Volar fixed-angle plates (VFAP) are currently widely used for the treatment of extra-articular distal radius fractures. Using these plates has a high risk of articular and dorsal screw protrusion due to their special configuration. The aim of this study is to assess the validity of the standard X-rays, performed with the help of wedged supports, in order to detect articular and dorsal screw protrusion. A comparison with computed tomography (CT) scan imaging has been made. The outcome of 26 patients with distal radius articular fracture, treated with a VFAP, is reported. Good correlation between modified X-rays and CT scan was observed. A sensitivity of 100% for articular protrusion and 66% for dorsal has been obtained. When detecting screw protrusion at the distal radius, the use of wedged supports to perform special X-rays intraoperatively is an effective tool.
El tratamiento de las fracturas intraarticulares del radio distal mediante placas volares de ángulo fijo (PVAF) está ampliamente difundido en la actualidad. El uso de estas placas, debido a su peculiar configuración, conlleva un elevado riesgo de protrusión de los tornillos a nivel intraarticular y dorsal. El objetivo de nuestro trabajo es determinar la validez de las proyecciones radiológicas habituales, realizadas con la ayuda de soportes en forma de cuña, para detectar la protrusión de los tornillos a nivel intraarticular y dorsal, utilizando la tomografía axial computarizada (TAC) como prueba de referencia. En el estudio se presentan los resultados obtenidos en 26 pacientes tratados de una fractura articular de radio distal mediante una PVAF, modelo DVR®. Se ha observado una correlación satisfactoria entre los resultados de las radiografías con soportes cuando han sido comparadas con la TAC, con una sensibilidad del 100% para las protrusiones intraarticulares y del 66% para las protrusiones dorsales. Se recomienda la realización de estas proyecciones especiales de muñeca como una herramienta intraoperatoria útil para detectar la protrusión de los tornillos en las PVAF.
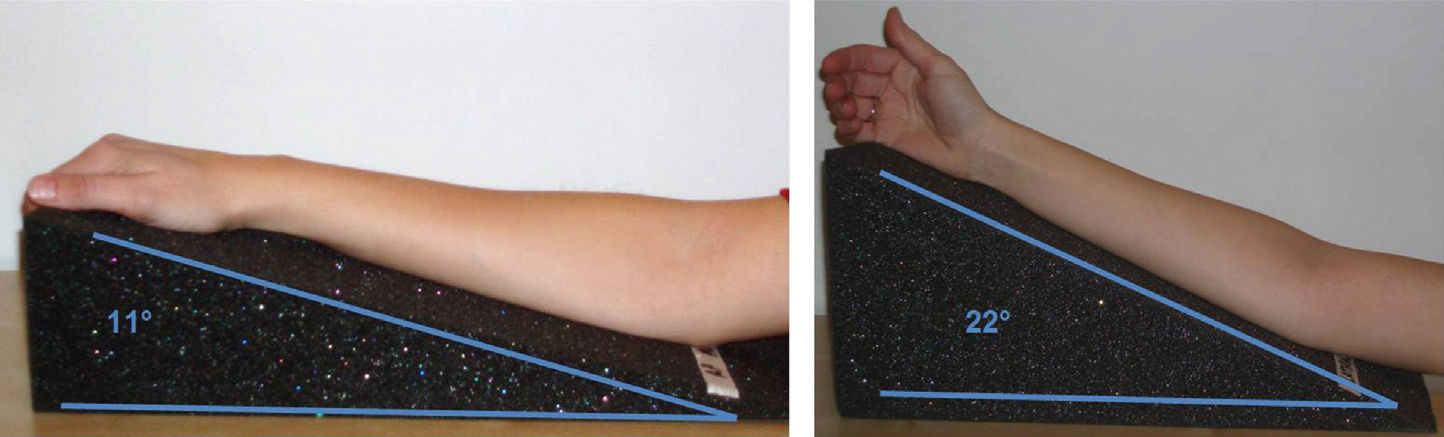
Osteosynthesis of distal radius fractures with a volar fixed-angle plate (VFAP)1,2 involves the risk of protrusion of the screws, which can invade the joint space or pierce the dorsal cortex. Tendon complications derived from dorsal protrusion are currently well documented.3–5In our department we have used the DVR® plate for the treatment of distal radius joint fractures since its introduction. Inadvertent protrusion of the screws is not uncommon, given the three-dimensional, diverging configuration of the screws of the DVR® plate, like that of many other VFAP, and the peculiar shape of the distal radius. This should be avoided during surgery through a careful radiological examination, which should take into account the natural, specific angulations of the distal radius: 11° palmar tilt and 22° ulnar tilt.6,7
Suspicion of protrusion of a screw during the postoperative follow-up period is difficult to confirm through a conventional radiographic study with anteroposterior (AP) and lateral (L) projections, since these are routinely performed without taking into account the aforementioned specific angulations. In general, it is necessary to conduct studies by computed tomography (CT) in order to determine if protrusion is truly present. Our group has developed a model of wedge-shaped supports which facilitate correct radiographic studies in order to obtain radiographs which are tangential to the joint surface of the distal radius.
