The concept "subtle Lisfranc" defines low energy lesions of the tarsometatarsal joint complex (TMC) that involve joint instability. Often unnoticed, with long-term sequelae.
The objective is to evaluate the clinical-functional results of patients with MTC ligament damage grade II-III (Nunley and Vertullo classification) treated with percutaneous surgery.
Material and methodsRetrospective study of 16 patients who underwent percutaneous surgery for MLC ligament damage. Demographic data, days of delay in diagnosis, surgical technique, joint reduction in load (adequate if C1-M2 space is less than 2 mm) and Manchester-Oxford scale (MOXFQ) score were collected. The sample consisted of 9 males and 7 females, mean age 43.6 years (17–71) and mean follow-up of 22 months (12–28).
ResultsDiagnosis was delayed for more than 24 h in 4 patients (3–6 days). In 11 patients the treatment consisted of closed reduction and percutaneous synthesis with cannulated screws from M2 to C1 and from C1 to C2. In 3 patients it was supplemented with Kirschner wires in the lateral radii. 2 patients were treated with only M2 to C1 screws. An anatomical reduction was not achieved in 6 patients, with a mean of 2.6 mm between C1-M2 (2.1−3 mm); the mean functional MOXFQ score of these patients was 41.1% (IC95% 23.1%–59.1%), worse results compared to the anatomical reduction: 17.2% (IC95% 5.7–28.7); statistically significant difference (p < 0.01).
ConclusionSubtle injuries from MTC are rare and can go unnoticed. Surgical treatment with percutaneous synthesis offers good clinical-functional results in the medium term. The anatomical reduction is a determining factor for the good functional result of our patients.
El concepto “Lisfranc sutil” define lesiones por baja energía del complejo articular tarso-metatarsiano (CTM) que suponen inestabilidad articular. Con frecuencia desapercibidas, con secuelas a largo plazo.
El objetivo es evaluar los resultados clínico-funcionales de los pacientes con lesión CTM ligamentosas grado II-III (clasificación de Nunley y Vertullo) tratados con cirugía percutánea.
Material y métodosEstudio retrospectivo sobre 16 pacientes intervenidos percutáneamente por lesión ligamentosa CTM. Se recogieron datos demográficos, días de demora del diagnóstico, técnica quirúrgica, reducción articular en carga (adecuada si espacio C1-M2 menor de 2 mm) y puntuación de la escala Manchester-Oxford (MOXFQ). Muestra constituida por 9 varones y 7 mujeres, edad media de 43,6 años (17-71) y seguimiento medio 22 meses (12-28).
ResultadosEl diagnóstico se demoró más de 24 horas en 4 pacientes (3-6 días). En 11 pacientes el tratamiento consistió en reducción cerrada y síntesis percutánea con tornillos canulados desde M2 a C1 y desde C1 a C2. En 3 pacientes se suplementó con agujas Kirschner en los radios laterales. 2 pacientes se trataron con único tornillo M2 a C1. No se consiguió una reducción anatómica en 6 pacientes, con una media de 2,6 mm entre C1-M2 (2,1-3 mm); la puntuación media funcional MOXFQ de estos pacientes fue 41,1% (IC95% 23,1-59,1%), peores resultados comparando con la reducción anatómica: 17,2% (IC95% 5,7-28,7); diferencia estadísticamente significativa (p < 0,01).
ConclusiónLas lesiones sutiles del CTM son poco frecuentes y pueden pasar desapercibidas. El tratamiento quirúrgico con síntesis percutánea ofrece buenos resultados clínico-funcionales a medio plazo. La reducción anatómica es un factor determinante para el buen resultado funcional de nuestros pacientes.
The tarsometatarsal joint complex (TMC) is formed by the intermetatarsal, tarsometatarsal and distal intertarsal joints. The Lisfranc ligament, which connects the M2 base with the medial cuneiform, is the main fibrous structure that provides stability to the complex, along with the plantar ligaments.1
The TMC can suffer a wide spectrum of injuries, from small avulsions of the Lisfranc ligament with opening of the first intermetatarsal space, to major tarsometatarsal joint incongruence in the context of high energy trauma. In general, they have an incidence of 1/55,000 people per year in the USA, and are more frequent in men.2 Up to 20% of TMC injuries go unnoticed at the first consultation3; these undiagnosed and initially treated lesions usually progress to collapse of the plantar arch with painful midfoot osteoarthritis.4 Diagnostic suspicion and early treatment maintaining tarsometatarsal joint congruence are fundamental for good functional clinical outcomes in these patients.
