Knee dislocation is an unusual condition, and can have catastrophic consequences, such as vascular and neurological complications, in addition to the ligament injuries.
ObjectiveThe aim of this study is to analyse the effectiveness of a protocol of early diagnosis of vascular injuries associated with knee dislocations.
Materials and methodsA retrospective study was conducted which included acute knee dislocations treated in our institution, with a minimum of 12 months follow-up, between 1999 and 2010. A diagnostic protocol based on physical examination and ankle-brachial index was used in order to detect vascular injuries.
ResultsTen dislocations, 30% with popliteal artery injury, were diagnosed early and received emergency treatment within 8h. There were associated neurological injuries in two patients. There were no amputations.
ConclusionsThe systematic use of this protocol has avoided consequences of late diagnosis and has drastically reduced the abusive use of invasive tests, such as arteriography.
La luxación de rodilla es una entidad infrecuente. Puede tener consecuencias devastadoras, no solo por las lesiones ligamentosas, sino también por las complicaciones vasculares y nerviosas.
ObjetivoAnalizar la eficacia de un protocolo para el diagnóstico precoz de lesiones vasculares asociadas a las luxaciones de rodilla.
Material y métodosSe presenta un estudio retrospectivo de las luxaciones de rodilla agudas tratadas entre 1999-2010 con un seguimiento mínimo de 12 meses. Se utilizó un protocolo diagnóstico basado en la exploración física y el índice tobillo-brazo como pruebas de cribado inicial de lesión vascular.
ResultadosSe obtuvo una muestra de 10 luxaciones, de las que en un 30% se produjo lesión de la arteria poplítea que fueron diagnosticadas precozmente, recibiendo tratamiento quirúrgico urgente antes de 8 horas. Dos pacientes tuvieron lesiones nerviosas asociadas a la vascular. Ningún caso acabó en amputación.
ConclusionesLa utilización sistemática del protocolo ha evitado consecuencias derivadas de un diagnóstico tardío y ha reducido drásticamente el uso abusivo de pruebas invasivas como la arteriografía.
Knee dislocation is a rare entity, with an estimated incidence of 0.001–0.013% of all urgent orthopaedic traumatological lesions.1 It generally results from high-energy trauma (traffic accidents), but can also occur in the context of sport or accidental falls. Spontaneous reduction occurs in up to 50% of cases, which is why the classical term “dislocation” has been replaced by multiligament or complex knee ligament injury; this concept includes injuries of at least 3 of the 4 major knee ligaments.1
In addition to the already mentioned ligament injuries, we may find vascular-nerve injuries which should not be overlooked due to their potentially catastrophic consequences.
In 1977, Green & Allen reported a 23–32% incidence of vascular lesions in acute knee dislocations.2 This is because the popliteal artery is fixed proximally in the adductor hiatus and distally in the fibrous arch of the soleus, thus becoming a vulnerable structure to injury. These authors found that 86% of amputations took place due to popliteal artery lesions which were not repaired within 8h of injury.2
There is no consensus about the best method to diagnose these injuries.
The classical approach advocated performing routine arteriography,2–4 but this has been recently called into question since the test involves significant morbidity, has limited availability and can sometimes delay urgent surgical treatment.5,6
The objective of this study is to analyse the usefulness of a diagnostic protocol based on noninvasive tests aimed at obtaining an early diagnosis of vascular injuries after knee dislocation. The working hypothesis is based on the premise that noninvasive diagnostic tests may be sufficient to identify acute vascular complications.
Material and methodsWe performed a retrospective analysis of knee dislocations diagnosed at our institution from January 1999 until January 2010.
The inclusion criteria employed were a clinical and radiological diagnosis of knee dislocation or multiligament knee injury with no prostheses, with a minimum follow-up period of 12 months.
We obtained a sample consisting of 12 dislocations, of which 2 cases were excluded because their follow-up period was less than 12 months.