The objective of this study is to evaluate the usefulness of special radiographic projections, with the aid of wedge-shaped supports, to detect intra-articular and dorsal protrusion of VFAP screws, using the CT diagnostic test as a reference.
Materials and methodsOut of all patients undergoing VFAP surgical interventions for distal radius fractures in our service, 26 agreed to participate in the study. We obtained informed consent in all cases. We conducted a physical examination of both wrists, measuring active palmar flexion, active and passive dorsal extension, ulnar and radial deviation and grip strength with a Jamar® dynamometer. We assessed 2 subjective parameters: pain measured by a visual analog scale (VAS) and satisfaction index expressed on a numerical scale from 0 to 10, with 0 representing total dissatisfaction and 10 representing the maximum possible satisfaction.
Following the examination, we conducted studies with 2 specific scales to assess independence and mobility of the affected upper limb: the Quick Dash8 scale and the Mayo9 wrist scale.
Radiographs (Rx) of each operated wrist were obtained using AP and L projections. Both projections were obtained by positioning wrists on wedge-shaped supports, designed for this study. The supports had inclinations of 11° and 22°, so as to obtain Rx which were tangential to the joint surface of the radius in the AP and L projections, respectively (Fig. 1).
We requested a multisection CT scan of all patients, obtaining images in all 3 dimensions. This imaging test was considered as the reference against which to compare radiographic images in the AP and L projections.
The evaluation of the images from the plain radiography and the CT scan were performed independently by the 2 researchers, with each patient being assigned a number, and findings were subsequently contrasted.
We defined the following situations:
- •
Absence of any type of protrusion.
- •
Slight articular protrusion of a screw.
- •
Slight dorsal protrusion of a screw.
- •
Clear articular protrusion of a screw.
- •
Clear dorsal protrusion of a screw.
Slight protrusion was considered as the simple prominence of the end of a screw beyond the cortex, whereas clear protrusion was considered when the prominence included the thread of the screw.
The results of the evaluation of the images were entered into an Excel® spreadsheet and statistical analysis was performed using the software package SPSS® for Windows version 15.0 (SPSS Inc., Chicago, IL, USA).
ResultsThe sample consisted of 17 females and 9 males, with a mean age of 58.55±10.12 years (range: 36–76 years). A total of 17 patients suffered left wrist fractures, whereas 9 suffered right wrist fractures.
Of the 26 CT requested we only obtained images from 20 patients, for reasons unrelated to the study (appointment errors and computer problems).
