Although, there are currently less invasive techniques available for the treatment of spinal injuries, open surgery is still required in many cases. Vascular injuries occurring during lumbar spine surgery, although uncommon, are of great importance due to their potential gravity. Clinical manifestations vary from an acute haemorrhagic shock that needs urgent treatment to save the patient's life, to insidious injuries or an asymptomatic evolution, and should be studied to choose the best therapeutic alternative. Four cases are reported that represent this range of possibilities and emphasise the importance of a careful surgical technique during lumbar spine interventions, and the need for high clinical suspicion, essential for the early diagnosis of these vascular complications. The current therapeutic options are also discussed.
Hoy en día han surgido técnicas poco invasivas para tratamiento de lesiones de columna; sin embargo, la cirugía abierta todavía es requerida en muchos casos. Las lesiones vasculares ocurridas durante la cirugía de columna lumbar; si bien son infrecuentes, revisten gran importancia por su potencial gravedad. Las manifestaciones clínicas de las mismas varían desde un shock hemorrágico agudo precisando tratamiento urgente para salvar la vida del paciente, hasta lesiones de evolución insidiosa e incluso asintomáticas, que permitirían estudiar la mejor alternativa terapéutica. Presentamos cuatro casos que representan este abanico de posibilidades y que enfatizan la importancia de llevar a cabo una técnica quirúrgica minuciosa durante las intervenciones de la columna lumbar y la necesidad de una alta sospecha clínica, imprescindible para el diagnóstico temprano de estas complicaciones vasculares, a la vez que se comentan las alternativas terapéuticas disponibles en la actualidad.
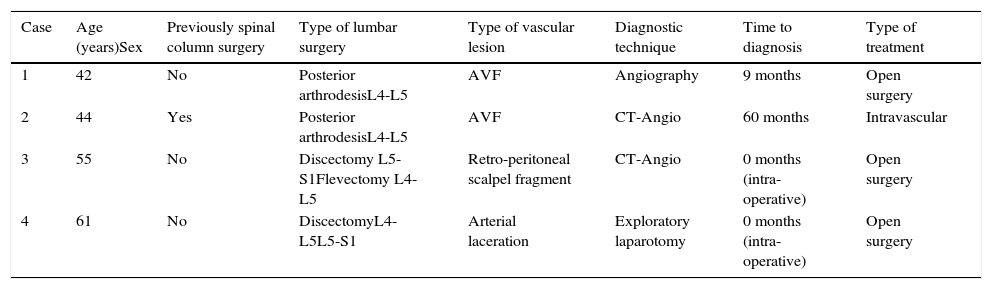
Iatrogenic lesions are a major issue in vascular surgery. Although, the majority occur during diagnostic and therapeutic intravascular procedures, they may also happen during a wide range of surgical procedures close to vascular structures. Orthopaedic surgery on the spinal column is one of the highest risk procedures. The surgical treatment of lumbar pathology using minimally invasive surgery or conventional techniques is one of the most common procedures in neurosurgery.1 The incidence of vascular complications during these operations is estimated to stand at from 0.02 to 0.06%,2 while reparative surgery mortality may surpass 65%,3 especially in emergency cases with haemodynamic instability. The aortal-iliac vessels and spinal column are closely connected anatomically, which largely explains the cause of these complications. Detection of these lesions requires a high level of suspicion, which is essential to prevent potentially fatal outcomes. We present four cases (Table 1) of vascular lesions caused during operations on the spinal column in our hospital from 1997 to 2012. We describe their clinical presentation and how they were caused and treated.
Summary of patient characteristics and the procedures used.
| Case | Age (years)Sex | Previously spinal column surgery | Type of lumbar surgery | Type of vascular lesion | Diagnostic technique | Time to diagnosis | Type of treatment |
|---|---|---|---|---|---|---|---|
| 1 | 42 | No | Posterior arthrodesisL4-L5 | AVF | Angiography | 9 months | Open surgery |
| 2 | 44 | Yes | Posterior arthrodesisL4-L5 | AVF | CT-Angio | 60 months | Intravascular |
| 3 | 55 | No | Discectomy L5-S1Flevectomy L4-L5 | Retro-peritoneal scalpel fragment | CT-Angio | 0 months (intra-operative) | Open surgery |
| 4 | 61 | No | DiscectomyL4-L5L5-S1 | Arterial laceration | Exploratory laparotomy | 0 months (intra-operative) | Open surgery |
AVF: arteriovenous fistula.
