The purpose of this study is to describe the outcomes of using a triple button device for the treatment of displaced distal-third clavicle fractures (Neer type II-b).
Material and methodA retrospective review was conducted on a series of patients between November 2011 and December 2014. Fourteen patients initially met the inclusion criteria, but 2 were excluded, leaving 12 patients (83.3% male; mean age 32.2 years) for the final analysis at a mean follow-up of 26±11.24 months (range, 12–48). Post-operative follow-up was performed at 2 weeks (two first months), and monthly thereafter, until was achieving clinically and radiological healing. The functional outcome was evaluated using the Constant score, and DASH score in the last follow-up.
ResultsThe mean Constant Score was 95.5±5.2 points (range, 85–100), with a mean DASH score of 3.3±4.4 points (range, 0–12.5). The mean time to clinical healing was 10.3±3.1 weeks (range, 8–16), and the mean time to radiological healing was 13.6±2.6 weeks (range, 12–20). There were no major complications. There were 5 minor complications without clinical impact: 2 coracoclavicular calcifications, 1 hypertrophic scar, 1 patient with discomfort due to the device, and 1 superficial wound infection. All patients returned their previous activity.
ConclusionGood clinical results can be achieved with the triple button device in unstable distal fractures of the clavicle, without the need to remove the hardware.
El objetivo de este estudio es describir los resultados de un dispositivo de triple botón para el tratamiento de las fracturas desplazadas de tercio distal de clavícula (tipo ii-b de Neer).
Material y métodoEstudio retrospectivo de una serie de pacientes entre noviembre de 2011 y diciembre de 2014. Catorce pacientes se ajustaron inicialmente a los criterios de inclusión, 2 de los cuales fueron excluidos, dejando 12 pacientes (83,3% varones; edad media 32,2 años) para el análisis final. El seguimiento medio fue de 26±11,24 meses (rango, 12-48). El seguimiento postoperatorio se realizó a las 2 semanas (en los 2 primeros meses) y después mensualmente, hasta que se consiguió la curación clínica y radiológica. El resultado funcional se evaluó mediante el test de Constant y la puntuación DASH en el último seguimiento.
ResultadosLa puntuación media del test de Constant fue de 95,5±5,2 puntos (rango, 85-100) y la del test DASH, de 3,3±4,4 puntos (rango: 0-12,5). El tiempo medio para la curación clínica fue de 10,3±3,1 semanas (rango, 8-16) y para la consolidación radiológica, de 13,6±2,6 semanas (rango, 12-20). No hubo complicaciones mayores. Hubo 5 complicaciones menores sin repercusión clínica: 2 calcificaciones coracoclaviculares, una cicatriz hipertrófica, un paciente con molestias sobre el dispositivo y una infección de la herida. Todos los pacientes retomaron su actividad previa.
ConclusiónEl dispositivo de triple botón consigue excelentes resultados en el tratamiento de las fracturas de tercio distal de clavícula sin necesidad de retirar el material.
In recent series distal-third clavicular fractures make up 21–28% of all clavicular fractures.1 Road or sports accidents are the most common mechanisms of trauma in young people, followed by low energy falls in elderly patients.2
Neer's classification3 is the most frequently used and includes 3 fracture types. In type I, the fracture is lateral to the coracoclavicular ligaments and there is minimal displacement. In type III there is an articular fracture line. Both types are considered stable and are treated conservatively.
Type II injuries are unstable, because the fracture is medial to the coracoclavicular ligaments and the medial fragment is drawn upwards and backwards by the effect of the trapezius. In addition, the distal fragment is pulled downwards by the weight of the arm and rotated by the scapula (Fig. 1). Neer type II is subdivided into 2 subtypes: type II-a, where both ligaments are joined to the distal fragment, and type II-b, where the trapezoid ligament remains inserted in the distal fragment, the conoid ligament being torn, which results in greater displacement between fragments.
