The term, sacral fracture with traumatic spino-pelvic dissociation, is applied to those fractures of the sacrum in which there are both transverse and sagittal fracture lines in the sacrum, leading to a mechanical dissociation of the spine and the proximal fragment of the sacrum from the remaining sacrum and the pelvis.
It is a quite rare pathological condition, and probably underdiagnosed. As it usually results from a high energy multiple trauma, an early diagnosis and treatment are mandatory for a better functional prognosis.
We present a literature review of this relatively unknown injury.
Se emplea el término de fractura de sacro con disociación espóndilo-pélvica, para aquellas fracturas del sacro que conjugan un trazo transversal con trazos sagitales en ambas alas sacras, provocando de esta forma una separación mecánica entre el raquis –junto con el fragmento de sacro proximal resultante– y la pelvis.
Se trata de una lesión muy infrecuente, aunque probablemente infradiagnosticada. Presentándose habitualmente en el contexto de un politraumatismo de alta energía, su diagnóstico y tratamiento tempranos son fundamentales para un mejor pronóstico funcional.
Presentamos una revisión bibliográfica sobre esta entidad, relativamente poco conocida.
Traumatic loss of connection between the spine and pelvis, which usually occurs in high-energy trauma, can adopt many forms, including lumbosacral fracture-dislocation and bilateral sacroiliac dislocation. However, the term spondylo-pelvic or spino-pelvic (SP) traumatic dissociation, coined by Bents et al. in 19961 to distinguish it from the abovementioned, refers to a pathological condition in which this dissociation occurs due to the association of a transverse fracture with sagittal fractures in both sacral wings, resulting in a proximal segment with the vertebral spine and the proximal sacral fragment, which is mechanically separated from a distal segment formed by the pelvic girdle and the rest of the sacrum. The most common consequence in the sagittal plane is a relative flexion of the distal segment relative to the proximal caused by gravity and the hip flexors. This gives rise to a kyphosis deformity in the fracture site.2 In addition, the distal fragment usually experiences anterior or, more rarely, posterior displacement. In order to illustrate these changes, we present 2 cases treated at our hospital during the past 2 years (Figs. 1 and 2).
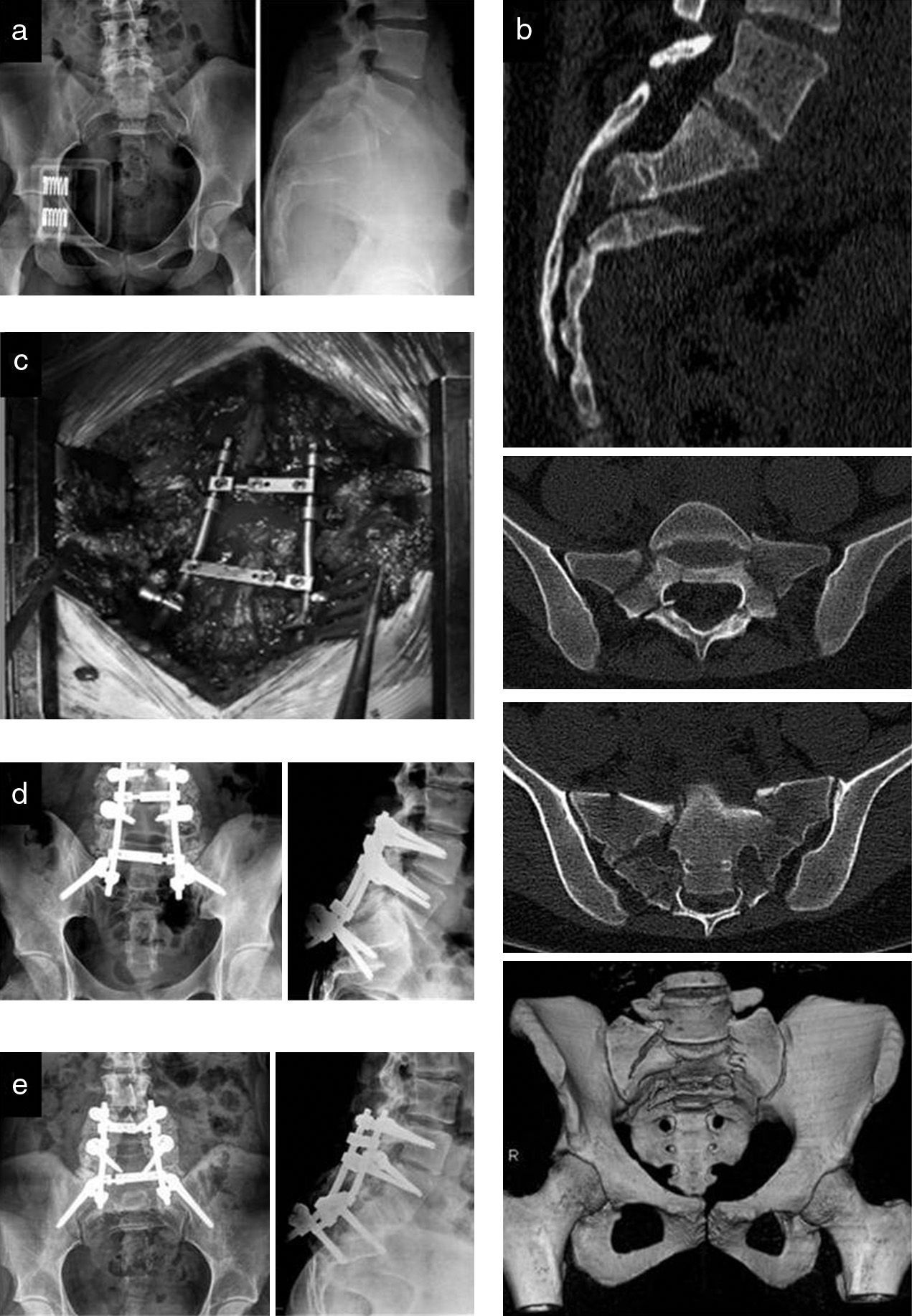
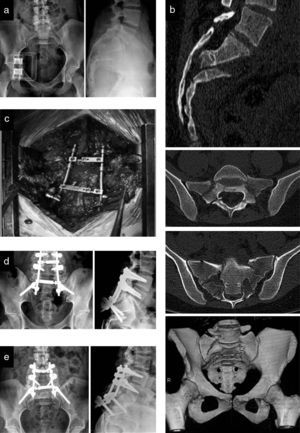
Images from a 24-year-old female patient who suffered an autolytic fall. (a) Simple radiograph showing a transverse sacral fracture with flexion and antepulsion of the distal fragment. (b) CT scan showing an H-shaped fracture of the sacrum with SP dissociation. She presented perineal hypoesthesia, fecal incontinence and urinary retention. The patient underwent surgery within 48hours of admission. (c) A bilateral, decompressive laminectomy, from L5 to S3, was performed by a direct