The term subtle Lisfranc refers to TMC injuries with joint disruption between M1 and M2, which may also affect the intercuneiform joints and/or navicular-cuneiform joints. In general, they are produced by low energy trauma, which represents up to 30% of TMC injuries.2 Subtle injuries are the most frequently under-diagnosed, but they can also evolve into painful osteoarthritis.
The aim of this paper is to evaluate the clinical-functional results of patients with grade II-III injuries of the tarsometatarsal joint complex according to the Nunley and Vertullo3 classification, treated with percutaneous surgery.
Material and methodsTo prepare this paper, we compiled a total of 36 patients who underwent surgery in our centre for injuries to the tarsometatarsal joint complex (TMCI) diagnosed by CT between May 2016 and November 2018. Patients with associated fractures of tarsal and/or metatarsal bones (except avulsion fracture or fleck sign), and patients treated with open reduction and fixation with osteosynthesis plate were excluded from the study. The final sample was reduced to 16 patients who met the inclusion criteria: diagnosis of subtle MTC injury, grade II-III of the Nunley and Vertullo5 classification, and percutaneous surgical treatment with cannulated screws. We collected demographic data, days of delay in diagnosis, C1-M2 joint space measured in mm by two independent observers, surgical technique performed, postoperative joint reduction on weightbearing control radiographs three months after surgery (adequate if C1-M2 space less than 2 mm), and validated Manchester-Oxford Foot Questionnaire score 12 months after surgery6 (MOXFQ: the lower the percentage, the better the clinical-functional outcome). The data were collected and analysed using Microsoft Excel® (Microsoft, Inc, Redmond, WA) and SPSS® (IBM Corporation, Armonk, NY) software, assuming 95% confidence intervals.
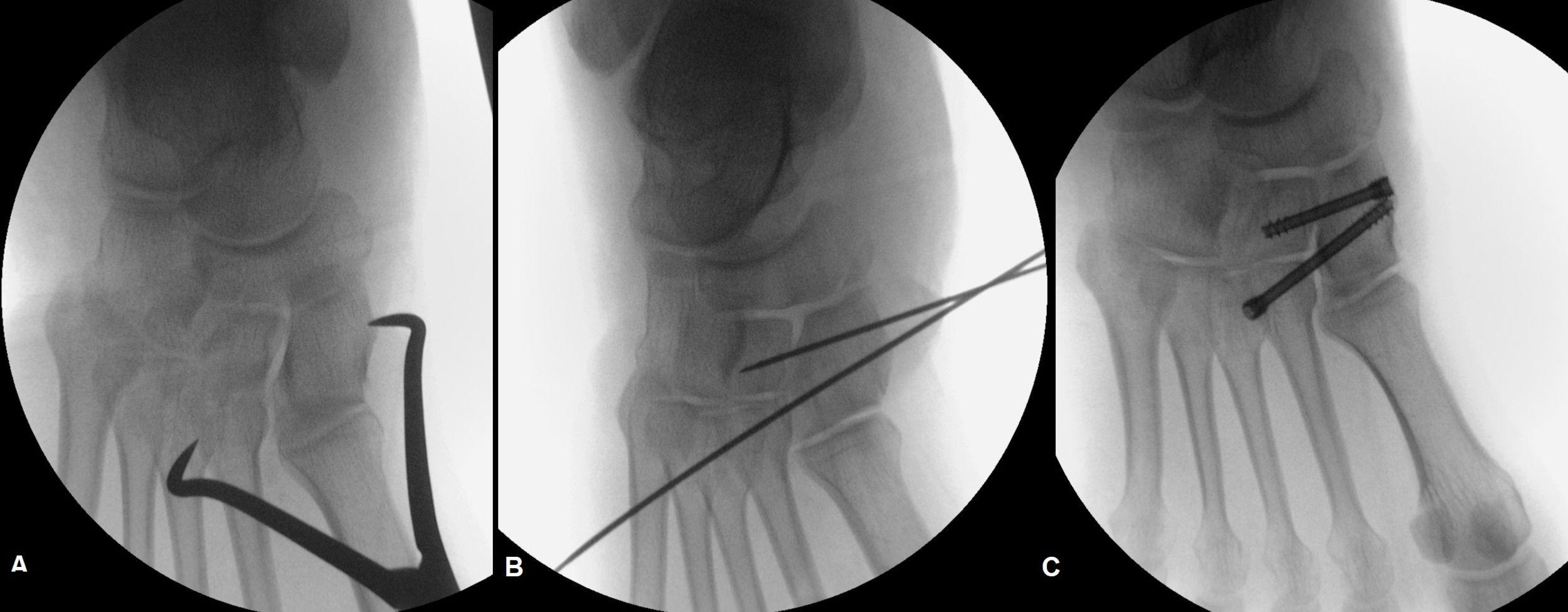
Diagnostic protocol and surgical techniquePatients are initially evaluated with non-weight-bearing AP and oblique X-ray in the emergency department, where the diagnosis of suspected MTC injury is confirmed with a computed tomography (CT) scan, which allows the evaluation of joint diastasis between M1 and M2, as well as the identification of other associated injuries and fractures unnoticed on the initial X-ray (Fig. 1). If the initial suspicion is low, the patient is immobilised and re-evaluated on an outpatient basis with a weight-bearing X-ray and/or CT scan (Fig. 2).