Since the first clinical series, the trend has been towards treating these Neer type II injuries surgically, justified by the high incidence of pseudoarthrosis, 22–50%, 4–6 consolidation delays (45–67% take more than 3 months to heal) and discomfort in the patients who are treated orthopedically, with the clinical and social consequences that this involves, especially for young patients.7,8
The number of treatment techniques has increased considerably in recent years, including arthroscopic alternatives, and generally achieve satisfactory outcomes.9–15 The problem with most relates to the implant, either because it moves, causes discomfort or pain, making it necessary to remove it, and fails to maintain proper reduction to enable correct consolidation.16 Because they are rare, it is difficult to obtain long series with sufficient follow-up to extract scientifically valuable data (most are level IV2 studies) so as to be able to decide the best therapeutic option. The objective of this study is to present our experience and outcomes with the coracoclavicular triple button TightRope system (Twin Tail TightRope™).
Material and methodA retrospective study was performed which included Neer type II-b distal-third clavicular fractures operated using the Twin Tail TightRope™ system (Arthrex, Naples, FL, U.S.A.) in our work centre from November 11 to December 2014, with a minimum of one year's follow-up in order to form part of the study. Patients with skeletal immaturity, fractures or previous shoulder injury surgery, patients with a high anaesthetic risk or those who did not want to participate in the study were excluded. Of the 14 patients who met the criteria, 2 were excluded: one was lost to follow-up and another presented a previous fracture in the injured clavicle, a total of 12 patients remained for the final study: 10 males (83.3%) and 2 females (16.7%). The mean age was 32.25±10.51 years (range, 18–56). The causes were 5 road traffic accidents (3 car and 2 motorbike), 6 were sports injuries (2 cycling, 2 football, one rugby and one martial arts) and one accidental fall. The right side was injured in 7 patients (58.3%) and the left in 5 patients (41.7%). Mean follow-up was 26±11.24 months (range, 12–48 months).
All the patients included in the study underwent a standard anteroposterior X-ray of the shoulder and projection of the clavicle with 30° cephalic tilt, both without load. Radiological assessment was undertaken preoperatively and postoperatively: every 2 weeks for the first 2 months, monthly from the third to the sixth month, and then annually. Radiological healing was defined as the presence of bone bridging obliterating the fracture space with no significant radiolucencies around it. Clinical healing was defined as the absence of spontaneous pain or pain on palpation of the fracture site, and articular balance of the shoulder with no pain. Similarly Constant17 and DASH18 scores were calculated at their very last follow-up. Radiological assessment and the clinical tests were undertaken by two surgeons who were independent of the study (JBG, FG).
The presence of major complications was assessed, such as those requiring a second unscheduled operation (deep infection requiring surgical drainage, implant failure, need for revision due to reduction loss, non-union), and minor complications which did not necessitate reoperation (intolerance to the material, superficial infection resolved with medical treatment, problems with scarring, calcifications). The need to remove the material was recorded independently from the rest of the complications. All the patients gave their written consent.
Surgical techniqueThe patients were operated in the deckchair position, with a pillow underneath the ipsilateral scapula. The arm was left free so as to be able to move it during the operation. The patients were given a general anaesthetic and an associated ultrasound-guided upper limb nerve block. Antibiotic prophylaxis with cefazolin was administered. All the operations were performed by 2 shoulder surgeons (JAC;GNS). The triple button system was used (AC Twin Tail®, Arthrex, Naples, FL, U.S.A.). This is a system designed for the treatment of acromioclavicular dislocation that comprises a button to place below the coracoid apophysis and 2 clavicular buttons intended to reproduce the disposition of the coracoclavicular ligaments.
