Surveillance systems make it possible to analyze the trends of infections associated with hip arthroplasty. The aim of this study is to determine risk factors associated with surgical site infection (SSI) and mortality following total hip arthroplasty (THA) or hemiarthroplasty (HHA).
MethodsObservational study including individuals ≥18 years who underwent THA or HHA between January 2007 and December 2017. Incidences of SSI were compared with the national rates according to NNIS indexes. Risk factors for SSI and mortality were evaluated using multiple logistic regression model.
ResultsIn THA, an association with a higher risk of SSI was found with hospital stay (OR 1.08; 95% CI: 1.02–1.15; p=.007).
In HHA, hospital stay was associated with a higher risk of SSI (OR 1.05; 95% CI: 1.02–1.08; p=.001), as also happened with obesity (OR 13.28; 95% CI: 2.68–65.74; p=.002), while inadequate antibiotic prophylaxis was associated with a higher risk of mortality (OR 4.69; 95% CI: 1.01–21.74; p=.048).
ConclusionIn THA, hospital stay was associated with an increased risk of SSI. In HHA this association is found with hospital stay and obesity, while inadequate antibiotic therapy was associated with mortality.
Los sistemas de vigilancia permiten analizar las tendencias de las infecciones asociadas con la artroplastia de cadera. El objetivo de este estudio fue determinar los factores de riesgo asociados con la infección de localización quirúrgica (ILQ) y la mortalidad tras artroplastia total (ATC) o parcial (APC) de cadera.
MétodosEstudio observacional que incluyó individuos ≥18 años que se sometieron a ATC o APC entre enero de 2007 y diciembre de 2017. Las incidencias de ILQ se compararon con las tasas nacionales según los índices NNIS. Los factores de riesgo de ILQ y mortalidad se evaluaron mediante el modelo de regresión logística múltiple.
ResultadosEn la ATC, la estancia hospitalaria (OR 1,08; IC 95%: 1,02-1,15; p=0,007) se asoció a un mayor riesgo de ILQ.
En la APC, la estancia hospitalaria (OR 1,05; IC 95%: 1,02-1,08; p=0,001) y la obesidad (OR 13,28; IC 95%: 2,68-65,74; p=0,002) se asociaron a un mayor riesgo de ILQ, mientras que la profilaxis antibiótica inadecuada (OR 4,69; IC 95%: 1,01-21,74; p=0,048) se asoció a mayor riesgo de mortalidad.
ConclusiónEn la ATC, la estancia hospitalaria se asoció con un mayor riesgo de ILQ. En la APC esta asociación se encontró con la estancia hospitalaria y la obesidad, mientras que la terapia antibiótica inadecuada se asoció a mortalidad.
During recent decades joint replacement surgery has undergone a significant improvement in the functional capacity of patients with arthropathy. However, surgical site infections (SSI) are one of the most important causes of complications associated with the implantation of joint prostheses.1
Several factors identified in the appearance of joint prostheses infections are: advanced age, diabetes mellitus, tumour, chronic kidney disease, obesity, previous prosthesis, NNIS (National Nosocomial Infections Surveillance risk index), and the duration of surgery.1–3
Acquired infection epidemiological surveillance systems in the hospital tend to include modules for monitoring SSI which prioritise preventive interventions. The INCLIMECC (indicators of continual improvement in quality) is a national prospective system of standardised surveillance, established in Spain in 1997, for health-care associated infection (HAI) in patients who undergo surgery.4 In 2011 the Community of Madrid developed the current system of vigilance and control of HAI (VIRAS-Madrid), which in addition to surveillance included specific measures of infection prevention.5 Since 2016 the Spanish Society of Preventative Medicine has aimed to reduce the number of surgical infections, has established the Zero Surgical Site Infection Project (ZSSI), the success of which lies in the joint application of individual measures (such as the use of verification lists) and a comprehensive safety plan.6
Although SSI or mortality risk factors have been widely studied in total hip arthroplasty (THA), there are few studies in Spain which analyse which factors could be independently associated with a higher risk of infection or mortality in hemiarthroplasty of the hip (HHA).
The aim of this study was to determine the risk factors associated with SSI and mortality after total and partial hip arthroplasty.
Material and methodsStudy design and populationAnalytical, observational, retrospective study in patients ≥18 years taken from the INCLIMECC cohort of the Hospital Universitario de La Princesa and who had undergone THA or HHA surgery between January 2007 and December 2017.
All the patients were followed-up from the time of surgical procedure until discharge, including re-admission for infections in any part of the body. Surveillance protocols were previously structured and consensual. The criteria used to define the SSI categories and the risk index of the patient were those established by the CDC and NNIS.7 The surgical procedures included are those listed by the NHSN and classified according to the ICD.
Outcome variablesFor SSI, the date of infection was recorded as determined by the doctor in the medical record, together with the degree of tissue involved (superficial, deep and/or organ/space). Isolated microorganism data were extracted from the patient's microbiological cultures.
Data on mortality were also obtained from the medical file.
