The aim of this study is to determine the different therapeutic options described for the treatment of radioulnar synostosis, and report our experience with posterior interosseous antegrade flow pedicled flap with technical amendments. Two patients, who were treated with the designed flap, and with more than one year of follow-up, were reviewed. The technical innovations, end result and complications are described. In the two cases described, there was no recurrence of synostosis, which is the most frequent complication described in this condition, and no postoperative complications were observed. In the literature, many filler materials, from artificial to biological, free or vascularized, have been used the radioulnar space after excision of synostosis. The technique that provides the best results is the interposition of muscle or vascularized adipofascial flaps. The interosseous posterior antegrade flow pedicled flap is reliable, with a low morbidity, and is an effective alternative for the treatment of proximal radioulnar synostosis.
Nuestro objetivo es estudiar las diferentes opciones terapéuticas descritas para el tratamiento de la sinostosis radiocubital y, aportar nuestra experiencia con las modificaciones técnicas introducidas con posterioridad. Hemos revisado 2 pacientes con más de un año de evolución, que fueron operados con el colgajo reseñado; describimos las novedades técnicas, el resultado final y las complicaciones. En los 2 casos descritos existe ausencia de recidiva de sinostosis, complicación más frecuente descrita en esta enfermedad, con ausencia de complicaciones postoperatorias. En la literatura se han empleado numerosos materiales interpuestos en el espacio radiocubital tras la exéresis de la sinostosis, desde artificiales hasta biológicos libres o vascularizados; siendo la técnica de interposición de colgajos musculares o adipofascial vascularizados, la que ofrece los mejores resultados. El colgajo interóseo posterior pediculado de flujo anterógrado es una alternativa fiable, de poca morbilidad y, efectiva para el tratamiento de la sinostosis radiocubital proximal.
Radioulnar synostosis is a heterotopic ossification of the interosseous membrane of the forearm which blocks rotational movements, representing a significant limitation for basic everyday activities.1 Its origin can be congenital or posttraumatic.
The most common form is the congenital, with posttraumatic occurrence being relatively uncommon. The true incidence of posttraumatic radioulnar synostosis is unknown, but it is estimated to appear in 1.22–6.6%3 of patients with fractures of one or both forearm bones treated with compression plates. In addition, there are other risk factors arising from the type of local lesion (open fracture, comminution and associated dislocations), surgical technique (approaches,4 immobilization or repair of the distal biceps insertion in up to 7%5,6) and other distant lesions and the condition of patients (traumatic brain injury [TBI], in up to 18% of cases7).
This lesion can be located along the various thirds of the forearm. Its length in the proximal third can vary and affect the elbow joint.
Multiple treatment alternatives have been proposed, with the surgical option being the first choice. Isolated resection of the calcifications has a high rate of recurrence, so various techniques for interposition of artificial or biological material to act as a barrier between both bone surfaces have been developed. Traditionally, materials such as silicone,8–10 bone wax11 and soft parts like free fat11–13 have been used. However, these techniques were not able to prevent recurrence and non-vascularized14 tissue could be replaced by necrotic tissue. Subsequently, especially in the cases of congenital synostosis, interposition techniques using vascularized tissue from the anconeus,15brachioradialis and flexor carpi ulnaris muscles,16 vascularized, pedicled or free flaps17,18 were employed using the radial or posterior interosseous artery.19–23
The use of posterior interosseous adipofascial flaps in radioulnar synostosis with a posttraumatic origin has been sparsely described prior to article.19,22,23 This highly useful flap was originally described by Zancolli and Angrigiani in 1988,24 and Penteado et al. in 1986.25
Multiple adjuvant treatments with NSAIDs have been proposed in conservative treatments, such as indometacin, perioperative irradiation at low doses26,27 and postoperative rehabilitation which may prevent recurrence.
We present 2 cases in which we used the adipofascial posterior interosseous flap with antegrade flow to interpose it as biological material at the focus of synostosis following its excision in order to prevent recurrence of the lesion.
Case reportsCase 1A 45-year-old male who suffered a posttraumatic rupture of the biceps brachii insertion tendon at the level of the radial tuberosity in his left arm while carrying out his work activities, without any other associated injuries. Tendon reinsertion was performed using 2 metal harpoons and posterior rigid immobilization was established for 4 weeks.
