To show the results and advantages of using the negative pressure closure system in a pediatric population with infections and wound closure defects.
Materials and methodsA retrospective analysis was conducted on pediatric patients in whom the VAC® negative pressure wound closure system was used in the Shriners Hospital for Children, Mexico, from January 2008 to December 2012. We were able to include 8 patients treated with this system. We evaluated the cause for use, wound colonizing microorganism, number of days of stay at the hospital, number of times applied, interval of application, and number of days in the hospital until discharge after VAC® application, and final treatment.
ResultsThe average days after VAC application till discharge was 13.7 days. The final treatment in 7 of the 8 patients was direct closure or application of skin grafts for closure of the wounds.
DiscussionThrough this study we were able to observe that, after the application of this treatment, there was an increase in the granulation tissue at the wounds, as well as resolution of the infection.
ConclusionsWe were able to confirm the efficiency of this treatment in controlling the infection and decreasing skin defects, allowing an easier and earlier wound closure.
Se exponen los resultados y ventajas del uso del sistema de presión negativa (VAC®) en los pacientes pediátricos con defectos cutáneos y/o infecciosos.
Material y métodosAnálisis retrospectivo de los pacientes sometidos al uso del VAC® en el Hospital Shriners para Niños México, desde enero de 2008 a diciembre de 2012. Se incluyeron 8 pacientes tratados con el VAC®. Se evaluó el motivo de colocación, microorganismo colonizante de la herida, número de días de estancia, número de ocasiones aplicadas, intervalo de aplicación, número de días al alta posterior a la aplicación, y el tratamiento final.
ResultadosSe observó que el promedio de días desde la colocación al alta fue de 13,7. El tratamiento final en 7 de los 8 pacientes fue cierre directo de la herida o aplicación de injerto cutáneo.
DiscusiónMediante este estudio se pudo observar que después de la aplicación de este tratamiento hay una mejoría importante en la capacidad de granulación de las heridas, así como erradicación de las infecciones.
ConclusionesSe ha podido constatar la eficacia de este tratamiento en el control de la infección, y la disminución de los defectos cutáneos haciendo más sencillo y rápido el cierre de las heridas.
Deep infections in pediatric patients represent a major complication, especially in spine surgery and neuromuscular disorders, with an infection rate up to 20%, involving high morbidity and costs, increasing pain and hospital stay, as well as a challenge for orthopedic surgeons. The use of the vacuum-assisted closure system (VAC®) (KCI Inc., San Antonio, TX, USA) for the treatment of soft tissue defects in traumatic wounds1 and deep infections in pediatric orthopedics has increased considerably in the last decade. There are a number of works on the VAC® system, which generally report favorable results.2
The VAC® system includes a polyurethane or polyvinyl alcohol sponge, placed in the wound and connected by a discharge tube to a negative pressure device. This is sealed in order to create a vacuum and can then be used for days or weeks, changing the sponge every 48–72h. This technique can be used to cover the exposed bone or soft tissue defects, reducing chronic edema and increasing local blood supply. The controlled application of sub-atmospheric pressure, continuously or intermittently, aids the formation of granulation tissue, acts as a sterile barrier decreasing bacterial colonization and infection by up to 82%,3 drains fluids through the pores of the polyurethane sponge, approximates the edges of the wound and accelerates the healing process compared to traditional methods.
The benefit of the application of VAC® for control of infections has been demonstrated. It creates a hypoxic environment which modulates the growth of gram-negative bacteria and, in turn, stimulates angiogenesis and the growth of fibroblasts and epidermal cells.
The aim of this study is to describe the results in pediatric patients with chronic wounds treated with VAC® to control infections and demonstrate the decreased length of stay after its application.
Materials and methodsWe performed a retrospective analysis of patients undergoing the use of VAC® at Shriners Hospital for Children in Mexico between January 2008 and December 2012. We collected data from medical records and found 8 patients treated with this method who were included in the study regardless of the reason for the application of the VAC® system.
We evaluated the reason for the use of the system, the results of wound culture, the number of days of hospital stay, the frequency of application, the system change interval and the number of days until discharge after application, as well as the final treatment for the wounds.
