Postero-medial deformity (DMPT), unlike other congenital forms that affect the tibia, presents a good evolution spontaneously correcting the important misalignments that present at birth based on the classic orthopaedic laws of Wolff and Hueter-Volkmann, leaving slight residual angulations and variable limb length discrepancy.
Material and methodsAuthors carry out a retrospective review of cases diagnosed with DPMT, the evolution of the tibial angulation and the discrepancy in the length of fourteen patients (11 males and 3 females) followed and treated between the years 2003 and 2018. Seven of these were treated by callus distraction. We have considered: PA and lateral of the tibia and stand-up entire limbs X-ray during age growth, along with the clinical records of the patients.
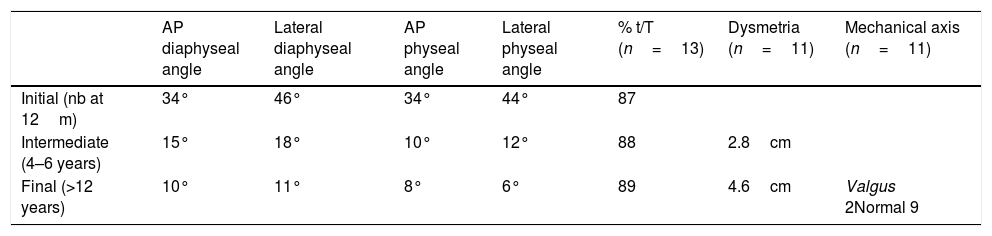
ResultsThe medial diaphyseal radiological deformity of the newborn or neonatal period was 34° and the final 10°. The posterior deformity evolved from 46° to a final angulation of 11°. The physeal angulation in the initial AP projection was 34° and the end view was 8° and in the lateral projection from 44 to 6°. The mechanical axis of the limb was correcting towards a neutral axis in relation to the aforementioned physeal and diaphyseal correction in all cases except two. In five of the cases, although the mechanical axis was normal-aligned, at the tibial level it ran eccentrically and externally to the tibial cortex. The length relationship between the short tibia and the healthy tibia maintains a constant proportion throughout the growth of 89%, that is, the inhibition of growth is 11%. We observe that 80% of the discrepancy is found in the tibia and that the remaining 20% was exposed from the height of the tarsus. Two patients presented a traumatic and accidental diaphyseal fracture of the tibia. The difference in the length of the tibia was compensated to seven patients by callus distraction of 5.4cm using the callotasis method with a Healing Index of 34.5days/cm.
ConclusionsDPMT improves substantially during the first years of life. Joint alignment of the knee and ankle is achieved before the correction of diaphyseal deformity. The tibia length discrepancy increases with the growth of the child since there is an 11% growth inhibition that will cause a skeletal maturity discrepancy between 4–7cm. Callus distraction before skeletal maturity is the method chosen to compensate this discrepancy.
La deformidad postero-medial (DPMT), a diferencia de otras formas congénitas que afectan a la tibia, presenta una buena evolución corrigiendo de forma espontánea las importantes desalineaciones que presentan al nacimiento en base a las clásicas leyes ortopédicas de Wolff y Hueter-Volkmann dejando unas angulaciones residuales leves y una dismetría variable.
Material y métodosLos autores realizan una revisión retrospectiva de casos diagnosticados de DPMT, de la evolución de la angulación tibial y de la discrepancia de la longitud de 14 pacientes (11 varones y 3 mujeres) seguidos y tratados entre los años 2003 al 2018 y a los que a 7 se les realizó una elongación ósea. Se han valorado los estudios efectuados mediante radiografía simple en 2 proyecciones y telerradiografía de mensuración de miembros en bipedestación a lo largo del crecimiento, así como las historias clínicas.
ResultadosLa deformidad radiológica diafisaria medial de recién nacido o periodo neonatal fue de 34° y la final de 10°. La deformidad posterior evolucionó de 46° hasta una angulación final de 11°. La angulación fisaria en la proyección AP inicial fue de 34° y final de 8° y en la proyección lateral de 44 a 6°. El eje mecánico de la extremidad también fue corrigiéndose hacia un eje neutro con relación a la corrección fisaria y diafisaria antes mencionadas en todos los casos excepto en 2. En 5 de los casos, aunque el eje mecánico se encontraba normo-alineado, a nivel tibial discurría de forma excéntrica y externo al córtex tibial. La relación de longitud entre la tibia corta y la tibia sana mantiene una proporción constante a lo largo del crecimiento del 89%, es decir, la inhibición de crecimiento es de un 11%. Observamos que el 80% de la discrepancia se halla en la tibia, y que el 20% restante era a expensas de la altura del tarso. Dos pacientes presentaron fractura diafisaria de tibia por causa traumática y casual. A 7 pacientes les fue compensada la diferencia de longitud de la tibia mediante una elongación ósea media de 5.4cm empleando la técnica de callotasis con un índice de curación de 34,5 días/cm.
ConclusionesLa DPMT mejora sustancialmente durante los primeros años de la vida. La alineación articular de rodilla y tobillo se consiguen antes que la corrección de deformidad diafisaria. La discrepancia de longitud de las tibias va aumentando con el crecimiento del niño ya que existe un 11% de inhibición del crecimiento que originará una discrepancia a la madurez esquelética entre 4-7cm. La elongación ósea progresiva antes de la madurez esquelética es el método de elección para compensar esta discrepancia.
Posteromedial Tibial Bowing (PMTB) is a rare congenital condition of unknown exact incidence. Few papers have been published in the medical literature with a small number of cases. Unlike the antero-medial deformity associated with pseudoarthrosis of the tibia or fibular hemimelia, PMTB was considered a benign condition due to its tendency to spontaneous correction, angular correction of both the tibia and the mechanical axis of the limb following the laws of Wolff and Hueter-Volkmann.1,2
The aetiology of this condition is unknown, although it has been related to placental anomalies,3 rupture of the amnion, amniotic bands, intrauterine fractures, etc., and these processes may lead to abnormal ossification. It usually presents unilaterally, and it can be diagnosed prenatally. It is commonly mistaken for club foot because of the significant tibial bowing presented by newborns at birth.