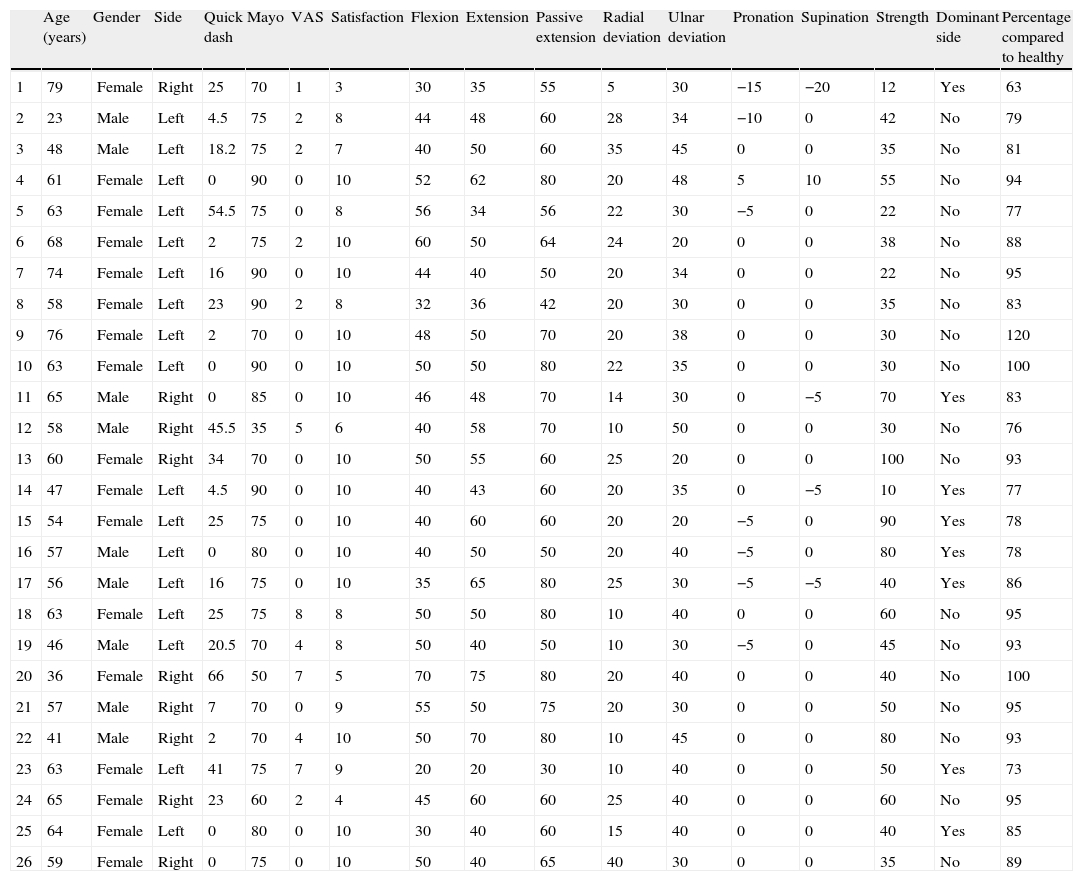
The results of the physical examination are shown in Table 1. Regarding the results of the scales, the Quick Dash presented a mean score of 17.5±18 (range: 0–66), whilst the Mayo wrist scale presented a mean score of 74.5±12.43 (range: 35–90).
Patient data and results of the exploration.