Risk exposure variablesThese were taken from the medical record of sociodemographic data (age, sex) and medical history (diabetes, chronic obstructive pulmonary disease [COPD], chronic kidney disease [CKD] and obesity). Admission and discharge data were recorded, taken from the hospital admission service and the ICD codes of diagnosis and intervention.
The duration of surgery was recorded, from start to closure, in minutes. The American Society of Anaesthesiologist's classification (ASA class) was defined as that determined by the anaesthesiologist, taken from the pre-anaesthesia sheet or from the medical file (codes 1–5).8
The level of contamination of surgery was classified as clean surgery, clean-contaminated surgery or dirty/infected surgery. When more than one procedure was undertaken during the same intervention, with a different degree of contamination, the one with the higher contamination was selected.
Compliance with the verification list was classed as complete (when all fields were completed, including the signatures), incomplete (when one field lacked completion) or not undertaken (not implemented).
Preoperative preparation was classed as: correct, incorrect or no preparation/no record of preparation. Incorrect preparation was classified according to causes such as: no antiseptic preoperative application; no oral antiseptic application; no washing of body prior to surgery or inadequate elimination of hair from surgical site.
Antibiotic prophylaxis was classified as appropriate or inadequate in accordance with the antibiotic policy guidelines issued by the hospital's antibiotic committee. Inadequate antibiotic prophylaxis was also classified as: inappropriate choice (when the agent used differed from that recommended in the guidelines with no apparent reason such as allergy), inappropriate timing (when the agent was used more than 60min prior to surgery, except if vancomycine or fluoroquinolone was used, or when used after surgery), inappropriate dose and inappropriate duration (when antibiotic prophylaxis was continued for over 48h).
Statistical analysisA descriptive analysis, indicating frequencies and percentages for qualitative variables and mean (SD) for quantitative variables was undertaken. Surgical infection incidence rates were also calculated according to the NNIS risk index of each one of the surgical procedures.
Bivariate analysis was undertaken using the Chi-square test to study the qualitative variables between independent groups, with the exact Fisher test or the likelihood ratio test when necessary. To study quantitative variables between independent groups, the Student's t-test was used (parametric, in the case of normality) and the Mann–Whitney U test (non parametric in the case of non normal distribution).
The infection rates were compared with the NNIS risk index through the indirect standardisation, using data from the INCLIMECC network on a national level as the standard population. Standardised infection rates (SIR) were used for reporting.
Association between each surgical or patient characteristic with SSI or mortality was summarised with odds ratios (OR) and confidence intervals (CI) of 95% obtained from the multiple logistic regression. The models were adjusted for the sociodemographic variables of age and sex, and as the variables which showed a significant association in bivariate analysis (see footnotes to the tables).
Statistical significance was established in p<.05. Analysis was undertaken with Stata/SE, version 13 (Stata Corp, College Station, TX, U.S.A.).
The study was approved by the Drugs Research Ethics Committee (CEIm for its initials in Spanish) of the Hospital Universitario de La Princesa, with file number: 3658.
ResultsIn the 10 years of follow-up 1213 hip procedures were collected, with 609 (5.2%) total hip arthroplasties, 480 (39.6%) hemiarthroplasties of the hip, 114 (9.4%) prothesis reviews and 10 (.8) other open surgery reductions without prostheses.
One thousand and thirty-nine primary clean surgical interventions were recorded, of which 563 were THA and 476 HHA. Of these, 532 (51.2%) were in patients with osteoarthritis, 489 (47.1%) hip fractures and 18 (1.7%) other diagnoses. There were 439 (42.3%) emergency admissions and 55 (5.3%) emergency surgical procedures. The HHA were most commonly emergency surgery (1.9% emergency HHA surgery compared with .5% THA, p<.001).
Mean age of patients was 76.6 years. The patients who underwent HHA were of a higher mean age (84.9 years in HHA vs. 69.6 years in THA, p<.001). Out of the total, 35.7% were male. The patients with HHA were more frequently women (73.3% women in HHA and 56.7% in THA, p<0001).
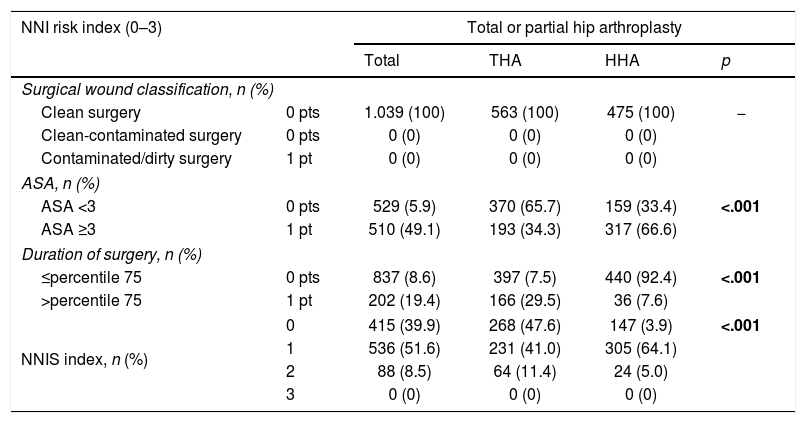
Out of the 1039 patients, 137 (13.2%) had diabetes, 49 (4.7%) COPD, 32 (3.1%) CKD and 48 (4.6%) obesity. Mean ASA class was 2.5 (SD .6). The NNIS index 0 was recorded in 415 (39.9%) patients, NNIS 1 in 536 (51.6%) and NNIS 2 in 88 (8.5%). Table 1 shows the comparison of the components of the NNIS index according to the type of arthroplasty.