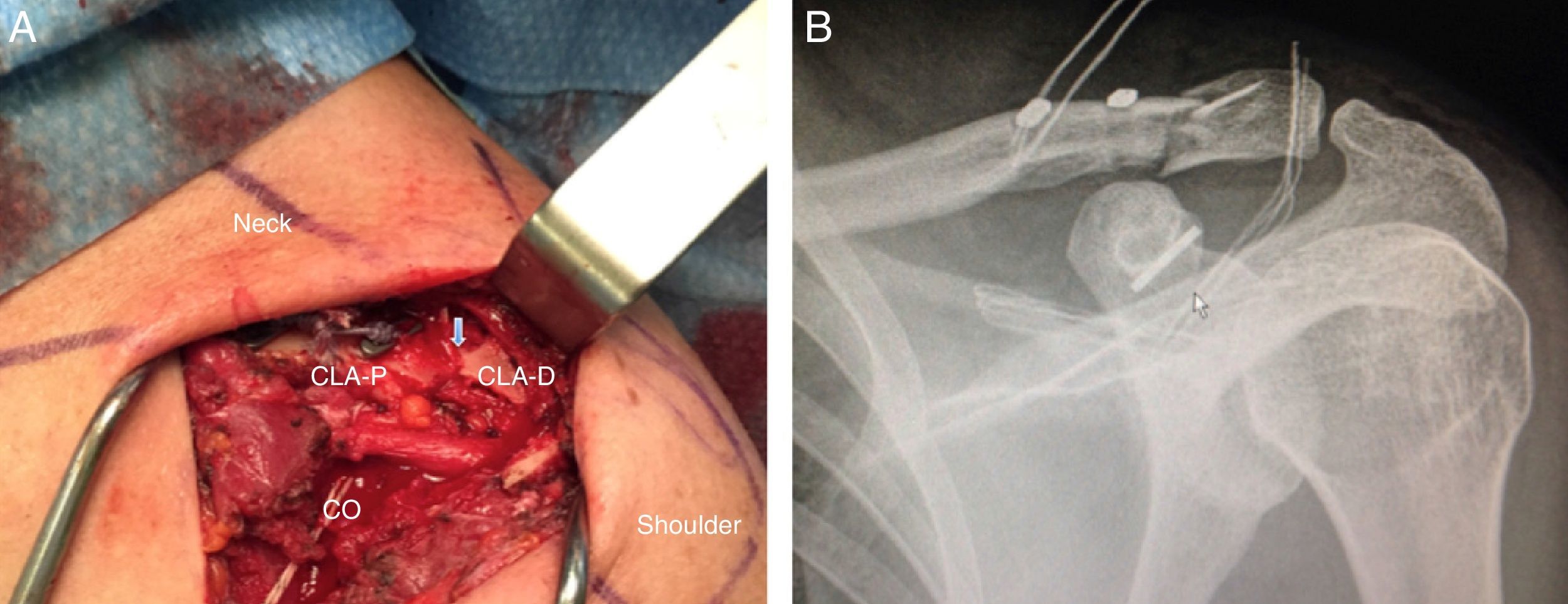
A vertical incision is made, slightly medial to the acromioclavicular joint, to the coracoid apophysis, about 5cm long. After opening the deltopectoral fascia the distal third of the clavicle is exposed (without stripping the periosteum of the distal fragment) and the upper surface of the coracoid apophysis is released by blunt dissection. An orifice is made with a 4.5mm drill bit with visceral protection placed below its lower surface; 2 4.5mm orifices are made in the same way in the proximal fragment of the distal clavicle (in the original technique they are 4mm): the most medial orifice in the posterior clavicular third (at around 40mm from the joint) and the most lateral, in the anterior clavicular third (at around 25mm from the joint). The device with its three buttons is introduced through these orifices, with the help of specific pins. The fracture is reduced indirectly, pushing the proximal fragment downwards to its anatomical location by digital pressure while abducting the arm; once it has been reduced in the desired place, the sutures are fastened, closing the fascia and the deltopectoral musculature (Fig. 2a and b). The skin is closed with a continuous intradermal suture, which is removed after approximately 15 days.
Case number 9. (A) Intraoperative image showing the anatomical reduction of the fracture (blue arrow) and the disposition of the implant in the proximal clavicle (D-CLA: distal clavicle; P-CLA: proximal clavicle; Co: coracoid). (B) Postoperative check shown in the anteroposterior projection of the shoulder.
The postoperative protocol involves immobilisation in a sling in internal rotation and abduction for one month, allowing pendular movements from the first postoperative day. Limited elevation and abduction movements at 90° are allowed from the third week, and complete articular balance from the sixth week. Muscle strength potentiation is allowed from week 12. Contact sport or intensive physical activity is not allowed until the sixth month.
Statistical analysisA descriptive analysis was made of each variable, and the data shown as arithmetic mean±standard deviation with the range in brackets. Fisher's exact test was used to analyse the relationship between 2 categorical variables. Mann–Whitney's U test was used to establish any differences between means of dichotomous qualitative variables. Kruskal–Wallis test was used to check equality between means of non-dichotomous variables. SPSS software, version 19.0, (IBM Corp, Armonk, NY, U.S.A.) was used for the statistical analysis. P<0.05 was considered a statistically significant level.
