Retentive treatment of prosthetic material superinfected by resistant microorganisms is a challenge, especially when the causative agent is a methicillin-resistant Staphylococcus aureus. We present the successful conservative management of osteosynthesis material implanted due to ankle fracture in an elderly patient who suffered superinfection by the aforementioned microorganism, in which the antimicrobial treatment consisted of the combination of antibiotic-guided systemic antibiotics (after a first ineffective empirical cycle), together with topical irrigations of sevoflurane, applications of silver sulfadiazine cream, and subsequently coverage of the skin defect with negative pressure therapy. We highlight the novel role of sevoflurane as an analgesic and as a topical antimicrobial agent (in addition to silver sulfadiazine) in the favourable evolution of the wound, especially in the period in which the empirical antibiotic therapy was ineffective and negative pressure therapy had not yet been applied.
El tratamiento retentivo de material protésico sobreinfectado por gérmenes resistentes es un desafío, especialmente cuando el agente causal es un Staphylococcus aureus resistente a meticilina. Presentamos el manejo conservador satisfactorio de material de osteosíntesis implantado por fractura de tobillo a un paciente añoso y que sufrió sobreinfección por el citado microorganismo, en el que el tratamiento antimicrobiano consistió en la combinación de antibioterapia sistémica guiada por antibiograma (tras un primer ciclo empírico ineficaz), junto a irrigaciones tópicas de sevoflurano, aplicación de crema de sulfadiazina de plata, y posteriormente cobertura del defecto cutáneo con terapia de presión negativa. Destacamos el novedoso papel del sevoflurano como analgésico y como antimicrobiano tópico (sumado a la crema de sulfadiazina de plata) en la evolución favorable de la herida, especialmente en el período en el que la antibioterapia empírica era ineficaz y todavía no se había comenzado con terapia de presión negativa.
The conservative treatment of prosthetic material is highly complicated when the surgical wound or joint is infected and particularly when the infection is caused by staphylococci. All the more so when the causative agent is methicillin-resistant Staphylococcus aureus (SARM).1,2 Some authors have even consider it is futile to attempt to retain an infected prosthesis when the infecting agent is a SARM2 and are in favour of removing it. The problem of the surgical solution, particularly in elderly patients, is its aggressiveness and the desired result cannot be guaranteed.3