Comparison of components, of the NNIS risk index according to type of hip arthroplasty.
| NNI risk index (0–3) | Total or partial hip arthroplasty | ||||
|---|---|---|---|---|---|
| Total | THA | HHA | p | ||
| Surgical wound classification, n (%) | |||||
| Clean surgery | 0 pts | 1.039 (100) | 563 (100) | 475 (100) | − |
| Clean-contaminated surgery | 0 pts | 0 (0) | 0 (0) | 0 (0) | |
| Contaminated/dirty surgery | 1 pt | 0 (0) | 0 (0) | 0 (0) | |
| ASA, n (%) | |||||
| ASA <3 | 0 pts | 529 (5.9) | 370 (65.7) | 159 (33.4) | <.001 |
| ASA ≥3 | 1 pt | 510 (49.1) | 193 (34.3) | 317 (66.6) | |
| Duration of surgery, n (%) | |||||
| ≤percentile 75 | 0 pts | 837 (8.6) | 397 (7.5) | 440 (92.4) | <.001 |
| >percentile 75 | 1 pt | 202 (19.4) | 166 (29.5) | 36 (7.6) | |
| NNIS index, n (%) | 0 | 415 (39.9) | 268 (47.6) | 147 (3.9) | <.001 |
| 1 | 536 (51.6) | 231 (41.0) | 305 (64.1) | ||
| 2 | 88 (8.5) | 64 (11.4) | 24 (5.0) | ||
| 3 | 0 (0) | 0 (0) | 0 (0) | ||
ASA: American Society of Anaesthesiologist's classification of physical status; HHA: hemiarthroplasty of the hip; NNIS: National Nosocomial Infections Surveillance system; THA: total hip arthroplasty.
Figures in bold indicate statistical significance (p<.05).
Mean hospital stay was 11.3 days (SD 7.7), preoperative hospital stay was 2.3 days (SD 3.8) and postsurgical hospital stay was 9 days (SD 6.4). Patients with HHA had a higher mean stay (14.2 days in HHA vs. 8.9 days in THA, p<.001), higher preoperative stay (3.7 days vs. 1.2 days, p<.001) and higher postsurgical stay (1.5 days vs. 7.7 days, p<.001).
With regard to patient safety practices, the surgical verification list was complete in 103 interventions (9.9%), incomplete in 137 (13.2%) and was not fulfilled in 799 (76.9%). Preoperative preparation was inappropriate in 309 (29.7%) interventions, with the most common cause being incorrect elimination of hair in 303 interventions. In 723 cases (69.6%) there was no record of whether surgical preparations had been carried out correctly.
Antibiotic prophylaxis was inappropriate in 48 interventions (4.7%), with the most common cause being inappropriate duration in 23 interventions (2.25%) and inadequate dose in 13 (1.3%).
Surgical site infectionsOf the 1039 primary interventions of THA or HHA, 27 SSI were recorded. Depending on the level of affected tissue, 15 were superficial, 10 deep and 2 organ/space. The most frequent microorganisms were Pseudomonas aeruginosa in 4 patients (21.1%) and methicillin-resistant Staphylococcus aureus in 2 patients (1.5%).
Among those with SSI, there were 6 (22.2%) patients with NNIS 0, 20 (47.1%) with NNIS 1 and 1 (3.7%) with NNIS 2.
The SIR was 1.38 (95% CI: .86–1.90) regarding data from the national level INCLIMECC network.
More infections were produced in patients who underwent HHA (3.99% SSI in HHA vs. 1.42% SSI in THA, p=.009).