All the patients with MTC ligament injury were operated with closed reduction under control with portable X-ray and percutaneous fixation, performed by the same team of surgeons. Under intrathecal anaesthesia, the diastasis between the medial cuneiform (C1) and the second metatarsal (M2) is checked by means of intraoperative simulated weight-bearing radiographic control, revealing the instability of the injury. Closed reduction is performed with the help of a clamp and under control with portable radiography; once the joint reduction is achieved, fixation is performed with a 4.5 mm cannulated screw from M2 to C1, avoiding over-compression (Fig. 3). Additionally, the C1-C2 joint is fixed with a 4.5 mm cannulated screw when significant instability of the C1-C2 space is observed intraoperatively. The screws we use are steel, cannulated 4.5 mm screws with a threaded head and partial thread HCS - Headless Compression Screw® (HCS, Synthes Inc, West Chester, PA, USA). This double-screw fixation can be supplemented with Kirschner wires in the external spine to protect the joint for a period of three weeks, according to the surgeon's preference.
Patients are kept non-weight-bearing for a minimum of six weeks, and then protected weight-bearing with a brace is started gradually. At 12 weeks after the operation, usual footwear with a plantar arch reinforcement insole is allowed. Sports activity is gradually resumed after six months. We do not routinely remove the material in our patients, only in those presenting discomfort after at least six months following the intervention.
ResultsWe present a total sample of 16 patients, of which nine were male and seven female; the mean age was 43.6 years (17–71); 10 injuries occurred on the left side and six on the right. In all cases the injury was due to a low energy mechanism, without associated fractures in the foot that would have required additional treatment.
The diagnosis of suspected TMCI was confirmed in all patients by confirming joint diastasis between M1 and M2 on CT images. Two patients underwent outpatient X-ray prior to the CT scan. In four patients the diagnosis was delayed for more than 24 h, with an average of 3.2 days (range 3–6); the two patients in whom weight-bearing X-rays were performed were part of this group. The average time from injury to surgery was 7.3 days (range).
Eleven patients were treated with closed reduction and percutaneous synthesis with two cannulated screws, one directed from M2 to C1 and the second from C1 to C2. In three patients this double screw fixation was supplemented with Kirschner wires in the external spine, according to the surgeon's preference, to protect the tarsometatarsal joint from the lateral radii, which had also received trauma. In two patients, only one screw was implanted from M2 to C1 since the stability of the C1-C2 space was confirmed with intraoperative simulated weight-bearing radioscopic control.
A mean space between the base of the second metatarsal and the first cuneiform (M2-C1) of 3.2 mm (range 2.3–4.5) was observed, measured with preoperative non-weight-bearing X-ray, with a moderate correlation index between two independent observers (K .66).