| Age (years) | Gender | Side | Quick dash | Mayo | VAS | Satisfaction | Flexion | Extension | Passive extension | Radial deviation | Ulnar deviation | Pronation | Supination | Strength | Dominant side | Percentage compared to healthy | |
| 1 | 79 | Female | Right | 25 | 70 | 1 | 3 | 30 | 35 | 55 | 5 | 30 | −15 | −20 | 12 | Yes | 63 |
| 2 | 23 | Male | Left | 4.5 | 75 | 2 | 8 | 44 | 48 | 60 | 28 | 34 | −10 | 0 | 42 | No | 79 |
| 3 | 48 | Male | Left | 18.2 | 75 | 2 | 7 | 40 | 50 | 60 | 35 | 45 | 0 | 0 | 35 | No | 81 |
| 4 | 61 | Female | Left | 0 | 90 | 0 | 10 | 52 | 62 | 80 | 20 | 48 | 5 | 10 | 55 | No | 94 |
| 5 | 63 | Female | Left | 54.5 | 75 | 0 | 8 | 56 | 34 | 56 | 22 | 30 | −5 | 0 | 22 | No | 77 |
| 6 | 68 | Female | Left | 2 | 75 | 2 | 10 | 60 | 50 | 64 | 24 | 20 | 0 | 0 | 38 | No | 88 |
| 7 | 74 | Female | Left | 16 | 90 | 0 | 10 | 44 | 40 | 50 | 20 | 34 | 0 | 0 | 22 | No | 95 |
| 8 | 58 | Female | Left | 23 | 90 | 2 | 8 | 32 | 36 | 42 | 20 | 30 | 0 | 0 | 35 | No | 83 |
| 9 | 76 | Female | Left | 2 | 70 | 0 | 10 | 48 | 50 | 70 | 20 | 38 | 0 | 0 | 30 | No | 120 |
| 10 | 63 | Female | Left | 0 | 90 | 0 | 10 | 50 | 50 | 80 | 22 | 35 | 0 | 0 | 30 | No | 100 |
| 11 | 65 | Male | Right | 0 | 85 | 0 | 10 | 46 | 48 | 70 | 14 | 30 | 0 | −5 | 70 | Yes | 83 |
| 12 | 58 | Male | Right | 45.5 | 35 | 5 | 6 | 40 | 58 | 70 | 10 | 50 | 0 | 0 | 30 | No | 76 |
| 13 | 60 | Female | Right | 34 | 70 | 0 | 10 | 50 | 55 | 60 | 25 | 20 | 0 | 0 | 100 | No | 93 |
| 14 | 47 | Female | Left | 4.5 | 90 | 0 | 10 | 40 | 43 | 60 | 20 | 35 | 0 | −5 | 10 | Yes | 77 |
| 15 | 54 | Female | Left | 25 | 75 | 0 | 10 | 40 | 60 | 60 | 20 | 20 | −5 | 0 | 90 | Yes | 78 |
| 16 | 57 | Male | Left | 0 | 80 | 0 | 10 | 40 | 50 | 50 | 20 | 40 | −5 | 0 | 80 | Yes | 78 |
| 17 | 56 | Male | Left | 16 | 75 | 0 | 10 | 35 | 65 | 80 | 25 | 30 | −5 | −5 | 40 | Yes | 86 |
| 18 | 63 | Female | Left | 25 | 75 | 8 | 8 | 50 | 50 | 80 | 10 | 40 | 0 | 0 | 60 | No | 95 |
| 19 | 46 | Male | Left | 20.5 | 70 | 4 | 8 | 50 | 40 | 50 | 10 | 30 | −5 | 0 | 45 | No | 93 |
| 20 | 36 | Female | Right | 66 | 50 | 7 | 5 | 70 | 75 | 80 | 20 | 40 | 0 | 0 | 40 | No | 100 |
| 21 | 57 | Male | Right | 7 | 70 | 0 | 9 | 55 | 50 | 75 | 20 | 30 | 0 | 0 | 50 | No | 95 |
| 22 | 41 | Male | Right | 2 | 70 | 4 | 10 | 50 | 70 | 80 | 10 | 45 | 0 | 0 | 80 | No | 93 |
| 23 | 63 | Female | Left | 41 | 75 | 7 | 9 | 20 | 20 | 30 | 10 | 40 | 0 | 0 | 50 | Yes | 73 |
| 24 | 65 | Female | Right | 23 | 60 | 2 | 4 | 45 | 60 | 60 | 25 | 40 | 0 | 0 | 60 | No | 95 |
| 25 | 64 | Female | Left | 0 | 80 | 0 | 10 | 30 | 40 | 60 | 15 | 40 | 0 | 0 | 40 | Yes | 85 |
| 26 | 59 | Female | Right | 0 | 75 | 0 | 10 | 50 | 40 | 65 | 40 | 30 | 0 | 0 | 35 | No | 89 |
VAS: visual analog scale.
The subjective test results presented a mean VAS score of 1.76±6.34 (range: 0–8), and a mean satisfaction score of 8.57±2.04 (range: 3–10). These results reflect a low incidence of residual pain and a high level of overall satisfaction.