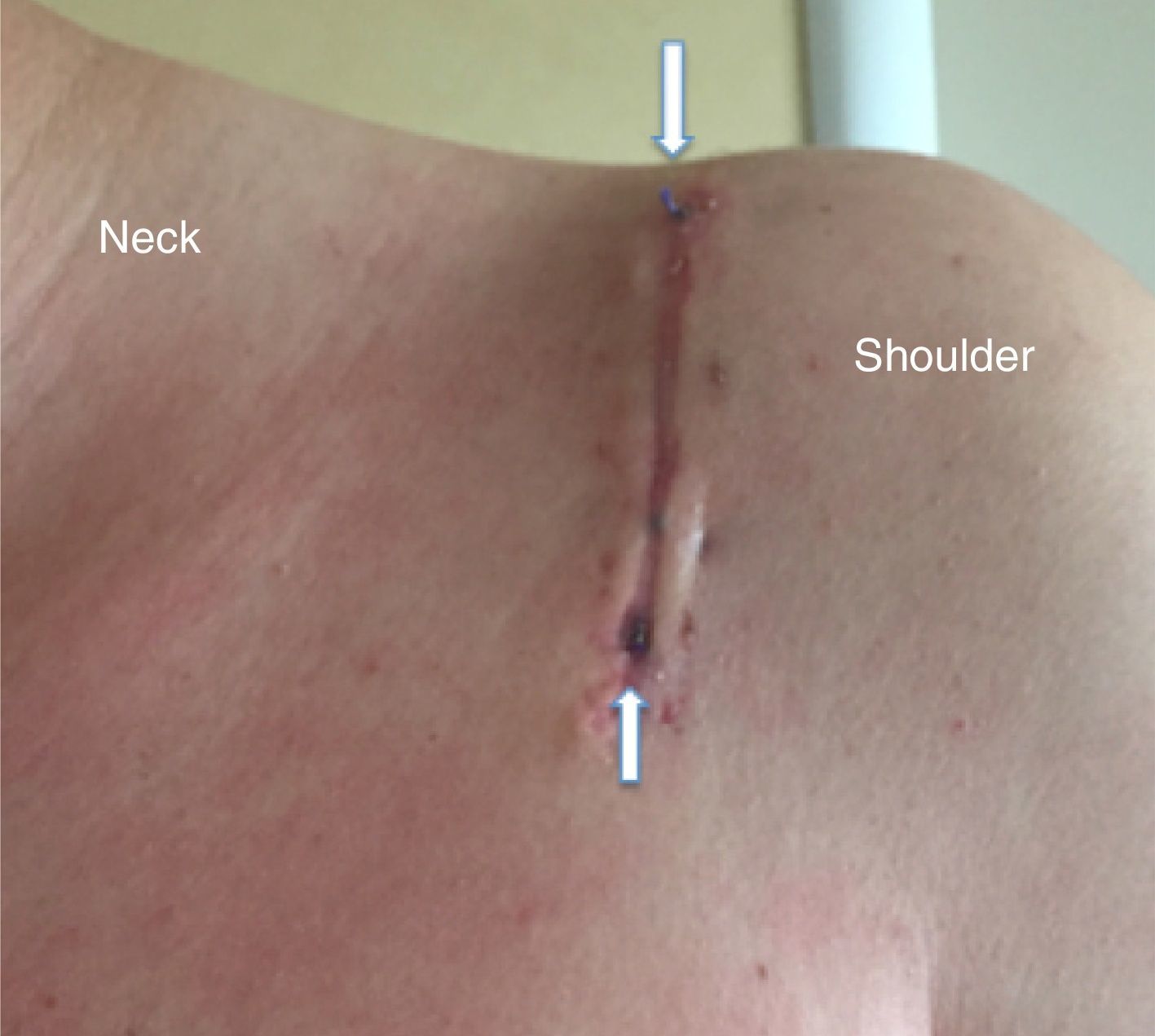
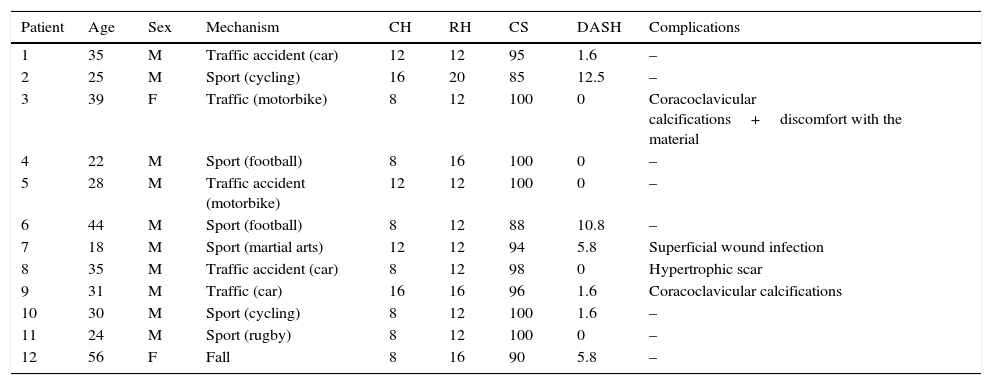
ResultsThe mean time to clinical healing was from 10.3±3.1 weeks (range, 8–16), and to radiological healing, from 13.6±2.6 weeks (range, 12–20) (Fig. 3a–c). The mean Constant score was 95.5±5.2 points (range, 85–100) and the mean DASH score, 3.3±4.4 points (range, 0–12.5). No major complications presented, such as reduction losses, fractures around the implant or deep infections. There were minor complications: one superficial surgical wound infection which was resolved with oral antibiotics (8.3%), one patient developed a hypertrophic scar with a poor cosmetic result (8.3%) (Fig. 4), another patient experienced discomfort with the clavicular buttons (8.3%), and another 2 patients showed calcifications in the coracoclavicular space on X-ray (16.6%) (Table 1; Fig. 5). No patient required reoperation to remove the implant. The patients resumed their usual activities prior to the injury at 15±3.8 weeks (range, 12–20) with no restrictions, and returned to sport from the sixth month in all cases. The mean surgery time was 53.8±11.6min (range, 42–81). There were no cases of non-union, degenerative joint changes or the presence of fractures around the triple button system orifices during follow-up. There was no statistically significant association between, sex, age, injured side or causative mechanism with the clinical outcomes (test score), radiological outcomes (clinical healing) or the onset of complications.
Epidemiology and outcomes of the cases in this review.
| Patient | Age | Sex | Mechanism | CH | RH | CS | DASH | Complications |
|---|---|---|---|---|---|---|---|---|
