To evaluate, by means of biomechanical analysis, functional alterations of gait and balance of patients with anterior cruciate ligament (ACL) injury.
Material and methodsTransversal analytical study on 64 people, 27 health subjects and 37 patients with ACL injury. Biomechanical analysis of gait in all individuals was performed by means of four tests: (1) kinematic test, to characterize gait pattern; (2) kinetic test, to characterize forces against the floor, duration of treads, symmetry of both legs, and the reproducibility of the gait; (3) pivot-shift test, to analyze the rotational stability of the knee on the sagittal axis; and (4) equilibrium test.
ResultsAlterations in kinematic and kinetic analysis were found in both the injured knee and the healthy knee compared to the control group. In the pivot-shift gait test there is a tendency to increase the forces on the three axes, both in the support leg and in the exit leg in patients with ACL injury, in comparison with healthy subjects.
ConclusionACL injury-induced changes in gait pattern, changes in forces against the floor, duration of treads, symmetry of both legs, and the reproducibility of gait and changes in rotational stability of the knee on the sagittal axis.
Evaluar, mediante un análisis biomecánico, la alteración funcional de la marcha y del equilibrio de pacientes con rotura del ligamento cruzado anterior (LCA).
Material y métodoEstudio analítico transversal en 64 sujetos, 27 sujetos sanos y 37 pacientes con lesión de LCA. A todos los sujetos se les realizó un análisis biomecánico de la marcha mediante cuatro pruebas: (1) prueba cinemática de la marcha, para caracterizar el patrón de marcha; (2) prueba de análisis cinético de la marcha, para analizar las características de las fuerzas ejercidas contra el suelo, la duración de las pisadas, la simetría entre ambas extremidades y la repetitividad del gesto analizado; (3) prueba de la marcha con pívot, para valorar la estabilidad rotacional de la rodilla alrededor del eje sagital; y (4) prueba de equilibrio.
ResultadosSe han encontrado alteraciones en el análisis cinemático y cinético tanto en la rodilla lesionada como en la sana respecto al grupo control. En la prueba de la marcha con pívot hay una tendencia al aumento de las fuerzas en los tres ejes, tanto en la pierna de apoyo como en la pierna de salida en los pacientes con rotura de LCA, en comparación con los sujetos sanos.
ConclusiónLa rotura del LCA produjo alteración del patrón de marcha, alteración de las fuerzas ejercidas contra el suelo, de la duración de las pisadas, de la simetría entre ambas extremidades y de la repetitividad del gesto durante la marcha y alteración de la estabilidad rotacional de la rodilla en el eje sagital.
Anterior cruciate ligament (ACL) tear is a very common injury, which also affects a range of young and physically active populations.1 Its incidence is estimated at .4–.8 injuries per 1000 people per year (aged between 10 and 64 years).2–4 ACL tear is related to sports activities such as football, handball, skiing or basketball in 65%–75% of cases,1,2,4–6 although approximately 25%–35% cases occur in the home, on public roads, in shopping centres or in the workplace.4 The mean age of patients with ACL tear is 28–35 years, with a higher proportion of males (58%–73%).2,4,5,7 However, if we examine risk populations (football, basketball and other contact sports), the incidence is higher in females than in males.3,8 There being more ACL tears in males than females would be explained by the fact that far more men carry out activities of risk for ACL tear than women.4,9
It is estimated that in approximately 70% of cases, ACL injury is caused by an indirect mechanism, which usually includes abrupt braking combined with a change of direction, pivoting or almost full extension of the knee after a jump.1,8,10,11 Direct contact injuries usually involve a translation force on the front of the leg that is fixed on the ground.1,8
ACL injury has been described as isolated in 10%–30% of cases,1,2 in 40%–45% of cases it is associated with some meniscal injury, and approximately 30%–35% is associated with another ligament injury.2,7
Anatomical reconstruction of the ACL has been of interest, since its function is directly related to its anatomy,12,13 and this in turn is directly related to knee function and consequently to gait pattern.14 Arthroscopic repair is currently the choice over open surgery, but there is still much controversy about the best repair procedure, which focuses on the number of fascicles (single fascicle, double fascicle or even triple fascicle); the choice of graft (allograft or autograft, goosefoot tendons, patellar tendon or quadriceps tendon); the fixation system to be used and the number and position of the tibial and femoral tunnels, and numerous conformations and variables have been described.15–19 Determining how ACL injury affects knee function could be the starting point for studying the best way to reconstruct the ACL and restore joint function.
The aim of this study was to assess the functional changes that occur in patients with ACL tears through a biomechanical analysis of gait and balance.
MethodsSixty-four subjects were studied to undertake this paper, 27 healthy subjects and 37 patients with ACL injury, of whom 7 were excluded from the study after surgery for various reasons. All the patients were treated in a mutual insurance company, and therefore their injuries were the result of an accident at work. A cross-sectional clinical study was conducted, comparing the knee functionality of the healthy subjects – 27 subjects – (control group) with that of the subjects with compete ACL tear prior to surgery – 30 patients – (pathological group). Data collection was done prospectively, including patients with consecutive ACL ruptures, only discarding those who did not meet the inclusion criterion. The study was approved by the ethics committee of our centre and all individuals signed the corresponding informed consent form for inclusion in the study and subsequently undergoing the intervention.