A 42 year-old woman operated for posttraumatic spondylolisthesis of L4, with anterior L4-L5 arthrodesis, posterior arthrodesis and fixation using a Harrington rod on the left side from L3 to L5. Immediately after the operation she remained in the Intensive Care Unit due to haemodynamic instability of indeterminate origin. After supporting measures this resolved after 48h. Nine months later she presented progressive dyspnoea due to medium efforts. Physical examination showed a systolic murmur III/VI in the mitral valve, crepitation in the bases of both lungs and a continuous abdominal murmur irradiating to the back, as well as recent varicose veins in the left leg and diffuse swelling of this limb. X-ray and ECG suggested a left cardiac overload. Given the suspicion of a vascular complication, angiography was performed. This showed communication between the right common iliac artery and the lower cava vein and right common iliac vein, although it was not possible to find the exact point where they were connected. Treatment consisted of resection of the segment of affected artery (the right common iliac artery) and the placing of an 8mm diameter Dacron prosthesis, as well as repair of the vein by continuous suture. There were no postoperative complications. The patient was monitored by check-ups during one year, after which she was discharged having remained asymptomatic.
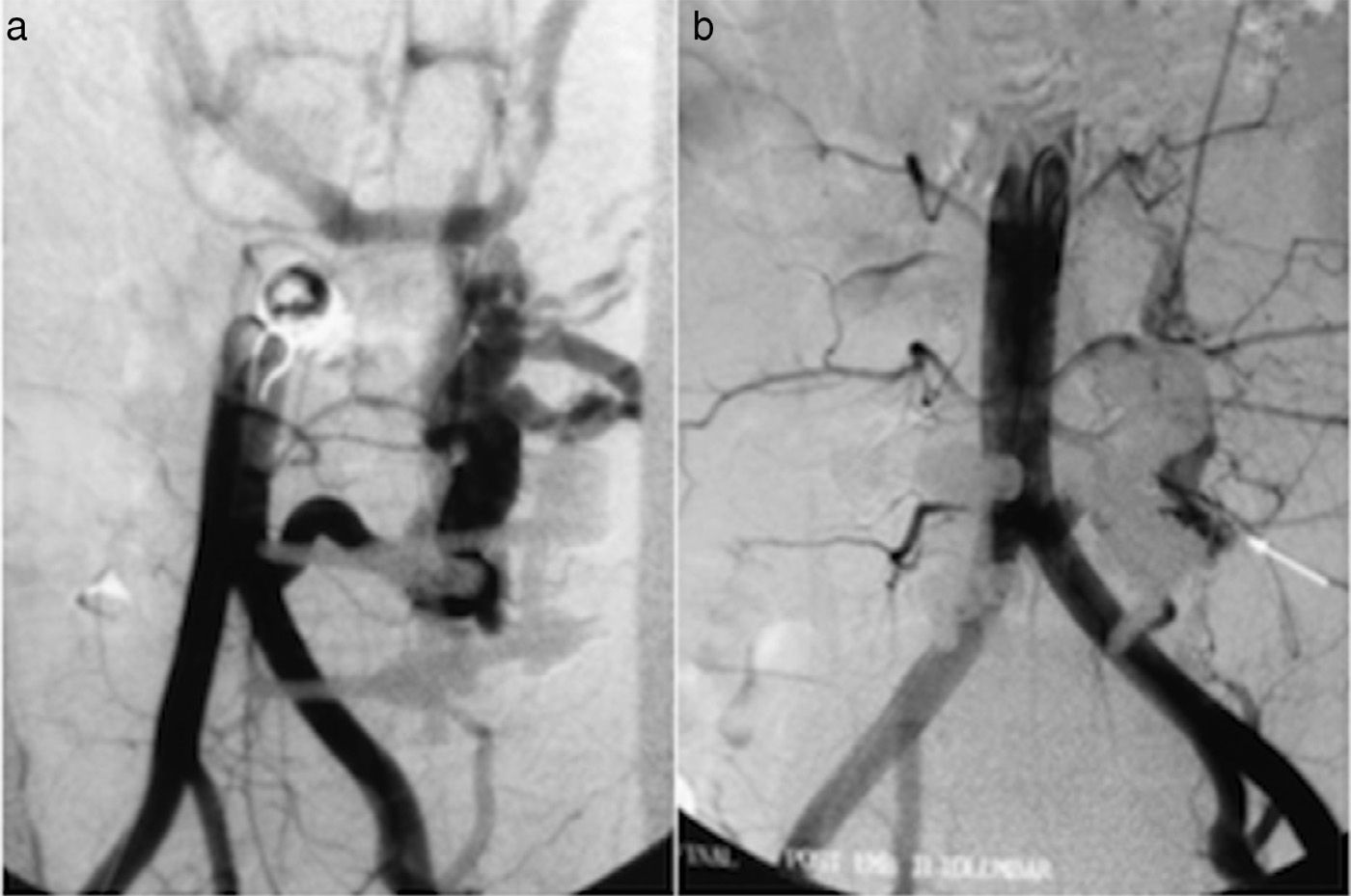
Case 2A 44 year-old man with a history of L4-L5 discectomy due to disc hernia six years beforehand and posterior arthrodesis of L4-L5 one year later, with TSRH (Texas Scottish Rite Hospital) instrumentation and the placement of an interspinal prosthesis in L3-L4. Physical examination detected an abdominal murmur as a casual finding without associated symptoms. A CT-angiography was performed for diagnostic purposes, showing an arteriovenous fistula that communicated the rear wall of the common left iliac artery with a left lumbar vein. Diagnostic-therapeutic angiography confirmed the presence of a high-flow arteriovenous fistula, originating in the left paralumbar plexus and communicating with lumbar arterial branches and with the common left iliac artery (Fig. 1a). Treatment consisted of embolisation of the lumbar artery with coils. The same procedure was used for an iliac-lumbar artery which contributed to the flow of the fistula (Fig. 1b). In the final angiography there was still a minimum flow, probably from higher lumbar branches, and it was decided to monitor this. CT-angiography at 3 months showed a notable reduction in the venous circulation of the paravertebral plexi, although there was still a hypertrophic vein draining into the left renal vein. After one year of follow-up the patient remains asymptomatic.