Despite the condition's usual tendency to angular correction, it cannot be said that it resolves fully. In fact, the most clinically relevant sequela is limb length discrepancy, which ranges from 3cm to 7cm when patients reach skeletal maturity.4,5
The aim of this study was to review the cases that have been followed up and treated in our unit, observing the behaviour of their postero-medial bowing, and the progression of dysmetria and its treatment by progressive bone elongation.
Material and methodsWe conducted a retrospective review of cases diagnosed with PMTB, and of the progression of tibial angulation and lower limb length discrepancy in 14 patients (11 males and 3 females) followed up and treated between 2003 and 2018. Their radiographic studies were evaluated, standing plain X-ray and teleradiography of the limbs, and medical records. One patient was excluded from the study as we could not obtain their initial studies.
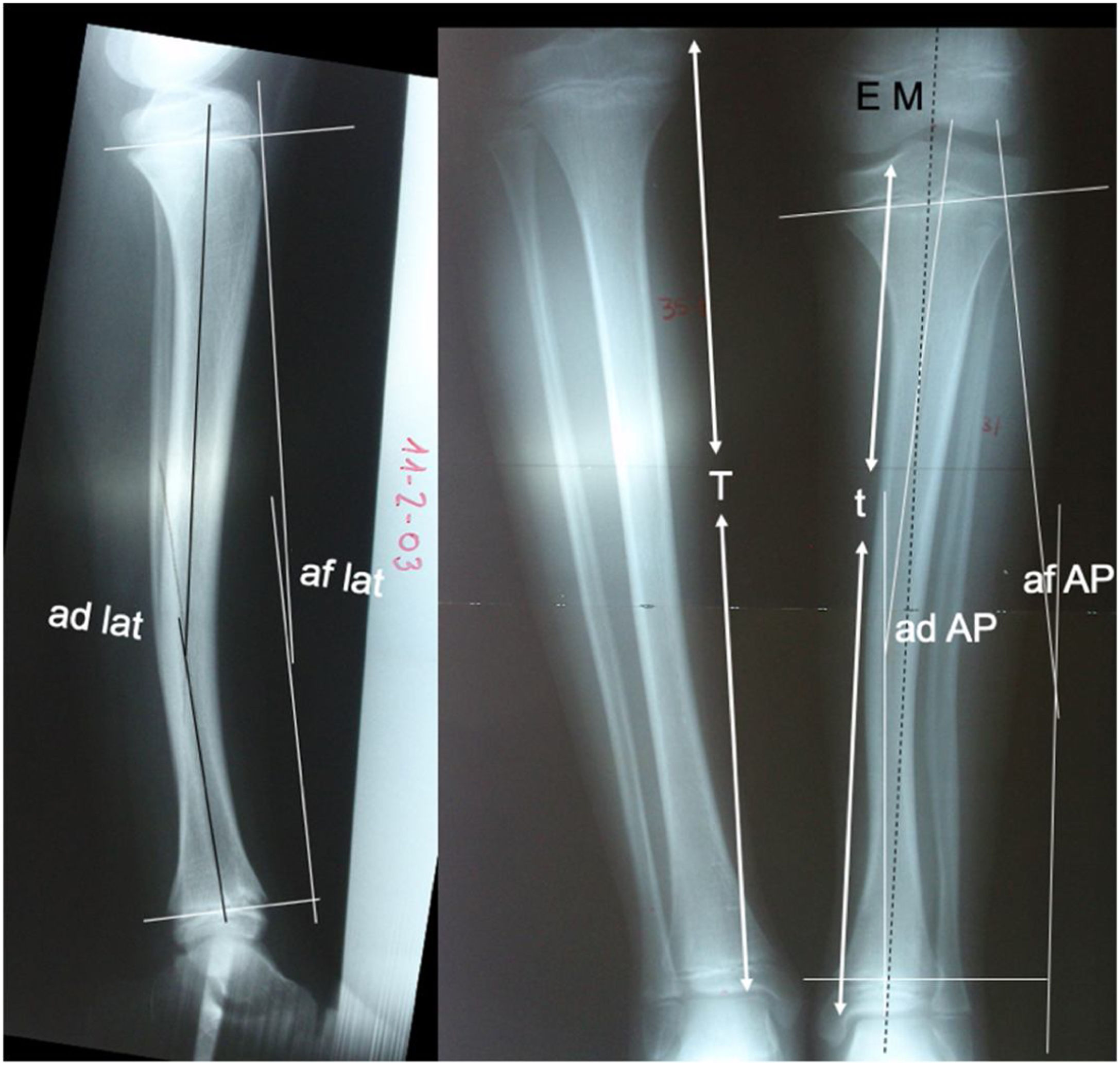
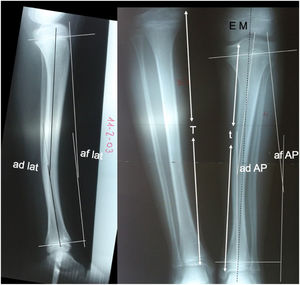
The radiological data of the 14 cases studied were recorded: (1) Diaphyseal angulation as angular bowing in the anteroposterior and lateral planes of the affected tibia. (2) Physeal angulation, measured as the angular ratio of the proximal physis to the distal physis in anteroposterior and lateral projections and compared to the healthy contralateral side. These measurements were taken at birth or in the first months of life, at 5 and at 12 years of age. The progression of growth inhibition percentage of the affected tibia (t) with respect to the healthy tibia (T) was also assessed. Limb length discrepancy was assessed by measurement overall and by anatomical segments (femurs, tibia, and tarsus, observing the difference in height of the tibiotalar joint space) using teleradiography in an anteroposterior projection. This same radiological study was used to view the progression of the mechanical axis of the affected limb, obtaining the centre of the femoral head and the centre of the talus as reference points, observing the medialisation or lateralisation of the axis as it passes through the knee and its course through the tibial diaphysis (Fig. 1).
da AP: tibial diaphyseal angle in anteroposterior projection; da lat: tibial diaphyseal angle in lateral projection; pa AP: physeal angle in anteroposterior projection; pa lat: physeal angle in lateral projection; MS: mechanical axis of the limb; T: length of the healthy tibia; t: length of the PMTB.