The following inclusion/exclusion criteria were used:
- •
Inclusion criteria for healthy individuals: 1) adult male under 40 years of age and over 16 years of age; and 2) no previous or current disease at lower limb level.
- •
Inclusion criteria for pathological individuals: 1) adult male under 40 years of age and over 16 years of age; 2) with no previous or current disease at lower limb level; 3) clinical suspicion of ACL tear (anamnesis and physical examination, including positive Lachman’s and anterior drawer tests); and 4) MRI suspicion of full ACL tear.
- •
Exclusion criteria for pathological individuals: 1) meniscal tear requiring suturing; 2) absence of surgical confirmation of ACL tear, either because it does not exist or because the tear is partial; and 3) onset of some other condition that could alter functional assessment of the knee.
Patient data were obtained relative to age, height and body weight.
For the functional assessment of the knee, the subjects underwent 4 tests based on 3D measurements of relative movements between the femur and the tibia and on the analysis of ground reaction forces recorded using a dynamometric platform: (1) kinematic gait test; (2) kinetic gait analysis test; (3) pivot-shift gait test; and 4) equilibrium test. The equipment and software of the Institute of Biomechanics of Valencia (IBV) were used to conduct these tests.
The kinematic gait test combines the kinetic information obtained from the force platforms and the kinematic information provided by the photogrammetry system to characterise the gait pattern of the subjects participating in the study. This is done using Kinescan/IBV software synchronised with a Dinascan/IBV force platform. In this test, the internal forces and joint moments of the lower limb (knee and ankle) are measured. Variables: mean knee mobility range; maximum mobility reaching the knee; maximum angular velocity reaching the knee; mean angular velocity of the knee; mean mobility range of the ankle; maximum mobility range reaching the ankle; maximum angular velocity reaching the ankle; mean angular velocity of the ankle; knee moment standardised for the 5th, 50th and 95th percentiles; ankle moment, standardised for the 5th, 50th and 95th percentiles. The angular velocities and accelerations and the knee and ankle moments are relative to body weight.
Kinetic gait analysis is performed on an instrumented walkway by means of a DINASCAN-IBV extensometric-type dynamometric platform, which records the force exerted against the floor by a subject when walking on it. Using NedAMH/IBV software it is possible to obtain information on the characteristics of this force, duration of treads, symmetry between both limbs and repetitiveness of the gesture analysed. Variables: velocity; support time; braking force; propulsion force; take-off force; oscillation force; Fx morphology (antero-posterior component); Fy morphology (medio-lateral component); Fz morphology (vertical component). The forces are expressed as a percentage of body weight. Morphologies are expressed as a percentage of the pattern of normality (considering 100 to be the pattern of normality). Finally, an overall assessment of gait is obtained, which is also expressed as a percentage of the pattern of normality.
The pivot-shift gait test comprises 2 phases, consisting of a gait test to which a 90-degree change in direction has been added, by stepping on the force platform with respect to the initial trajectory. The combination of both phases forms a rotation of the body over the support leg, while it remains motionless, at this moment a practically pure rotation is applied to it from the body weight. In this test, force (f)and derivative force (df) values are obtained in the anteroposterior (x) mediolateral (y) and vertical (z) axes, with the 5th, 50th and 95th percentiles, both in the support leg and in the exit leg (pis2_). The force values are expressed in Newtons (N) and are relative to body weight; on the antero-posterior axis the positive values refer to forward and the negative values to backward; on the mediolateral axis the positive values refer to sideways and the negative values to medially, and on the vertical axis the positive values refer to upward and the negative values to downward.
The equilibrium test is performed with the aid of NedSVE/IBV posturography, which is a system for the functional assessment of human balance disorders based on dynamometric platforms. This application combines static posturographic assessment tests with dynamic tests, providing an overall index of the patient’s balance assessment.20,21 The test protocol consists of two tests: dynamic sensory evaluation, based on the Romberg test, and an assessment of control and ability.
The tests were performed in our medical-surgical centre, with the apparatus and material provided by the IBV.
Statistical analysisData collection respected the confidentiality and anonymity of the patients and was entered into a Microsoft Excel 2013 database. Once the results were obtained for each of the tests, the statistical treatment was performed using SPSS 22. The mean and standard error of the mean (SEM) of the subjects belonging to each group was calculated for each of the variables. A test for normality was performed for quantitative variables (Shapiro–Wilk test) and for homogeneity of variance (Levene’s test). Comparisons between the means of the variables of each of the groups were made by one-way analysis of variance (ANOVA) with a post-hoc test of multiple comparisons (parametric —Bonferroni—, or nonparametric —Mann-Whitney or Kruskal Wallis—, depending on the results of the test for normality and homogeneity of variance). Statistically significant differences were considered for p values <.05.
ResultsTwenty-seven healthy subjects and 30 subjects with ACL tears participated in this study. The age (30±1year), weight (82±2) and height (176±1cm) of the subjects with ACL tear were not significantly different from those in the control group (31±1year, 79±2kg and 175±1cm).
Kinematic gait testThe kinematic gait test was performed on healthy subjects and on subjects with ACL tear. In the latter, each of the different parameters were obtained for both the healthy leg and the injured leg.