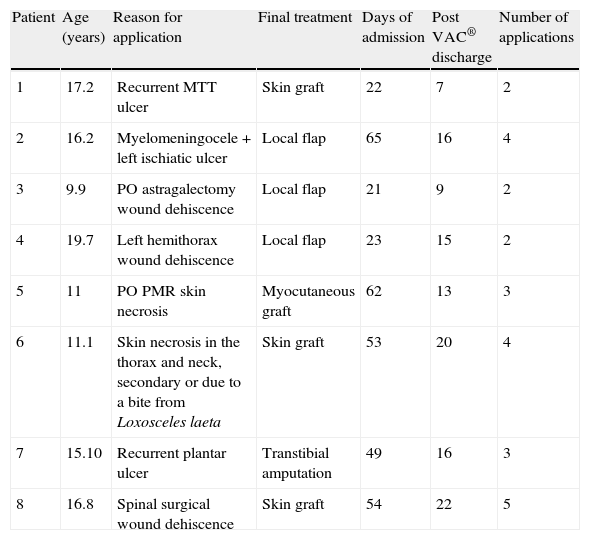
ResultsThe 8 patients in the sample analyzed in this study required the application of the VAC® system due to defects in wound closure. A wound culture was taken prior to the application and colonization by pathogenic microorganisms was found in all cases. Staphylococcus aureus was the most prevalent organism in these patient samples, followed by Enterococcus faecalis, in 4 and 3 patients, respectively. In 6 cases, the infection was monobacterial. The results of the variables analyzed are shown in Table 1.
Demographic data.
| Patient | Age (years) | Reason for application | Final treatment | Days of admission | Post VAC® discharge | Number of applications |
| 1 | 17.2 | Recurrent MTT ulcer | Skin graft | 22 | 7 | 2 |
| 2 | 16.2 | Myelomeningocele + left ischiatic ulcer | Local flap | 65 | 16 | 4 |
| 3 | 9.9 | PO astragalectomy wound dehiscence | Local flap | 21 | 9 | 2 |
| 4 | 19.7 | Left hemithorax wound dehiscence | Local flap | 23 | 15 | 2 |
| 5 | 11 | PO PMR skin necrosis | Myocutaneous graft | 62 | 13 | 3 |
| 6 | 11.1 | Skin necrosis in the thorax and neck, secondary or due to a bite from Loxosceles laeta | Skin graft | 53 | 20 | 4 |
| 7 | 15.10 | Recurrent plantar ulcer | Transtibial amputation | 49 | 16 | 3 |
| 8 | 16.8 | Spinal surgical wound dehiscence | Skin graft | 54 | 22 | 5 |
MTT: metatarsal; PMR: posteromedial release; PO: postoperative.
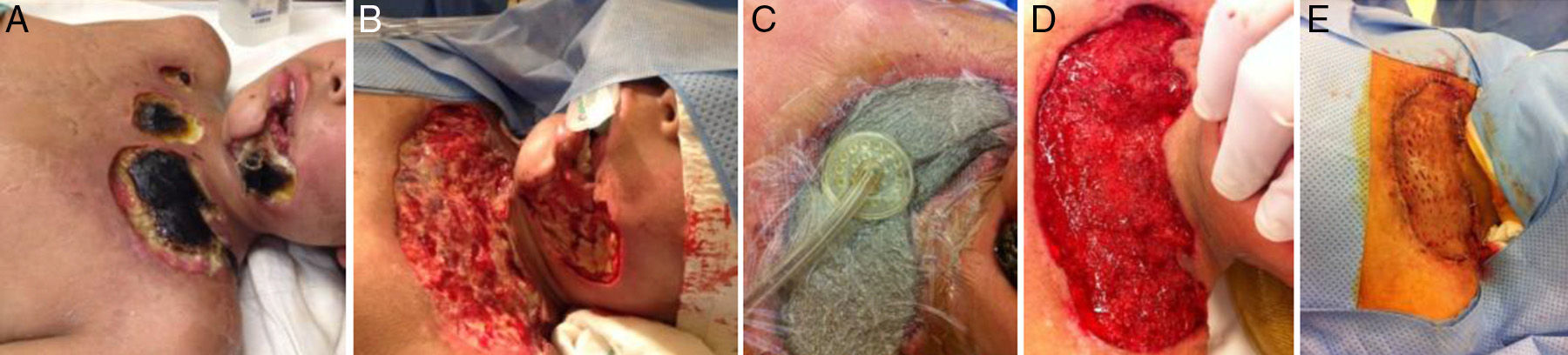
The mean application interval was 3 days, at an intermittent pressure of 125mmHg. We observed that the mean discharge time after applying the VAC® system was 14.7 days. Of all the patients who were administered the system, only 1 (Fig. 1) required a transtibial amputation due to the chronicity of the process and bone involvement. In the remaining cases there was no recurrence of the infectious process or new wound dehiscence, with complete healing by the final closure method selected by the surgeon after a monitoring period of 2 months.
