To describe iatrogenic lesions of the peripheral nervous system and their relationship with different orthopaedic and traumatological procedures, through their assessment by means of electromyographic study.
Material and methodsRetrospective descriptive study of the electromyographies performed in the clinical neurophysiology service of the Hospital General Universitari de Castelló between July 2015 and March 2019, recovering those in which the aetiology was diagnosed as iatrogenic in relation to surgical procedures and analysing those that were initiated after orthopaedic and traumatological procedures.
ResultsOf the total number of electromyographies reviewed, 1.37% corresponded to iatrogenic surgical lesions and 55.1% of these were secondary to orthopaedic surgery and traumatology procedures, the incidence in relation to the procedures performed was 0.65%. The most frequent locations related to injuries were the lumbar spine, hip and hand/wrist. Injuries due to postural causes not directly related to the surgical field are noteworthy.
ConclusionIatrogenic injuries to the peripheral nervous system after orthopaedic surgery and traumatology procedures are infrequent, but given their mechanism of injury and the high severity of most of them, it would be advisable to implement corrective mechanisms to reduce their incidence.
Level of evidence: IV.
Describir las lesiones iatrogénicas de sistema nervioso periférico y su relación con los diferentes procedimientos ortopédicos y traumatológicos, a través de su valoración mediante estudio electromiográfico.
Material y métodosEstudio descriptivo retrospectivo de las electromiografías realizadas en el servicio de neurofisiología clínica de Hospital General Universitari de Castelló en el periodo comprendido entre julio de 2015 y marzo de 2019, recuperando aquellas en las que la etiología se diagnosticó como iatrogénica en relación con procedimientos quirúrgicos y analizando las que se iniciaron tras procedimientos ortopédicos y traumatológicos.
ResultadosDel total de electromiografías revisadas el 1,37% correspondieron con lesiones iatrogénicas quirúrgicas y de ellas el 55,1% fueron secundarias a procedimientos de cirugía ortopédica y traumatología, la incidencia respecto a los procedimientos realizados fue del 0,65%. Las localizaciones más frecuentemente relacionadas con las lesiones fueron el raquis lumbar, cadera y mano/muñeca. Son destacables las lesiones por causa postural sin relación directa con el campo quirúrgico.
ConclusiónLas lesiones iatrogénicas del sistema nervioso periférico tras procedimientos de cirugía ortopédica y traumatología son poco frecuentes, pero dado su mecanismo lesivo y la elevada gravedad en la mayor parte ellas, sería aconsejable la implementación de mecanismos correctores para reducir su incidencia.
Nivel de evidencia: IV.
Iatrogenesis associated with the complications of surgical procedures has been scarcely covered in published studies, probably because it has been considered difficult to avoid, inherent to the surgical technique used and due to its medico-legal implications. Iatrogenic lesions in the peripheral nervous system can be caused by various mechanisms, by drugs, manipulations, and after and by surgical procedures, both directly and indirectly.1–3 We found no review that specifically analyses iatrogenesis associated with trauma and orthopaedic surgery (TOS) procedures. We consider that it is of interest for practitioners to know which procedures are most associated with iatrogenic injuries and the nerve structures involved, to determine the riskiest surgical interventions and manoeuvres. This study identifies the iatrogenic injuries related to surgical procedures referred to the clinical neurophysiology department of the Hospital General Universitari de Castelló for electromyographic assessment and analyses those corresponding to trauma and orthopaedic procedures. Electromyography (EMG) is a diagnostic technique that identifies the injured nerve structure to establish the type and degree of injury and to help in the indication for prompt reparative surgery. As the lesion progresses, EMG can detect early signs of active reinnervation and progression of reinnervation for prognostic and therapeutic purposes.4–7
Material and methodsA retrospective descriptive study reviewing all electromyographies performed in our department between July 2015 and March 2019. The clinical neurophysiology department of the Hospital General Universitari de Castelló is responsible for the electromyographic studies requested in the Castelló health area and the Vinaròs health area. We have included cases in the present review from these two health areas, although the surgical procedure for neurological symptoms could have been performed in other public or private centres. The procedures followed complied with the ethical standards of the committee for responsible human experimentation, the World Medical Association, and the Declaration of Helsinki. In accordance with our centre's protocols on the right to privacy, no patient data appear in this article.