posterior approach to the sacrum and last lumbar segments, as well as partial reduction of the fracture and SP fixation with L4, L5 and iliac pedicled screws and double longitudinal bars with transverse reinforcement. Since we achieved adequate decompression with this action and did not have complete control of the distal sacral fragment, we did not opt for complete anatomical reduction in order to avoid possible morbidity resulting from manipulation. We associated posterolateral arthrodesis with an iliac crest autograft. (d) Satisfactory postoperative radiographic control. (e) Control at 7 months after surgery, showing fracture consolidation and arthrodesis of the L4-S1 levels. In the annual control, the patient was able to walk without aids and pain, presenting residual perineal hypoesthesia and an acceptable sphincter control, although mild urinary dysfunction persisted.
Images from a 25-year-old male patient who suffered an accidental fall. (a) Plain radiographic images showing a transverse fracture of the sacrum with flexion and retropulsion of the distal fragment. (b) The CT scan showed a U-shaped fracture of the sacrum with SP dissociation. The patient presented mild paresis of the left lower limb and an adequate sphincter control. The patient underwent surgery within 48h of admission. Bilateral, decompressive laminectomy of the L4-S1 levels was performed by a posterior approach. As in the previous case, due to the appropriate decompression achieved and difficulty to control the distal sacrum, we chose to accept a partial reduction of the fracture. We conducted SP fixation with lumbar L3-L4 and iliac pedicled screws joined by longitudinal bars with a single cross brace. We associated a posterolateral arthrodesis with iliac graft. (c) Satisfactory postoperative radiographic control. (d) Control at 1 year after surgery showing fracture consolidation and fusion of the L3-S1 levels. In the annual control the patient was able to walk unaided, with moderate low back pain which could be related to the prominence of the osteosynthesis material. He also had complete control of sphincters.
The mechanism of injury includes a very high energy trauma with axial compression on the sacrum,3 which often occurs in falls from great heights and, on many occasions, with autolytic intent; in fact this entity was described as “suicidal jumper fracture” by Roy-Camille in 1998.4 Nevertheless, other mechanisms such as accidents, crushing or even gunshot injury5 have also been described.
Although the terms “U-shaped sacral fracture”6 and “H-shaped sacral fracture”,7 named thus because of the path of the fracture lines, have been used as equivalents we will see that these are strictly subtypes of sacral fractures with SP dissociation, as the shape of the sacrum fracture in the coronal plane is described according to the path and intersection of the transverse and sagittal fracture lines mentioned. Occasionally, this leads to forms other than the “U” and the “H”.