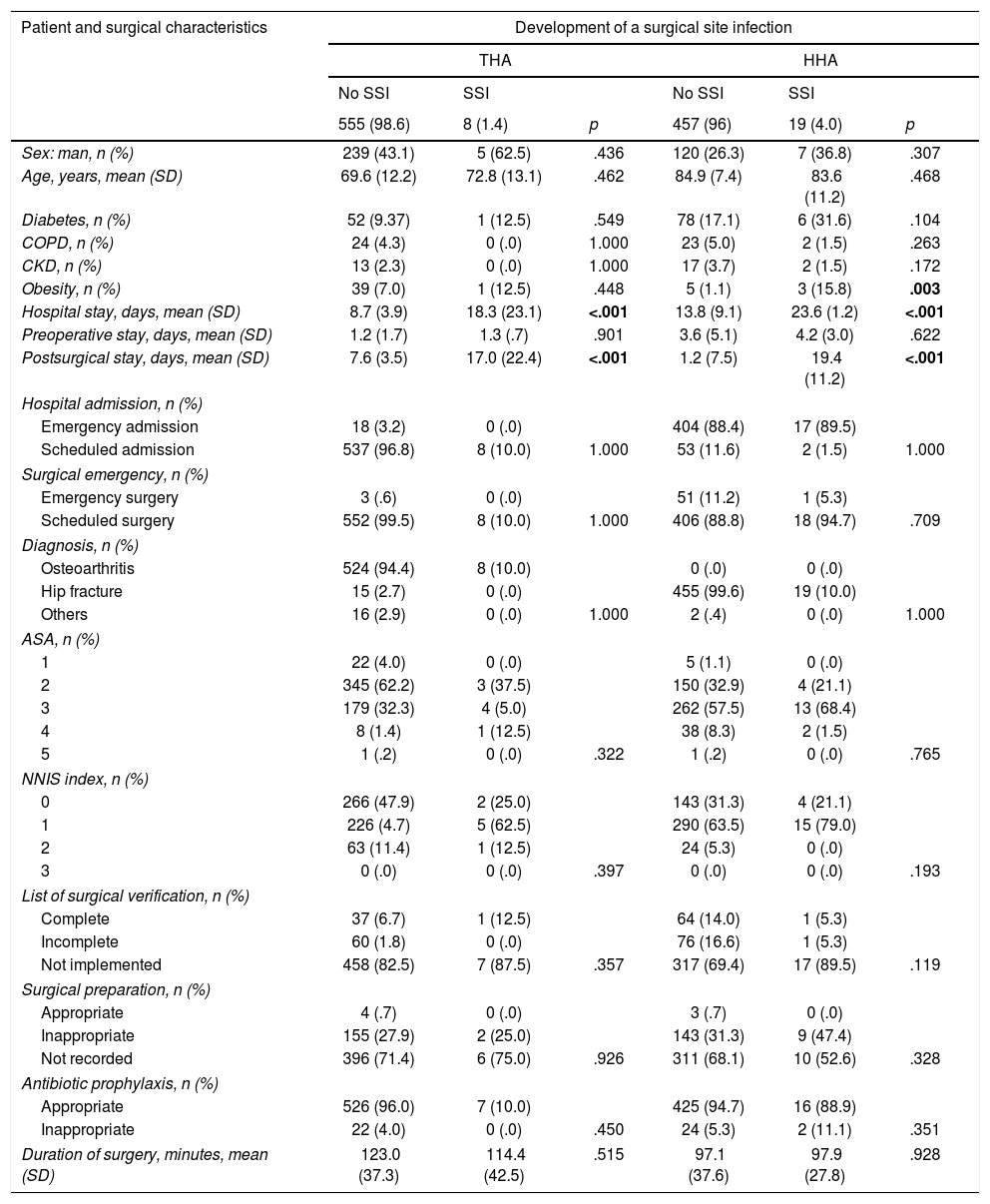
Table 2 compares the characteristics of patients who developed SSI vs. non infected patients.
Comparison of risk factors according to the development of a surgical site infection.
| Patient and surgical characteristics | Development of a surgical site infection | |||||
|---|---|---|---|---|---|---|
| THA | HHA | |||||
| No SSI | SSI | No SSI | SSI | |||
| 555 (98.6) | 8 (1.4) | p | 457 (96) | 19 (4.0) | p | |
| Sex: man, n (%) | 239 (43.1) | 5 (62.5) | .436 | 120 (26.3) | 7 (36.8) | .307 |
| Age, years, mean (SD) | 69.6 (12.2) | 72.8 (13.1) | .462 | 84.9 (7.4) | 83.6 (11.2) | .468 |
| Diabetes, n (%) | 52 (9.37) | 1 (12.5) | .549 | 78 (17.1) | 6 (31.6) | .104 |
| COPD, n (%) | 24 (4.3) | 0 (.0) | 1.000 | 23 (5.0) | 2 (1.5) | .263 |
| CKD, n (%) | 13 (2.3) | 0 (.0) | 1.000 | 17 (3.7) | 2 (1.5) | .172 |
| Obesity, n (%) | 39 (7.0) | 1 (12.5) | .448 | 5 (1.1) | 3 (15.8) | .003 |
| Hospital stay, days, mean (SD) | 8.7 (3.9) | 18.3 (23.1) | <.001 | 13.8 (9.1) | 23.6 (1.2) | <.001 |
| Preoperative stay, days, mean (SD) | 1.2 (1.7) | 1.3 (.7) | .901 | 3.6 (5.1) | 4.2 (3.0) | .622 |
| Postsurgical stay, days, mean (SD) | 7.6 (3.5) | 17.0 (22.4) | <.001 | 1.2 (7.5) | 19.4 (11.2) | <.001 |
| Hospital admission, n (%) | ||||||
| Emergency admission | 18 (3.2) | 0 (.0) | 404 (88.4) | 17 (89.5) | ||
| Scheduled admission | 537 (96.8) | 8 (10.0) | 1.000 | 53 (11.6) | 2 (1.5) | 1.000 |
| Surgical emergency, n (%) | ||||||
| Emergency surgery | 3 (.6) | 0 (.0) | 51 (11.2) | 1 (5.3) | ||
| Scheduled surgery | 552 (99.5) | 8 (10.0) | 1.000 | 406 (88.8) | 18 (94.7) | .709 |
| Diagnosis, n (%) | ||||||
| Osteoarthritis | 524 (94.4) | 8 (10.0) | 0 (.0) | 0 (.0) | ||
| Hip fracture | 15 (2.7) | 0 (.0) | 455 (99.6) | 19 (10.0) | ||
| Others | 16 (2.9) | 0 (.0) | 1.000 | 2 (.4) | 0 (.0) | 1.000 |
| ASA, n (%) | ||||||
| 1 | 22 (4.0) | 0 (.0) | 5 (1.1) | 0 (.0) | ||
| 2 | 345 (62.2) | 3 (37.5) | 150 (32.9) | 4 (21.1) | ||
| 3 | 179 (32.3) | 4 (5.0) | 262 (57.5) | 13 (68.4) | ||
| 4 | 8 (1.4) | 1 (12.5) | 38 (8.3) | 2 (1.5) | ||
| 5 | 1 (.2) | 0 (.0) | .322 | 1 (.2) | 0 (.0) | .765 |