We present the case of multimodal management of an infected surgical wound of an elderly patient, aimed at preserving the osteosynthesis material and avoiding further surgery.
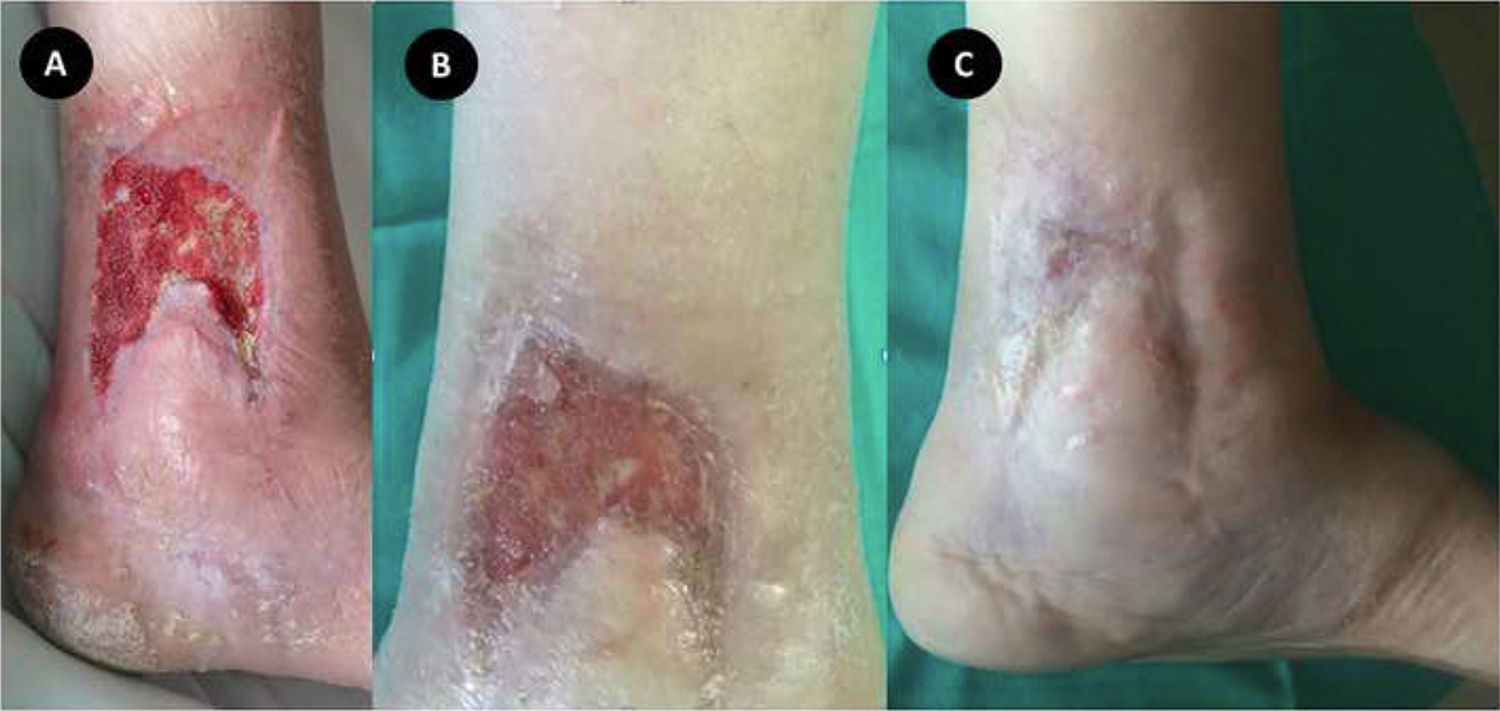
Clinical caseAn 83 year-old male patient with no history of interest presented at the emergency services with a closed fracture of the left tibial pilon and fibula after being run over. Under spinal anaesthesia and with a prior intravenous infusion of 2 g of cefazolin as surgical prophylaxis, open reduction of the fracture was performed and osteosynthesis with a plate in the fibula and a medial plate in the tibial pilon (Fig. 1A) was applied. It was not possible to perform direct closure of the medial surgical wound, and a fasiocutaneous flap was therefore used. Postoperative evolution was satisfactory, including the administration of 4 doses of 1 g of cefazolin every 6 h, and the patient was discharged from the hospital 72 h after surgery with favourable appearance of the flap.
The patient was followed up with periodical weekly check-ups in the outpatient department, with favourable evolution of the flap, but at 8 weeks necrosis was observed and the patient was referred to hospital. The patient presented with a necrotic slough with an ulcer measuring 9 × 9 cm and malodorous exudate surrounded by a red area around the flap. On removal of the necrotic slough the tibial osteosynthesis plate was visible (Fig. 1B). Analysis showed mild leukocytosis (11.840 × cells/μl; range: 4000–10,000 × cells/μl) with marked elevation of acute phase reactants (PCR: 205 mg/l; range: 0−5 mg/l; VSG: 55''; range: 1–20''). Two samples were taken under aseptic conditions for the aerobic and anaerobic microbiological culture—one of the wound exudate obtained with an aspirate syringe and the other consisting of a biopsy of the tissue which included part of the necrotic slough tissue and tissue from the wound. Empirical antibiotherapy was administered with amoxicillin/clavulanic acid and levofloxacin.
At this point the fracture had not yet consolidated and two surgical therapeutic approaches were suggested:
- a)
Removal of the osteosynthesis material, application of an external fixator, prolonged antibiotic treatment and then a new flap. This option was, a priori, the most aggressive and time-consuming.
- b)
Retention of the osteosynthesis material with the application of a new vascularised flap. The advantages of this second option were that it would be less aggressive and that results would be obtained faster, but it required the performing of an arteriography prior to surgery to observe the vascular status of the limb and decide if a flap was viable or not.
