The study objective was to assess the results of a thumb metacarpophalangeal joint (MCPJ) arthrodesis using intramedullary interlocking screws at 25°, XMCP ™ (Extremity Medical, Parsippany, NJ). Radiographs evaluated the angle of arthrodesis, time of fusion and fixation of the implant. Clinical and functional outcomes were assessed using the DASH questionnaire and the VAS scale. Any complications found during surgery or the follow-up period were noted. We studied 9 patients. The mean follow-up was 27.6 months. Patients showed clinical and radiological evidence of fusion in an average of 8 weeks, the angle of fusion was 25°. There were no complications and no implant had to be removed. The XMCP™ system provides a reliable method for MCPJ arthrodesis for several indications and can be used with other procedures in the complex hand.
El objetivo de estudio fue valorar el resultado de la artrodesis de la articulación metacarpofalángica del pulgar mediante el sistema de tornillos intramedulares de ángulo fijo a 25°, XMCP™ (Extremity Medical, Parsippany, NJ). En las radiografías se evaluó el ángulo de artrodesis, el tiempo de fusión ósea y fijación del implante. Los resultados clínicos y funcionales se evaluaron mediante el cuestionario DASH y la escala EVA. Se observó cualquier complicación encontrada durante la cirugía o el período de seguimiento. Se estudiaron 9 pacientes. El seguimiento medio fue de 27,6 meses. Los pacientes presentaron evidencia clínica y radiológica de fusión en un promedio de 8 semanas, y el ángulo de fusión promedio fue de 25°. No se presentaron complicaciones y no se ha tenido que retirar ningún implante. En conclusión, el sistema XMCP™ proporciona un método fiable para la artrodesis metacarpofalángica del pulgar para una variedad de indicaciones, y puede usarse junto con otros procedimientos en la mano compleja.
Instability of the thumb metacarpophalangeal joint (MPJ) is often associated with trapeziometacarpal arthrosis and rheumatoid arthritis, which are common indications for MPJ arthrodesis.1 In addition, chronic postraumatic instability with or without arthrosis and failed repairs of the collateral ligament are also indications for MPJ arthrodesis.2
Various arthrodesis techniques are described in the literature. These procedures can include Kirschner wires with or without tension band,3 and cannulated screws,4 among others.5 Optimal techniques for MPJ instability arthrodesis would offer sufficient fixation to enable early movement of the thumb, promote rapid fusion, and apply to all the indications for arthrodesis.2 The recommended fusion angle is typically between 10° and 32°; this recommendation is based on studies that evaluated MPJ joint motion during activities of daily living.1,6,7
The aim of this study was to assess the result of MPJ arthrodesis using intramedullary interlocking screws at a fixed angle of 25°, XMCP™ (Extremity Medical, Parsippany, NJ).