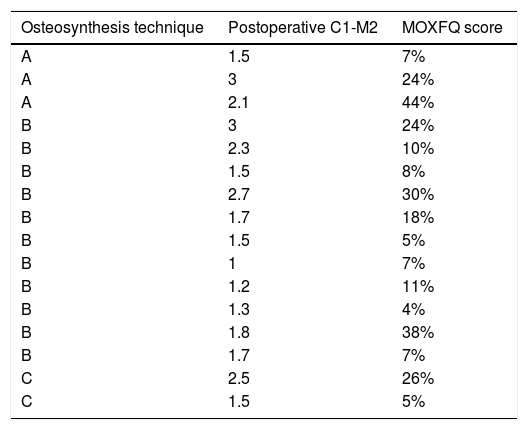
All the patients were followed-up clinically in consultation, with a mean of 22 months (range 12–28) (Fig. 4). The mean total MOXFQ score at 12 months was 26.2% (6.3%-68.7%). An anatomical reduction (M2-C1 less than 2 mm) was not achieved in six patients, of whom the mean MOXFQ was 41.1% (95% CI 23.1%-59.1%). The mean MOXFQ score was higher in this group compared to those in whom an anatomical reduction was achieved (17.2%: 95% CI 5.7–28.7), this difference being statistically significant (p < .01) (Table 1).
60-year-old male, with subtle TMC injury; MOXFQ score at 12 months of 5 points. A). Preoperative non-weight-bearing X-ray note fleck sign visible between M2 and C1. B) Postoperative control radiography. C) Post-surgical weight-bearing radiography at 12 weeks after the intervention.
Relationship between surgical technique used, C1-M2 space and MOXFQ score in each of the patients included.
| Osteosynthesis technique | Postoperative C1-M2 | MOXFQ score |
|---|---|---|
| A | 1.5 | 7% |
| A | 3 | 24% |
| A | 2.1 | 44% |
| B | 3 | 24% |
| B | 2.3 | 10% |
| B | 1.5 | 8% |
| B | 2.7 | 30% |
| B | 1.7 | 18% |
| B | 1.5 | 5% |
| B | 1 | 7% |
| B | 1.2 | 11% |
| B | 1.3 | 4% |
| B | 1.8 | 38% |
| B | 1.7 | 7% |
| C | 2.5 | 26% |
| C | 1.5 | 5% |
Technique A: cannulated M2-C1, cannulated C1-C2 and Kirschner wires in the external spine. Technique B: cannulated M2-C1 and cannulated C1-C2. Technique C: only cannulated in M2-C1. Note: the outcomes are considered better the lower the MOXFQ score.
The complications described were three cases of mild complex regional pain syndrome that improved with rehabilitation treatment. Only one of the patients required removal of the material, due to loosening of the C1-C2 screw, after 12 weeks following implantation; the rest of the patients did not present discomfort subsidiary to the removal of material during follow-up.
During the subsequent clinical follow-up, the good initial progress of the patients was maintained, without the need to remove the material due to discomfort, nor the appearance of new complications. Apart from one, all the patients returned to their previous physical and work activities.
DiscussionTMC injuries are generally produced by an axial load mechanism with the foot in plantar flexion, which generates an overload at the base of the second metatarsal, the cornerstone of the plantar vault.4 In high-energy trauma, major injuries occur with significant involvement of soft tissue and bone structures, which are easily identifiable on X-rays. This mechanism of plantar flexion and load can occur in low energy situations, which also generates an energy overload at the base of the second MTT and which can result in failure of the capsulo-ligamentous structures, giving rise to instability at the level of the TMC.4 It is not uncommon for this type of injury, caused in the context of minor trauma, to go unnoticed and be classified as ankle sprains, which explain the resulting swelling at foot level.