Whilst waiting for the arteriography to be performed we decided to start treatment of the wound with irrigations of topical sevoflurane (Sevorane®, AbbVie, Campoverde di Aprilia, Italy), having previously obtained the informed consent from the patient.
To irrigate the wound, we covered it with a sterile plastic dressing to create a cavity which was then filled with 20 ml of sevoflurane (Fig. 1C) so as to minimise the environmental contamination of the room due to the volatisation of this anaesthetic. After waiting 5 min the remaining sevoflurane was aspired and the intense analgesic effect caused by the sevoflurane facilitated debridement of the necrotic flap with very good analgesic quality and without the need to use other systemic analgesics. Antibiotic cream with silver sulfadiazine was then applied and the wound was covered with a flexible lipid-colloid dressing. This procedure (sevoflurane-cream-dressing) was repeated for further healing treatments.
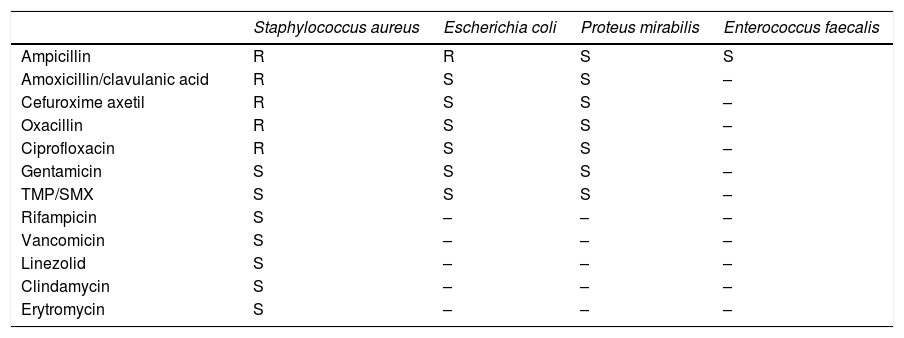
Three days later a second wound healing treatment was performed. Analysis did not reveal any major changes (leukocytes: 11,880 cells/μl; PCR: 227 mg/l, VSG: 28'') but the wound did not present any exudate and granulation tissue had appeared on the wound bed. That same afternoon the result from the aerobic culture arrived (the anaerobic tested negative) for the samples taken on hospital admittance. Polymicrobial flora were isolated, both gram negative (low Proteus mirabilis and low Escherichia coli, both sensitive) and gram-positive (a few Enterococcus faecalis, and moderate S. aureus resistant to meticillin and to quinolones) (Table 1), and all these germs had grown in the sample of the wound exudate and in the tissue biopsy. Due to these results, the initial empirical antibiotherpay was replaced by rifampicin, ampicillin and trimetoprim/cotrimoxazol, in keeping with the criterion of the infectious diseases unit.
Microbiological result with patter of sensitivities of the samples of wound exudate and biopsy of the tissue obtained for the culture on hospital admittance.
| Staphylococcus aureus | Escherichia coli | Proteus mirabilis | Enterococcus faecalis | |
|---|---|---|---|---|
| Ampicillin | R | R | S | S |
| Amoxicillin/clavulanic acid | R | S | S | – |
| Cefuroxime axetil | R | S | S | – |
| Oxacillin | R | S | S | – |
| Ciprofloxacin | R | S | S | – |
| Gentamicin | S | S | S | – |
| TMP/SMX | S | S | S | – |
| Rifampicin | S | – | – | – |
| Vancomicin | S | – | – | – |
| Linezolid | S | – | – | – |
| Clindamycin | S | – | – | – |
| Erytromycin | S | – | – | – |
One day later the requested arteriography was performed, where it was observed that the peroneal artery presented with a stenosis which would impede the application of a free pediculated flap. In view of this situation and the favourable evolution of the wound, we decided to continue with the same strategy of topical healing with sevoflurane every 3 days, combined with the new systemic antibiotherapy and the silver sulfadiazine cream applications.
