preoperative | 68.6±9.9 | 72.2±10.3 | .58 | 1.5±1.1 | 2.3±1.2 | .25 | 51.5±10.8 | 55.4±12.7 | .36 | 2.6±.6 | 2.3±.5 | 0.27 |
| Final follow-up | 91.8±7.6 | 96.1±8.1 | .42 | .3±.5 | .4±.5 | .83 | 81.2±6.1 | 87.1±7.4 | .03 | 1.5±.3 | 1.0±.4 | 0.05 |
| Between 25 and 35 | ||||||||||||
| Preoperative | 72.6±8.5 | 67.2±8.9 | .34 | 1.7±.8 | 2.0±.6 | .75 | 52.1±12.5 | 57.5±14.8 | .30 | 2.4±.5 | 3.0±.7 | 0.41 |
| Final follow-up | 89.5±7.2 | 94.9±6.6 | .42 | 1.3±.6 | .7±.7 | .49 | 80.4±7.2 | 85.1±8.3 | .77 | 1.2±.7 | 1.2±.4 | 0.89 |
| Over 35 years of age | ||||||||||||
| Preoperative | 69.5±9.1 | 70.8±10.5 | .74 | 2.5±.8 | 2.6±.9 | .87 | 50.1±11.1 | 48.7±13.6 | .23 | 2.0±.9 | 2.5±1.0 | 0.73 |
| Final follow-up | 88.3±6.1 | 90.5±7.8 | .32 | 1.2±.5 | 1.3±.4 | .55 | 82.3±7.5 | 84.4±6.9 | .35 | 1.4±.5 | 1.1±.3 | 0.36 |
Figures expressed as mean±standard deviation.
Number and percentage of patients who reached clinical significance according to age group.
| Lysholm | Subjective IKDC | Tegner | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Woman | Man | p | Woman | Man | p | Woman | Man | p | |
| Under 25 years of age (16 women, 40 men) | |||||||||
| MCID | 14 (87.5) | 36 (90) | .78 | 15 (93.7) | 37 (92.5) | .68 | 2 (12.5) | 5 (12.5) | 1 |
| PASS | 14 (87.5) | 36 (90) | .83 | ||||||
| Between 25 and 35 (10 women, 39 men) | |||||||||
| MCID | 8 (80) | 35 (89.7) | .76 | 9 (90) | 36 (92.3) | .68 | 1 (10) | 3 (7.6) | .68 |
| PASS | 8 (80) | 33 (84.6) | .89 | ||||||
| Over 35 years of age (7 women, 20 men) | |||||||||
| MCID | 6 (85.7) | 18 (90) | .69 | 6 (87.5) | 19 (95) | .97 | 1 (14.2) | 4 (10.2) | .81 |
| PASS | 6 (87.5) | 18 (90) | .69 | ||||||
Figures expressed as n (%).
There were no postoperative complications or hospital readmissions in the first 30 days after surgery, no tendon ruptures or need for surgical reintervention throughout the entire follow-up period.
Return to sportThe level of sporting activity increased to 5.8 (95% CI: 4.5–7.0) in women and 5.6 (95% CI: 4.9–6.3) in men, with no significant difference between the two groups (p=.58). 87.7% (29 patients) of the women and 86.8% (86 patients) of the men maintained the same level of sporting activity according to the Tegner scale. There was a change in the level of sport activity in 4 women (3 up one level and one down one level) and in 13 men (9 up one level and 4 down one level).
DiscussionOur study shows a significant functional improvement in women after ACL reconstructive surgery at 3 years of follow-up, reaching similar results to men, so we reject our hypothesis. A significantly lower mean score on the subjective IKDC questionnaire was only detected in women under 25 years of age compared to men, with an effect size of medium magnitude. The percentage of patients reaching clinical significance was similar between women and men.