A clinical history is taken from all patients referred to our department for EMG. They undergo a clinical neurological examination and are informed of the procedure.
The following were defined as injuries of iatrogenic aetiology and therefore as inclusion criteria for the study:
- •
Absence of signs and symptoms of peripheral nerve damage prior to the surgery performed.
- •
Sudden onset of symptoms observed objectively after the surgical procedure performed.
- •
Topography of the injury consistent with the surgical manoeuvres performed or associated with surgical positioning.
- •
Injury diagnosable by EMG.
Injuries associated with surgical procedures that did not meet the above criteria were excluded from the study.
The cases found were classified according to the specialty performing the procedure. Each case from TOS was reviewed to identify the surgical procedure performed, the injured structure and extent of injury on EMG. All scans were performed within 21–75 days from the date of surgery, which enabled adequate assessment of the degree of injury in an acute injury situation.
The anatomical location was classified according to the surgical reports as articular, specifying the joint operated, and extra-articular, specifying the injured bone or structure operated. The data obtained in cases secondary to TOS were divided into two groups according to the procedures performed, one group where the reason for surgery was a trauma injury and another group where the intervention was for a non-trauma reason. This classification was made based on the difference in the type of lesions operated and surgery scheduling, with trauma lesions being performed urgently in most cases and non-trauma cases being delayed. Spinal surgery was divided into cervical and lumbosacral surgery. Cases of iatrogenic injury not directly associated with the surgical field were identified; these were classified as positioning injuries if they were consistent with the surgical position and did not correspond topographically to locoregional anaesthesia if this had been used. These cases were included in each group according to whether the surgery was for a trauma or a non-trauma condition.8,9
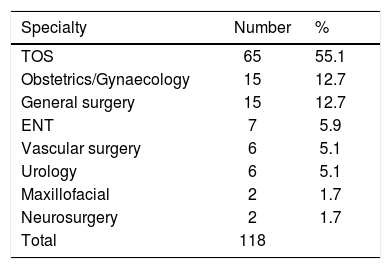
ResultsOf the total number of scans performed (9404), 129 cases were identified as being of surgical iatrogenic aetiology, i.e., 1.37% of the total. The 129 scans identified related to 118 patients, since 11 of them underwent a control scan during the period studied, of which 63 were female and 55 male. Of the total number of patients identified, in 65 onset of the injury followed an TOS procedure, which comprises 55.1% of the total. The age range was between 22 and 80 years with a mean age of 55.7 years. Female patients numbered 33 and male patients 32. Given the patients’ diverse provenance, it was only possible to calculate the incidence of iatrogenesis for cases from the Castelló area. In this area there were 8603 surgical TOS procedures in total over the period studied, and of the total number of patients studied (65) 56 underwent surgery in this area, giving an incidence of 0.65%. From the remaining specialties in which an iatrogenic injury was identified, the cases associated with gynaecology and obstetrics procedures and general surgery stand out. Table 1 shows the number of patients affected by specialty and their percentage with respect to the total number of iatrogenic surgical injuries.
Showing the number of patients affected by specialty and their percentage of the total number of surgical iatrogenic injuries.
| Specialty | Number | % |
|---|---|---|
| TOS | 65 | 55.1 |
| Obstetrics/Gynaecology | 15 | 12.7 |
| General surgery | 15 | 12.7 |
| ENT | 7 | 5.9 |
| Vascular surgery | 6 | 5.1 |
| Urology | 6 | 5.1 |
| Maxillofacial | 2 | 1.7 |
| Neurosurgery | 2 | 1.7 |
| Total | 118 |
ENT: ear, nose and throat; TOS: trauma and orthopaedic surgery.