| NNIS index, n (%) | ||||||
| 0 | 266 (47.9) | 2 (25.0) | 143 (31.3) | 4 (21.1) | ||
| 1 | 226 (4.7) | 5 (62.5) | 290 (63.5) | 15 (79.0) | ||
| 2 | 63 (11.4) | 1 (12.5) | 24 (5.3) | 0 (.0) | ||
| 3 | 0 (.0) | 0 (.0) | .397 | 0 (.0) | 0 (.0) | .193 |
| List of surgical verification, n (%) | ||||||
| Complete | 37 (6.7) | 1 (12.5) | 64 (14.0) | 1 (5.3) | ||
| Incomplete | 60 (1.8) | 0 (.0) | 76 (16.6) | 1 (5.3) | ||
| Not implemented | 458 (82.5) | 7 (87.5) | .357 | 317 (69.4) | 17 (89.5) | .119 |
| Surgical preparation, n (%) | ||||||
| Appropriate | 4 (.7) | 0 (.0) | 3 (.7) | 0 (.0) | ||
| Inappropriate | 155 (27.9) | 2 (25.0) | 143 (31.3) | 9 (47.4) | ||
| Not recorded | 396 (71.4) | 6 (75.0) | .926 | 311 (68.1) | 10 (52.6) | .328 |
| Antibiotic prophylaxis, n (%) | ||||||
| Appropriate | 526 (96.0) | 7 (10.0) | 425 (94.7) | 16 (88.9) | ||
| Inappropriate | 22 (4.0) | 0 (.0) | .450 | 24 (5.3) | 2 (11.1) | .351 |
| Duration of surgery, minutes, mean (SD) | 123.0 (37.3) | 114.4 (42.5) | .515 | 97.1 (37.6) | 97.9 (27.8) | .928 |
ASA: American Society of Anaesthesiologist's classification of physical status; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; HHA: hemiarthroplasty of the hip; SSI: surgical site infection; THA: total hip arthroplasty.
NNIS: National Nosocomial Infections Surveillance system.
Figures in bold indicate statistical significance (p<.05).
Patients with THA who developed SSI had a global hospital stay (13 days for SSI vs. 8.7 days without SSI, p<.001) and longer postoperative stay (17 days for SSI vs. 7.6 days without SSI, p<.001).
There was a higher percentage of HHA patients who developed SSI with obesity (15.8% vs. 1.1%; p=.003) and with longer overall hospital stay (23.6 days vs. 13.8 days; p<.001) and longer postsurgical periods (19.4 days vs. 1.2 days; p<.001).
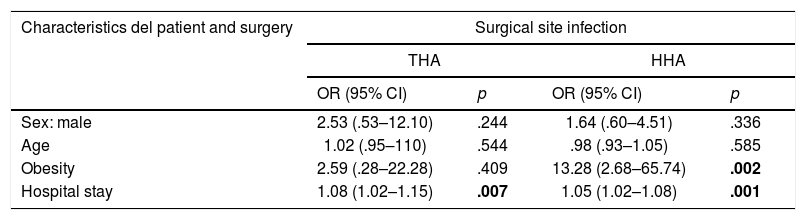
In the multivariable analysis, in THA, hospital stay (OR 1.08; 95% CI 1.02–1.15; p=.007) was associated with a higher SSI risk.
In HHA, hospital stay was associated with a higher risk of SSI (OR 1.05; 95% CI: 1.02–1.08; p=.001), and also obesity (OR 13.28; 95% CI: 2.68–65.74; p=.002) (Table 3).