EpidemiologyThis type of sacral fractures is very infrequent. Therefore, the majority of published works correspond to isolated cases or small series.1,5,8–10 In a large series of 442 patients with pelvic ring disruption, Nork et al. noted only 13 cases of sacral fracture with SP dissociation, described as “U-shaped sacral fracture”, that is, only 2.9% of pelvic ring disruptions.2
Given the characteristics of the trauma necessary to cause this lesion, it is common for sacral fractures with SP dissociation to occur in multiple trauma patients with associated bone and visceral lesions, as well as a high mortality rate.1,3,4,6 In many cases, this leads to a delay in diagnosis – Roy-Camille et al. reported 5 delays in their series of 13 patients, 38%4 – and, probably, to a lack of diagnosis in critical patients who fail to regain consciousness.8 In these cases, late diagnosis is established through the appearance of suggestive symptoms once the general condition of the patient improves and/or there is a progression of the eventual neurological deficit. This is of great importance, as the delay in diagnosis and treatment of this entity is associated with a worse functional prognosis. Abdominal lesions are associated in up to 42% of cases, thoracic in 37%, head trauma in 21%, lower limb fractures in 63% and vertebral fractures in 47%.11
Out of these associated lesions, it is worth highlighting the high incidence of neurological lesions, ranging from incomplete monoradiculopathy to cauda equina. Schildhauer et al. found a prevalence of 56% neurological lesions,11 while Huittinen observed 35% of lumbar or sacral root sections for transverse sacral fractures.12 However, it should be noted that the small number of cases makes it difficult to establish generalizations regarding the frequency of neurological involvement in sacral fractures with SP dissociation.
ClassificationAs there is no specific classification for fractures of the sacrum with SP dissociation, other classification systems for sacral fractures13 are commonly used, such as those described, in chronological order, by Tile,14 Denis et al.,15 Isler,16 and Strange-Vognsen and Lebech17 as a modification of that proposed by Roy-Camille et al.4
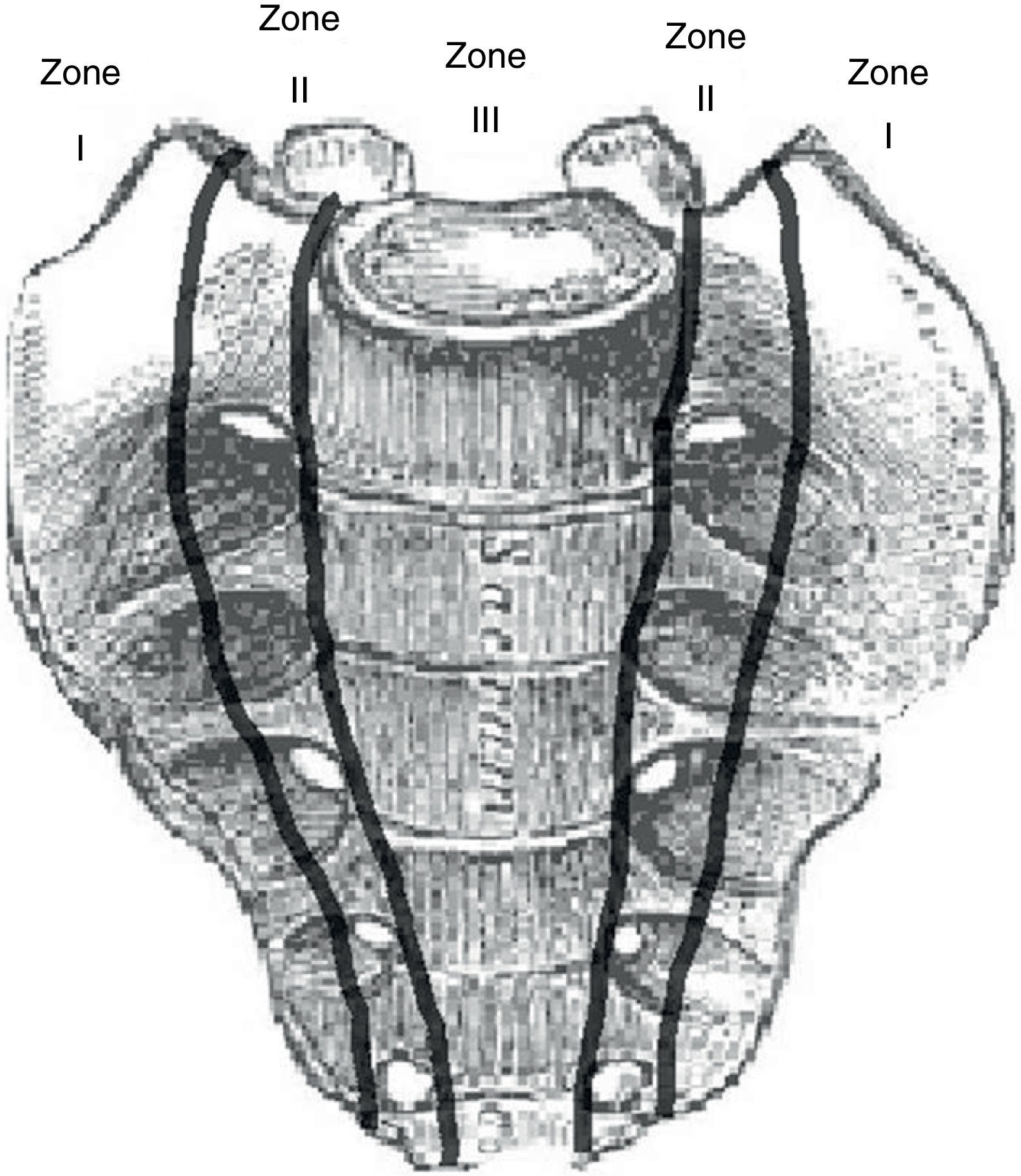
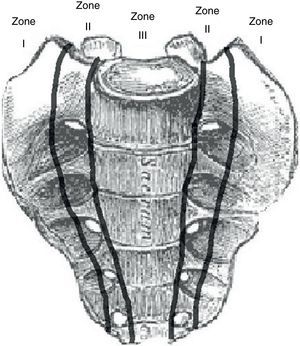
The classification of Denis is based on the relation between the fracture line and the sacral foramina in the coronal plane, distinguishing (Fig. 3):
- •
Type I: transalar with the line being lateral thereto.
- •
Type II: transforaminal.