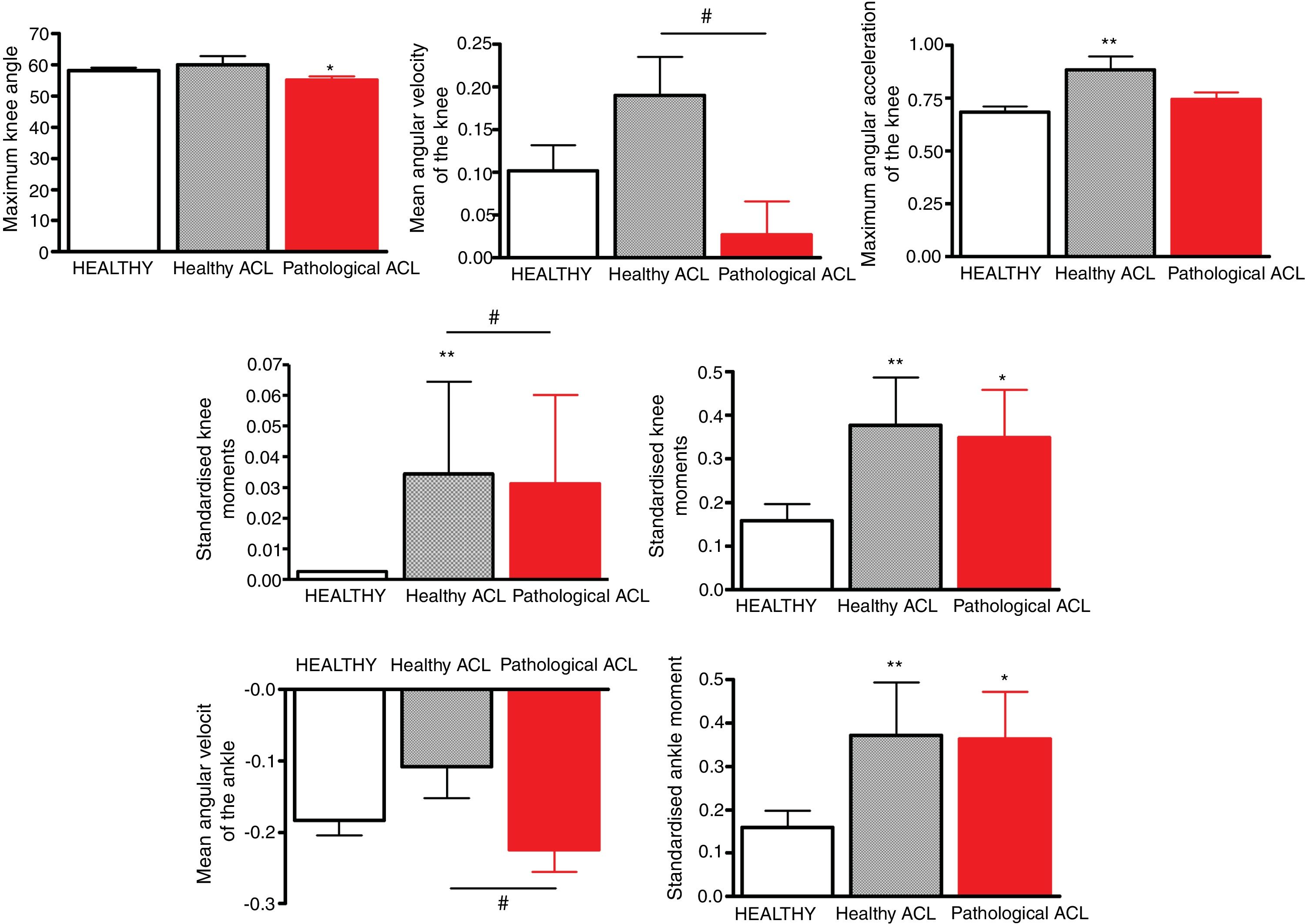
In the healthy leg of the subjects with ACL tear, the maximum angular acceleration of the knee, standardised knee moment 5th (Mrod_norm_p5) and 50th (Mrod_norm_p50) percentiles and the standardised ankle moment 50th percentile (Mtob_norm_p50) were significantly higher than in the healthy subjects; in the leg with ACL tear the maximum knee angle was significantly lower and the standardised knee and ankle moments 50th percentile (Mrod_norm_p50 and Mtob_norm_p50) were significantly higher than in the healthy subjects (Fig. 1).
Kinematic test. Maximum knee angle, mean angular velocity of the knee, maximum angular velocity of the knee, standardised knee moments 5th and 50th percentiles, mean angular velocity of the ankle and standardised ankle moment 50th percentile in the kinematic test in the control subjects (HEALTHY, N=50) and in subjects with ACL tear(N=30), in both the healthy leg (LCA_sano) and the injured leg (LCA_patol). The values are expressed as mean±SEM.
*p<.05.
**p<.01 Significantly different compared to control subjects.
#p<.05.
##p<.01 significantly different compared to healthy ACL.
The mean angular velocity of the knee, the standardised knee moment 5th percentile (Mrod_norm_p5) and mean angular velocity of the ankle were significantly lower in the injured leg than in the healthy leg, without any significant differences in any of the cases compared to the value obtained in the healthy subjects (Fig. 1).