Association between risk factors and the development of surgical site infection in total and partial hip arthroplasty.
| Characteristics del patient and surgery | Surgical site infection | |||
|---|---|---|---|---|
| THA | HHA | |||
| OR (95% CI) | p | OR (95% CI) | p | |
| Sex: male | 2.53 (.53–12.10) | .244 | 1.64 (.60–4.51) | .336 |
| Age | 1.02 (.95–110) | .544 | .98 (.93–1.05) | .585 |
| Obesity | 2.59 (.28–22.28) | .409 | 13.28 (2.68–65.74) | .002 |
| Hospital stay | 1.08 (1.02–1.15) | .007 | 1.05 (1.02–1.08) | .001 |
CI: confidence interval; HHA: hemiarthroplasty of the hip; OR: odds ratio; THA: total hip arthroplasty.
Regression model adjusted by age (in years) sex, obesity and hospital stay (in days).
The figures in bold indicate statistical significance (p<.05).
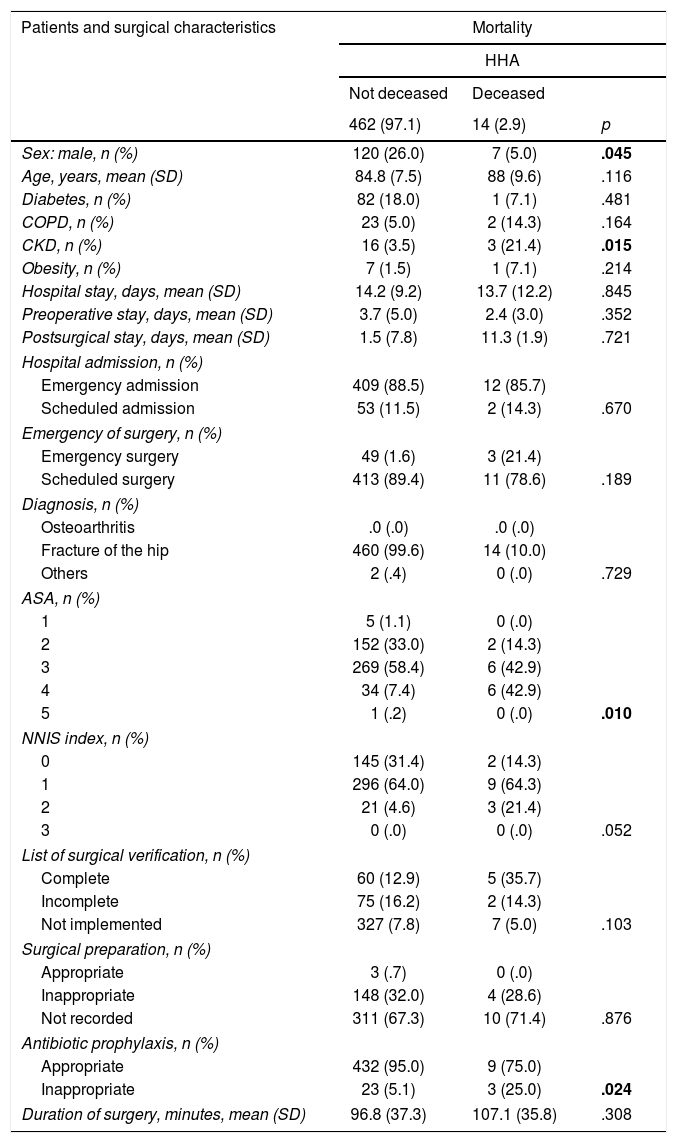
Of the 1039 patients, 14 deaths were recorded (1.35%). No patients died with primary THA during the study period (2.92% died in HHA vs. 0% in THA, p<.001).
Table 4 compares deceased patient characteristics with those who did not die.
Comparison of risk factors according to mortality.