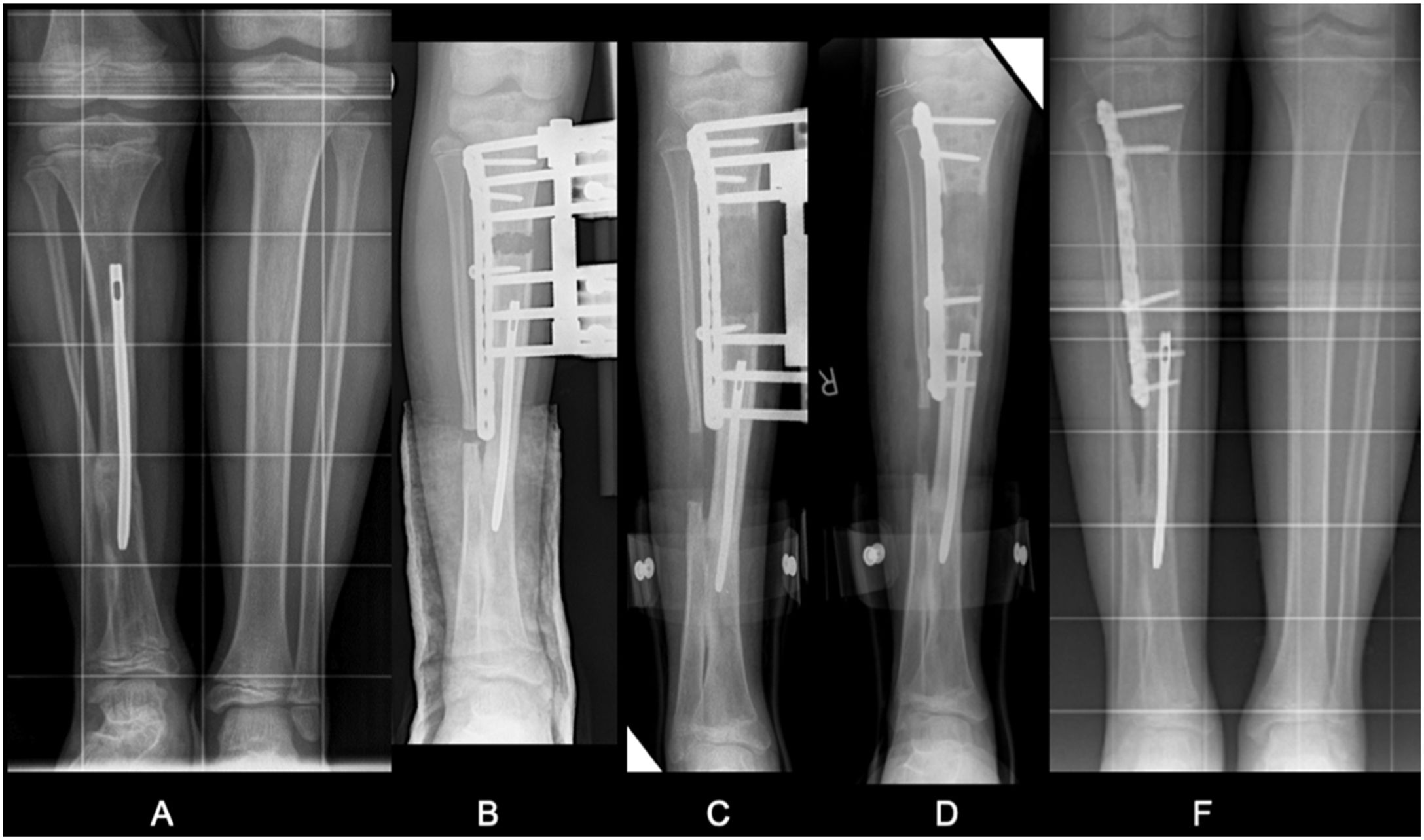
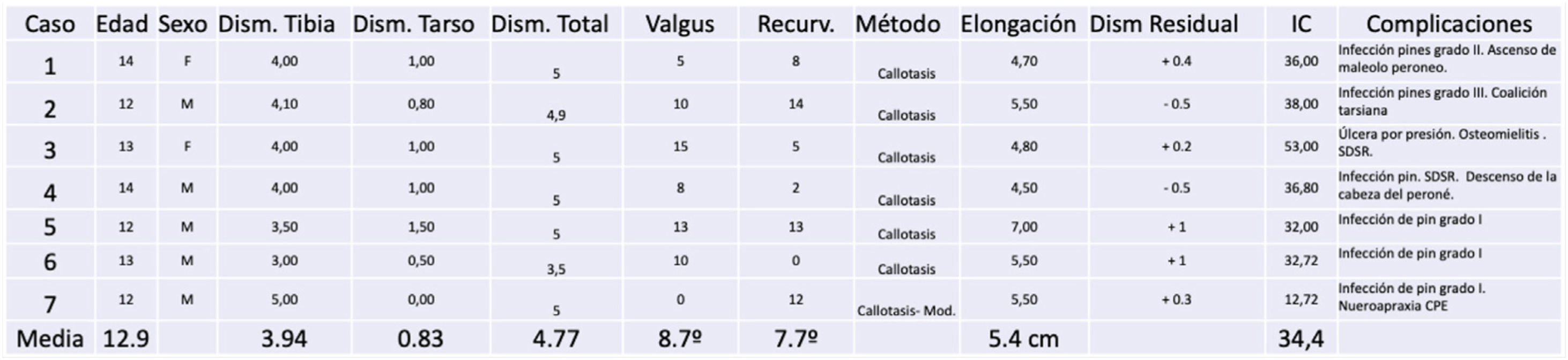
We also undertook a retrospective review of the 7 cases that required surgical treatment to correct the discrepancy by callotasis and angular correction of residual deformity by external fixation. The tibial discrepancy, the lengthening performed and the healing rate of the procedure are quantified in centimetres, as well as the duration of bone lengthening, from fixator placement to fixator removal, divided by the number of centimetres achieved, and the complications according to Paley.6 One of the cases was treated using a modification of the callotasis technique which, in addition to placing the external fixator on the anterointernal aspect of the tibia, consists of inserting a previously slotted AO plate in the submuscular plane and extraperiosteally on the external aspect of the tibia. This plate is locked proximally, and a guide screw is placed in the slot. After achieving the planned elongation, in a second stage the plate is locked distally and the guide screw in the slot is tightened, after which the external fixator is removed. This allows the external fixation time to be reduced.