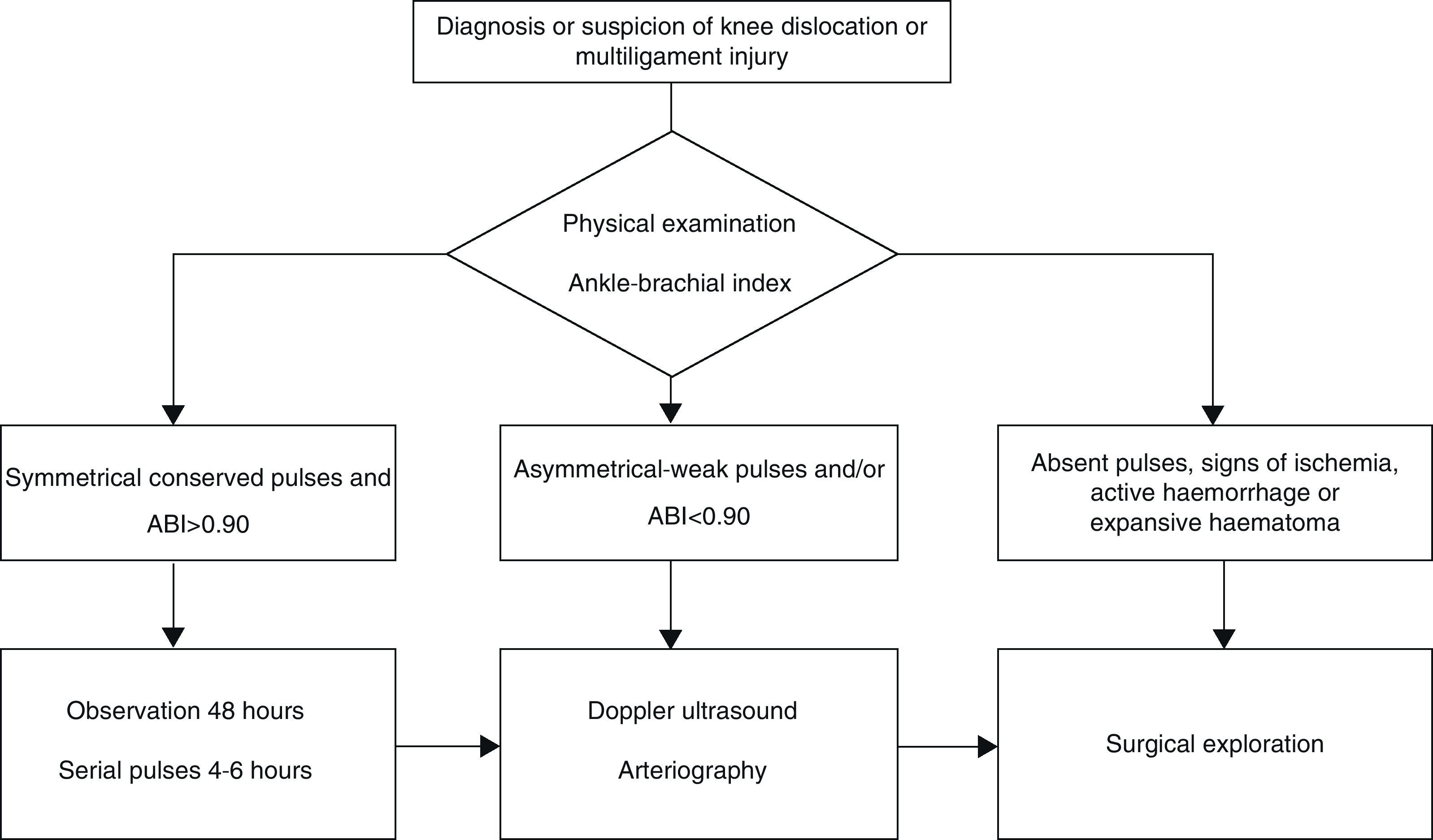
We assessed vascular condition in patients with diagnosed or suspected knee dislocation, according to a series of explorations which are summarised in the proposed protocol (Fig. 1). This protocol is based on physical examination and ankle-brachial index (ABI) as noninvasive, initial screening tests for early diagnosis of vascular lesions.5,7,8
According to the protocol, upon their arrival at the emergency service, patients underwent a rigorous physical examination of peripheral pulses (posterior tibial and dorsalis pedis), with a special focus on signs of acute ischemia (coldness, pallor, paresis and pain). This was followed by an emergency measurement of the ABI. The ABI is the ratio of peak systolic blood pressure at the ankle divided by that at the arm.
When these examinations were normal, observation for 48h with serial monitoring of pulses was sufficient. If distal pulses were impaired or ABI<0.9, the suspicion of vascular injury had to be confirmed through complementary tests, such as Doppler ultrasound or arteriography.
Arteriography was performed selectively in cases in which noninvasive tests were altered, provided that it did not delay vascular intervention if this was necessary.
ResultsA total of 10 patients were included in the series, of which 8 were males, with a mean age of 42.3 years (range: 30–74 years). Mean follow-up time was 31.3 months (range: 12–82 months).
The mechanism of injury was high-energy trauma in 7 cases (70%), 6 of them associated with traffic accidents and 1 with a sporting accident. The remaining 3 cases were due to accidental falls.
Vascular lesionsThe implementation of the proposed protocol led to the detection of alterations or asymmetries in peripheral pulse, signs of ischemia or ABI<0.9 at the time of initial evaluation in 3 cases (30%).
In 2 of these cases, the study was completed by a Doppler ultrasound which confirmed injury of the popliteal artery in its second portion. These cases underwent emergency operation involving femoropopliteal bypass with inverted, internal saphenous vein autograft, immobilisation with external fixation and prophylactic fasciotomy, all within the first 8h after injury.