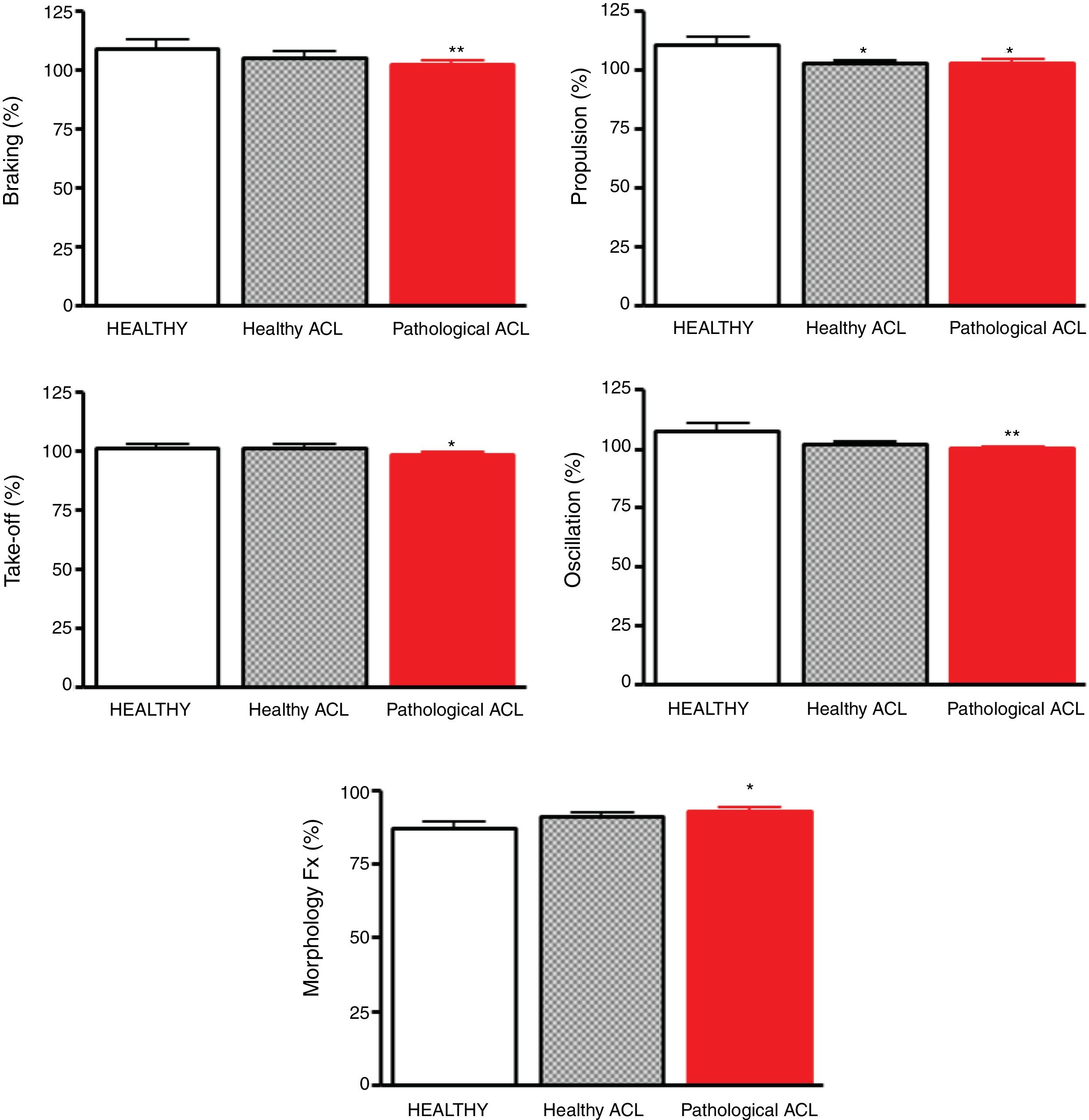
Kinetic gait testThe kinetic gait test was performed on healthy subjects and subjects with ACL tear. In the healthy leg of the subjects with ACL tear, the propulsion force was significantly lower than in the healthy subjects; in the leg with the ACL tear the braking, propulsion, take-off and oscillation forces were significantly lower and the Fx morphology was significantly higher than in the healthy subjects (Fig. 2).
Kinetic test. Kinetic test of gait in control subjects (HEALTHY, N=24) and in subjects with ACL tear (N=30), both in the healthy leg (LCA_sano) and in the injured leg (LCA_patol). The values are expressed as mean±SEM.
*p<.05.