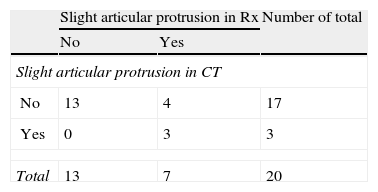
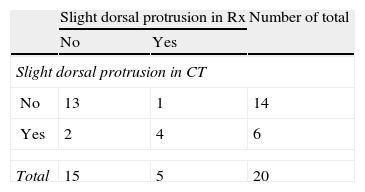
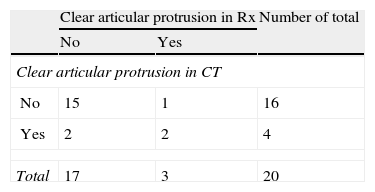
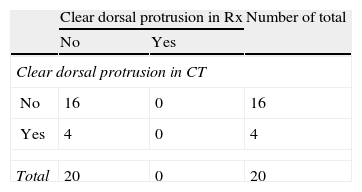
When comparing the findings of the AP and L radiographic images obtained with the aid of wedge-shaped supports, with those obtained by CT scan, we observed a statistically significant relationship in all types of protrusion, except for clear protrusion of screws at the dorsal level (Tables 2–5).
Regarding the reliability of these special radiographic projections, we obtained the following results:
For the diagnosis of slight intra-articular screw protrusion, the sensitivity of special projections was 100% and the specificity was 76%. For the assessment of slight dorsal protrusion, the special projections presented a sensitivity of 66% and a specificity of 92%.
For the diagnosis of clear intra-articular screw protrusion, the special projections offered a sensitivity of 50% and a specificity of 93%. Regarding clear dorsal screw protrusion, the special projections showed a sensitivity of 0% and a specificity of 100%.
DiscussionInternal fixation with VFAP has been established as an effective technique for the surgical treatment of complex fractures of the distal radius. Radiographic control to verify the correct placement of the screws is essential during surgery. Lister's tubercle, the triangular profile of the dorsum of the distal radius and the shape of the sigmoid cavity are some of the specific anatomical features which impede the assessment of the adequate length of the screws intraoperatively.10 It is not uncommon for protrusions up to 2–3mm to go unnoticed using standard radiographic projections.11 The phenomenon known as “skiving”12 (also referred to as “slight protrusion”), which represents a breakage of the cortex with bulging of the articular cartilage but without clear screw protrusion, is also currently attracting notable attention. It has been speculated that this condition may cause long-term joint damage.
Apart from the obvious implications of intra-articular protrusions, dorsal protrusion is also associated with extensor tendon tears,13 given their proximity to the dorsal cortex. In our series we did not detect any cases of tendon rupture, although the limited sample size did not allow any firm conclusions to be drawn about its true incidence.
As we have observed in this postoperative study, the use of special AP and L projections, tangential to the articular surfaces, can provide a more sensitive detection during the surgical procedure. Obtaining a projection tangential to the longitudinal axis of the dorsal of the radius is also useful, although we have observed that the wrist hyperflexion required for the test hinders its execution. Joseph et al.14 used this projection in an intraoperative study on 15 patients. In 4 cases (26.6%) they had to modify the screws after detecting a dorsal protrusion. Another projection that can provide information is the oblique pronated to 45°, as described by Smith and Henry,15 which enables visualization of the scaphoid and lunate facet of the radius.