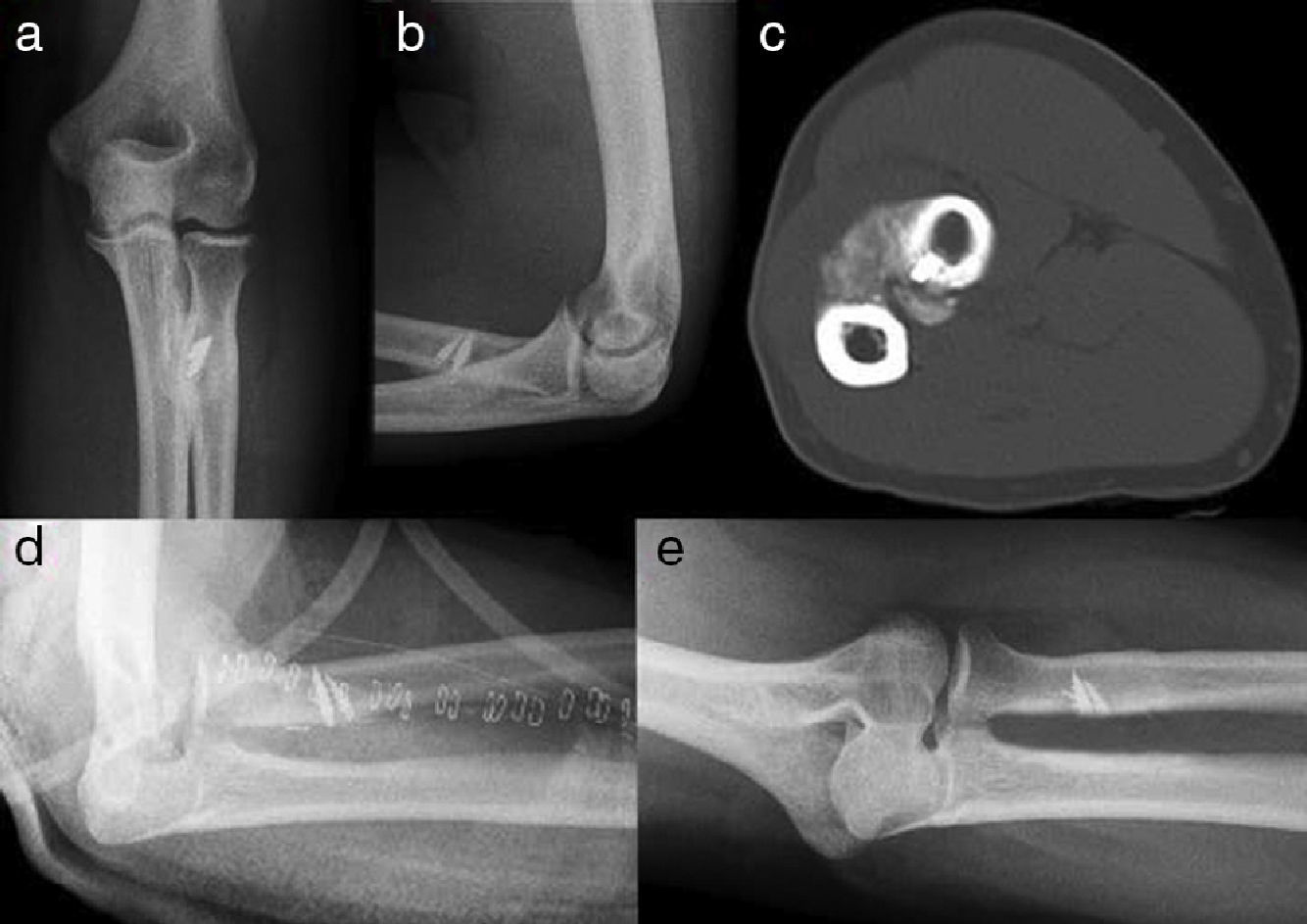
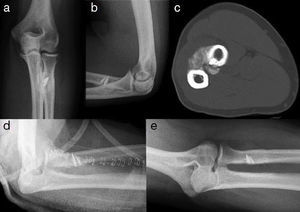
During the rehabilitation process, the patient presented a blockage of forearm pronosupination at 75° pronation. Plain radiographs (anteroposterior and lateral) and a computed tomography (CT) scan of the affected elbow were obtained, showing a bone bridge in the proximal third of the radius and ulna at the level of the radial tuberosity (Fig. 1). The patient was diagnosed with radioulnar synostosis, type III in the Vince classification28 or proximal type IIIA in the Jupiter classification.11
Images (a) and (b) show anteroposterior and lateral radiographs, whilst (c) is the CT scan showing the synostosis generated after the implantation of harpoons for the reinsertion of the biceps tendon. The inferior line shows the radiographs in the postoperative period (d) and at 1 year (e) with absence of synostosis.