**p<.01 significantly different compared to the control subjects.
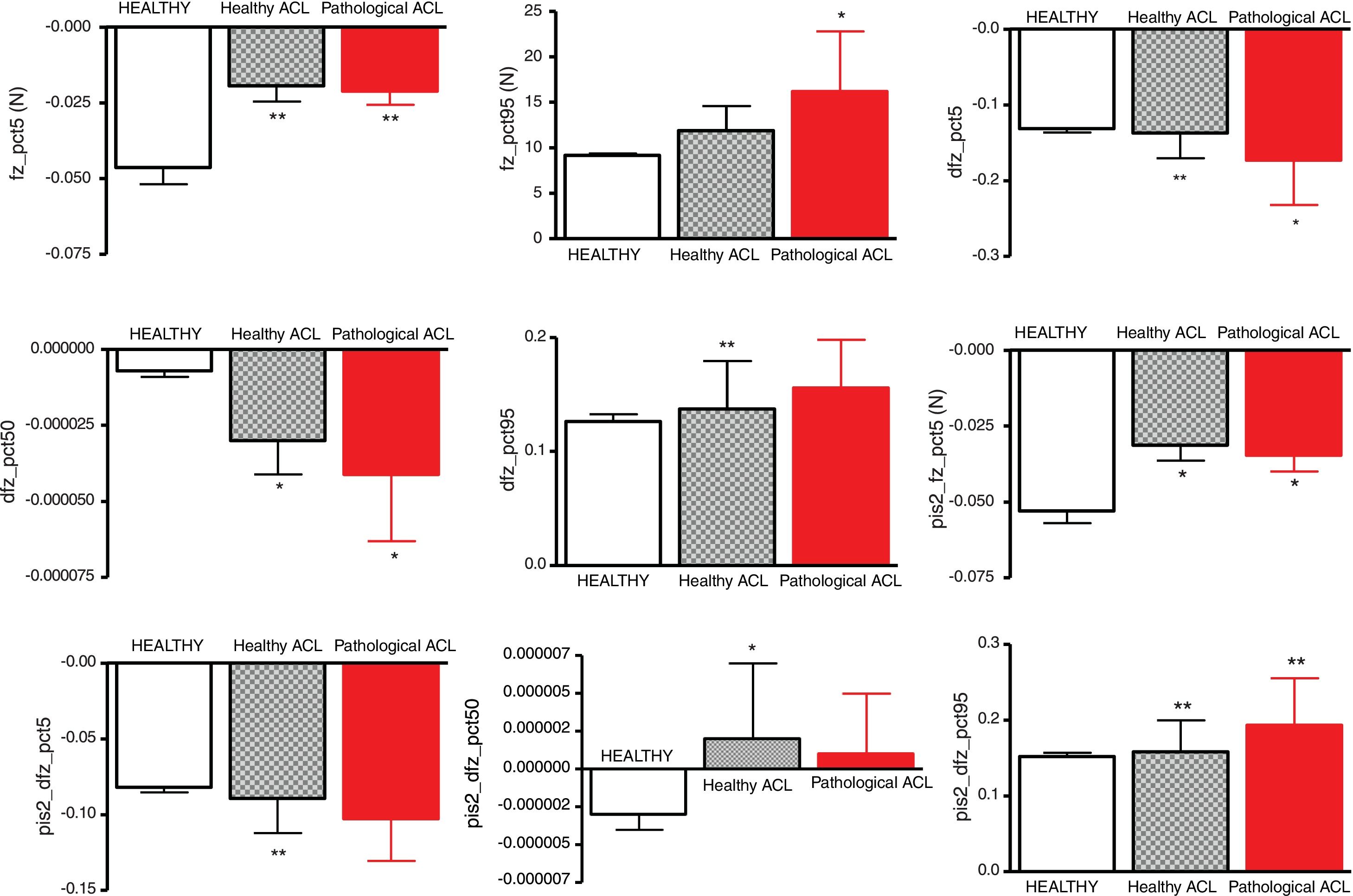
The pivot-shift gait test was performed on the healthy subjects and the subjects with ACL tear. In the latter, each of the different parameters were obtained for both the healthy leg and the injured leg. This study shows in that the subjects with ACL tear there was a tendency to increase forces on the 3 axes, anteroposterior, mediolateral and vertical, both in the support leg and the exit leg, compared to the healthy subjects.
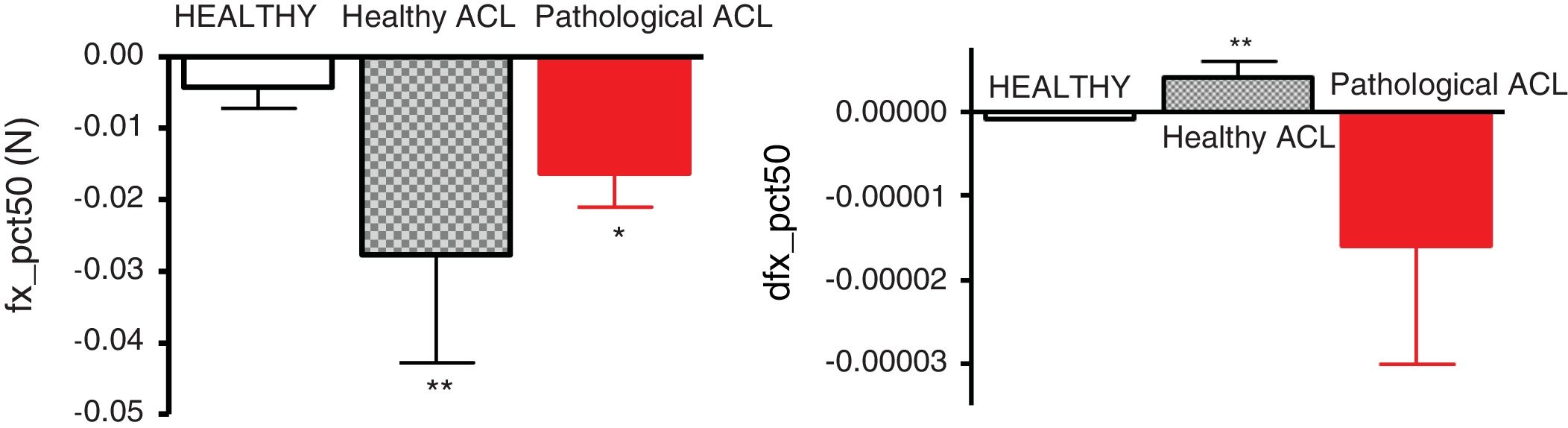
In the antero-posterior axis (Fig. 3) the 50th percentile force (fx_pct50) was significantly higher in the subjects with ACL tear than in the control subjects, both in the injured leg and in the healthy leg, and the 50th percentile force derivative (dfx_pct50) was significantly higher in the healthy leg than in the control subjects, without there being significant differences between both legs in the injured subjects for any of the 2 variables.