| Patients and surgical characteristics | Mortality | ||
|---|---|---|---|
| HHA | |||
| Not deceased | Deceased | ||
| 462 (97.1) | 14 (2.9) | p | |
| Sex: male, n (%) | 120 (26.0) | 7 (5.0) | .045 |
| Age, years, mean (SD) | 84.8 (7.5) | 88 (9.6) | .116 |
| Diabetes, n (%) | 82 (18.0) | 1 (7.1) | .481 |
| COPD, n (%) | 23 (5.0) | 2 (14.3) | .164 |
| CKD, n (%) | 16 (3.5) | 3 (21.4) | .015 |
| Obesity, n (%) | 7 (1.5) | 1 (7.1) | .214 |
| Hospital stay, days, mean (SD) | 14.2 (9.2) | 13.7 (12.2) | .845 |
| Preoperative stay, days, mean (SD) | 3.7 (5.0) | 2.4 (3.0) | .352 |
| Postsurgical stay, days, mean (SD) | 1.5 (7.8) | 11.3 (1.9) | .721 |
| Hospital admission, n (%) | |||
| Emergency admission | 409 (88.5) | 12 (85.7) | |
| Scheduled admission | 53 (11.5) | 2 (14.3) | .670 |
| Emergency of surgery, n (%) | |||
| Emergency surgery | 49 (1.6) | 3 (21.4) | |
| Scheduled surgery | 413 (89.4) | 11 (78.6) | .189 |
| Diagnosis, n (%) | |||
| Osteoarthritis | .0 (.0) | .0 (.0) | |
| Fracture of the hip | 460 (99.6) | 14 (10.0) | |
| Others | 2 (.4) | 0 (.0) | .729 |
| ASA, n (%) | |||
| 1 | 5 (1.1) | 0 (.0) | |
| 2 | 152 (33.0) | 2 (14.3) | |
| 3 | 269 (58.4) | 6 (42.9) | |
| 4 | 34 (7.4) | 6 (42.9) | |
| 5 | 1 (.2) | 0 (.0) | .010 |
| NNIS index, n (%) | |||
| 0 | 145 (31.4) | 2 (14.3) | |
| 1 | 296 (64.0) | 9 (64.3) | |
| 2 | 21 (4.6) | 3 (21.4) | |
| 3 | 0 (.0) | 0 (.0) | .052 |
| List of surgical verification, n (%) | |||
| Complete | 60 (12.9) | 5 (35.7) | |
| Incomplete | 75 (16.2) | 2 (14.3) | |
| Not implemented | 327 (7.8) | 7 (5.0) | .103 |
| Surgical preparation, n (%) | |||
| Appropriate | 3 (.7) | 0 (.0) | |
| Inappropriate | 148 (32.0) | 4 (28.6) | |
| Not recorded | 311 (67.3) | 10 (71.4) | .876 |
| Antibiotic prophylaxis, n (%) | |||
| Appropriate | 432 (95.0) | 9 (75.0) | |
| Inappropriate | 23 (5.1) | 3 (25.0) | .024 |
| Duration of surgery, minutes, mean (SD) | 96.8 (37.3) | 107.1 (35.8) | .308 |
HHA: hemiarthroplasty of the hip; ASA: American Society of Anaesthesiologist's classification of physical status; COPD: chronic obstructive pulmonary disease; CKD: chronic kidney disease; SSI: surgical site infection; NNIS: National Nosocomial Infections Surveillance system.
Figures in bold indicate statistical significance (p<.05).
Patients with HHA who died were more frequently male (50% vs. 26%; p=.045), had a higher percentage of CKD (21.4% vs 3.5%; p=.015), of ASA class ≥3 (85.7% vs. 66%; p=.010) and a higher percentage of inadequate antibiotic prophylaxis (25% vs. 5%; p=.024). The cause of inadequacy of prophylaxis in the three deceased patients was the inappropriate choice of antibiotic in two of them and the duration of the prophylaxis in the other.
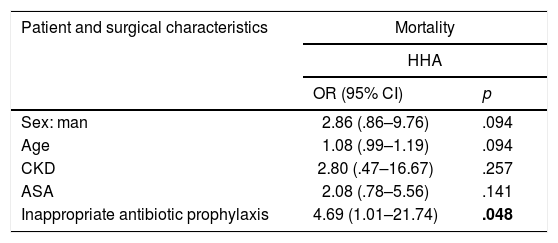
In multivariate analysis, in the HHA, inadequate antibiotic prophylaxis was associated with a higher risk of mortality (OR 4.69; 95% CI: 1.01–21.74; p=.048) (Table 5).
Association between risk factors and mortality in hemiarthroplasty.
| Patient and surgical characteristics | Mortality | |
|---|---|---|
| HHA | ||
| OR (95% CI) | p | |
| Sex: man | 2.86 (.86–9.76) | .094 |
| Age | 1.08 (.99–1.19) | .094 |
| CKD | 2.80 (.47–16.67) | .257 |
| ASA | 2.08 (.78–5.56) | .141 |
| Inappropriate antibiotic prophylaxis | 4.69 (1.01–21.74) | .048 |
ASA: American Society of Anaesthesiologist's classification of physical status; CI: confidence interval; CKD: chronic kidney disease; HHA: hemiarthroplasty of the hip; OR: odds ratio.
Regression model adjust by age (in years), sex, chronic kidney disease, ASA and antibiotic prophylaxis.
Figures in bold indicate statistical significance (p<.05).
Surgical site infections associated with prosthetic surgery of the hip are a major clinical problem. Although risk factors of infection or mortality associated with THA have been widely studied, less is known about the factors associated with these complications in HHA.
This study shows the factors associated with a higher infection between these two types of prosthetic surgery do not have to coincide.
Surgical site infection and mortality risk factorsSSI rates of 2.5% after THA have been described and between 1.7% and 7.3% after HHA.9,10 in our study the SSI rate for THA was 1.4% and 4.0% for HHA.