Case 3A 55 year-old man with a history of a discectomy due to extruded disc hernia of L5-S1 and flavectomy of L4-L5. In the operation severe calcification of the intervertebral disc was detected, together with intense fibrosis and adherences of the dural sac. During the surgical operation the point of the scalpel fragmented and lodged in the space between L4-L5, from where it could not be recovered during the operation. Computerised tomography one month after surgery showed the fragment was moving towards the retroperitoneal space. Two months later a further displacement forwards was observed, potentially affecting vascular structures, so that it was decided to operate to extract the fragment even though the patient was asymptomatic. The surgical procedure consisted of a retroperitoneal approach through an incision in the right flank, accessing the homolateral iliac vessels. The scalpel point was found lodged in the rear face of the bifurcation of the common right iliac artery, adhering to the common right iliac vein. This was extracted by means of a venotomy. The affected arterial and venous vessels were stitched by continuous suture. There were no immediate postoperative complications. One month after the operation the patient presented deep vein thrombosis in the poplitheal, femoral and iliac zone of his right leg, which evolved favourably with anticoagulation. The total duration of follow-up amounted to 15 years. He currently has a mild postphlebitic syndrome in his right leg as a consequence of the thrombosis.
Case 461 year-old woman with a history of obesity and arterial hypertension, diagnosed lumber disc hernia in L4-L5 and L5-S1. She was admitted to our hospital for the planned discectomy of the said segments. A posterior lumbar approach was used. The operation took place without any incidents except for a tendency to present hypertension during the last phase of surgery. Once the operation had terminated, when the patient was about to be transferred to the unit of post-surgical care, signs of hypovolemic shock associated with a taut abdomen were observed: given the suspicion of intraabdominal bleeding with haemodynamic instability, emergency transperitoneal laparotomy was performed. Examination revealed left retroperitoneal haematoma due to tearing of the common proximal left iliac artery in its posterolateral face, as well as severe artherosclerotic lesions at this level. The defect was repaired by placing a short 8mm diameter Dacron graft sutured termino-terminal in the common left iliac artery. There were no immediate postoperative complications. Total follow-up lasted for two years, and there were no complications.
DiscussionAlthough, injury to vascular structures during surgical procedures on the lumbar column is very rare, it is possible that its actual incidence is underestimated. In the last year, 246 orthopaedic operations were performed on the lumbar sector in our hospital. The complication reported the most often in the literature is laceration of major vessels, at 53.4%, followed by the formation of arteriovenous fistulas (17.2%), pseudoaneurisms (13.8%) and a combination of the above (15.5%).1 The finding of a foreign body lodged in the area of the iliac vessels due to lumbar column surgery, as described in case 3, is even rarer, and no similar reports (in operations that did not involve the implantation of orthopaedic material) were found in a revision of the bibliography.