Pivot-shift gait test, anteroposterior axis. Force and derivative force on the anteroposterior x axis, in the 2 legs of control subjects (HEALTHY, N=50) and in subjects with ACL tear (N=30), both in the healthy leg (LCA_sano) and in the injured leg (LCA_patol). The positive values refer to forward and the negative values to backward. The values are expressed as mean±SEM.
*p<.05.
**p<.01 significantly different compared to control subjects.
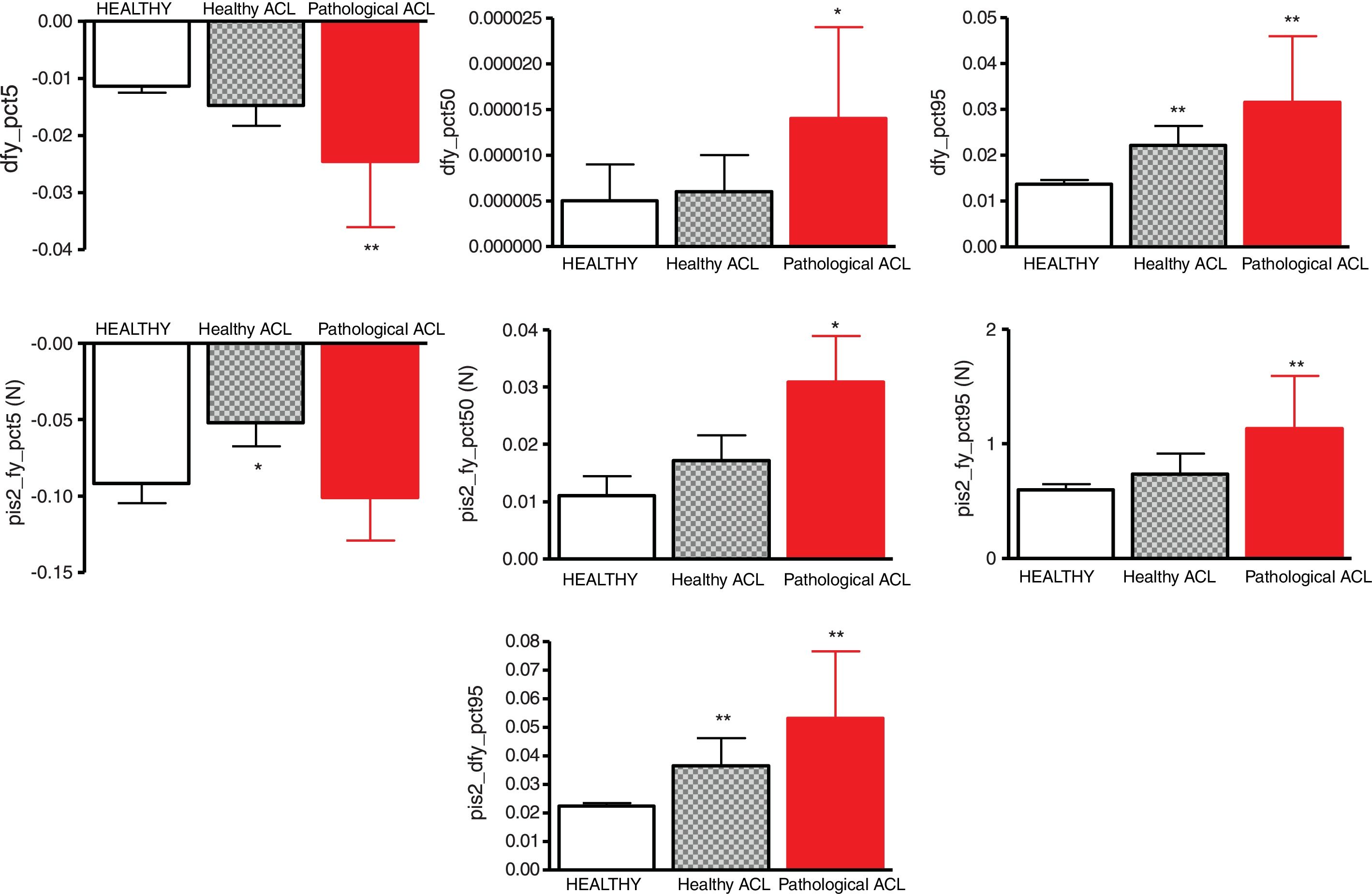
In relation to the mediolateral axis (Fig. 4), in comparison to the healthy subjects, the subjects with ACL tear presented lower force values on the healthy leg in the 5th percentile (pis2_fy_pct5) and significantly higher forces on the injured leg for the 50th (pis2_fy_pct50) and 95th (pis2_fy_pct95) percentiles, with no significant differences in the remaining force values. In addition, in the support leg, the force derivative values in the 5th percentile (dfy_pct5) and in the 50th percentile (dfy_pct50) were higher than in the control subjects in the injured leg; the 95th percentile force derivative values (dfy_pct95) were significantly higher in the injured leg and in the healthy leg, both in the first tread (support leg) and the second tread (exit leg).