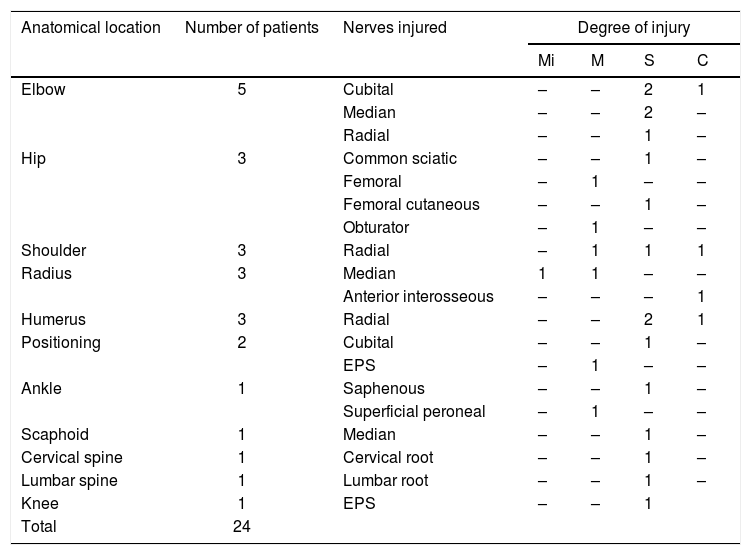
Of the total 65 patients, 24 sustained an injury in the context of surgery for trauma reasons and the remaining 41 in the context of surgery for non-trauma reasons.
In some locations the number of injured structures is greater than the number of patients. This is because there were cases in which two nerves were injured.
Injuries were classified based on the EMG into degrees of axonotmesis: mild, moderate, severe, and complete. It should be noted that the electromyographic findings recorded for an injury classified as a complete axonotmesis and a neurotmesis are equivalent, and therefore we make no distinction between them in this review. No injuries were classified as neurapraxia, and therefore they are not included in the results.
The results for each group are shown in two different tables. Table 2 shows the cases indicated for trauma surgery and Table 3 shows the cases indicated for non-trauma surgery.
Cases identified after indication for trauma surgery. Each row shows, in descending order of cases, the location of surgery, number of patients and the nerve structures injured, specifying their corresponding degree of axonotmesis (Mi – mild, M – moderate, S – severe, C – complete).
| Anatomical location | Number of patients | Nerves injured | Degree of injury | |||
|---|---|---|---|---|---|---|
| Mi | M | S | C | |||
| Elbow | 5 | Cubital | – | – | 2 | 1 |
| Median | – | – | 2 | – | ||
| Radial | – | – | 1 | – | ||
| Hip | 3 | Common sciatic | – | – | 1 | – |
| Femoral | – | 1 | – | – | ||
| Femoral cutaneous | – | – | 1 | – | ||
| Obturator | – | 1 | – | – | ||
| Shoulder | 3 | Radial | – | 1 | 1 | 1 |
| Radius | 3 | Median | 1 | 1 | – | – |
| Anterior interosseous | – | – | – | 1 | ||
| Humerus | 3 | Radial | – | – | 2 | 1 |
| Positioning | 2 | Cubital | – | – | 1 | – |
| EPS | – | 1 | – | – | ||
| Ankle | 1 | Saphenous | – | – | 1 | – |
| Superficial peroneal | – | 1 | – | – | ||
| Scaphoid | 1 | Median | – | – | 1 | – |
| Cervical spine | 1 | Cervical root | – | – | 1 | – |
| Lumbar spine | 1 | Lumbar root | – | – | 1 | – |
| Knee | 1 | EPS | – | – | 1 | |
| Total | 24 | |||||
EPS: external popliteal sciatic nerve.
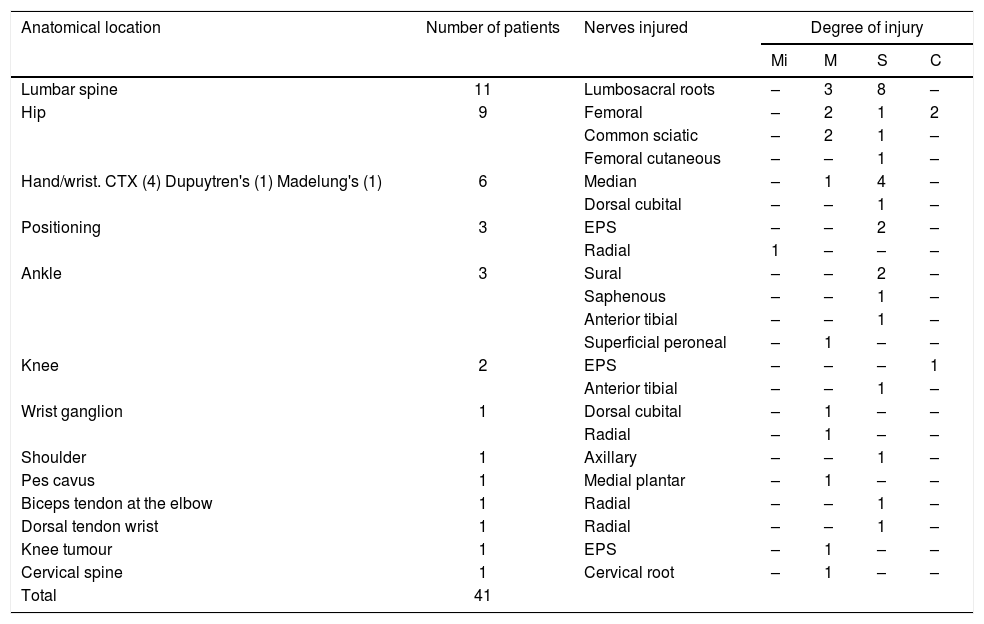
Cases identified after non-traumatic indication for surgery. Each row shows, in descending order of cases, the number of patients and nerve structures injured, specifying their corresponding degree of axonotmesis (Mi – mild, M – moderate, S – severe, C – complete).