In the third case, the patient presented an open dislocation with wide exposure: abundant active bleeding, weak distal pulses, coldness and pallor of the foot. Given the severity of the injury we performed surgical exploration and found a laceration of the popliteal artery and vein, which were repaired with saphenous vein autograft.
Nerve lesionsNerve lesions were identified in 20% of patients. In 1 case the vascular lesion was associated with common peroneal nerve neuropraxia, which was treated conservatively with drop-foot orthosis achieving full recovery after 7 months. Another patient presented tibial nerve neurotmesis in the context of an open knee dislocation. In this case we performed termino-terminal suture of the nerve during emergency vascular repair. Neurological recovery was incomplete at 14 months, although the patient had recovered sufficient force for plantar flexion and toe flexion towards severity (grade 2/5), with persistence of residual plantar hypoesthesia.
Compartment syndromeThere were no cases of compartment syndrome, although prophylactic fasciotomy was performed on the 3 patients who underwent emergency surgery due to popliteal artery injury.
ReductionWe performed emergency surgical closed reduction on 4 patients, while 1 patient with open dislocation underwent open reduction in the operating room (Table 1). The remaining cases were reduced spontaneously after trauma. Out of the cases with vascular complications, reduction after trauma was spontaneous in 1 of them. In the other 2 patients, 1 case of anterior dislocation and 1 case of posterior dislocation, it was necessary to conduct reduction under sedation.
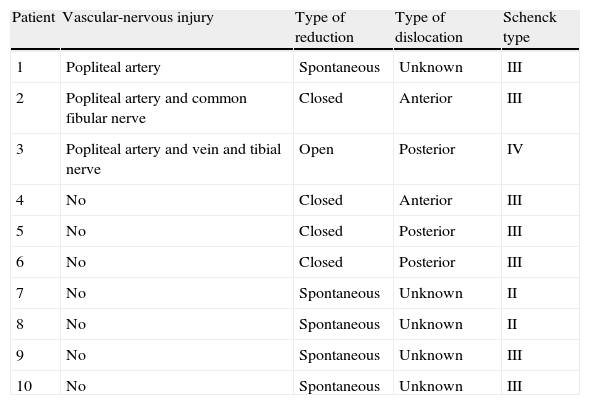
Description of dislocations and associated lesions.
| Patient | Vascular-nervous injury | Type of reduction | Type of dislocation | Schenck type |
| 1 | Popliteal artery | Spontaneous | Unknown | III |
| 2 | Popliteal artery and common fibular nerve | Closed | Anterior | III |
| 3 | Popliteal artery and vein and tibial nerve | Open | Posterior | IV |
| 4 | No | Closed | Anterior | III |
| 5 | No | Closed | Posterior | III |
| 6 | No | Closed | Posterior | III |
| 7 | No | Spontaneous | Unknown | II |
| 8 | No | Spontaneous | Unknown | II |
| 9 | No | Spontaneous | Unknown | III |
| 10 | No | Spontaneous | Unknown | III |
N: nerve.
Patients requiring surgical reduction were immobilised with an external fixator (Fig. 2), while the remaining patients (5 cases, 50%) were immobilised with casts that were later replaced by hinged orthosis.
Image from a 23-year-old male, suffering anterior dislocation of his left knee after a traffic accident. Upon arrival he presented weak pulse and ABI<0.9. We performed urgent femoropopliteal bypass with fasciotomy and immobilisation with an external fixator. Simple radiology: anterior dislocation in anteroposterior (A) and lateral (B) projections, anteroposterior (C) and lateral (D) reduction and external fixation.
Ligament injuries were classified according to the Schenck classification1: 7 patients suffered injury to both cruciate ligaments and at least one of the collateral ligaments (KD III), 2 patients suffered lesions of both cruciate ligaments (KD II) and 1 patient suffered lesions to both collateral ligaments of both cruciate ligaments (KD IV) (Table 1).
Regarding treatment of ligament injuries, 5 patients underwent conservative treatment with hinged orthosis due to their refusal to undergo surgery for personal reasons. In the remaining patients, repair of the ligament injury took place at the time when general and vascular condition allowed it. Of these, 2 patients underwent repair of the capsule and posterolateral or posteromedial complexes within 2–3 weeks, with reconstruction of the cruciate ligaments being completed in the first 6–8 weeks. There were no vascular complications surrounding these procedures. In the 3 patients with vascular lesions reconstruction was delayed more than 3 months on average, following the recommendations of the vascular surgeon. We do not present the clinical and functional results thereof, since this falls outside the scope of this study.
Tendon injury was added in 3 cases, with complete injury of the femoral biceps tendon appearing in 2 patients and the patellar tendon in 1 patient.