- •
Type III: central, with the line being medial to the sacral foramina.
This classification has prognostic value, with the risk of neurological injury increasing progressively from type I to type III. Sacral fractures with SP dissociation behave like a Denis type III, as their fracture line involves the central canal of the sacrum. Therefore, the use of letters which resemble the lines of transverse and sagittal fractures, such as “H”, “U”, “T” and “Y”,6 has been proposed to complete the description of the fracture in the coronal plane, (Fig. 4). Fracture lines in “H” and “U” shapes are the most common, and the term “H-shaped/U-shaped sacral fracture” has been used as an equivalent to the concept of sacral fracture with SP dissociation, although they only represent one of the ways in which dissociation can occur.
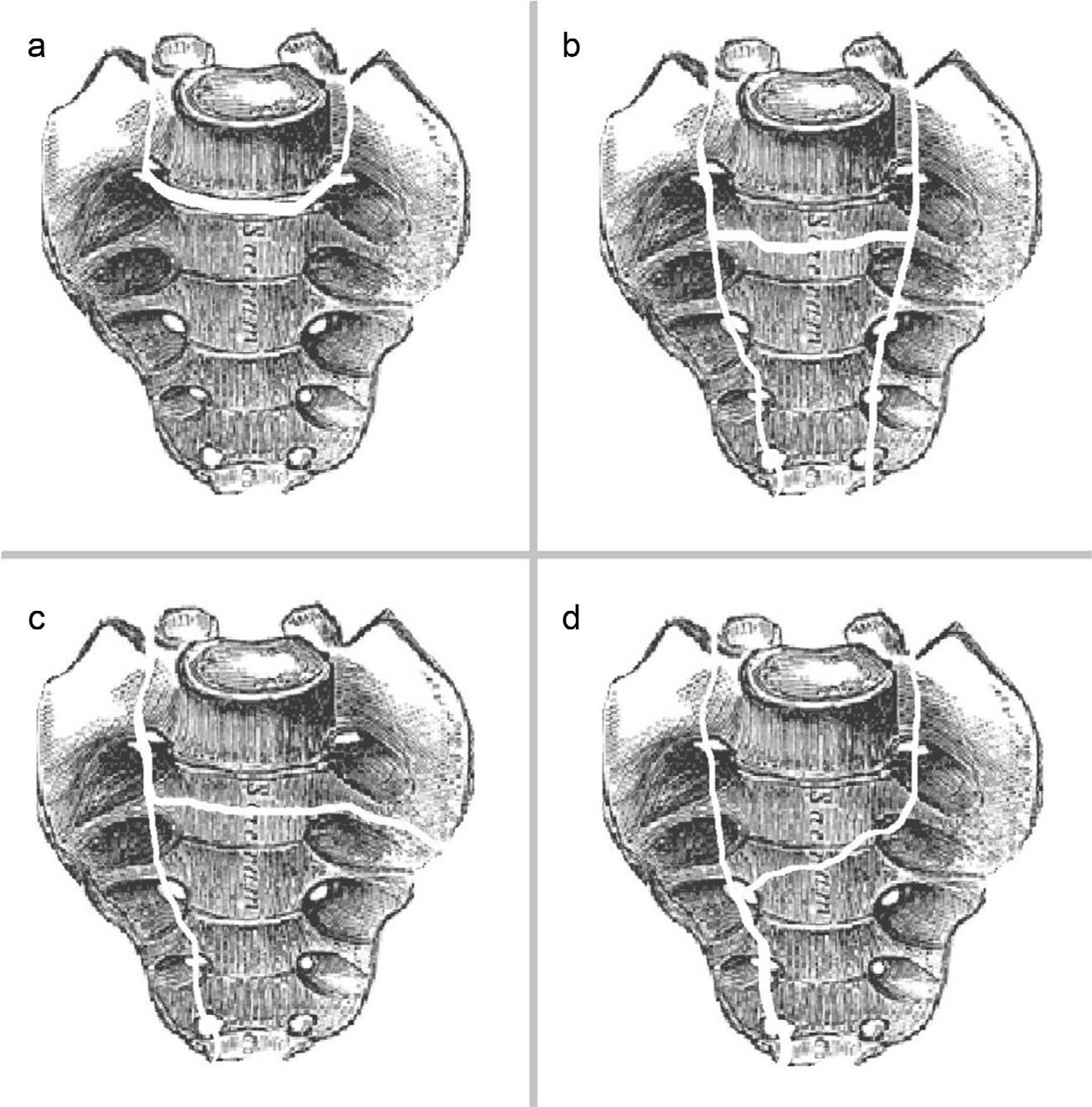
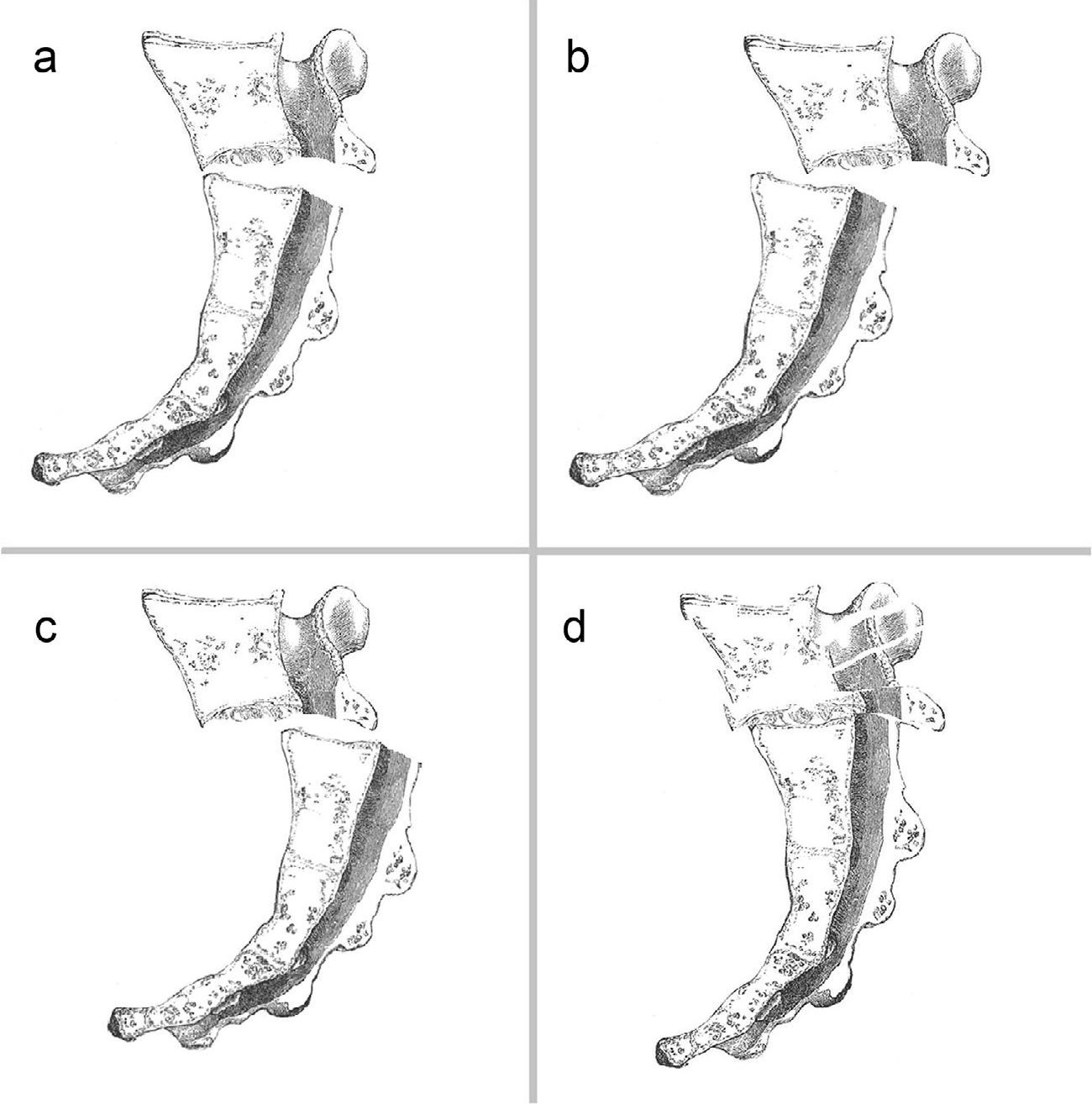
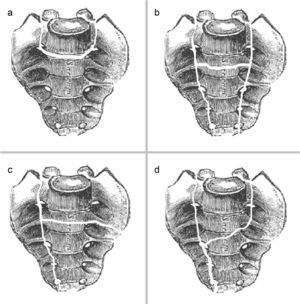
The Roy-Camille classification modified by Strange-Vognsen and Lebech is often used to refer to displacement in the sagittal plane. This distinguishes 4 types, with the first 3 described by the position of the distal fragment relative to the proximal (Fig. 5):
- •
Type I: angulation in kyphosis, without displacement.