| 1 | 35 | M | Traffic accident (car) | 12 | 12 | 95 | 1.6 | – |
| 2 | 25 | M | Sport (cycling) | 16 | 20 | 85 | 12.5 | – |
| 3 | 39 | F | Traffic (motorbike) | 8 | 12 | 100 | 0 | Coracoclavicular calcifications+discomfort with the material |
| 4 | 22 | M | Sport (football) | 8 | 16 | 100 | 0 | – |
| 5 | 28 | M | Traffic accident (motorbike) | 12 | 12 | 100 | 0 | – |
| 6 | 44 | M | Sport (football) | 8 | 12 | 88 | 10.8 | – |
| 7 | 18 | M | Sport (martial arts) | 12 | 12 | 94 | 5.8 | Superficial wound infection |
| 8 | 35 | M | Traffic accident (car) | 8 | 12 | 98 | 0 | Hypertrophic scar |
| 9 | 31 | M | Traffic (car) | 16 | 16 | 96 | 1.6 | Coracoclavicular calcifications |
| 10 | 30 | M | Sport (cycling) | 8 | 12 | 100 | 1.6 | – |
| 11 | 24 | M | Sport (rugby) | 8 | 12 | 100 | 0 | – |
| 12 | 56 | F | Fall | 8 | 16 | 90 | 5.8 | – |
CH, clinical healing (weeks); RH, radiological healing (weeks); CS, Constant-Murley Score; DASH, Disabilities of the Arm, Shoulder and Hand; M, male; F, female.
The definitive treatment for distal-third clavicular fractures, more specifically Neer type II-b fractures, remains a challenge. In any case, due to instability and the multiple deforming forces that act on the fracture site, surgical treatment is the best therapeutic option,6,19,20 since rates of over 14% of symptomatic pseudoarthrosis in young patients are not acceptable.21,22
The different ways of radiographically assessing these fractures (projections with or without load, purely anteroposterior or with degrees of tilt),23 and the different clinical tests used in the different studies (Constant-Murley Score18, DASH19, Taft Score24, ASES20, UCLA25, Oxford26 or MSRS27), make comparison difficult.