Clinical suspicion is the main tool available to us for the diagnosis of these injuries. In any case, it is mandatory to take AP and oblique X-rays of the foot, which in the case of subtle injuries can appear normal and lead to diagnostic error. Several radiological signs have been described on non-weight-bearing radiographs that alert us to subtle TMC injuries7: fleck sign, disruption of C2-M2 continuity, either dorsal or medial,8 C1-M2 diastasis greater than 2 mm,9 C1-C2 diastasis and M1-C1 subluxation. In our study, retrospectively, the M2-C1 space was measured by two independent observers, obtaining a mean value of 3.2 mm (range 2.3–4.5), with a moderate correlation index between observers (K .66); therefore it seems that this is a measurement that has its limitations and is not free of error when taken as a benchmark to establish diagnosis. Weight-bearing or stress X-rays to check for joint diastasis are a diagnostic alternative10; in this case, the radiological signs to be taken into account in weight-bearing X-rays are similar to the abovementioned, and allow the identification of subtle injuries that remain reduced non-weight-bearing and are not diagnosed initially.11 However, this is a test that is not available in all emergency departments, and is painful and not well tolerated by the patient, giving rise to error.5 Therefore, It should be performed with adequate pain control with local anaesthesia or trunk block. CT is also useful for the diagnosis of subtle TMC injuries, since it allows the identification of joint incongruities, small avulsion fractures (fleck sign) and associated tarsometatarsal fractures, which go unnoticed on conventional X-rays.11,12 For this reason, and in view of the impossibility of carrying out X-rays in our centre’s emergency department, in all cases of clinical suspicion of TMC injury we carry out a CT scan to confirm the diagnosis at the patient’s first visit to the emergency department. In our series, we have four patients where the diagnosis was delayed beyond the first consultations, by an average of 3.2 days. In these cases, the initial suspicion was low and no complementary CT study was performed initially; two were re-assessed in the emergency department with CT due to the persistence of symptoms and the remaining two were assessed in consultations, where weight-bearing X-rays were performed, prior to confirming the diagnosis with CT. Subtle TMC injuries are classified following the scheme proposed by Nunley and Verullo,5 which establishes three groups according to findings on weight-bearing radiography of the foot. Eleftheriou and Rosenfeld in a later modification of this classification, maintaining the same stages, include CT as a diagnostic test, including in type II patients with any degree of tarsometatarsal diastasis of the first space diagnosed by CT.13 All the patients in the series were diagnosed by CT, where a joint diastasis with absence of associated fracture of the TMC was found, except for the presence of fleck sign, and therefore we can affirm that all of them presented a subtle TMC injury of Eleftheriou and Rosenfeld type II or Nunley and Vertullo type II-III. In our opinion, CT is an excellent diagnostic tool for subtle lesions of TMC, especially to detect the presence of fleck sign, so characteristic of type II ligamentous injuries, and it can be a quick and painless alternative, available in the emergency department, unlike weight-bearing X-rays.
The aim of treatment is to restore the functional anatomy of the TMC, key to achieving good outcomes.8 High energy injuries with great instability have been treated with open reduction and transarticular synthesis with cannulated full thread screws,10 which is not free from complications due to exposure and soft tissue injury.2 This is why authors increasingly recommend the use of less invasive closed reduction and fixation techniques either by means of cannulated screws14–16 or percutaneous plates.17 Dynamic fixation systems are also being postulated as an alternative to classical cannulated screws, proving to be biomechanically comparable.18 Treatment by means of a dorsal plate also enables restoring the stability of TMC without damaging the joint surface, but it implies greater dissection and aggression to soft tissues.19 Primary arthrodesis, traditionally reserved as rescue for failed osteosynthesis, has also shown comparable results with respect to open reduction and internal fixation with cannulated screws, in complex TMC injuries. In all the patients in the study, closed reduction and percutaneous fixation with cannulated partially threaded screws without over- compression, HCS - Headless Compression Screw (HCS, Synthes Inc, West Chester, PA, USA), was performed; the most important screw is the one that supplements the function of the Lisfranc Ligament, between C1 and M2. In addition, we use another screw of similar characteristics between C1 and C2 to increase the stability of the assembly and to ensure correct reduction of the first tarsometatarsal space; a recent study indicates that up to 50% of subtle, low-energy injuries of the TMC in athletes, involve the C1-C2 joint proximally, recommending its fixation either with one or two cannulated screws, or a plate if the tarsometatarsal instability is frank.20 In our series, in two patients, C1-C2 fixation was not considered necessary because adequate stability was confirmed once the screw was implanted between M2 and C1. In three cases additional stability was provided in the external spine with KW, this decision was taken intraoperatively at the surgeon's preference and once the medial spine was fixed, with the intention of protecting the lateral radii, which had also been subjected to trauma, although this does not affect their stability. The KWs were removed three weeks after the operation on an outpatient basis.