| Anatomical location | Number of patients | Nerves injured | Degree of injury | |||
|---|---|---|---|---|---|---|
| Mi | M | S | C | |||
| Lumbar spine | 11 | Lumbosacral roots | – | 3 | 8 | – |
| Hip | 9 | Femoral | – | 2 | 1 | 2 |
| Common sciatic | – | 2 | 1 | – | ||
| Femoral cutaneous | – | – | 1 | – | ||
| Hand/wrist. CTX (4) Dupuytren's (1) Madelung's (1) | 6 | Median | – | 1 | 4 | – |
| Dorsal cubital | – | – | 1 | – | ||
| Positioning | 3 | EPS | – | – | 2 | – |
| Radial | 1 | – | – | – | ||
| Ankle | 3 | Sural | – | – | 2 | – |
| Saphenous | – | – | 1 | – | ||
| Anterior tibial | – | – | 1 | – | ||
| Superficial peroneal | – | 1 | – | – | ||
| Knee | 2 | EPS | – | – | – | 1 |
| Anterior tibial | – | – | 1 | – | ||
| Wrist ganglion | 1 | Dorsal cubital | – | 1 | – | – |
| Radial | – | 1 | – | – | ||
| Shoulder | 1 | Axillary | – | – | 1 | – |
| Pes cavus | 1 | Medial plantar | – | 1 | – | – |
| Biceps tendon at the elbow | 1 | Radial | – | – | 1 | – |
| Dorsal tendon wrist | 1 | Radial | – | – | 1 | – |
| Knee tumour | 1 | EPS | – | 1 | – | – |
| Cervical spine | 1 | Cervical root | – | 1 | – | – |
| Total | 41 | |||||
CTS: carpal tunnel syndrome; EPS: external popliteal sciatic nerve.
In cases of lumbosacral and cervical spinal surgery, both trauma and non-trauma, arthrodeses were performed. In the spinal surgery sites, the lesions identified were radiculopathies directly related to the level operated. The nerve structures with the highest number of injuries were the lumbosacral roots with a total of 12 cases (one case of L4 injury, seven cases of L5 injury and four cases of S1 injury), in the cervical site the roots injured were C5 in one case and C7 in one case.
Regarding the trauma injuries, the fractures located in the hip did not affect the pelvis or acetabulum, they were subcapital or femoral neck fractures and the surgery performed was arthroplasty with total or partial prosthesis implantation. In the remaining trauma cases, the surgery performed was fracture fixation by osteosynthesis.
Orthopaedic surgery for ganglion resection, tumours, pes cavus and tendon repair were included in the group of non-trauma cases. Cases of carpal tunnel syndrome (CTS), Dupuytren's contracture and Madelung's deformity were included in hand/wrist surgery for non-trauma reasons. At the hip, knee and shoulder level, arthroplasties were performed for degenerative processes. At the ankle level, three cases were included in which, although the injury was initially trauma, the surgery related to the injury was arthrodesis to repair old injuries that had occurred years earlier.