Prior to the third healing treatment further culture samples were obtained, taken in this case with aspirate syringe from the exudate present on the wound surface. The appearance of the wound continued to improve, with an increase in granulation tissue and a reduction in the diameter of the ulcer, although the tibial plate continued to visible in part (Fig. 2A), in addition to a drop in the PCR value (73 mg/l). On this occasion we decided to initiate negative pressure therapy mainly aimed at ensuring the osteosynthesis material would remain covered and the healing treatment was spaced out to every 5 days. The culture obtained on that day would produce a negative result 5 days later.
Ten days later, after two more healing treatments where sevoflurane was used, it was observed that the wound had reduced in size and was completely covered with granulation tissue and the acute phase reactants had almost normalised (PCR: 13,5 mg/l); prior to the latest healing treatment a new culture sample was prepared (which tested negative). Due to favourable clinical evolution it was decided to discharge the patient from hospital with systemic oral antibiotic treatment (amoxicillin 1 g/8 h, trimetoprim-cotrimoxazol 160−800 mg/12 h and rifampicin 600 mg/24 h), keeping the wound covered with hydrophibre dressings of hydrocolloid with silver ions which was changed every 4 days. This outpatient antibiotic treatment was maintained for 45 days.
The protocol for outpatient healing performed every 4 days consisted in simply removing the dressing, irrigating the wound with sevoflurane and replacing the dressing with a new one. The wound reduced in size gradually, with no signs of any infection (Fig. 2B), and was completely healed over 2 months after the healing process began, thus achieving the objective of retaining the osteosynthesis material despite superinfection and thereby avoiding further surgery for the patient (Fig. 2C).
One year later it was necessary to extract all the osteosynthesis material due to mechanical complications, since a screw had protruded in the ankle joint. During the operation it was noted that there were no signs of infection in the bone tissue or soft tissue. One year later a control magnetic resonance was performed where degenerative signs in the angle joint were observed, without any symptoms suggestive of oseteomyelitis.
DiscussionIn this case of superinfection of osteosynthesis material caused by SARM, conservative treatment of the wound was successful and this avoided aggressive surgery for the elderly patient. The conservative treatment combined systemic antibiotherapy with topical antiseptic treatment, among which stands out the novel role of irrigating with sevoflurane, together with the important role of negative pressure therapy.
It is our belief that the sevoflurane played a major part in the initial favourable evolution of the wound up until the appropriate antibiotherpay was prescribed for the germs involved. The patient was initially treated with systemic antibiotics but the isolated germs in the sample taken on hospital admittance were resistant to these antibiotics. Logically this treatment could not have significantly contributed to the favourable clinical evolution of the wound during the first 5 days and yet from a clinical viewpoint there was a favourable evolution of the wound during that time. As we have already stated, we believe that the two applications of topical sevoflurane played an important role for this. Sevoflurane is a halogenated derivative of ether which is regularly administered by the inhaled route for surgical anaesthesia. Apart from this anaesthetic effect, the antibacterial effect of this family is also well known in in-vitro studies for both ether and its halogenous derivatives, sevoflurane included.4 In the specific case of sevoflurane, several favourable clinical experiences have also been described with the use of topical sevoflurane with an antimicrobial intention such as the curing of a recurring epidural abscess caused by E. coli5 or in the healing of a superinfected postoperative wound caused by multiresistant Pseudomonas aeruginosa and sensitive S. aureus in an immunodepressant patient after receiving a liver transplant.6 The anaesthetics of this family act as organic solvents and it is supposed that they act as local antiseptics by disruption of the bacterial membranes.4 This hypothetical non-specific mechanism of action would mean all types of germs could be treated, even those resistant to standard antibiotics,6 as was the case of this patient. Furthermore, the bactericidal effect could appear in a few minutes, as with other antiseptics.7 It could be considered that sevoflurane produces a chemical debridement which would also obviously affect the more superficial layer of fibroblasts, but they would be replaced by deeper layered fibroblasts. The final result would be that the granulation process of the wounds would not be interfered with and this would help to create a cleaner environment.