Two main groups of surgical techniques are used for treatment: those that attempt direct healing by rigid fixation (traditional osteosynthesis, with different types of plates) and those that attempt indirect healing by flexible fixation (different coracoclavicular fixation systems, some of which can be performed arthroscopically). Most of the techniques used have provided good outcomes in terms of clinical and radiological healing, although to date no technique has proved superior to another. The problem with these techniques is essentially down to the material (intolerance, movement, infection), inadequacy of the technique (reduction loss) or articular damage (acromioclavicular arthrosis).
Transfixation systems14,28,29 associated or otherwise with tension band30 are problematic in that they can damage the acromioclavicular joint, and can generate secondary arthrosis. With all of them the material has to be removed before starting complete range of movement since, as they interfere with normal scapular rotation, they can fail and break. Another problem with them is that the pins can migrate31 (80% in some series), they can become infected, and they can prove inadequate in maintaining suitable reduction in up to 10% of cases.32 The coracoclavicular screw,33 as well as the malleolar screw,8 are not easy to implant, it is also necessary to remove them before they can break. Furthermore, in small coracoids or porous bone there is a failure rate of up to 32%.34 Amongst these systems, hook plating9,35 is a technique that has demonstrated more consistent outcomes and has been used in a greater number of patients.2 It is very useful when the distal fragment is very small and has proved more effective than treatment with Kirschner tension band wiring,36 although it presents more complications than the use of plates together with coracoclavicular cerclage.16,37 The problem is that it is too rigid a technique and it protrudes into subcutaneous tissue, and therefore has to be removed in almost 100% of cases as soon as the fracture has consolidated in order to prevent acromion osteolysis and fracture, injury to the cuff or subacromial conflict.38
Conventional clavicle plates, distal radius plates or the recent preshaped plates have the great advantage of providing rigid fixation, with screws locked to the plate of different sizes and angulations, without affecting the acromioclavicular joint. The main problems with them are the need for wide exposure which can devascularise the clavicle, and the need to remove them due to discomfort produced by the material in between 17% and 45%.24,39,40 Another problem is that fractures due to weakness (stress shielding) in the site of the screw orifices34 can occur when they are removed. On other occasions, the lateral fragment is so small and comminuted that an insufficient number of screws can be put into the frame (at least 2 bicortical screws)39 to ensure stability, which has to be supplemented with another coracoclavicular technique.41
Isolated coracoclavicular cerclages (1 or 2), secured to harpoon suture anchors in the coracoid or otherwise, have also proved effective, although they present frequent reduction losses42 with the added risk of “wearing down” and causing a differed fracture to the clavicle itself in 11% of cases.43,44 These techniques performed arthroscopically have provided satisfactory outcomes, but require a high learning curve in order to perform them effectively.45,46 The use of combined techniques has become more widespread47,48: plates with coracoclavicular cerclage using harpoon suture anchors,16,49 harpoon suture anchors for coracoclavicular suture with transarticular fixation14,25,27 or plates with TightRope-type systems.1 Although the outcomes of these combinations are satisfactory, they involve greater financial cost, make surgery more complex as various techniques are used, and they increase the risk of devascularising fragments in order to be able to implant the 2 systems correctly. Robinson et al.20 used a simple TightRope system (double button) by open surgery; this shares the advantage with our technique of theoretically not having to remove the implant, but had a 6.25% incidence of non-unions, which we did not experience in our series. This might be due to the fact that this system is not effective in treating more complex injuries with greater tissue damage.
The literature describes clinical healing as taking place from the sixth32,33,37,50 to the fourteenth25 week if there are no complications, which coincides with the data obtained in this review. In our series, clinical healing always preceded radiological healing (around 3.4 weeks), as also described by Abdeldayem et al.,50 since soft tissues heal before radiological changes are visible. In fact, as it is an anatomical and stable reduction, consolidation is essentially per primam, and therefore a large bone callous would not be expected to appear.