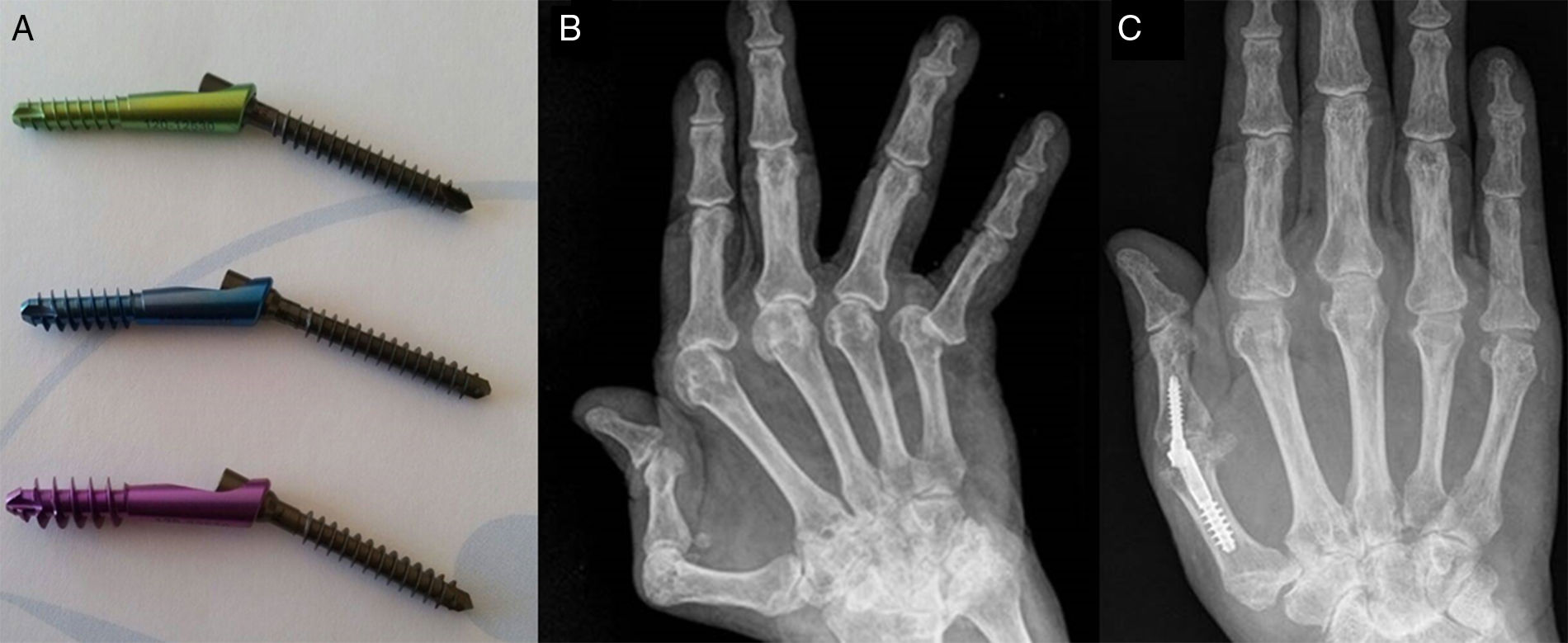
Material and methodA descriptive study was conducted of patients with a clinical and radiological diagnosis of thumb metacarpophalangeal joint arthrosis that underwent arthrodesis using the XMCP™ system (Fig. 1A) between 2012 and 2016.
(A) Details of the XMCP™ system. The 3 implant sizes: Xpost Small (green), Medium (blue), and Large (violet). All have a nominal angle of 25°. (B) Rheumatic hand with ulnar drift and MP instability of the 5 radii. (C) Result after MPJ arthrodesis using the XMCP™ system, release of extensor apparatus, correction of ulnar drift by radial transposition and tenodesis of the intrinsics, MP prosthesis of 4–5 fingers with silicone MCP (INTEGRA®); 21 months’ evolution.
The demographic data and follow-up time were recorded, as well as the indication for surgery and procedures associated with MPJ arthrodesis, and cases with a course of at least 6 months were selected.
Posteroanterior, lateral and oblique X-ray views were taken of the hand, focussing on the MPJ.
The patients were examined at one week, at 2 weeks to remove the sutures, at one month and at 3 months after surgery; then every 3 months over the first year and every 6 months thereafter. Radiographic follow-up of all the patients comprised posteroanterior and lateral projections of the hand and thumb during the first 3 months, at 6 months and at 1 year's follow-up. The time to union and the fusion angle of the MPJ were assessed. We considered union of arthrodesis when we observed bridges at both bone ends, the absence of pain at the focus, and few inflammatory signs. The final result was assessed 6 months after surgery. The clinical and functional status was assessed using the Disabilities of the Arm, Shoulder, and Hand-questionnaire (DASH)8 and the Visual Analogue Scale (VAS). We included the questions “are you satisfied with the surgery?” and “would you undergo the operation again?” to assess the patients’ level of satisfaction.
We used the Statistical Package for the Social Sciences (SPSS) version 21.0 for the data analysis. The qualitative variables were expressed in numbers and percentages. Mean and standard deviation were used for the quantitative variables. The pre and post-intervention quantitative results were compared using the Wilcoxon test.
Surgical techniqueWe performed the procedure using the technique described by Vanderzanden et al.2 The procedure was performed creating ischaemia of the limb using a pressure cuff placed at the level of the arm, with a variable time depending on the procedure, 45min for MPJ arthrodesis as a single procedure to 160min for more complex rheumatic hands, the cuff had to be removed in these cases after 90min and then replaced (Fig. 1B and C). At the end of the procedure, a simple bandage was applied for the isolated MPJ arthrodesis procedures, and a cast for 2 weeks for the more complex procedures that required immobilisation to stabilise the soft tissues.