Pivot-shift gait test, mediolateral axis. Force and derivative force on the mediolateral axis and, on the support leg and on the exit leg (pis2_), on the 2 legs of control subjects (HEALTHY, N=50) and in subjects with ACL tear (N=30), both on the healthy leg (LCA_sano) and on the injured leg (LCA_patol). The positive values refer to towards the lateral area and the negative to towards the medial area. The values are expressed as mean±SEM.
*p<.05.
**p<.01 significantly different compared to control subjects.
On the vertical axis (Fig. 5), compared to the healthy subjects, the 5th percentile force (fz_pct5) in the injured leg and in the healthy leg was significantly lower, both on the first tread (support leg) and on the second tread (exit leg, pis2_). On the first tread the 95th percentile force (fz_pct95) was significantly higher in the injured leg than in the control subjects, and z axis force derivative 5th (dfz_pct5) and 50th (dfz_pct50) percentiles was significantly higher than in the control subjects in the injured leg and in the healthy leg, and in the 95th percentile (dfz_pct95) it was significantly higher in the healthy leg than in the control subject. On the second tread (exit leg), the force derivative values 5th percentile (pis2_dfz_pct5) were significantly higher and those of the 50th percentile (pis2_dfz_pct50) were significantly lower in the healthy leg than in the control subjects, while the values corresponding to the 95th percentile (pis2_dfz_pct95) were significantly higher than in the control subjects, both in the healthy leg and in the injured leg for the exit leg.
Pivot-shift gait test, vertical axis. Force and derivative force on the vertical z axis, on the support leg and on the exit leg (pis2_), on the 2 legs of the control subjects (HEALTHY, N=50) and in subjects with ACL tear (N=30), both in the healthy leg (LCA_sano) and in the injured leg (LCA_patol). The positive values refer to upwards and the negative to downwards. The values are expressed as mean±SEM.
*p<.05.
**p<.01 significantly different compared to control subjects.
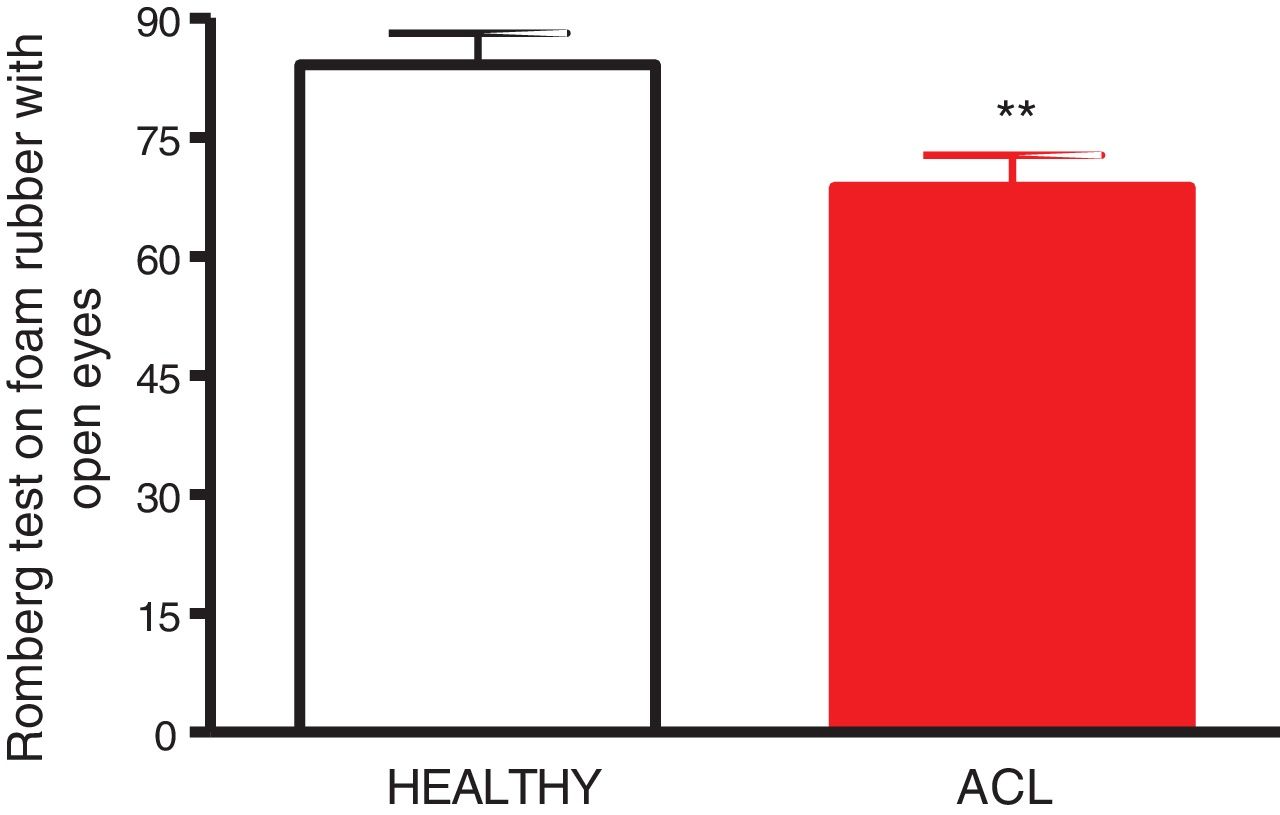
The equilibrium test was performed on the healthy subjects and the subjects with ACL tear. No statistically significant differences were observed between the injured and healthy subjects in any of the parameters analysed with this test, except in the Romberg test on foam rubber with eyes open, which was significantly less in the subjects with ACL tear than the healthy subjects (Fig. 6).