The triple button system, initially designed to treat acute acromioclavicular dislocation and demonstrated to be effective in the laboratory,51 recreates the anatomy of the coracoclavicular ligaments. We have not found previous use of the system for this type of injury in the literature. For us this system has several advantages compared to others, as follows:
- (1)
Mechanical. The orthogonal disposition of the implant in 2 planes of the space at clavicle level enables the function of the conoid ligament to be supplanted and the injured remainder of the trapezoid ligament to be supported, providing more stability than the simple coracoclavicular systems.52,53 This technique enables the forces of the arm and the scapula to pass from the coracoids to the medial fragment, reducing the forces that act on the fracture site.
- (2)
Biological. An indirect reduction of the fracture site is made, size and lateral fragment comminution are not important. The injury site is cleaned without stripping the periosteum, maintaining the soft tissue insertions which might be essential for the injury to heal and for it to consolidate earlier, avoiding consolidation delays and pseudoarthrosis; this is an advantage compared to the use of plates. Furthermore, not crossing the joint prevents secondary articular damage, and therefore the stiffness and capsulitis described in other studies.2
- (3)
Technical. This technique is fast (less than one hour's surgery), safe (everything takes place under direct vision) and easy (at no time does the distal fragment need to be manipulated, which is often comminuted and difficult to synthesise).
- (4)
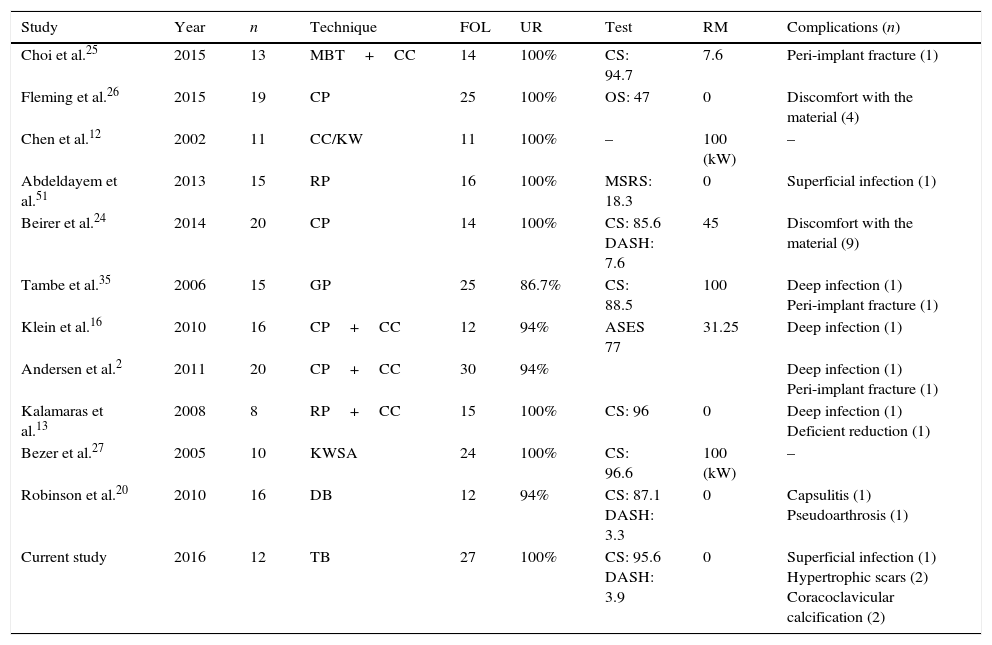
Clinical. The clinical test scores show outcomes that are at least equal to those described after the traditional techniques (Table 2). There is less neurovascular risk than with the arthroscopic techniques and traditional coracoclavicular cerclages, because the orifice in the coracoid is made under direct vision and there is no need to pass through any element medial to it. We did not need to reoperate any of the patients to remove the material, which reduces morbidity. Despite the subcutaneous position of the clavicle, the low profile of the implants means that the material implanted in it does not protrude through the skin, cause discomfort or even hurt when certain movements are made. Even so, one patient in the series, slim (with little adipose panicle), presented discomfort with the clavicular buttons, but this did not warrant their removal. All the patients were able to resume their previous activities with no restrictions.
Table 2.Comparison of our review with studies published in the literature.