Postoperative careWeekly dressings were applied until the sutures were removed. Mobilisation was started immediately after the simple thumb arthrodesis procedures, and gradually after the complex hand procedures. Grip and pinch strength exercises were started from the sixth week, depending on the complexity of the procedures.
ResultsNine patients were operated in our centre using the XMCP™ system between 2012 and 2016.
The sample comprised 7 women (77.7%) and 2 men (22.2%), with an average age of 85 years (range: 55–73). Seven right hands and 2 left hands were operated. The average follow-up was 27.6 months (range: 6–51).
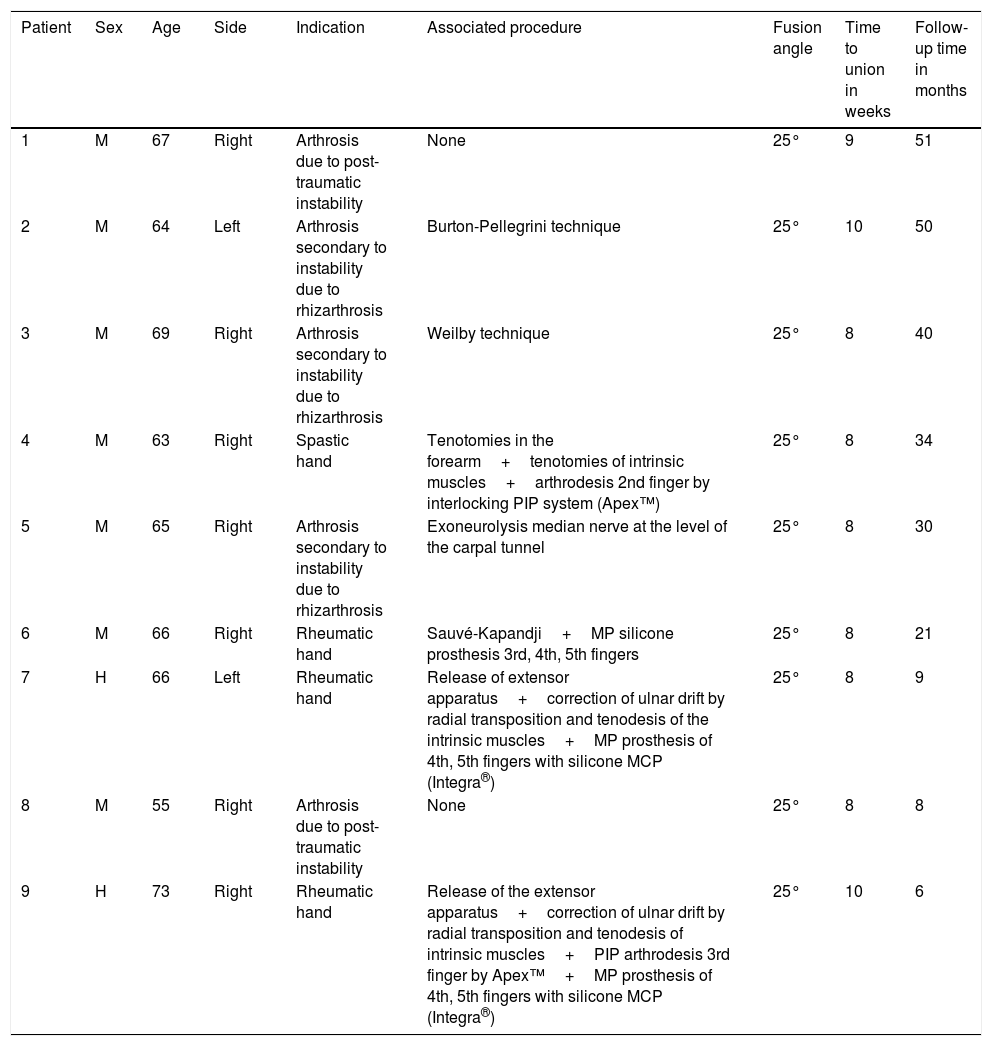
Table 1 shows the indications for arthrodesis and the associated procedures.