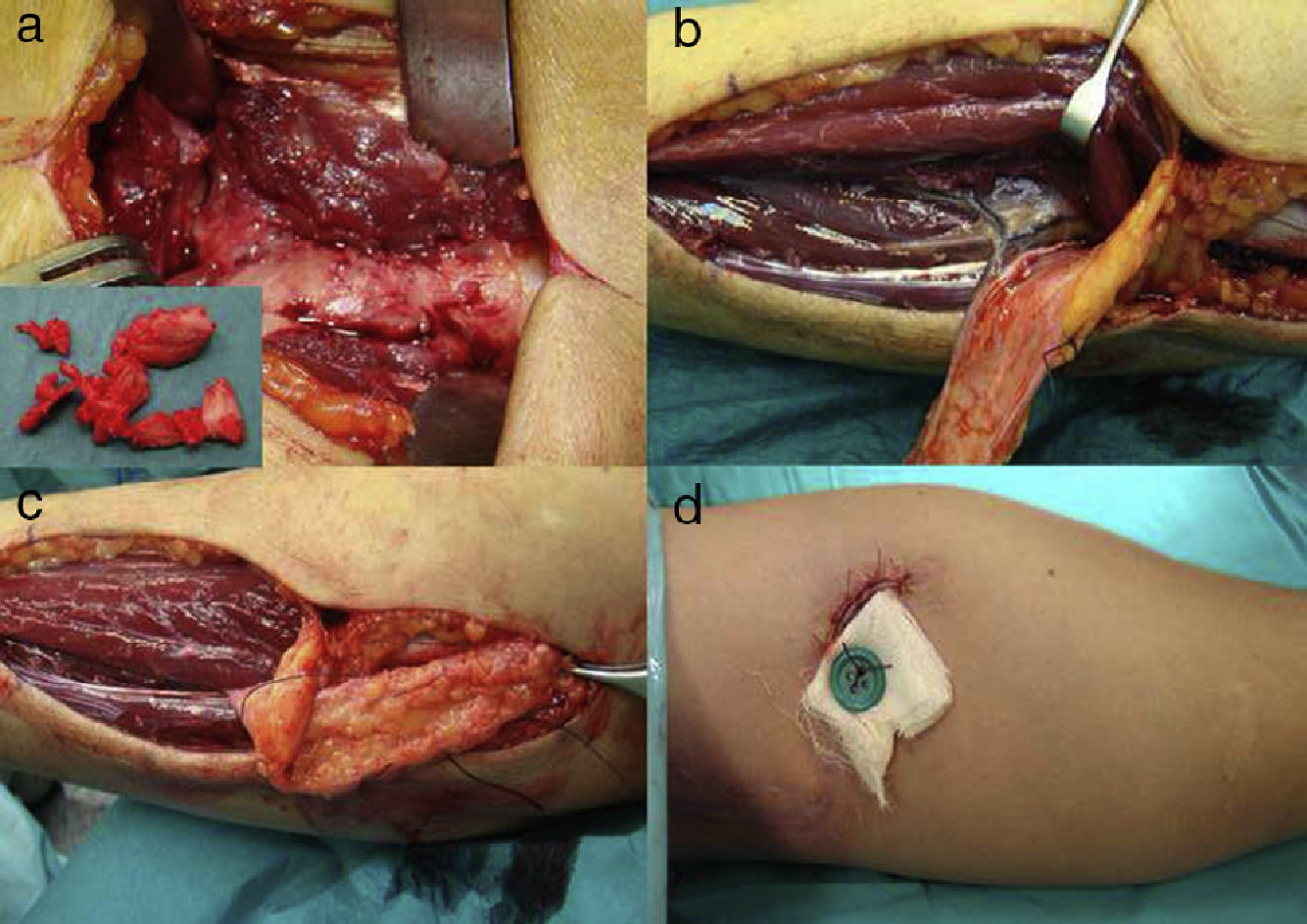
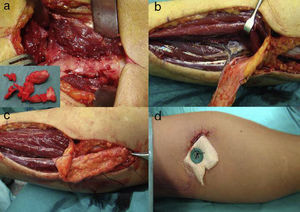
The patient was scheduled for surgery (Fig. 2), which was carried out through a posterior forearm approach which enabled excision of the heterotopic calcifications. Recovery of the passive rotational movement of the forearm, with full articular balance, was verified immediately.