The vessels which are usually affected are the common iliac artery (51.2%), the common iliac vein (23.3%), the lower cava vein (9.3%) and the abdominal aorta (4.7%).1 This may be explained by the characteristics of the orthopaedic surgical technique and the topographic proximity of vascular structures: the aortic bifurcation is to the left of the upper edge of L4-L5; both common iliac arteries pass in front, and the left common iliac vein crosses in front of the same. Some factors have been reported to predispose to a higher risk, as they lead to fibrotic changes and alterations to normal anatomy. These include degeneration of the anterior common vertebral ligament, spinal column or vertebral anomalies (arthrosis and spondylolisthesis), obesity and previous surgery for disc hernia.4
The symptoms and clinical findings deriving from arterial lacerations include hypotension, tachycardia, active bleeding, a reduction in haemoglobin level, a taut abdomen, the presence of an abdominal mass and/or abdominal pain, while it is usually detected early (<24h).1 On the other hand, arteriovenous fistulas and pseudoaneurisms usually establish gradually, and they are detected later (from >24h to several years). The symptoms which lead to the suspicions of a fistula are the finding of a murmur, abdominal pain, an abdominal mass, signs of heart failure, oedema of the legs or dyspnoea, etc.,1 above all when they appear in young patients soon after a lumbar operation. Jarstfer et al.5 report that these symptoms appear after 24h in 9% of cases; from 24h to one year in 70% and after one year in 21%. The intraoperative finding of minimum blood residues in the surgical field or after removing the forceps following a discectomy may lead us to suspect a possible vascular lesion, given that the intervertebral disc is an avascular structure.
Careful surgical technique and exact anatomical knowledge are indispensible to avoid serious complications, even in highly experienced surgical teams.6 Early detection and treatment are essential to reduce mortality and morbidity.
Angiography is considered to be the gold standard for the diagnosis of acute iatrogenic vascular lesions, as it makes it possible to locate the exact site of bleeding and perform intravascular treatment if this is indicated.1,7 Computerised axial tomography with intravenous contrast is the initial imaging test that is used the most for the diagnosis of fistulas and pseudoaneurisms, and it is especially useful for the diagnosis of haematomas and venous bleeding, on condition that the situation of the patient permits it. In situations when the patient is in shock or swiftly deteriorating complementary examinations may be contraindicated, while an emergency exploratory laparotomy may be the only diagnostic alternative.
The treatment technique will depend on the type of lesion and the context in which it arises. Classically open surgery was used to repair actively bleeding lacerations with associated shock, exposing the large retroperitoneal vessels through xyphopubic laparotomy. Dissection is often aided by the plane created in the expansion of the retroperitoneal haematoma. It is sometimes necessary to section the affected artery when the defect is in its rear surface or when it is wished to correct an adjacent venous defect. This is followed by termino-terminal suture or the placing of a prosthetic graft if a very long section is involved. Venous repair is usually more difficult, and primary vein suture is almost impossible in the majority of cases; a valid alternative in these situations is the complete ligature of the vessel, as this is preferable to a defective repair which increases the risk of thrombosis and pulmonary embolism. With the aim of reducing the morbimortality associated with open surgery, in recent years attention has focussed on intravascular treatment. Although this has generally been used for the elective repair of pseudoaneurisms or fistulas, it can also be used in emergency situations due to iatrogenic lacerations or trauma, in which high rates of success have been described.8 When active bleeding is suspected, it is possible to place an intra-arterial occlusion balloon at the level of the defect to control the bleeding, followed by intraoperative angiography to determine the exact location and proceed to the definitive treatment (endoprosthesis, coils). In these cases limitations arise due to the need for a permanent X-ray team in the operating theatre, the availability of material and the surgeon's expertise in the technique.
The treatment of late-arising complications using conventional surgery may be hindered by fibrosis and the presence of an abundant collateral vascular network. On the other hand, the clinical course of these complications usually allows enough time to study and program their definitive treatment. In 1995, Zaiko et al.9 published the first case of intravascular repair of an iliac-cava fistula, and since then many series have described the success of this therapeutic technique in arteriovenous fistulas with different causes.10 The technique consists of embolisation or implanting a covered stent to seal the communication. The use of one technique or the other depends on lesion anatomy, the presence of a high flow and the risks of remote embolisation.
We can conclude that although iatrogenic vascular trauma during lumbar column surgery is rare, it is especially important due to its potential seriousness, and it may even be caused by experts. A high level of diagnostic suspicion is necessary, together with early treatment.
The progress in intravascular techniques represents an excellent therapeutic alternative.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments with human beings or animals were undertaken for this research.
Confidentiality of dataThe authors declare that they followed the protocols of their hospital on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Please cite this article as: Riedemann-Wistuba M, Alonso-Pérez M, Llaneza-Coto JM. Complicaciones vasculares asociadas a la cirugía de columna lumbar. Rev Esp Cir Ortop Traumatol. 2016;60:148–152.