Study Year n Technique FOL UR Test RM Complications (n) Choi et al.25 2015 13 MBT+CC 14 100% CS: 94.7 7.6 Peri-implant fracture (1) Fleming et al.26 2015 19 CP 25 100% OS: 47 0 Discomfort with the material (4) Chen et al.12 2002 11 CC/KW 11 100% – 100 (kW) – Abdeldayem et al.51 2013 15 RP 16 100% MSRS: 18.3 0 Superficial infection (1) Beirer et al.24 2014 20 CP 14 100% CS: 85.6
DASH: 7.645 Discomfort with the material (9) Tambe et al.35 2006 15 GP 25 86.7% CS: 88.5 100 Deep infection (1)
Peri-implant fracture (1)Klein et al.16 2010 16 CP+CC 12 94% ASES 77 31.25 Deep infection (1) Andersen et al.2 2011 20 CP+CC 30 94% Deep infection (1)
Peri-implant fracture (1)Kalamaras et al.13 2008 8 RP+CC 15 100% CS: 96 0 Deep infection (1)
Deficient reduction (1)Bezer et al.27 2005 10 KWSA 24 100% CS: 96.6 100 (kW) – Robinson et al.20 2010 16 DB 12 94% CS: 87.1
DASH: 3.30 Capsulitis (1)
Pseudoarthrosis (1)Current study 2016 12 TB 27 100% CS: 95.6
DASH: 3.90 Superficial infection (1)
Hypertrophic scars (2)
Coracoclavicular calcification (2)KW, Kirschner wires; KWSA, Kirschner wires plus harpoon suture anchor; ASES, American Shoulder and Elbow Surgeons; MBT, modified tension band; CC, coracoclavicular cerclage; CS, Constant-Murley Score; DASH, Disabilities of the Arm, Shoulder and Hand; DB, double button; RM, removal of material; MSRS, Modified Shoulder Rating Scale; n, number of cases; OS, Oxford Score; CP, clavicle plate; GP, hook plate; RP, radius plate; Fol, follow-up in months; TB, triple button; CS, coracoclavicular screw; UR, rate of clinical-radiological union in percentage.
- (5)
Financial. As a second operation was not required, we avoided the costs of further intervention, associated sick leave and possible complications.
The main radiological complication of the triple button system was the appearance of calcifications – already described in other studies with rates of 7–12%14—although this is not associated with poorer clinical outcomes and, as in the case of acromioclavicular dislocation, might be no more than the organism attempting to stabilise an injured joint. The appearance of a hypertrophic scar is explained by the anatomical location of the operation, because the shoulder area is more likely to develop these types of scars. This results in poorer cosmetic results but not in poorer clinical outcomes. We had one superficial wound infection that responded to conservative treatment; this is a possibility inherent to any surgical procedure and appears in practically all the series described in the literature. Our rehabilitation protocol does not differ greatly from those described in the literature, it being important to find a balance between the immobilisation time – which should not be excessive so as to avoid scapular dyskinesis 54—and movement sequences once healing is underway. This injury is defined as a bone fracture, but is principally a ligament problem with the instability it generates; therefore any system must provide sufficient rigidity without excessively damaging the tissue insertions so that the bone can consolidate correctly.
This study has a series of limitations. Firstly, it is a retrospective observational study; secondly, it presents a low number of patients, since the frequency of the injury makes long series with a minimum follow-up difficult in order to be able to compare surgical techniques with sufficient scientific evidence2; thirdly, the lack of a control group to compare outcomes limits the validity of the conclusions. Therefore, prospective and comparative studies with a greater number of cases are necessary to clarify which technique offers the best outcomes in the management of these injuries.
ConclusionsThe triple button system is an alternative to the more conventional methods for the treatment of Neer type II-b distal-third clavicular fractures. It is reproducible and effective, both clinically and radiologically. Its main advantage is that a second intervention is not required to remove it.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of people and animals subjectsThe authors declare that neither human nor animal testing have been carried out under this research.
Confidentiality of dataThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
FundingThere was no source of funding available to undertake this study.
Conflict of interestsThe authors have no conflict of interest to declare in preparing and submitting this article.
To the department of Orthopaedic Surgery and Traumatology of the General University Hospital Los Arcos del Mar Menor.
Please cite this article as: Cano-Martínez JA, Nicolás-Serrano G, Andrés-Grau J, Bento-Gerard J. Tratamiento de fracturas de tercio distal de clavícula (tipo ii-b de Neer) con sistema de triple botón. Rev Esp Cir Ortop Traumatol. 2016;60:378–386.