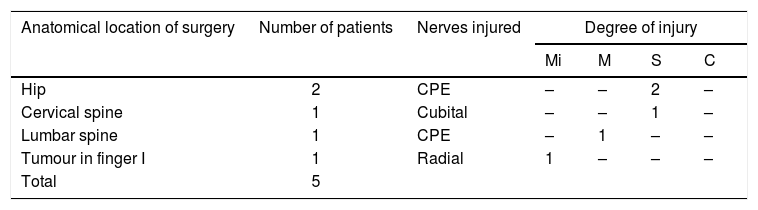
In the cases classified as caused by positioning, of the total five, in the three where an injury to the external popliteal sciatic nerve (EPS) was found, two underwent surgery at hip level, one case with a trauma and one for a non-trauma reason, in both cases a total arthroplasty was performed in a lateral decubitus surgical position and the injured nerve was in the operated limb, the third case occurred after surgery on the lumbosacral spine of non-trauma cause and using prone surgical positioning. The radial nerve injury occurred after surgery for a tumour in the first finger of the hand of the same limb; this case was performed under plexus anaesthesia and the nerve injury was located at the distal level of the plexus. The ulnar injury occurred after surgery at cervical spine level due to a trauma injury using the prone position during surgery. The cases of positioning injury were extracted from the total and are shown in Table 4.
Cases identified as postural injury are extracted from the total and showing, in descending order of cases, the location of surgery, number of patients and nerve structures injured, specifying their corresponding degree of axonotmesis (Mi – mild, M – moderate, S – severe, C – complete).
| Anatomical location of surgery | Number of patients | Nerves injured | Degree of injury | |||
|---|---|---|---|---|---|---|
| Mi | M | S | C | |||
| Hip | 2 | CPE | – | – | 2 | – |
| Cervical spine | 1 | Cubital | – | – | 1 | – |
| Lumbar spine | 1 | CPE | – | 1 | – | – |
| Tumour in finger I | 1 | Radial | 1 | – | – | – |
| Total | 5 | |||||
EPS: external popliteal sciatic nerve.
Of the 65 patients included in the study, a combined injury to two nerves was identified in six, giving a total of 71 injured nerve structures. The combined nerve injury was superficial saphenous-peroneal in two patients, both cases after surgery at ankle level, one case caused by trauma and one with a non-trauma cause. The remaining combined injuries occurred in four different patients and the following nerves were affected: femoral-obturator in hip surgery due to a trauma cause, anterior sural-tibial in surgery at ankle level due to a non-trauma cause, dorsal radial-ulnar in ganglion resection at wrist level and radial-ulnar in traumatic surgery at elbow level.
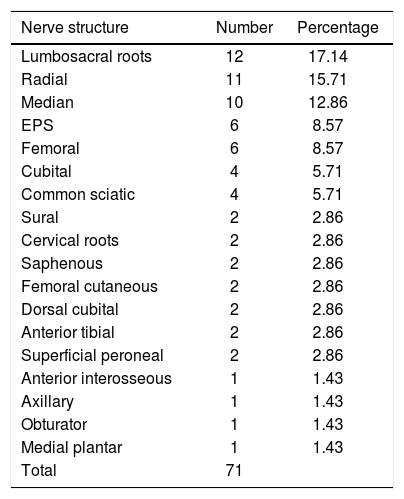
Table 5 shows the number of each nerve structure injured and its percentage with respect to the total.
Number of each nerve structure injured and its percentage of the total.
| Nerve structure | Number | Percentage |
|---|---|---|
| Lumbosacral roots | 12 | 17.14 |
| Radial | 11 | 15.71 |
| Median | 10 | 12.86 |
| EPS | 6 | 8.57 |
| Femoral | 6 | 8.57 |
| Cubital | 4 | 5.71 |
| Common sciatic | 4 | 5.71 |
| Sural | 2 | 2.86 |
| Cervical roots | 2 | 2.86 |
| Saphenous | 2 | 2.86 |
| Femoral cutaneous | 2 | 2.86 |
| Dorsal cubital | 2 | 2.86 |
| Anterior tibial | 2 | 2.86 |
| Superficial peroneal | 2 | 2.86 |
| Anterior interosseous | 1 | 1.43 |
| Axillary | 1 | 1.43 |
| Obturator | 1 | 1.43 |
| Medial plantar | 1 | 1.43 |
| Total | 71 |
EPS: external popliteal sciatic nerve.