Demographic features, indications, associated surgical procedures and radiological results of MPJ arthrodesis using the XMCP™ system.
| Patient | Sex | Age | Side | Indication | Associated procedure | Fusion angle | Time to union in weeks | Follow-up time in months |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 67 | Right | Arthrosis due to post-traumatic instability | None | 25° | 9 | 51 |
| 2 | M | 64 | Left | Arthrosis secondary to instability due to rhizarthrosis | Burton-Pellegrini technique | 25° | 10 | 50 |
| 3 | M | 69 | Right | Arthrosis secondary to instability due to rhizarthrosis | Weilby technique | 25° | 8 | 40 |
| 4 | M | 63 | Right | Spastic hand | Tenotomies in the forearm+tenotomies of intrinsic muscles+arthrodesis 2nd finger by interlocking PIP system (Apex™) | 25° | 8 | 34 |
| 5 | M | 65 | Right | Arthrosis secondary to instability due to rhizarthrosis | Exoneurolysis median nerve at the level of the carpal tunnel | 25° | 8 | 30 |
| 6 | M | 66 | Right | Rheumatic hand | Sauvé-Kapandji+MP silicone prosthesis 3rd, 4th, 5th fingers | 25° | 8 | 21 |
| 7 | H | 66 | Left | Rheumatic hand | Release of extensor apparatus+correction of ulnar drift by radial transposition and tenodesis of the intrinsic muscles+MP prosthesis of 4th, 5th fingers with silicone MCP (Integra®) | 25° | 8 | 9 |
| 8 | M | 55 | Right | Arthrosis due to post-traumatic instability | None | 25° | 8 | 8 |
| 9 | H | 73 | Right | Rheumatic hand | Release of the extensor apparatus+correction of ulnar drift by radial transposition and tenodesis of intrinsic muscles+PIP arthrodesis 3rd finger by Apex™+MP prosthesis of 4th, 5th fingers with silicone MCP (Integra®) | 25° | 10 | 6 |
The patients are organised according to follow-up time.
M: male; PIP: proximal interphalangeal; F: female; MP: metacarpophalangeal.
One hundred percent union of arthrodesis was achieved, in a mean 8.5 (±1) weeks and a 25° fusion angle, which was the standard for the device (Table 1).
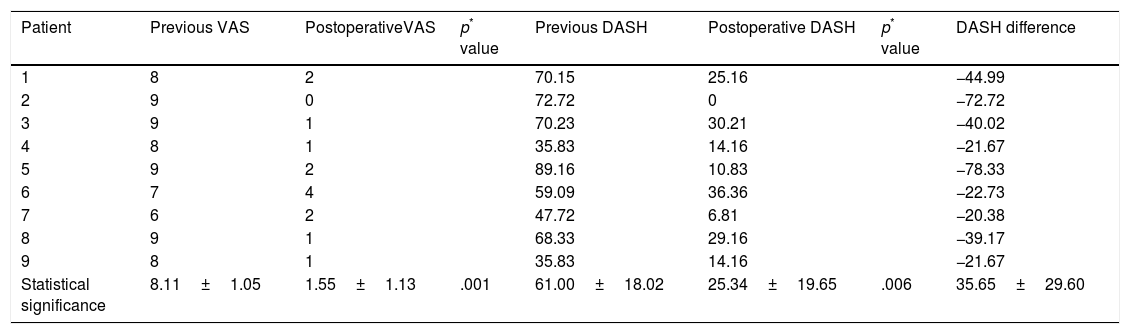
The pain levels of all the patients calculated by the VAS significantly reduced. A favourable result was achieved when the functionality of the operated limb was assessed using the DASH questionnaire. When we evaluated clinical relevance based on the DASH score, 100% of the patients’ pain had reduced by at least 10 points compared to the previous score.9 Although this result is difficult to interpret because most of our patients did not undergo a single isolated procedure (Table 2).