ResultsThe left limb was affected in 9 cases and the right in 5 cases. The mean follow-up of our patients was 12.8 years (r: 3–20).
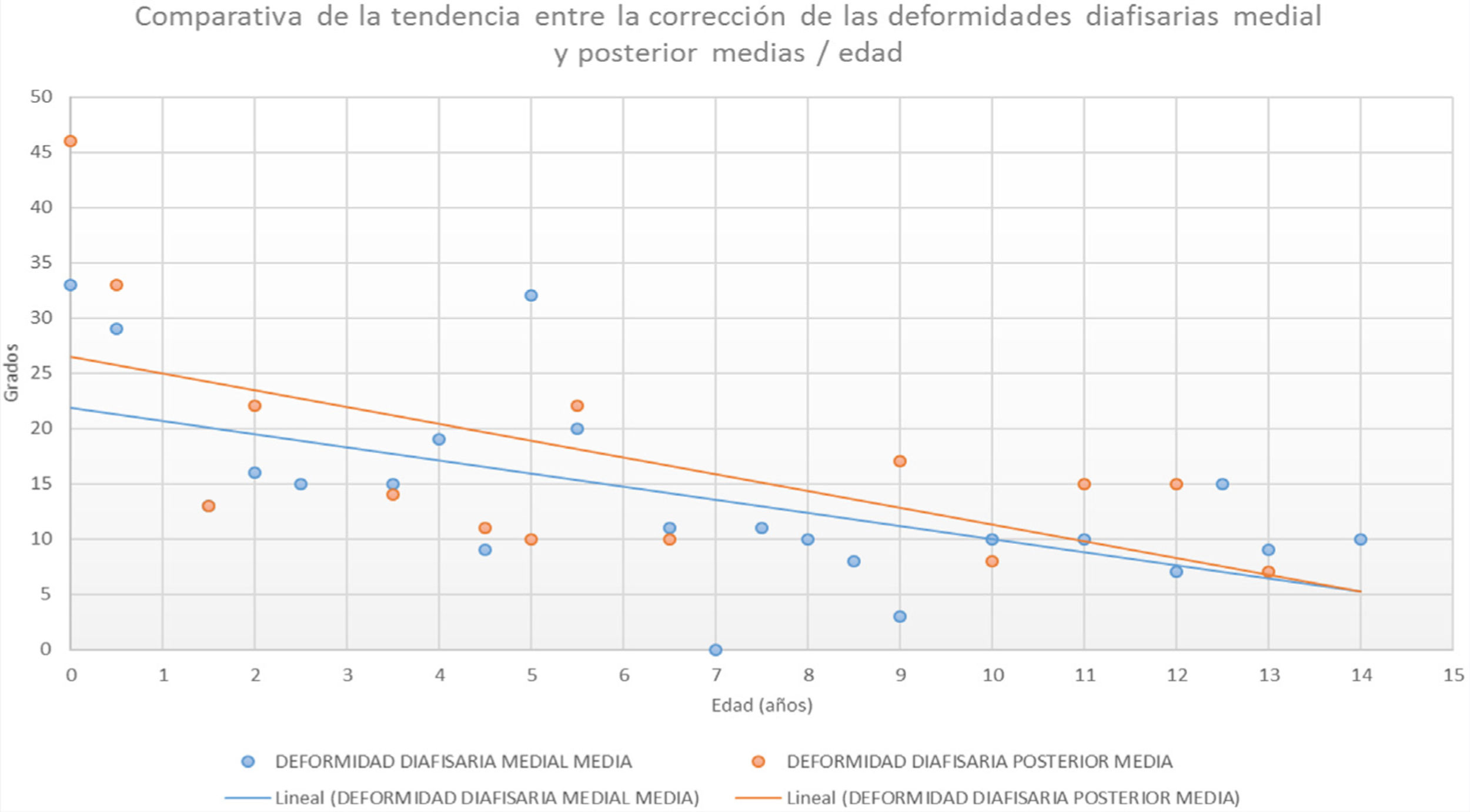
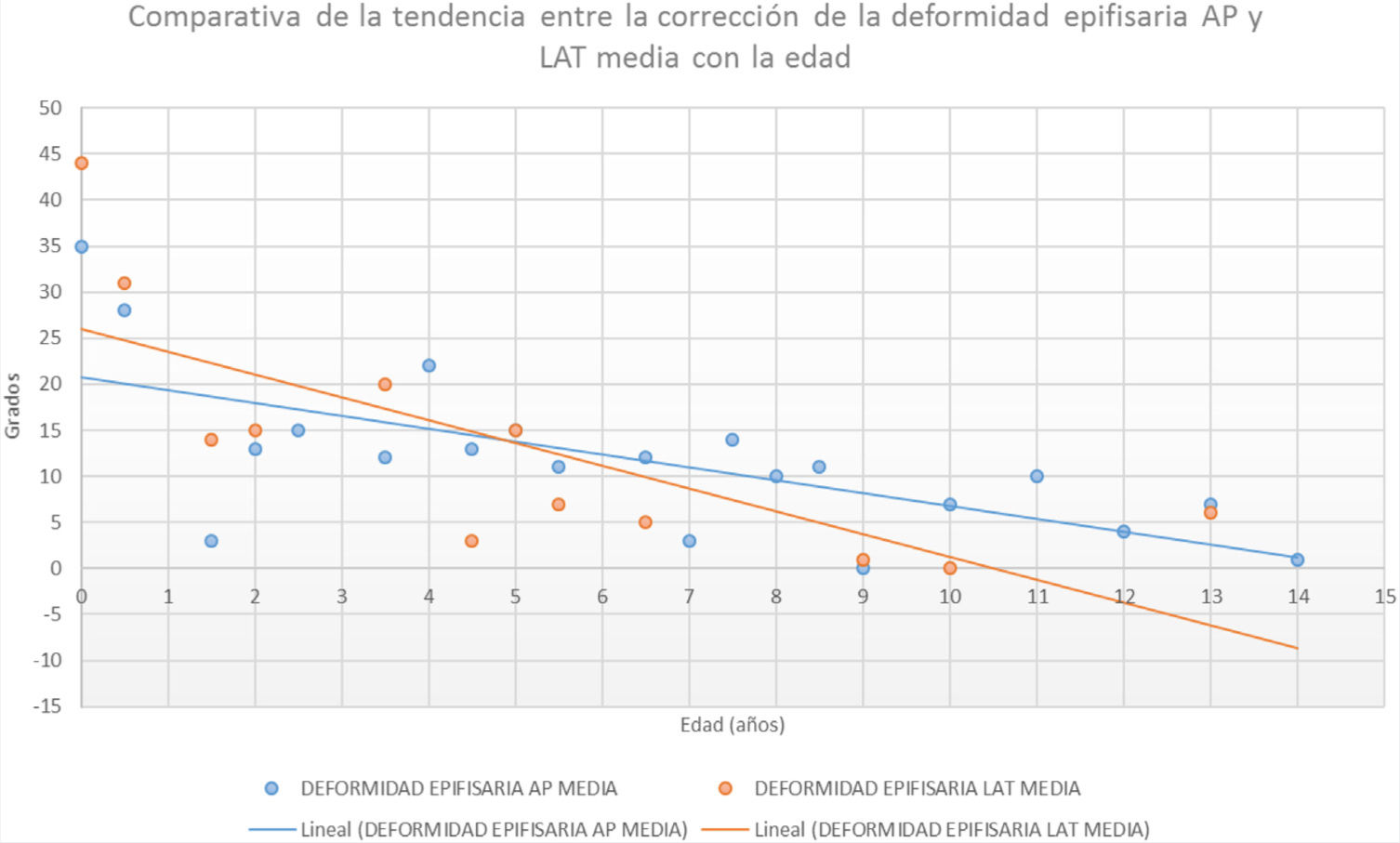
The initial medial diaphyseal bowing in the newborn or neonatal period was 34° (r: 15°–50°). The initial posterior deformity 46° (r: 40°–50°). Tables 1 and 2 show progression during growth quantitatively and graphically. The mean final medial tibial deformity was 10° (r: 0°–32°). The mean final posterior deformity at the last measurement taken in these patients was 11° (r: 5°–22°). The physeal angulation (Tables 1 and 3) in the initial AP projection was 34° (r: 26°–50°) and final physeal angulation was 8° (r: 0°–30°). In the lateral projection the initial physeal angulation of the deformity was 44° (r: 35°–60°) and the final angulation was 6° (r: 0°–15°).
Initial radiological progression of tibial diaphyseal and physeal angulations. Percentage ratio of PMTB length to healthy tibia (t/T), discrepancy and mechanical axis of the limb.
| AP diaphyseal angle | Lateral diaphyseal angle | AP physeal angle | Lateral physeal angle | % t/T (n=13) | Dysmetria (n=11) | Mechanical axis (n=11) | |