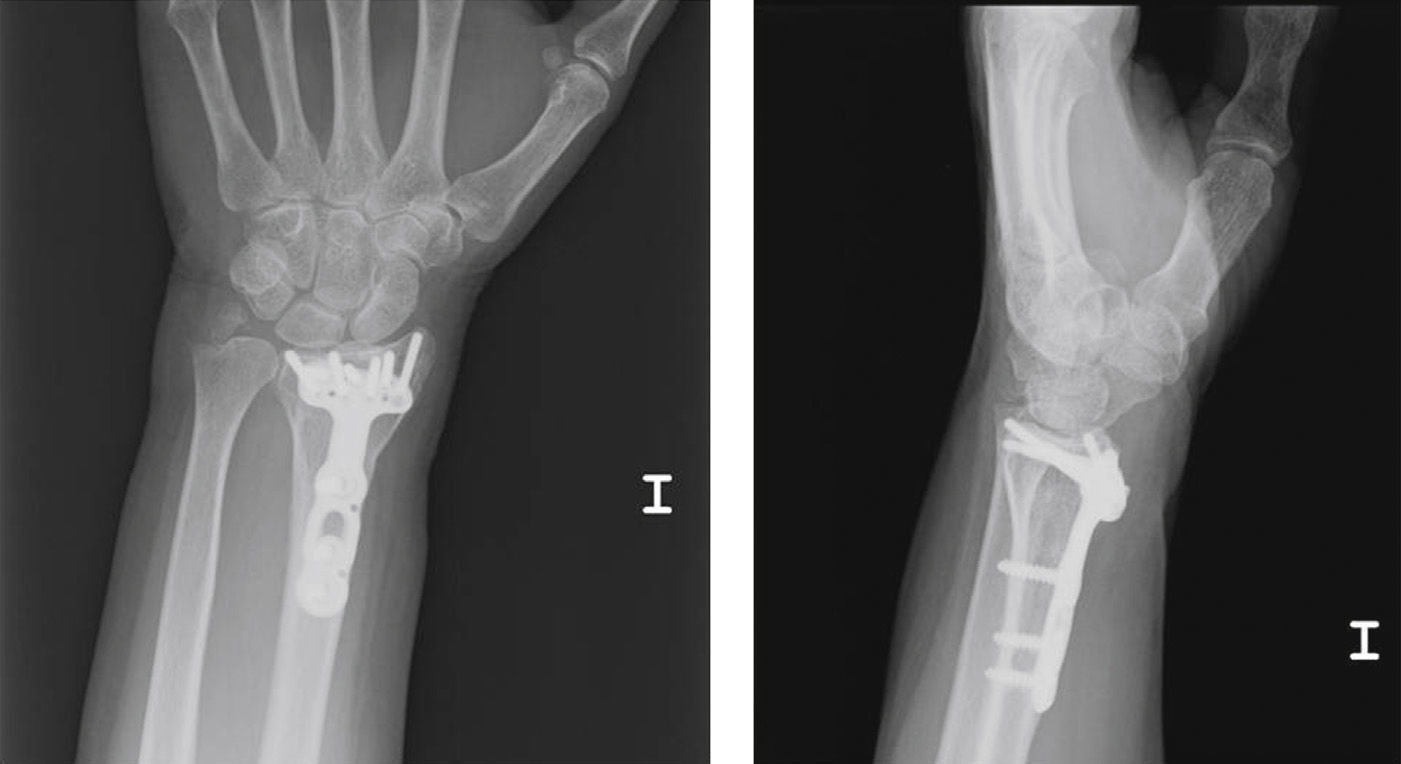
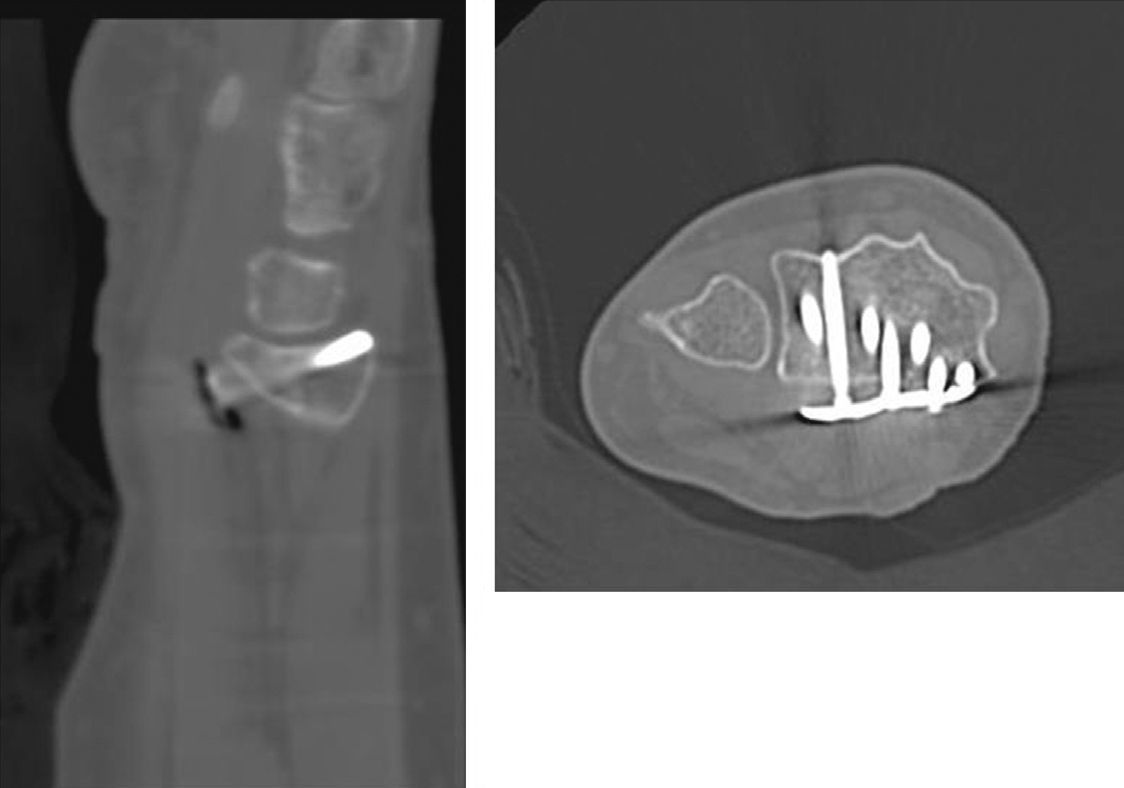
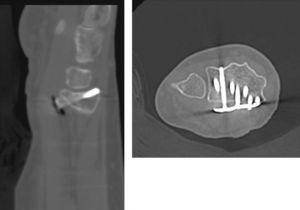
The use of supports to modify common radiographic projections has already been reported previously by other authors.16 Boyer et al.17 conducted a study on cadavers, establishing the variability between the observations in conventional Rx and in situ findings. They concluded that a projection tangential to the articular surfaces enables a better assessment of the protrusion of the screws. Our experience is similar, as we have repeatedly observed the existence of screw protrusions which had gone unnoticed in conventional projections. As shown in Figs. 2 and 3, the length of the screws can be assessed correctly in the Rx images obtained using wedge-shaped supports, without the need to obtain CT images.
Images from the CT study compared with Rx using supports. It is possible to confirm the slight dorsal protrusion observed in Fig. 2.
The present study has demonstrated a satisfactory correlation between plain radiography performed with wedge-shaped supports and CT studies. The main limitation of the study is the sample size. A larger sample size would probably offer similar results regarding assessment of clear dorsal protrusion to those obtained with other protrusions. In fact, the lack of correlation in this type of protrusion is due to 2 false negatives: one due to an excessively cubital position of the plate, which hindered the visualization of the sigmoid fossa, and another one due to a bone deformity of the patient, who had undergone a corrective osteotomy prior to placement of the plate. The other 2 false negatives detected are assumable by possible interobserver error. The strong point of the study is the fact of having CT studies available as a reference test to validate the results obtained, unlike other studies which did not perform these CT studies.14
In conclusion, obtaining radiographic projections tangential to the articular surface of the radius aided by wedge-shaped supports is an effective method to detect protrusion of VFAP screws. Their use during surgery in order to adequately modify the length of the screws is recommended.
Level of evidenceLevel of evidence i.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Mora-Pascual FE, Aguilella-Fernández L. Validez de la radiología simple con proyecciones especiales para detectar la protrusión de tornillos en el radio distal. Estudio comparativo con tomografía axial computarizada. Rev Esp Cir Ortop Traumatol. 2013;57:276–81.