We do not routinely remove the cannulated screws from the medial spine, except for discomfort due to the material six months after the intervention. Thus far, this has not been necessary in any of our patients, except in one case that presented osteolysis around the C1-C2 screw on starting weight-bearing with usual footwear (12 weeks postoperatively). There is no consensus in the literature on the indication for routine implant removal, which depends on the patient's discomfort and the surgeon's preference, and never earlier than four months after the intervention.14,21
According to Myerson et al., joint reduction should be considered satisfactory when the M2-C1 space is less than 2 mm8; in our series we achieved six cases where the reduction was not anatomical, and in which the mean MOXFQ was 41.1% (95% CI 23.1%–59.1%). These results were significantly worse than those obtained among patients in whom an anatomical reduction was achieved (mean MOXFQ of 17.2%: 95% CI 5.7–28.7): p < .01. As previously mentioned, in our series we found three different configurations of osteosynthesis, the majority being the group with double screw (M2-C1 and C1-C2); the results obtained in terms of MOXFQ functional assessment are heterogeneous in the patients of the three groups. The series we present is a small sample, with groups not sufficiently comparable to draw relevant conclusions; in any case, it seems that functional outcome can be related to the reduction achieved in the tarsometatarsal joint complex. Classical studies such as those carried out by authors such as Myerson et al., Hardcastle et al. or Arntz et al., already showed that anatomical joint reduction was the main factor for good prognosis in TMC injuries; however, these are studies that mix high and low energy injuries of different complexity.8,22,23 Kuo et al., in a retrospective study on 48 patients with TMC lesions treated by open reduction and internal fixation, found rates of osteoarthritis of 25%, with arthrodesis being necessary in six patients, during an average follow-up of 54 months, and recommend stable fixation of these injuries to prevent the development of osteoarthritis and improve functional outcomes; but once again this is a study where the sample of patients is not homogeneous with regard to the type of injury, the outcomes being worse in purely ligamentous injuries.24 Wagner et al., in a study on 22 patients with low energy TMC injuries without associated fractures in whom they carried out percutaneous treatment achieving an anatomical or almost anatomical reduction in all the patients, achieved good functional outcomes (AOFAS scale).15 Results similar to those published by Vosbikian et al., on a sample of 38 patients with low energy injuries treated percutaneously, although in this case patients with associated fractures of metatarsal bones were also included.16
There is little literature on the percutaneous treatment of subtle TMC injuries25; the papers often report results of heterogeneous samples in terms of selection of patients and complexity of injuries. We found no studies in the literature that assess the relationship between tarsometatarsal joint reduction in subtle injuries, with statistically significant results, such as those presented here. The main strengths of the present paper are that it is a homogeneous sample of patients in terms of type of injury, since all the patients presented subtle, purely ligamentous injuries (II-III of Nunley and Vertullo's classification). This is a number to be taken into consideration, given the low overall frequency of TMC injuries, especially subtle injuries, which are under-diagnosed. Furthermore, we present a protocolised methodology for the management of subtle TMC injuries, which aims to reduce the incidence of unnoticed injuries and delay in treatment.
Our paper has the weaknesses of retrospective studies. It is also a paper with a small sample size, although we should not forget the low incidence of the injuries covered. In our centre we base the diagnosis on symptoms, and it is confirmed with CT images. Since it is a non-weight-bearing diagnostic test, it is possible that some injuries that only become visible on weight-bearing or stress may go unnoticed during first assessment. Similarly, the fact that no weight-bearing X-rays are available poses a problem when using Nunley's and Vertullo's classification of subtle TMC injuries. The average follow-up of patients is short. The future objective is to assess the progress of our patient series in the long term to evaluate the need for screw removal due to discomfort and/or loosening, and the development of tarsometatarsal osteoarthritis.
The ultimate intention of our working group is to protocolise, the diagnosis and management of these injuries in our centre to reduce the number of cases that go unnoticed and optimise our patients’ outcomes.
ConclusionsThe surgical treatment of subtle Eleftheriou and Rosenfeld type II or II-III Nunley and Vertullo MTC injuries, by closed reduction and percutaneous synthesis, offers good clinical-functional outcomes in the medium term. We have been able to confirm how anatomical reduction is a determining factor for good functional outcomes in our patients (p < .01).
FundingThis research study has received no specific support from public sector agencies, commercial sector, or non-profit entities.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Abarquero-Diezhandino A, Ferrero-Recasens J, Vacas-Sanchez E, Mellado-Romero MA, Sánchez-Morata EJ, Vila-Rico J. Resultados funcionales del tratamiento quirúrgico percutáneo de las lesiones sutiles del complejo tarso-metatarsiano. Rev Esp Cir Ortop Traumatol. 2020;64:367–374.