- •
Type II: angulation with anterior partial displacement.
- •
Type III: angulation with full displacement.
- •
Type IV: segmental comminution of the S1 vertebral body.
Modified Roy-Camille classification. Relationship between sacral fragments in the sagittal plane. (a) Type I: angulation in kyphosis without displacement. (b) Type II: angulation with partial anterior displacement. (c) Type III: angulation with complete displacement. (d) Type IV: S1 segmental comminution.
Additionally, a further type 5 is described, corresponding to lower sacral fractures, with less morbidity.18
Clinical assessmentGiven the risk of delayed diagnosis, clinical examination is particularly important. Since these patients usually suffer multiple trauma, initial care should follow the Advanced Trauma Life Support (ATLS) or similar protocol, ensuring airway, breathing and hemodynamic monitoring before performing an examination of neurological, visceral and locomotor damage.19
Whenever possible, an anamnesis regarding the mechanism of injury, location of pain and other symptoms in the pelvis or lower limbs should be obtained. In many cases this cannot be done until the patient has recovered sufficiently, so we must maintain a high level of suspicion. The examination should be conducted in a thorough and systematic manner in all cases: pelvic ring stability must be assessed through slight rotational forces (log-roll maneuver),20 and areas of crepitus, edema and hematoma should also be sought. Even with a high level of suspicion of sacral fracture it would be appropriate to perform a rectal exam – and vaginal, in women – to rule the possibility of an open fracture with perforation of the rectum and/or vagina. On the other hand, a complete neurological examination should be conducted, in order to rule out lesions at the level of the last lumbar and sacral roots, including the cauda equina. Thus, although exploring the lower limbs for possible L4, L5 and/or S1 damage is a necessity, we must not forget that there will be no clear motor deficit due to the presence of neurological damage at a lower level, making it is essential to seek possible bladder weakness, decreased tone of the anal sphincter and saddle and/or limb hypoesthesia or anesthesia, to guide our suspicions. Moreover, we must not forget that these neurological symptoms could be masked by the initial trauma.13 When neurological deficit is identified, it is usually classified according to the neurological scale of Gibbons et al.,21 which distinguishes the following grades:
- •
Grade 1: no neurological lesion.
- •
Grade 2: paresthesias.
- •
Grade 3: paresis in lower limbs.
- •
Grade 4: sphincter deficit.
Although the performance of a pelvic anteroposterior projection is covered by all multiple trauma protocols,22 we should take into account that their sensitivity to detect a sacral fracture is estimated at only 30%.6 Nevertheless, the possible onset of so-called “stepladder sign” has been described as an indicator of disruption of the anterior sacral foramina,23 and the existence of a fracture in the L5 transverse process has also been identified as a possible indirect indicator of sacral fracture.15 This anteroposterior projection should be complemented by inlet and outlet pelvic views and, especially, by a lateral sacral projection, which clearly reveals the transverse fracture line.
Performing a CT scan of the spine and pelvis which enables a better understanding of the fracture pattern and facilitates decision-making regarding treatment is mandatory in the study of these diseases.24 Obtaining sections in the sagittal and coronal planes is especially advisable, as it allows us to classify the fracture according to the previously described classifications.
Lastly, MRI studies can provide relevant information which helps to identify nerve compression areas, as well as displacement of the fragments, but their limited availability compared to CT make them less useful in emergency care.
Initial treatmentThis would consist in damage control, according to the ATLS protocol or similar,19 followed by a provisional stabilization of the pelvis, especially in the context of Tile type C pelvic fractures with rotational and vertical instability.25,26
No advantages associated with any type of temporary fixation, among those commonly described for pelvic fractures,27 has been described in cases of sacral fractures with isolated SP dissociation.