DiscussionChronic wounds represent a challenge for any surgeon, especially in orthopedic surgery, in which implants act as a reservoir for infectious microorganisms. In recent years, the use of the VAC® system has revolutionized the way in which these injuries are treated, as it reduces swelling, so local perfusion is increased up to 4 times more than normal,4 stimulating the formation of large amounts of granulation tissue. In the study by Barnaby et al. there was a 50% decrease in the need for free or pedicled flaps for the coverage of defects in open fractures in children, with this method being reported as safer and more effective.1
The study by Suissa et al. observed a significant reduction in wound size compared with traditional methods,5 thereby decreasing hospitalization time. Regarding costs, no increase has been observed, despite the fact that the materials employed in the care of wounds with the VAC® system are more costly than with traditional treatment methods. This balance in costs is explained by a decrease in the need for staff to change wound dressings many times per day.6
Regarding infection control, we have not observed a decrease in the bacterial load within the wounds, although we have observed a decrease of non-fermenting Gram-negative microorganisms caused by the hypoxic environment. Establishing a hypoxic environment stimulates angiogenesis, fibroblasts and epidermal growth factors. We have also observed that continuous aspiration of excess fluid leads to decompression of small caliber blood vessels, increasing local blood flow. All these factors favor wound healing.7
In this study we examined the time elapsed for wound closure after application of the VAC® system and found that the mean time until discharge of patients after initiation of VAC® treatment was 37% of the total hospitalization time. This datum enabled us to verify the usefulness of adjuvant therapy for the control of infections, as well as the improvement in granulation tissue, which created the ideal conditions within the wounds for the application of skin grafts or local rotation flaps.
As noted in the study, we should emphasize that the wound closure treatment with negative pressure alone is not a substitute for lavage and surgical debridement. When considering this type of treatment we must bear in mind the natural progression of the injuries, as well as the need for appropriate antibiotic coverage according to microorganism susceptibility and the final treatment of injuries, which often require the application of skin grafts or local rotation flaps from healthy tissue (Fig. 2).8
ConclusionThe cases presented in this study showed a decrease in length of stay after application of VAC® treatment compared to the total time of stay; with a mean time until discharge of 14 days after VAC® application. This was due to an increase in granulation tissue and the lack of clinical evidence of infection, which generated favorable conditions for the application of the final treatment with local flaps or skin grafts. Only 1 case required a radical treatment due to bone involvement which prevented a feasible limb.
There are few studies on the use of the VAC® system in pediatric patients with orthopedic conditions, especially of neuromuscular origin. The results recorded in this study showed the efficacy of the treatment in this population. Thus, we recommend its use, in conjunction with adequately selected antibiotic treatment according to the susceptibility of the pathogen, for the treatment of chronic wounds in pediatric patients.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Dabaghi-Richerand A, Gómez-Chavarría J, González-Sánchez M, Saleme-Cruz J, Garavito E. Experiencia con el sistema de cierre de presión negativa en heridas crónicas en pacientes pediátricos: experiencia de 8 casos. Rev Esp Cir Ortop Traumatol. 2013;57:282–5.