|---|---|---|---|---|---|---|---|
| Initial (nb at 12m) | 34° | 46° | 34° | 44° | 87 | ||
| Intermediate (4–6 years) | 15° | 18° | 10° | 12° | 88 | 2.8cm | |
| Final (>12 years) | 10° | 11° | 8° | 6° | 89 | 4.6cm | Valgus 2Normal 9 |
AP: anteroposterior; nb: newborn; PMTB: posteromedial tibial bowing; t/T: healthy tibia.
The mechanical or load-bearing axis in the affected limbs corrected towards a neutral axis in relation to the above-mentioned physeal-articular and diaphyseal correction. The axis in all but two cases was neutral at 12 years of age. We observed that, in 5 of the cases, although the mechanical axis was normo-aligned, at the tibial level it ran eccentrically, external to the tibial cortex. This finding occurs when a correction is made at the physeal level rather than at the diaphyseal level.
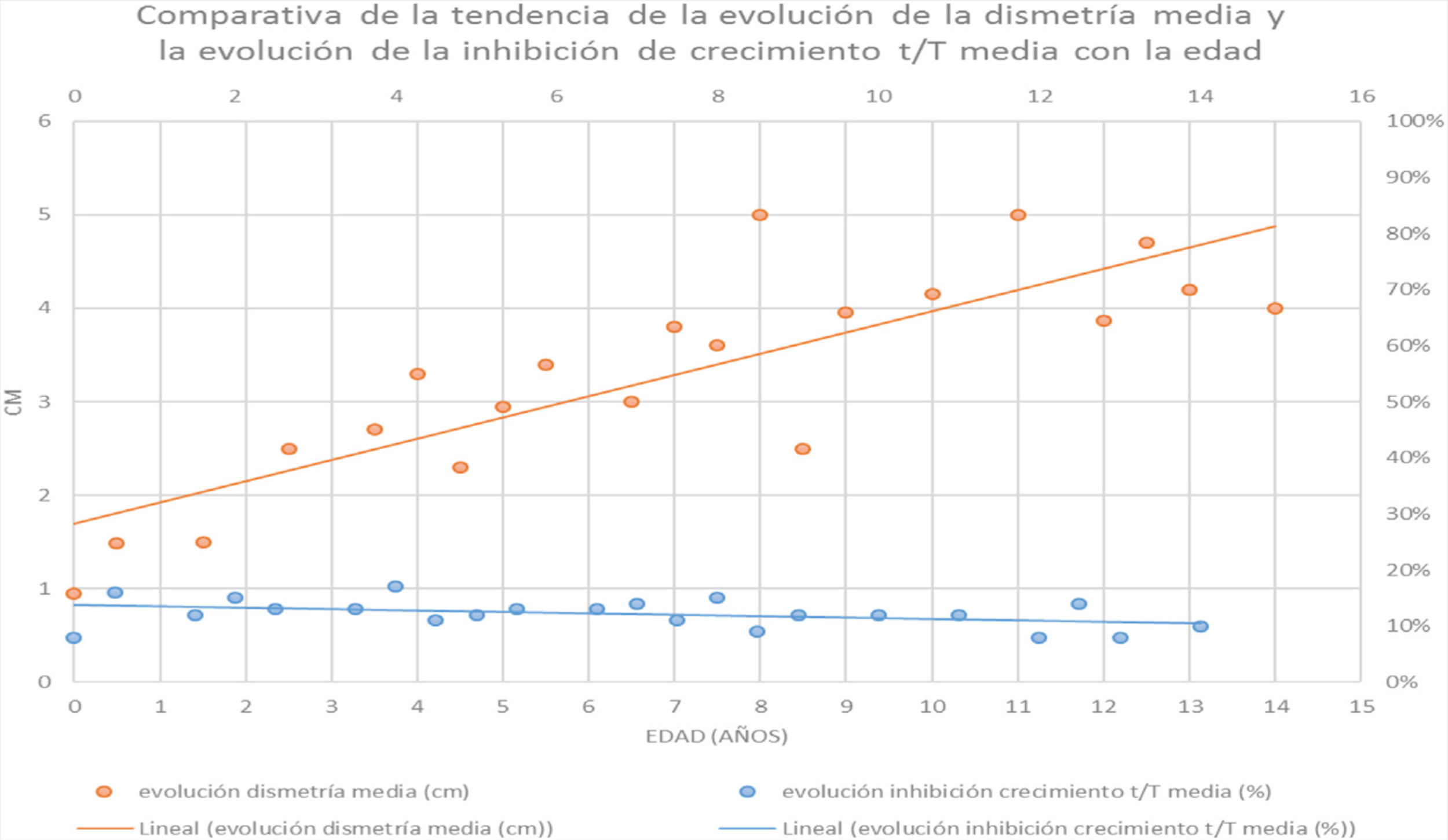
In terms of growth inhibition (1−t/T), this ratio maintains a constant proportion throughout the life of these patients. The affected tibia was a mean 89% (r: 85–91%) of the healthy contralateral tibia, i.e., there is growth inhibition of 11% (Tables 1 and 4).