The image (a) shows the synostosis (fragments of the synostosis are in smaller size), and (b) the flap with the posterior interosseous artery and perforating septal. The image (b) also shows the everted flap to be interposed in the area of synostosis, and the (d) anterior cutaneous anchor which stabilizes the flap.
Subsequently, we performed an interosseous posterior fascio-fatty flap with antegrade flow through distal extension of the posterior approach, and an 8-10cm dissection of the subcutaneous fascio-fatty plane between the extensor carpi ulnaris and extensor digiti minimi including the septum between both where the posterior interosseous artery, along with its vein, was located. A 6-8cm wide adipofascial pedicled flap with antegrade flow was obtained. Next, it was turned 180° so that the distal third of the flap could be interposed at the site of calcification between both bones, in order to prevent recurrence of the lesion. A small anterior incision was made to recover the flap and attach it to the skin through suture and a dermal button, so it prevented mobilization and retraction of the interposed tissue and allowed patient rehabilitation to start as early as possible. The approximate duration of the surgical intervention was 120min.
Postoperative immobilization of the elbow was maintained for 1 week and mobilization of the joint was started immediately thereafter.
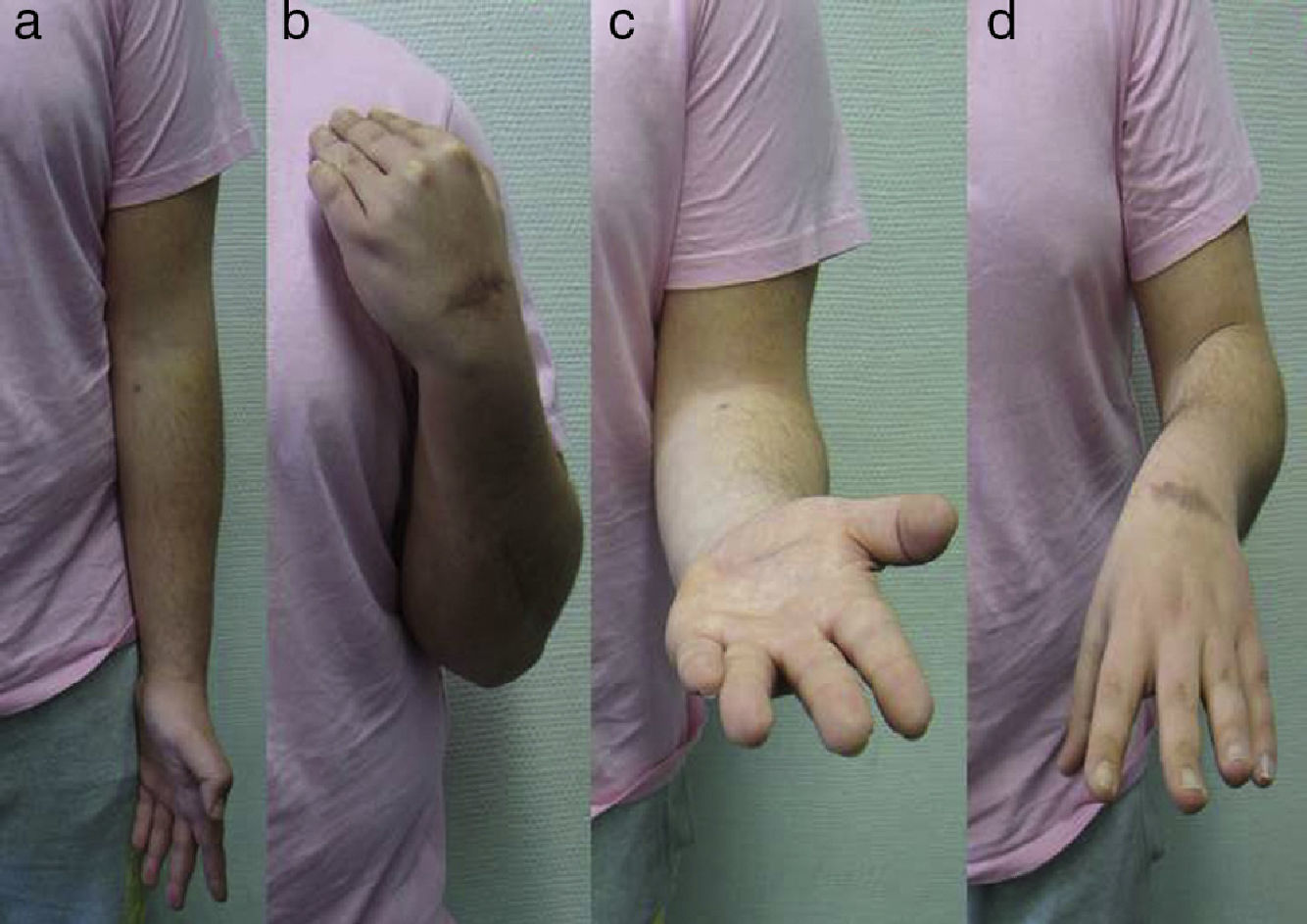
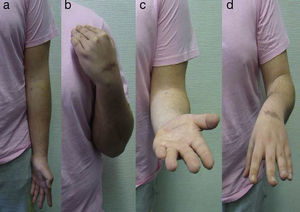
The patient presented satisfactory functional results during monitoring in consultation. At 3 months, the patient was able to perform 75° pronation (contralateral value of 75°) and 75° supination (contralateral value of 85°) (Fig. 3) which were maintained until discharge. The radiological control conducted in the immediate postoperative period (Fig. 1) and 1 year later showed no recurrence of the synostosis bone bridge.
No complications, such as infection, hematoma and distal neurovascular involvement, were observed. The range of motion was maintained until discharge 1 year after surgery. The patient was satisfied with the results and was able to return to his previous employment.
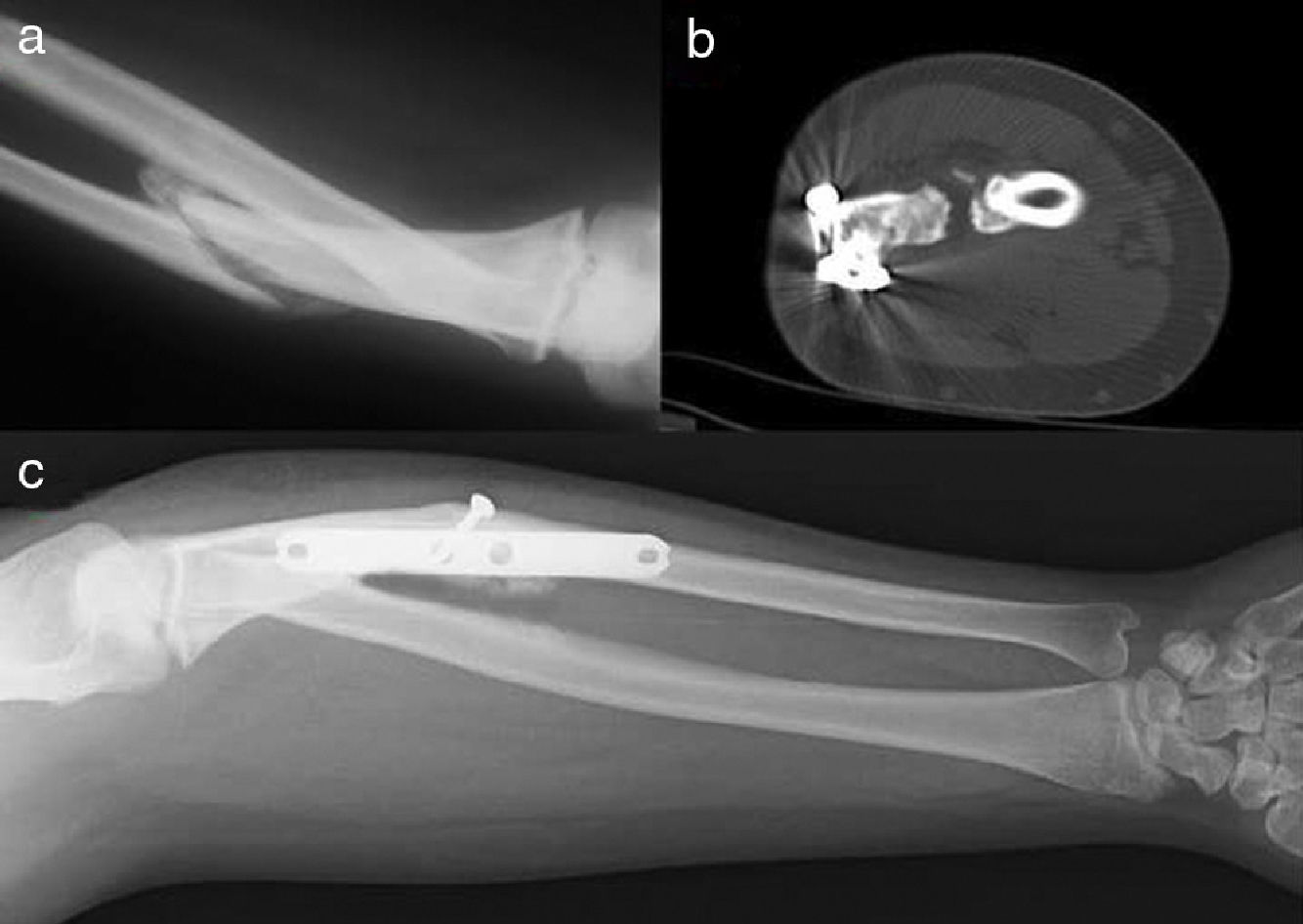
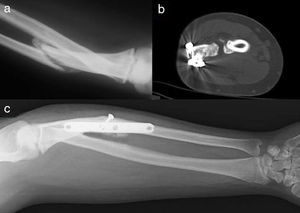
Case 2A 23-year-old male, who suffered TBI due to a motorcycle accident, requiring ICU admission and mechanical ventilation for 19 days. At 5 weeks after the accident he attended consultation due to deformity and functional limitation of the left forearm, with a blockage in 50° pronation. We obtained simple radiographs (Fig. 4) which showed malunion in shortening-rotation of the ulna with hypertrophic callus and proximal type IIIA radioulnar synostosis.11
The patient underwent focal osteotomy, excision of the hypertrophic callus plus the synostosis, osteosynthesis with a plate and posterior interosseous fascio-fatty flap, as described for the first case.
The patient presented satisfactory functional results during the follow-up visit. At 3 months, he reached 70° pronation (contralateral value of 75°) and 80° supination (contralateral value of 85°). Postoperative radiographs and a CT scan (Fig. 4) showed a fracture callus with no presence of synostosis.
No complications, such as infection, hematoma and distal neurovascular involvement, were observed. The range of motion was maintained until discharge, 1 year after surgery. The patient was satisfied with the results and returned to his previous employment.
DiscussionRadioulnar synostosis is rare in its congenital form, but even rarer as a posttraumatic complication. It produces major joint limitation for patients, making it a very disabling injury.
The recurrence rate after simple excision is high. Based on 3 extensive cases series, after excision of a primary synostosis this rate was 32%.16,29
In 2002, Kamineni et al.30 suggested proximal resection of the radius for cases with severe posttraumatic proximal radioulnar synostosis where it was not possible to excise the synostosis, with a mean rotational range of 98° during follow-up. Thus, it was considered that flaps or interposition techniques may not be necessary.