Half of the cases were associated with other bone lesions: vertebral compressions, avulsion of the tibial spines, ankle dislocations and diaphyseal femoral fractures.
DiscussionInterest in knee dislocations lies mainly in their associated vascular-nervous complications, which can even lead to supracondylar leg amputations.9,10 Occasionally, a low-energy mechanism of injury or spontaneous reduction of the dislocation may be misleading about the severity of subsequent complications. Therefore, early diagnosis is of vital importance and this requires the use of protocols, as well as the evaluation of the usefulness of different diagnostic methods available.11
In the present study, noninvasive tests were effective for the early identification of the 3 patients who suffered vascular lesions, leading to appropriate emergency treatment before 8h from the time of injury.
Physical examinationPhysical examination is the initial step and one of the key pillars in the diagnosis of possible vascular lesions.5,12,13Miranda suggests that exploration of distal pulses reaches a positive predictive value of 94% and a negative predictive value of 100%.14 It has been proposed a scheme of serial examination of distal pulses during the first 48h after a knee dislocation, as well as the use of physical examination as a method to discriminate cases in which selective arteriography was to be conducted.15 By contrast, other authors argue that physical examination alone is not sufficient for the diagnosis of vascular lesions.13,16–18
There are several published cases of popliteal artery lesions with preserved pulses.4,18,19 Casañas presents a series of 43 knee dislocations, of which 14 presented positive distal pulses during the initial evaluation and which became negative hours later.19
For this reason, physical examination should be complemented by other noninvasive diagnostic tests such as ABI or Doppler ultrasound.15
Ankle-brachial indexThe ABI has been shown to play an important role as a noninvasive screening test to detect vascular lesions, in order to avoid systematic angiography of all knee dislocations.20 In 1991, Johansen defended an ABI>0.9 as a test with a negative predictive value of up to 99% to rule out arterial injuries.7
In the same line, Mills published results in which an ABI<0.90 predicted vascular lesions with a sensitivity of 87–100%, specificity of 97–100% and positive predictive value of 91–100%.21 Seroyer et al. proposed the ABI as a useful test for early diagnosis of vascular lesions and to discriminate those cases in which selective arteriography was to be performed.12,22The ABI test is considered as a safe, inexpensive, reproducible and effective test. We believe it may be of great use when performing vascular injury screening in knee dislocations.7,21–24
In those cases in which distal pulse alterations and/or ABI<0.9 are found, the suspicion of vascular injury should be confirmed through other tests such as Doppler ultrasound or arteriography.
Doppler ultrasoundDoppler ultrasound is a diagnostic test with a sensitivity of 95% and specificity of 99% for the diagnosis of vascular lesions. It may be very useful to avoid employing invasive explorations.8 The main problem it entails is the need for trained personnel, as it is an observer-dependent test.
ArteriographyArteriography has traditionally been considered as the gold standard in the diagnosis of vascular lesions.2,4 Being an invasive test, it carries a risk of complications between 1.7% and 3.3%. These include: intimal dissection, thrombosis, pseudoaneurysms, haemorrhaging and arteriovenous fistulas.6,15
In addition, considerable incidences of false negatives up to 1.2–6% and false positives up to 2.4–7% have been reported.23Arteriography may delay emergency treatment by up to 3h, with subsequent risk for the viability of the affected limb.5–7Revascularisation after 8h should be avoided, since the time elapsed from injury to vascular repair represents one of the main prognostic factors.2,25–28For all these reasons, there is currently a tendency towards restricting invasive tests such as arteriography to selected cases. Multiple publications recommend performing selective arteriography only in cases where noninvasive tests suggest vascular lesion.9,10,12,20,22,29–32
Diagnostic protocolAccording to the above, we propose the systematic use of protocols for the early diagnosis of vascular lesions in knee dislocations. Noninvasive tests such as physical examination and ABI are important in the initial screening.
Invasive tests such as angiography may be performed selectively when there are weak/asymmetrical pulses, signs of ischemia, active bleeding or ABI<0.9.9,10,12,13,15,20–23,29–31 In any case, performing an arteriography should not delay vascular repair more than 8h after injury, since this is one of the main prognostic factors.5,7,10,23,33
Urgent surgical exploration should be performed upon encountering significant signs of ischemia, open or irreducible dislocations.
LimitationsThe limitations of our study include its retrospective design and the limited size of our population.
ConclusionsThe systematic use of the protocol based on noninvasive testing has avoided consequences derived from delayed diagnosis and drastically reduced the overuse of invasive tests such as arteriography.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: López-Hualda A, et al. Lesiones vasculares asociadas a luxación de rodilla: protocolo diagnóstico. Rev Esp Cir Ortop Traumatol. 2012; 56:260–6.