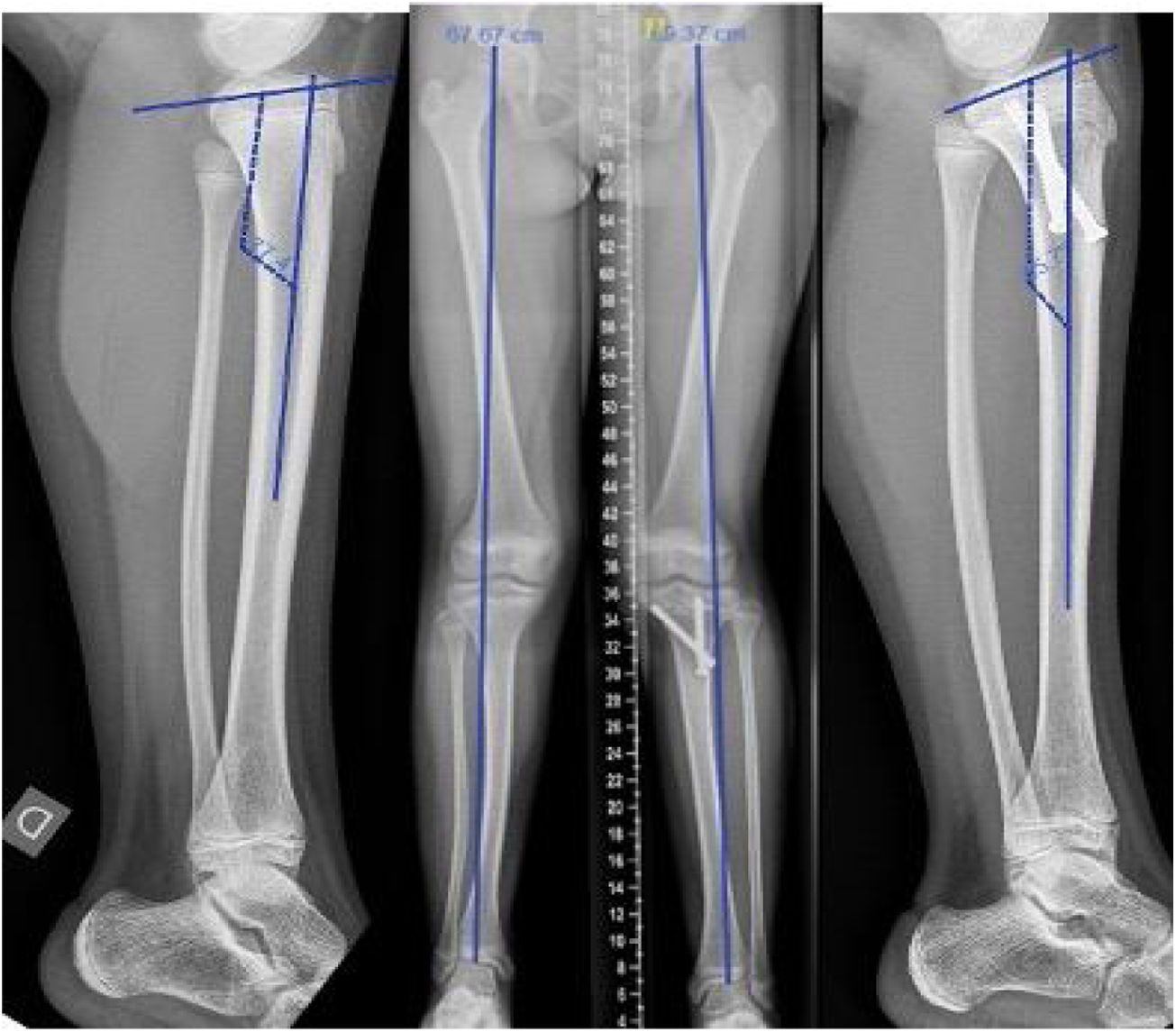
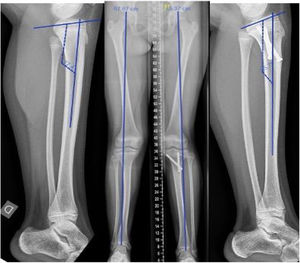
The mean age of the 7 patients with dysmetria at the time of lengthening (Table 5) was 12.6 years (r: 11–14 years). The mean discrepancy prior to bone lengthening was 4.6cm (r: 4–5.5cm). We observed that 80% of the discrepancy was in the tibia and the remaining 20% was at the expense of tarsal height.9cm (r: 0–1.5cm). Using the callotasis technique (Fig. 1), the mean lengthening achieved was 5.4cm (r: 4.5–7cm) and the final residual discrepancy .6cm (−.5 to +1cm). Of the remaining 7 patients, two are still under follow-up because they are under 12 years of age, 3 are on the waiting list for bone elongation at the time of this study, one patient was treated for the discrepancy at the age of 15 years in another health centre and one girl underwent epiphysiodesis of the healthy contralateral tibia with a poor outcome as she developed an unexpected angular deformity (valgum and procurvatum) in the proximal tibia (Fig. 2).