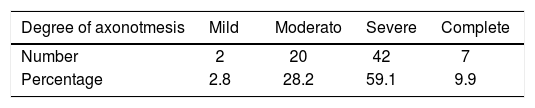
In terms of degree of injury identified by EMG, most of the injuries, 69% of the total, were complete and severe axonotmesis, only 2.8% of the total injuries were classified as mild. Table 6 shows the total number of injuries according to degree of injury.
DiscussionThere are few published studies on iatrogenic injuries secondary to TOS procedures. These studies are retrospective with very diverse methodology primarily focussing on a specific surgical technique. The incidence of iatrogenesis varies and is low; in the series reviewed with the largest number of cases, percentages range from 0% to 3.5%, with the cervical spine and hip being the sites most affected.10–13 The published series that have a clearly higher incidence than the rest concern surgery to very specific locations: biceps tendon fixation in which an iatrogenic incidence of 11% is described due to musculocutaneous injury and surgical reduction of distal radius fractures with an incidence of up to 20% in superficial radial nerve injuries.3 In fact, up to 21.6% of musculocutaneous injuries are reported to be of iatrogenic origin.14 A series from a neurosurgical repair unit indicates that 17.4% of injuries treated were of iatrogenic aetiology and 19% of these were secondary to TOS, with osteosynthesis, osteotomies and arthrodesis being the procedures with the highest percentage risk.15 Iatrogenesis is also described as the most frequent cause of sciatic injury.16 Other studies relate the total number of iatrogenic injuries to the total number of traumatic injuries to nerves and roots, resulting in a percentage of about 11%.17,18 A review of iatrogenic nerve injuries, including surgical and non-surgical procedures, shows that TOS leads in terms of percentage of injuries with 33.5% of the total, and spinal surgery involves the highest risk of injury with an incidence of 1.5%. Total hip arthroplasty comes second with an estimated incidence of 0.3%.19 A study conducted in the New York area puts the percentage of iatrogenic injuries associated with TOS at 4.1%, including all types of injuries, not only neurogenic.20 A study conducted in Catalonia places TOS as the specialty with the most medico-legal claims.21 A review of court rulings issued in Spain against Traumatologists concluded that claims for neurovascular injuries were the second most common at 34% of the total, only surpassed by osteoarticular disorders, surgical error being the main reason for the claims.22
Regarding the higher incidence of iatrogenic injuries in TOS procedures compared to other surgical specialties, the published series agree that this would be due to the anatomy of the regions operated and the intimate relationship of the bone structures with the nerve structures.15,23 The cause of iatrogenic injury is unclear in up to 50% of cases and re-interventions double the incidence of iatrogenic injury.11
Various mechanisms of injury to nerve structures during surgery have been described, both directly in the surgical field and indirectly. Ninety-four percent of the injuries are secondary to direct mechanisms and the rest to indirect mechanisms.24 The following have been described as direct mechanisms: crushing, compression by cerclage wires, suturing, penetration by screws, removal of osteosynthesis material, elongation, cuts or thermal injuries by the electric scalpel, compression by haematomas and by bone cement hardening. Indirect injuries have been described as related to surgical positioning, catheter puncture and ischaemia cuffing. Nerve injuries are more likely in different circumstances: inadequate exposure of nerves in the surgical field, confusion with a tendon or vessel, unusual nerve tracts or if nerves or nerve roots are in intimate contact with ganglia or tumours.11,15,24–29
Experimental attempts have been made to detect the mechanism of injury to the sciatic nerve in hip operations, even predicting the traction required to injure the nerve.30 In a specific review on anaesthesia malpractice claims in TOS procedures excluding spinal surgery, 26% of the total were due to nerve injury, although the incidence in relation to the total number of surgical procedures is not specified.31
As we mention above, the results of the studies reviewed are diverse, but they point to a high incidence of iatrogenic nerve injuries in TOS procedures compared to other specialties, with particular incidence in spine and hip surgery. In our review we found a general incidence like the series reviewed. In terms of specific locations, we found that those with the highest number of nerve injuries are those of the greatest anatomical complexity: the spine and joints.