Previous studies published in the literature have shown disparity between women and men after ACL reconstructive surgery, with significantly lower scores in women at 1 and 2 years,5 similar scores,6 or lower scores in women but no significant differences.7 Ageberg et al. published results from the Swedish Knee Ligament Register with 4,438 patients (42% female), preoperatively and at 1- and 2-years follow-up, on the KOOS scale, with significantly lower scores in women compared to men. However, the effect size of the differences found was small in magnitude (mean difference between 1.4 and 4.4 points; Cohen's d values between .05 and .16), and no differences in increases were detected between preoperative and one year postoperative, or between one and two years postoperative.5 Ryan et al. conducted a systematic review including 9 comparative studies with a minimum of 2 years follow-up and 5410 patients (2325 women and 3085 men). Only one study reported significant differences on the KOOS5 scale between women and men, concluding that the results of ACL reconstructive surgery were similar between women and men.6 Tan et al. analysed 7 studies in a systematic review and meta-analysis assessing outcomes using the IKDC scale and found no significant differences between women and men. However, they did report significantly lower scores in women on the Lysholm scale analysed in 11 studies and on the KOOS scale analysed in 6 studies, although they highlighted a high heterogeneity between studies.7 Recently, Kuenze et al. compared by age (±1 year) and date of surgery (±1 month) the results in 45 women and 45 men, with significantly lower scores in women on the subjective IKDC scale and on the KOOS subscale for pain, with a follow-up between 5 and 9 months.19 In our study we found significant differences on the IKDC scale between women and men in the under 25 age group. This finding coincides with the results of Kuenze et al.19 in their series of patients with a mean age of 18 years and a range between 13 and 25 years. The effect size was larger in our study (mean difference 5.9 and Cohen d=.77 vs. mean difference 5.5 and Cohen d=.48), possibly because the follow-up of patients in the Kuenze et al.19 study was between 5 and 9 months, much longer than in the Kuenze et al.20 study was between 5 and 9 months, much shorter than in our study and with the possibility of changes in the assessment questionnaire, as reported by Agarwalla et al.20 in their systematic review on the evolutionary chronology of patient improvement after ACL reconstructive surgery.
Regarding clinical significance, Kuenze et al.19 report a significantly lower percentage of women achieving MCID for the subjective IKDC scale compared to men (33.3% vs. 60%), but not for the KOOS questionnaire. It should be considered that the follow-up of their patients was between 5 and 9 months, and that there was still room for improvement in the assessment questionnaires used.20 In our study we found no differences in the percentages of patients achieving MCID for the Lysholm, IKDC and Tegner scales, nor in PASS for the IKDC scale. Our results show that women perceive clinical improvement and satisfaction at the same level as men after ACL reconstructive surgery.
The series published in the literature refer to a 33–95% return to sport one year after surgery, and different influential factors are established, including gender.21,22 Ardern et al. published, in a systematic review and meta-analysis including 69 articles with 7556 patients, that there were no differences in the return to sport between women and men, but that women did have lower scores on the Tegner scale.23 Ryan et al. published in a systematic review that there were no significant differences in postoperative Tegner scale scores between women and men.6 However, Tan et al. did report lower scores on the Tegner scale in women compared to men, although they indicated a high heterogeneity of the studies analysed in their systematic review and meta-analysis.7 In our study we found no significant differences in the Tegner scale preoperatively or at the end of follow-up.
We should not consider our results without knowing the limitations of the study. The sample size of the series is smaller than that of previous published studies. Postoperative laxity was not recorded with a validated arthrometer, nor was the degree of psychological preparation for return to sport, to determine whether there were significant differences between women and men. The size of the graft, which may affect the results, was not recorded.24 But the study also has strengths. It is a retrospective comparative study of a prospective database, with analysis of statistical and clinical significance, with no loss to follow-up. All patients were operated on by the same surgical team, with no heterogeneity in graft type, surgical technique, management of meniscal and cartilage lesions or postoperative rehabilitation plan.
ConclusionAt 3 years of follow-up after ACL surgery using the anatomical reconstruction technique semitendinosus-rectus internus 4 fascicles, women showed statistically and clinically significant improvement in the Lysholm, VAS, IKDC and Tegner scales, with no differences with respect to men.
Level of evidenceLevel of evidence iii.
FundingNo funding was received for this study.
Conflict of interestsThe authors have no conflict of interests to declare.