Female aged 12.5 years right PMTB. Discrepancy of 3cm treated by epiphysiodesis of the healthy limb with screws using the Metaizeau technique at the age of 9.5 years. Control at 3 years showing a reduction of the discrepancy to 1.5cm with associated valgus and procurvatum deformity of the healthy knee.
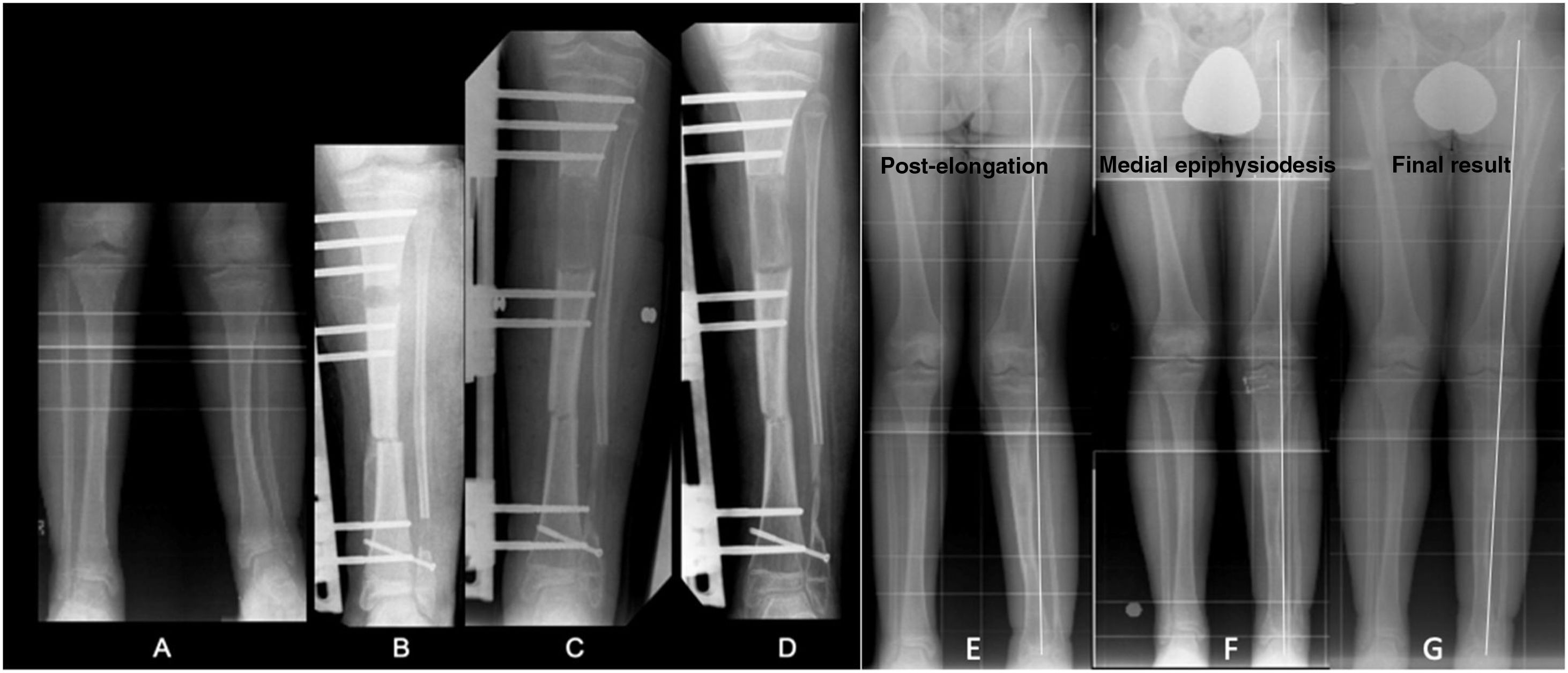
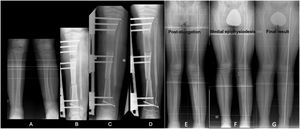
We observed a mean healing rate of 34.5days/cm (13–53days/cm). In one of the cases where we used the modified lengthening technique on a 3.5mm slotted AO-type plate, the average healing rate was 13days/cm (Fig. 3).
(A) PMTB in a 12-year-old male. Dysmetria of 5cm and valgus of 13°. (B–D) Treatment with monolateral external fixation for proximal tibial bone elongation of 7cm and mediodiaphyseal shortening varising osteotomy. (E) Result after compensated discrepancy with residual valgas. (F) Guided medial proximal tibial growth. (G) Final result at 15 years.
The most frequent “problem” according to Paley6 during the bone lengthening procedure was infection around the external fixation screws (superficial or deep) and it affected all cases. In all the patients the infection was resolved by local measures and/or oral antibiotherapy. Two of the patients had asymptomatic pseudarthrosis of the fibula at the level of the supramalleolar osteotomy. The “obstacles” included two cases presenting osteoporotic changes associated with pain compatible with CRPS that resolved when assisted weightbearing of the limb was initiated and limb function was restored with physiotherapy and rehabilitation. Two had weakness and limitation of plantar flexion of the ankle (greater than preoperatively). Another obstacle was presented by one of the cases who presented paralysis of the EPS nerve that required orthotic treatment with a Rancho Los Amigos splint and physiotherapy, which resolved after 4 months.
Of note among the “complications” was a minor complication in one patient who required correction of the mechanical axis due to genu valgum after tibial lengthening of 7cm which required temporary hemiepiphysiodesis with “8” plates (guided growth) of the medial proximal tibia (Fig. 4).