DiscussionIn the subjects with ACL tear, in the kinematic test, a decrease in maximum knee angle was observed, which coincides with that observed in the series by Hemmerich et al.,22 and an increase in the knee and ankle joint moments of the injured leg. López Hernández et al.23 attribute kinematic alterations of the injured leg, at least in part, to quadriceps atrophy after ACL tear, which is interpreted as a protective mechanism that reduces anterior tibial translocation and reduces the sensation of rotational instability. In the healthy leg of injured subjects, an increase in knee and ankle joint moments is also observed, and in addition, an increase in angular acceleration of the knee. This suggests that these alterations in the angular parameters in the injured knee are compensated for by changes in the standardised knee and ankle moments of both legs. Between both legs of the subjects with ACL tear, a lower mean angular velocity of the knee and ankle and a lower standardised knee moment in the injured leg than in the healthy leg are observed, but none of the values are significantly different from the control group, suggesting that small alterations in the injured knee are compensated for by small adaptive changes in the healthy knee. Fuentes et al.24 described that of all the parameters measured in the kinematic test of gait, only a few are altered and, moreover, the parameters that are altered are mostly not due to incapacity of the knee, but rather an attempt by the knee to protect itself against the instability caused by the ACL tear. However, these compensatory changes, modifying the biomechanics of walking, could contribute to the onset of osteoarthritis of the knee.25
ACL tear affects gait kinetics, especially the vertical forces, particularly in jumping exercises.23 In the kinetic test the subjects with ACL tear presented a reduction in braking force, propulsion, take-off and oscillation of the injured leg, while in the healthy leg they presented a decrease in propulsion force, without significant changes in the rest of the parameters measured in this test. We should highlight that the overall assessment parameter of the subjects’ gait, both the pathological and the healthy subjects, had assessments of over 90%, regardless of the leg studied, and with no significant differences between the injured leg and the healthy leg of the subjects with ACL tear, or either of the 2 legs with the healthy subjects, which indicates that despite the injury all the subjects had normal values in their lower limbs with respect to this parameter. A possible explanation for this could be that some of the alterations in the parameters observed are not a consequence of the injury, but part of adaptive mechanisms that allow the subject to maintain a normal overall gait, despite having alterations in various parameters. These results indicate that ACL tear is not highly important in the gait of the individuals under the conditions studied (in a straight line on flat and stable ground).
In the pivot shift gait test, this study shows that the subjects with ACL tear tended to increase forces on all 3 axes, anteroposterior, medial and vertical, in both the support and the exit leg, compared to the healthy subjects. The increase in forces during walking is transmitted via shock waves from the foot, through the musculoskeletal system, to the head, which can affect the natural shock absorbers (joints, muscles, intervertebral discs, etc.) and may case degenerative changes in them if the situation persists over a prolonged period of time.26 Fuentes et al.24 suggested that adaptive gait changes, with reduced internal rotation of the knee and a greater flexion angle, occur in subjects with ACL tears, to prevent anterolateral rotational instability of the knee, which would be less efficient for high gait velocities.
In the equilibrium test, compared to the healthy subjects, the subjects with ACL tears had a decrease in the Romberg test score on rubber foam with open eyes, although they did not show changes in the dynamic sensory evaluation that jointly assesses the results obtained with the different modalities of the Romberg test (eyes open/closed and stable or instable surface – foam rubber). The rest of the parameters measured in this test were not significantly different from the healthy subjects. The absence of major differences in the equilibrium test may be due to the fact that equilibrium tests with bipodal support are not sufficiently sensitive to detect possible disturbances in balance or postural control caused by ACL injuries,27 contrary to that described in previous papers.28
In this paper we describe functional impairments that occur in patients with ACL tear in gait, rotational knee stability and balance. This gives us a starting point for assessing how this function is restored with the ACL reconstruction techniques currently used and offers us the possibility of comparing them or devising new techniques that attempt to restore knee functionality in a more physiological way.
ConclusionsACL tear causes changes in gait pattern, changes in forces against the ground, tread duration, symmetry between both limbs and reproducibility of gait, impaired rotational knee stability on the sagittal axis and impaired balance with bipodal support.
Further studies are necessary to determine the best anatomical and functional assessment tests for ACL tear patients. Studies of impaired rotational stability under stress (stairs, running or jumping) and balance measurements with monopodal support could be considered.
Level of evidenceLevel of evidence ii.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sánchez-Alepuz E, et al. Evaluación funcional de los pacientes con rotura del ligamento cruzado anterior. Estudio analítico transversal. Rev Esp Cir Ortop Traumatol. 2020;64:99–107.