Definitive treatmentConservative treatment was used in the past because surgery could only offer a limited capacity for fracture reduction and stabilization.28,29 However, it currently finds few applications. Consisting of bed rest with traction of the lower limbs, it is almost justified in patients in whom surgery is contraindicated by severe comorbidities. Even in patients without neurological damage and scarcely displaced fractures, surgical treatment with stabilization thereof would enable early mobilization, thus decreasing the morbidity and mortality derived from bed rest and improving long-term functional outcomes in multiple trauma patients.11
Therefore, the standard is surgical treatment with decompression of the neural elements and reduction and stabilization of the lesion. Stabilization aims to avoid prolonged bed rest, to enhance neurological decompression, and to correct or prevent any displacement that could alter the sagittal axis and cause chronic pain or nerve compression. Although there is no categorical indication for the periods, the recommendation is to perform this surgery in the first 24–72h, in order to maximize the capacity for recovery from neurological damage.30 Nevertheless, earlier treatment would be advisable in case of onset of cauda equina.
Decompression is performed directly through the removal of bone fragments from the fractured plate, performing as wide a laminectomy in the sacrum as necessary. Moreover, achieving reduction of the fracture can increase indirect decompression by restoring the natural anatomy.
Various direct and indirect maneuvers have also been described for the reduction, such as placing a Schanz screw in the superocentral sacrum to enable direct reduction and manipulation of this fragment and/or the use of Schanz screws with a distal thread in both iliac wings, acting as a lever or joystick, to perform indirect manipulation.30 In any case, in the process of reduction it is very important to restore SP alignment, both in the coronal and in the sagittal planes. While the first is usually adequately achieved through controlled manipulation and fluoroscopy control, sagittal realignment often entails significant difficulties: as there is no intact cortical bone in the sacral wings to guide the reduction, in many cases aligning the proximal and distal fragments of the sacrum does not guarantee their reduction regarding the sacral wings. To minimize these problems, Vresilovic et al.10 recommend the use of a fluoroscope to control the sagittal axis when positioning the patient on the operating table, with subsequent confirmation before internal fixation. For their part, Hart et al.7 described pelvic incidence – a parameter historically described in spondylolisthesis to determine pelvic orientation and SP balance31 – as a helpful tool in their experience. Pelvic incidence is defined as the angle obtained by crossing a line perpendicular to the midpoint of the S1 upper plate, with another from that point to the center of the femoral heads (or midpoint between the two, in cases where they do not overlap). Knowing or inferring the pelvic incidence of a patient prior to the trauma is helpful to guide anatomical reduction and also to retrieve sagittal balance, which is very important to obtain a good functional result. We must again point out that achieving a complete anatomical reduction can be difficult, as it is often not possible to ensure adequate control of the distal sacral fragment. Any manipulation should always be carried out with maximum guarantees, in order to avoid iatrogenic injury. Ultimately, we must not forget that the bases of treatment are decompression and stabilization, with a perfect anatomical reduction remaining as an ideal, albeit secondary, objective.
The very anatomy of the sacrum on the one hand, and the fracture lines on the other, create an unfavorable environment for an appropriate direct osteosynthesis in the sacrum, which in the past has led some authors to advocate a non-surgical treatment of fractures at this level.32 Harrington rods, iliosacral screws, transiliac rods or plates and transsacral plates have been used for this purpose in the past.
In biomechanical terms, such techniques have been rendered obsolete by SP fixation systems,33 which have become the standard. These assemblies include solid lumbar fixation with pedicled screws at multiple levels, reinforced by bars with iliac screws placed at the level of the posterosuperior iliac spine. Although it is possible to achieve adequate fixation with a single screw in each iliac wing, some biomechanical studies have demonstrated the superiority of using 2 screws.34 Nevertheless, their placement is probably technically more difficult and may increase the problems caused by prominence of the osteosynthesis material.
SP fixation discharges the lesion area, bypassing normal load transmission generated from the acetabulum to the lumbar spine through sacroiliac joints,30,33,35,36 thus achieving adequate vertical stability. However, this construct offers a worse control of rotational instability,37 which is frequent in this type of lesions. In order to improve stabilization a cross connector can be added or a triangular osteosynthesis system can be used which adds iliosacral screws or a transsacral bar to lumbosacral fixation.31,38
In specific cases of non-displaced fractures with a U-shaped coronal morphology and without neurological involvement, Nork et al.2 described good results through the use of percutaneous iliosacral screws. Nevertheless, this technique would not be indicated for unstable, displaced, comminuted and closed irreducible fractures.10,30 Moreover, certain limitations have been identified, such as the scarce reach of single iliosacral screws in a comminuted sacrum, their inability to stabilize the sagittal deformity and the possibility of causing iatrogenic neurological damage through eventual compression or occupation of the sacral foramina.28
Results and complicationsThe short-medium term results published following treatment of sacral fractures with SP dissociation are highly conditioned by the frequent and severe comorbidities associated. Moreover, the scarcity and complexity of these lesions make it difficult to draw conclusions with a sufficient level of evidence to recommend an optimal treatment. Therefore, it is preferable to assess the long-term results, taking the residual neurological deficit as the key determinant of the quality of life of patients.6
Following a chronological order, in 1991, Phelan et al.32 described neurological improvement around 80% in transverse sacral fractures with nerve damage treated conservatively. This percentage is comparable to that reported with surgical treatment.39 However, in 2004, Vaccaro et al.23 predicted a poor prognosis when there was bilateral avulsion or section of roots, and a considerable potential improvement with reduction, decompression and surgical fixation in cases of nerve compression damage. Meanwhile, in 2006, Schildhauer et al.30 reported complete recovery of sphincter function in up to 86% of patients with integrity of the nerve roots, and only 36% in cases with at least 1 sectioned root.