In our study, the lumbosacral roots were the nerve structure with the highest number of injuries. The spinal column is a very complex area anatomically, with a close relationship between the nerve roots and the bony structures. The second most frequently injured structure was the radial nerve, which was involved in various joint repair surgeries after a trauma injury (shoulder, elbow and humerus), tendon (biceps at the elbow, extensor tendon at the wrist), resection of ganglion in the wrist and from positioning after resection of tumour of the first finger of the same extremity, the locations with the highest number of injuries (more than half of the total) being the shoulder and humerus, precisely where the nerve is in greater contact with the structure operated. Regarding the median nerve, the third structure in terms of number of injuries, most cases (40%) occurred after CTS surgery, the rest after surgery due to trauma, with two cases at the elbow and another two at the radius, the remaining two for Dupuytren's contracture and for repair of scaphoid fracture, in all cases the nerve pathway is anatomically related to the surgical site. There are much fewer cases of other nerve injuries and anatomical locations. The percentage of double nerve injuries is relevant, up to 10% of the total, all following joint surgery (ankle, hip, wrist, and elbow). In the group of positioning injuries, the incidence is close to 8% of the total, the most affected nerve is the EPS in three cases out of five, probably linked to the superficial pathway of this nerve at the level of the fibular head and its high susceptibility to injury by pressure and stretching27; the radial and ulnar nerves also injured in this group are also susceptible to injury by external pressure due to their pathway.9
Most of the resulting iatrogenic injuries were severe or complete axonotmesis, probably corresponding to the mechanism of injury and the sensitivity of the nerve structures to ischaemia and the consequent difficulty in functional recovery.32 These results are in line with those obtained in the few publications that give the degree of injury.29
The greater number of iatrogenic injuries secondary to surgery for non-trauma causes compared to trauma causes would be due to the greater volume of surgery for non-trauma compared to trauma causes. In none of the cases reviewed was neurophysiological monitoring performed during the intervention.
Procedures have been suggested to reduce the incidence of iatrogenic injuries, such as the appropriate protocolisation of the various surgeries by implementing a Surgical Safety Checklist. More specifically with regard to nerve iatrogenesis, adequate anatomical knowledge of the nerve pathways and their variants is recommended, including labelling the pathways.21,23 In recent years, the indications for intraoperative neurophysiological monitoring have progressively increased, in tandem with the evolution of recording equipment. This technique includes various modalities: somatosensory evoked potentials, motor evoked potentials with transcranial stimulation, stimulation of peripheral roots and nerves and free EMG recording. These procedures allow continuous assessment of nerve structures during surgery, helping to flag up early warning signs and the possibility of reversing manoeuvres to prevent injuries.28,33–40
The main limitation of our study is that the EMG studies performed for suspected iatrogenic injuries and the cases extracted come from a wide variety of sources. This prevents us from establishing the specific incidence of iatrogenic injuries by anatomical location in the procedures reviewed. The high degree of injury found could be because injuries that only cause neurapraxia, with spontaneous recovery, or mild axonotmesis, with little functional impact, may not be referred for EMG study. This possible limitation could increase the percentage of iatrogenic injuries, but because there is no significant functional deficit, it would be of little importance as a surgical sequela. On the other hand, the diagnosis of injuries by EMG objectively determines the degree and topography of the lesion. Ideally studies with a similar aim to ours should be conducted prospectively. Given how complex they are to conduct due to the large number and technical variety of TOS interventions performed, no study of these characteristics with a significant number of patients has been published.
ConclusionsIatrogenic injuries to the peripheral nervous system are uncommon, but in our study, they led to neuropathies with a high degree of injury in most cases, with the consequent difficulty in subsequent functional recovery. The locations with the highest number of cases are those of the greatest anatomical complexity, in our review the joints and in particular the lumbosacral spine, hip and hand/wrist, as well as positioning injuries not directly related to the surgical field. Given the mechanism of injury, the strict application of surgical protocols, better anatomical knowledge of usual and unusual nerve pathways, together with intraoperative neurophysiological monitoring, could help to reduce the incidence of these injuries.
Level of evidenceLevel of evidence: IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Orenga Orenga JV, Parra Escorihuela S, Barreda Altaba I, Estarelles Marco MJ, Ghinea AD, Leal Galicia DE, et al. Lesiones iatrogénicas del sistema nervioso periférico en procedimientos de cirugía ortopédica y traumatología. Rev Esp Cir Ortop Traumatol. 2021;65:264–271.