Pain and functional results.
| Patient | Previous VAS | PostoperativeVAS | p* value | Previous DASH | Postoperative DASH | p* value | DASH difference |
|---|---|---|---|---|---|---|---|
| 1 | 8 | 2 | 70.15 | 25.16 | −44.99 | ||
| 2 | 9 | 0 | 72.72 | 0 | −72.72 | ||
| 3 | 9 | 1 | 70.23 | 30.21 | −40.02 | ||
| 4 | 8 | 1 | 35.83 | 14.16 | −21.67 | ||
| 5 | 9 | 2 | 89.16 | 10.83 | −78.33 | ||
| 6 | 7 | 4 | 59.09 | 36.36 | −22.73 | ||
| 7 | 6 | 2 | 47.72 | 6.81 | −20.38 | ||
| 8 | 9 | 1 | 68.33 | 29.16 | −39.17 | ||
| 9 | 8 | 1 | 35.83 | 14.16 | −21.67 | ||
| Statistical significance | 8.11±1.05 | 1.55±1.13 | .001 | 61.00±18.02 | 25.34±19.65 | .006 | 35.65±29.60 |
DASH: Disabilities of Arm, Shoulder and Hand Spanish version; VAS: Visual Analogue Scale.
Eight of the operated patients were satisfied with the surgery and would repeat the same procedure. One of them was not satisfied with the result and would not be operated again. This patient had a spastic hand after a cerebrovascular accident, and gained little functionality in the operated limb after the surgery.
There were no complications associated with the MPJ arthrodesis, and no case of migration or rupture of the implant, and no peri-implant irritation of soft tissues was recorded.
DiscussionThere is a wide range of MPJ arthrodesis techniques. Fixation with Kirschner wires is the traditional technique; however, problems with fusion failure, infection along the course of the wire, and soft tissue irritation commonly require removal of the implant.2
Herbert screws are a useful alternative for MPJ arthrodesis.10 Schmidt et al.,4 in a series of 26 patients with a follow-up of 32 months, reported stable MPJ fusion without pain in 25 patients, and no implants had to be removed. The average fusion angle was 18° (range 0–38°), and the mean time to fusion was 10 weeks. Postoperatively the patients were kept immobilised in plaster for 2 weeks; they did not specify the protocol for complex hands.
As far as we are aware, there is only one series of 17 patients for whom an intramedullary interlocking device was used for MPJ arthrodesis. This study was by Vanderzanden et al.,2 who reported 100% union in an average of 7.9 weeks after the operation, with a fusion angle of 24.4° and a mean follow-up of 4.9 months. They reported no complications in relation to the implant. The patients with simple MPJ arthrodesis were allowed immediate postoperative mobility, and the complex hands were immobilised in plaster for 2 weeks until stabilisation of the soft tissues.
We achieved 100% arthrodesis union in our series, in a mean 8.5 weeks, and there were no complications, and no implant had to be removed. The average fusion angle on the lateral radiograph was 25°. In order to determine the most functional position for MPJ arthrodesis for each patient, the surgeon must assess the compromised joint preoperatively in the context of their disease, determine the initial cause of the joint disease and evaluate the condition of the surrounding joints.11 In the thumb, the importance of the fixation angle is based on maintaining its opposition ability. In very wide angles the thumb's ability to reach the 4th and 5th finger is very limited, and MPJ angles that are too flexed can limit pinch; this is particularly important when the carpometacarpal joint is affected.1 Jørgensen et al.,12 had to remove 7.7% of the implants in their series due to suboptimal positioning of the MPJ joint.
The weakness of our study is the sample size, which is relatively small, and the scanty follow-up, therefore we cannot discount longer term studies with larger sample sizes detecting complications with these types of implants, such as the development of pantrapezial arthrosis in patients where this joint was respected prior to the surgery or potential bone defects that might remain after removal of these implants, if this were necessary. The strength of our study is that because this is a single-centre study the internal validity is high, due to the homogeneity of the treatment protocol and of the test evaluation.
ConclusionThe XMCP™ system provides a reliable method for MPJ arthrodesis for a variety of indications. Inserting the device is not technically demanding, even when performed together with other procedures to the thumb and on a complex hand. Bone fusion is fast and with a consistent fixation angle.
Level of evidenceLevel IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Please cite this article as: Novoa-Parra CN, Montaner-Alonso D, Morales-Rodríguez J. Artrodesis de la articulación metacarpofalángica del pulgar con tornillos intramedulares entrelazados de ángulo fijo XMCP™. Rev Esp Cir Ortop Traumatol. 2018;62:387–391.