The work published in 2008 by Dussa and Soni40 represents the only study of which we are aware that compares surgical vs. conservative treatment in transverse sacral fractures. The authors concluded that there was no evidence of the superiority of surgical treatment in terms of recovery of sphincter control. This work defined indirect data – severe angulation or displacement of the fracture – as well as direct data – neurotmesis – of severe neurological damage, as predictors of a poor outcome, regardless of the treatment performed.
In relation to quality of life after these lesions, in 2009, Gribnau et al.29 published a review of 8 patients with U-shaped sacral fracture with SP dissociation, in whom the EuroQoL-6D questionnaire was used, concluding that the influence of surgical treatment on long-term morbidity was scarcely assessable by the associated lesions and derivative psychiatric disorders. All the patients in this series appeared capable of performing self-care and basic activities of daily living.
The consolidation of the fracture does not seem to be a problem, at least in the surgical series consulted, with excellent union rates for both the mentioned percutaneous technique by Nork et al.,2 and for open triangular osteosynthesis, as in the series of Schildhauer et al.33 However, a solid but vicious consolidation, due to an incomplete reduction or insufficient fixation of the fracture, may influence development in the sagittal plane of lumbosacral kyphosis, which in turn could lead to lumbar hyperlordosis and/or compensatory flexion of hips and knees (sagittal imbalance),7 hindering the functional outcome.
The frequent association of extensive soft tissue damage does seem to condition a relatively high rate of surgical wound complications. In a series of 19 patients, Bellabarba et al.3 described 1 hematoma, 1 seroma and 3 wound infections, in all cases requiring revision surgery.
Finally, we must highlight the complications derived from iliac screw prominence. The incidence was not quantified but they were considered frequent6 and they may cause problems ranging from simple discomfort to pressure ulcers and superinfection, especially in multiple trauma patients who experience loss of adipose tissue and prolonged bed rest. In an attempt to minimize this problem, Schildhauer et al.30 recommended using an entry point as medial as possible for the introduction of iliac screws, as well as burying the head thereof using a countersink or bore tool.
ConclusionsSacral fracture with SP dissociation is a rare, but often underdiagnosed entity. It is therefore essential to maintain a high level of suspicion in multiple trauma patients, especially when due to high falls. A detailed neurological examination of the lumbar and sacral roots should always be conducted, and supplemented by radiographic projections including AP, inlet and outlet of the pelvis and, inexcusably, a lateral sacral projection, as well as an urgent CT or MRI scan if any pathological findings are identified. It is important to remember the conceptual description of sacral fracture with SP dissociation in order to distinguish it from other entities, as well as the Denis, Roy-Camille and morphological classifications, to obtain a better understanding of the fracture. Although the small number of cases prevents us from gathering strong evidence, there is consensus on the superiority of surgical treatment for the management of these patients, as it enables neurological decompression, as well as reduction and fixation of the fracture to facilitate early mobilization. This treatment should be implemented in an urgent, deferred manner, within the first 2 or 3 days, once the lesion has been characterized and provided the general condition of each patient allows it, although a progression of the neurological deficit could determine emergency surgery. During the procedure, it is important to achieve an adequate reduction in the sagittal and coronal planes. Regarding fixation, there seems to be evidence pointing to a superiority of SP stabilization, combining lumbar pedicular fixation with iliac fixation. Moreover, performing a triangular osteosynthesis seems to increase rotational stabilization. The short-term outcome is closely dependent on patient comorbidity. We can expect a high frequency of local complications, both of the surgical wound and caused by the osteosynthesis material. The medium-long term results are significantly influenced by the presence of neurological sequelae. Other factors that may influence the final result are the lack of consolidation, residual deformities and loosening of the osteosynthesis material.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Cearra I, Alonso R, Martínez-Ogalla D, Hoyos J, Lauzirika A, Mongil R, et al. Fractura de sacro con disociación espóndilo-pélvica. Revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2013;57:434–442.