Although no association was found in this study for emergency surgery with the SSI rate, a higher percentage of infection was found in HHA patients. Total primary hip arthroplasty from osteoarthritis is usually an elective procedure, whilst that of hemiarthroplasty from fracture may be a more urgent procedure,11 which could explain these differences. Other studies also found higher SSI rates in patients who underwent THA due to hip trauma fracture.12,13
Bearing in mind the effect of comorbidities, several studies found there was a higher risk of infection after primary hip replacement among diabetic and obese patients.14,15 In one systemic review they identified preoperative comorbidities (such as obesity or a more advanced age) as SSI risk factors after HHA. Also included were factors relating to surgery (such as time in operating theatre) and postoperative management (such as length of hospital stay or prolonged wound drainage).10 In this study, this association was not found after THA, but an association after HHA was found with obesity, with a higher SSI risk.
The NNIS index allowed for risk of infection in the surgical site to be calculated,16 whilst the ASA class was an independent predictor of mortality after surgery.17,18 In this study, patients with SSI had no significant differences in their NNIS index, but a higher ASA class in bivariate analysis was found in those who died.
The longer length of surgery was also related to a higher risk of postoperative complications after total arthroplasty,19 although this association was not found in this study. The longest interventions were usually the most complicated ones but, on the other hand, duration of surgery could depend on the variability of the surgical act, and a more prolonged surgery could imply greater precaution and surgical attention than others.
Several studies have demonstrated that a longer preoperative stay was associated with a higher risk of SSI after primary THA20 although in this study we were unable to find that association. However, the association found between hospital stay and the risk of SSI may be due to the fact that a longer postoperative stay is a consequence of SSI and not a risk factor for it. Other studies have demonstrated that infection, among other complications, may prolong hospital stay in patients who undergo orthopaedic surgery.21
Although infection of the prosthesis does not appear to be the main cause of death in patients, some studies indicate that longer stay, due to infection could lead to a higher risk of mortality. One explanation could be that successive interventions and treatments with antibiotics precipitate the appearance of complications.22 It may also be due to the fact that, because they are patients with pre-existing pathologies, their poor baseline status and weakened immune systems are precisely what contribute to infection.23
Microorganisms in surgical site infectionsAccording to previous studies, the most common microorganisms in hip prosthesis infections are Staphylococcus aureus and Staphylococcus epidermidis.1,16 However, in our study we found Pseudomonas aeruginosa to be among the most frequent. Although gram-positive organisms are responsible in the majority of cases for joint prosthetic infection, gram-negative SSI are becoming increasingly more frequent.24
Preventative practices and patient safetyPrevious studies have shown that surgical verification lists reduced SSI and mortality,25,26 thanks to the improvement of teamwork and the safety culture.27 In this study, the incomplete or non implemented surgical verification list was significantly associated with a lower risk of mortality in bivariate analysis for HHA.
In the case of surgical preparation, several studies demonstrated their association with SSI.28,29 It is possible that this association was not found in this study because in the preoperative preparation only preoperative bathing at the time of surgery was taken into consideration. However, patients with scheduled interventions were admitted the day before surgery and bathing with chlorhexidine began from that time onwards.
With regard to the appropriateness of the antibiotic prophylaxis, previous studies found there was an association with SSI.30 But one study in Spain did not find any relationship between them.31 In one previous study in this same hospital, an association was also found between inadequate prophylaxis and SSI.2 Although other studies did not find any association between inadequate antibiotic prophylaxis and mortality,32 in this study, this association was found in HHA.
Strengths and limitationsThe strong points of this study include adjustment for many possible factors of confusion, and the fact that analysis of SSI risk factors was undertaken separately in THA and HHA.
However, this study also had several limitations. Due to the sample size and small number of events developed, studying THA and HHA separately meant no patients developed the events in all groups. In the case of THA, among the 11 patients who developed infection none had inadequate antibiotic prophylaxis, and on studying mortality, no patient died. Another major limitation of the surveillance system used was the lack of patient follow-up after discharge, and the infections which occurred after this, and which did not require readmission, could not be studied.
ConclusionsThis study suggests that SSI-associated risk factors in patients who have undergone THA or HHA may differ. In those who undergo HHA an association between obesity and a higher risk of SSI was found. In both interventions, a higher risk of SSI was associated with a longer hospital stay. Inadequate antibiotic therapy in HHA was associated with a higher risk of mortality.
Further studies in patients who undergo THA or HHA are required to identify the factors which may favour the appearance of complications so as to develop preventative measures.
Level of evidenceLevel of evidence II.
FinancingThis research study did not receive any specific aid from public or commercial sector agencies or any not-for-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Dr. Vicente Monge-Jodrá for his important work in the development of the INCLIMECC programme and his support in everything relating to its use, without which this study would not have been possible.
Please cite this article as: Hernández-Aceituno A, Ruiz-Álvarez M, Llorente-Calderón R, Portilla-Fernández P, Figuerola-Tejerina A. Factores de riesgo en artroplastia total y parcial de cadera: infección y mortalidad. Rev Esp Cir Ortop Traumatol. 2021;65:239–247.