Other complications unrelated to bone elongation included 2 patients who suffered a diaphyseal fracture of the tibia. One at 8 months of age and treated conservatively, and the other in adulthood due to a motorbike accident requiring surgical treatment by intramedullary nailing. Another patient with stiffness of the subtalar joint was diagnosed with painful calcaneal-talar coalition after CT scan, requiring resection of the bony bar and interposition of fat.
One patient was treated in another centre for a real discrepancy of 3cm (expected to be 4.5cm) at the age of 9.5 years by epiphysiodesis of the proximal tibia of the healthy limb. She presented knee deformity in procurvatum and valgus of the health tibia as a complication, for which she is being followed-up in our unit (Fig. 2).
DiscussionCongenital posteromedial bow of the tibia was first described by Heyman et al.1 distinguishing it from other deformities with a tendency to pseudarthrosis or to cause large discrepancies and, confirmed by later studies by Miller,7 highlighting the tendency for this deformity to correct spontaneously, although they gave little importance to limb length discrepancy. Later publications, such as that by Hoffman y Wenger,2 conclude that this condition does not progress as well as initially thought and that clinical-radiological follow-up of discrepancy should continue until maturity, so that compensation by epiphysiodesis of the longer leg could be carried out if necessary. Pappas8 proposed a similar approach in his study of 33 patients, in which he observed a final dysmetria of 6.9cm, which related to the severity of the deformity. We, like other authors8,9 observed that the growth inhibition of PMTB remains constant throughout development and apparently from the embryonic period,10 a useful condition for calculating the discrepancy at skeletal maturity using growth remaining tables or the multiplier method.10 In our series we observed small variations during infancy, with about 11% inhibition of growth of the affected tibia with respect to the healthy tibia as shown in Table 4, causing discrepancies of between 4cm and 7cm. However, for others, the length discrepancy relates to the severity of the deformity at birth,4 which we were unable to verify in our case.
With regard to the remodelling of the diaphyseal deformity and realignment of joint surfaces, Murray et al.11 produced a transverse proximal tibial fracture deviated in valgus in 12 eight-week-old New Zealand white rabbits demonstrating the mechanisms involved, observing that joint realignment is much more rapid due to eccentric growth of the physis according to the well-known Hueter-Volkmann law and how the remodelling of the diaphyseal deformity is slower and incomplete at the expense of the periosteum according to Wolff's law. This means that after a few years’ progression we will find that the knee and ankle joints will be well aligned, but with a slight or moderate residual diaphyseal deformity, almost constant, with decentralisation of the tibial mechanical axis. In our series we found that the mechanical axis of the limb is normoaligned, but in a large number of cases the anatomical axis does not coincide with the mechanical axis at the tibial level. Regarding the distal physis, few authors report morphological changes in the distal end of the tibia4 and none mention tarsal abnormalities such as those found in our study, which account for up to 20% of the total limb discrepancy, in some cases more than one cm, and which should be considered when planning surgery to compensate limb length.
The therapeutic management of PMTB is debated. Whether it is better to treat large tibial angular deformities early by osteotomy,9 or to use bone lengthening procedures at an early age12 or to wait until the end of growth.5,13 We agree with the idea of waiting until the age of 12 years to make surgical decisions, since if elongation is performed at an early age, other additional techniques may be necessary on maturation, such as epiphysiodesis14 or new elongation to equalise the length of the limbs. Physiologically, the periosteum of the tibia will remodel diaphyseal deviations in valgus and recurvatum and asymmetric physeal growth will reorient the joints. By the age of 12 years, which is when a child will have tripled their birth height, we will have a better idea of the final discrepancy at skeletal maturity and whether there are significant angular deviations to plan whether angular correction is required in addition to bone elongation.
We do not believe that it is useful to use temporary or definitive epiphysiodesis techniques in the healthy limb due to the unpredictability of the method, the fact that it is not free of complications, and the anticipation necessary to keep the 2 tibias equal. According to the Menelaus arithmetic method, to compensate for a difference of 36mm we would have to perform an epiphysiodesis of the proximal tibia at 8 years of age in girls and at 10 years in boys, and if we also blocked the growth of the distal femur it would be at 11.5 years in girls and 13.5 years in boys, assuming asymmetry in their knee height as well.
Therefore, length discrepancy behaves independently from the initial diaphyseal angulation and requires compensation between 4cm and 7cm by bone elongation as proposed by different authors at around 12 years of age. The method of choice in our centre, and preferable to slowing down the growth of the healthy limb, was progressive bone elongation or conventional callotasis and recently with a modification of the technique – lengthening on a slotted plate – which significantly reduces the external fixation time, from 35days/cm to 13days/cm and with fewer complications by substantially reducing the external fixation time. This mixed method and elongation with magnetic nailing when there is no residual deformity are the methods of choice to compensate for the difference in limb length. The mean final residual discrepancy was .6cm at skeletal maturity and in all cases, the usual complications of lengthening were resolved satisfactorily without sequelae. We believe that bone lengthening is the best therapeutic option in discrepancies greater than 4cm (whether or not an angular deformity is present) compared to epiphysiodesis of the healthy contralateral tibia, which a priori, being a quick and simple procedure, is error-free in prediction calculations and undesired angular deformities in a previously healthy limb.
To conclude, we would like to highlight that there is substantial improvement during the first years of life in PMTB. Joint alignment at the expense of asymmetric physeal growth is achieved before diaphyseal deformity correction, with persistent residual valgus and recurvatum. The length discrepancy of the tibia increases as the child grows because there is approximately 11% growth inhibition which will result in a discrepancy at skeletal maturity of between 4cm and 7cm. Progressive bone elongation, callotasis or its variants, is the method of choice to compensate for this discrepancy at skeletal maturity, it being possible to correct associated angular deviations in the same surgical procedure.
Level of evidenceLevel of evidence: IV.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: González-Herranz P, Penelas-Abelleira N, Barreiro-Pensado C, Castellano-Romero I. Deformidad posteromedial de la tibia: evolución radiológica y tratamiento de la discrepancia. Rev Esp Cir Ortop Traumatol. 2021;65:207–215.