After using some artificial materials, like silicone, or non-vascularized biological materials, such as fat and fascia, the interposition of vascularized grafts was reported. In 1999, Bell and Benger15 reported 3 patients with type III radioulnar synostosis who were successfully treated through a vascularized graft of anconeus muscle interposed after excision which improved forearm rotational range up to 130°. In 2004, Fernandez and Joneschild16 used a brachioradialis flap in 3 cases and a flexor carpi ulnaris flap in 2 cases, with excellent results.
In 1998, Kanaya and Ibaraki17 described a vascularized adipofascial free graft from the side of the arm dependent on the posterior radial collateral artery in 7 children with congenital proximal radioulnar synostosis, with rotation ranges of 71° upon monitoring. In 2004, Muramatsu et al.18 reported 2 patients with posttraumatic radioulnar synostosis treated by interposition of a vascularized inguinal free graft, with ranges of 130° in both cases. Although the results of the interposition of vascularized free grafts were promising, they did require expertise in microsurgery and could cause morbidity in the donor region.
The interposition of vascularized pedicled grafts, such as radial or posterior interosseous flaps, seems to be a good alternative to the previously described techniques. These flaps are safe and relatively simple to obtain, without requiring microsurgical anastomosis. Few cases of radioulnar synostosis treated through vascularized pedicles flaps have been described to date, especially in children.
In 1996, Sugimoto et al.19 presented a case of posttraumatic type III radioulnar synostosis treated by resection and interposition of a posterior interosseous flap. However, 1 year later the patient presented a rotational range of only 65°. In 2004, Funakoshi et al.20 described a patient with congenital bilateral radioulnar synostosis treated with a pedicled posterior interosseous fat graft, obtaining a rotational balance of 60° pronation and 10° supination for both forearms. In 2004, Jones et al.21 presented a patient with posttraumatic type II synostosis, successfully treated by resection and interposition of a radial adipofascial flap. In 2007, Jones et al.22 reported excellent results in 4 children treated with posterior interosseous proximal base adipofascial flaps. Recently, in 2011, Sonderegger et al.23 described 6 patients with posttraumatic radioulnar synostosis, 5 type III and 1 type I, treated by resection and interposition of a pedicled adipofascial flap, 4 of the radial artery and 2 of the posterior interosseous, with excellent results and a mean rotational range of approximately 140°.
The use of the radial artery for these types of flaps may affect the distal vasculature, resulting in donor site morbidity. Moreover, it poses anatomical difficulties that limit its use in cases of proximal radioulnar synostosis.
Pedicled adipofascial flaps of the proximal base with posterior interosseous or antegrade flow can be obtained without great difficulties, following the directions proposed by Penteado et al. in 198625 and Zancolli and Angrigiani in 1988.24 The distal apex allows them to be turned on themselves to be moved proximally to their pedicle and used in the proximal third of the forearm. We recognize that obtaining this flap requires an extensive surgical approach in the dorsal aspect of the forearm, compared to that required for a simple excision of the synostosis, although none of our patients expressed their concern about this issue.
We believe that the attachment of the flap to the affected area is a very important part of this technique. Most authors leave the vertex of the flap interposed in the affected region without any anchor. Others prefer to use suture anchors to prevent flap retraction. In our case, the system of percutaneous anchor with a button guarantees the interposition without any risk of retraction and without adding new fixation material in the affected region, which we believe could enhance the onset of new heterotopic ossification in the area.
Excision of the lesion along with the interposition of a posterior interosseous flap with antegrade flow and anterior percutaneous anchor is a valid technique for the treatment of posttraumatic radioulnar synostosis located in the proximal third of the forearm, with excellent functional results and a low rate of recurrence.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Please cite this article as: Martínez-Martínez F, Moreno-Fernández JM, García-López A, Izquierdo-Santiago V, Illan-Franco S. Tratamiento de la sinostosis mediante colgajo interóso posterior. Rev Esp Cir Ortop Traumatol. 2014;58:120–124.