After applications of sevoflurane and cleaning of the wound, it was covered with a silver sulfadiazine cream and it is known that the silver ions possess a bactericidal effect against a large variety of microorganisms.8 It is therefore highly commendable to first treat infected wounds topically combining the eventual fast bactericidal effect of the sevoflurane with the bactericidal effect maintained over time due to the silver ions, particularly when the causative germs are resistant to standard antibiotics, as occurred in our case.
Sevoflurane also has a highly important added advantage compared with other topical antimicrobial products, since it produces a fast and intense analgesic /anaesthetic effect when it is irrigated on wounds,9 and this improves the quality of the irrigations and debridements and eases the processes of healing, as occurred in this case.
After the reception of the result of the culture the empirical antibiotic treatment was replaced by a combination of antibiotics specifically aimed at covering the SARM. However, this action did not ensure the therapeutic success in the case of osteosynthesis material being implicated, and it was highly probably that a biofilm had formed over the said osteosynthesis material. The biofilm hugely impedes the application of systemic antibiotics in sufficient concentration to act on the bacteria protected by the biofilm and consequently the percentage of therapeutic failure rates may be high.3 In our case the existence of the biofilm was not appropriately diagnosed, but there was a high probability that it existed, because it is very common in infections where gram positives are involved,10 particularly if they are polymicrobials as was the case described and the risk of therapeutic failure using systemic antibiotherapy exclusively was high. Due to this situation surgeons very frequently remove the osteosynthesis material,2 but in this case an attempt was made not to reach this point because it would have resulted in a series of aggressive actions for such an elderly patient. As an alternative to these surgical interventions there are authors who defend the possibility of irrigating the osteosynthesis material with antiseptics in an attempt to eradicate the biofilm,7 and this is what we believe occurred in this case with the application of sevoflurane, the silver sulfadiazine cream and the negative pressure therapy. As far as we know the solvent capacity of sevoflurane on biofilms has never been studied, although it is a highly appealing hypothesis.
With regard to negative pressure therapy, in this case the main indication was to keep the wound and the osteosynthesis material covered, but it is highly probably that this therapy would notably contribute to the favourable evolution of the wound from the moment it was put into practice. Considering its mechanism of action it is evidence that, in addition to encouraging the healing process, it also mechanically contributes to reducing or eliminating the bacterial load of the wound bed. One advantage of the non specific mechanism of action is that it enables infections caused by germs resistant to standard antibiotics to be treated.11
It is of note that the combination of the actions described (sevoflurane, silver sulfadiazine cream, negative pressure therapy) led to the healing of the infection and wound closure without any adverse effects and whilst maintaining ankle function. An inherent advantage of avoiding further operations was saving the patient from aggressive procedures and also saving on economic resources.
To conclude, the addition of sevoflurane to the topical treatment of infected surgical wounds has potentially outstanding advantages, particularly when the germs are resistant to standard treatments and there is osteosynthesis material to preserve. This new treatment therefore deserves to be studied in depth, ideally through a clinical trial which would compare the effect of applying or not applying sevoflurane to patients with infections similar to the case described and treated with a combination of systemic antibiotherapy, healing with silver sulfadiazine cream and debridement. Whilst these studies are being conducted, we would recommend assessing this therapeutic option for cases similar to the one we have described.
Level of evidenceLevel of evidence IV.
Conflict of interestsManuel Gerónimo Pardo has received fees from the company Vapogenix as a consultancy source and holds share options in this company.
Sergio Losa Palacios and Ainara Achaerandio de Nova have no conflict of interests to declare.
Please cite this article as: Losa Palacios S, Achaerandio de Nova A, Gerónimo Pardo M. Manejo multimodal conservador de material de osteosíntesis ante herida quirúrgica con sobreinfección polimicrobiana, incluyendo Staphylococcus aureus resistente a meticilina. Caso clínico. Rev Esp Cir Ortop Traumatol. 2020;64:125–129.