Talipes equinovarus or clubfoot is a congenital deformity of the foot with bone, muscle, and tendon involvement. It is one of the most frequent foot malformations in pediatric orthopedics. Although generally idiopathic, it may have a syndromic cause and be associated with musculoskeletal, neurological, or connective tissue conditions. The treatment of choice in idiopathic clubfoot is the Ponseti method based on manipulation and fixation with serial casts that seek progressive correction of the deformity. The Ponseti method effectiveness has been demonstrated in arthrogryposis and myelomeningocele clubfoot. There are few clinical studies demonstrating the efficacy of this therapeutic option in patients with syndromic clubfoot.
Material and methodsRetrospective study with 6 patients (9 feet) with syndromic clubfoot treated in a tertiary center with the Ponseti method with a minimum follow up of two years (2–18). The results were evaluated with the Pirani classification, assessing clubfoot severity before and after treatment.
ResultsOf the six patients treated were used an average of 6.5 casts. The Pirani scale obtained a mean score of 5.2 before treatment, with a decrease to 1.27 after treatment, with a mean improvement of 3.93 points. In more than half of the cases it was necessary to lengthen the Achilles tendon to correct the equine deformity. In addition, an ankle-foot orthosis was used to reduce recurrences in patients with dysmetria or psychomotor retardation. The most frequently observed residual deformity was the adduct. A patient relapsed twice.
ConclusionsThe Ponseti method obtains effective results in the correction of syndromic clubfoot, although it requires a greater number of corrective casts than other pediatric foot pathologies.
El pie zambo supone una de las malformaciones congénitas del pie más frecuentes. Generalmente la etiología es idiopática. Sin embargo, pueden presentar una causa sindrómica y asociarse con afecciones musculoesqueléticas, neurológicas o del tejido conjuntivo, recibiendo en estos casos, la denominación de pie zambo sindrómico.
El tratamiento de elección del pie zambo idiopático es el método Ponseti, basado en la manipulación y yesos seriados. También se ha demostrado su utilidad en pie zambo asociado con artrogriposis y mielomeningocele, pero existen pocas publicaciones sobre la eficacia en el pie zambo sindrómico.
Material y métodosEstudio retrospectivo en seis pacientes (nueve pies) con pie zambo sindrómico tratados en un centro terciario siguiendo el método Ponseti. Tiempo de seguimiento mínimo de dos años (2-18). Los resultados fueron evaluados con la clasificación de Pirani, para valorar la severidad del pie zambo, previa y posteriormente al tratamiento.
ResultadosEn los seis pacientes tratados, se emplearon una media de 6,5 yesos. La escala de Pirani obtuvo una valoración media de 5,2, previamente al tratamiento, con un descenso hasta 1,27 tras el tratamiento, con una mejoría media de 3,93 puntos.
En más de la mitad de los casos fue necesario una tenotomía del tendón Aquileo para corregir la deformidad en equino. Se utilizó una ortesis tobillo-pie para reducir las recidivas si retraso psicomotor o dismetría severa. La deformidad residual más frecuente fue el aducto, que no requirió tratamiento quirúrgico. Un paciente recidivó en dos ocasiones.
ConclusionesEl método de Ponseti es útil en el tratamiento del pie zambo sindrómico, aunque precisa un número mayor de yesos correctores que en el pie zambo idiopático. La deformidad residual más frecuente en esta muestra fue el adductus.
Clubfoot, also known as talipes equinovarus, is a congenital foot deformity affecting all three planes of space. It is characterised by pes cavus with hindfoot equinus, hindfoot varus and forefoot adduction. Along with hip dysplasia and scoliosis, it is one of the most common orthopaedic deformities in children.
In most cases, clubfoot is idiopathic in aetiology, however a percentage can be associated with a heterogeneous cohort of diseases, known, in this case, as syndromic clubfoot. Some of the conditions described are neurological, connective tissue syndromes, neuromuscular disorders, or chromosomal abnormalities.1–3
The Ponseti method, based on manipulation and serial casting, is currently the treatment of choice for idiopathic clubfoot.1 It has also been shown to be useful in the treatment of rigid teratologic clubfoot associated with arthrogryposis and myelomeningocele.4–9 However, there are currently few publications in the literature on the results of using this method in cases of clubfoot associated with syndromic conditions.1,10
This paper reviews the results obtained in a tertiary hospital using the Ponseti method to treat patients with syndromic clubfoot.
Material and methodsConsecutive retrospective review of patients with clubfoot associated with a syndromic condition treated in a tertiary hospital from 2001 to 2019.
The patients were assessed and treated by a paediatric orthopaedic team with experience in the management of clubfoot and several publications on the subject.9,10
Patients of paediatric age with syndromic clubfoot, treated and followed up in this centre during the study period were included. Patients with idiopathic clubfoot were excluded, as well as cases associated with myelomeningocele and arthrogryposis, as the efficacy of the Ponseti method in this type of pathology has already been widely demonstrated.
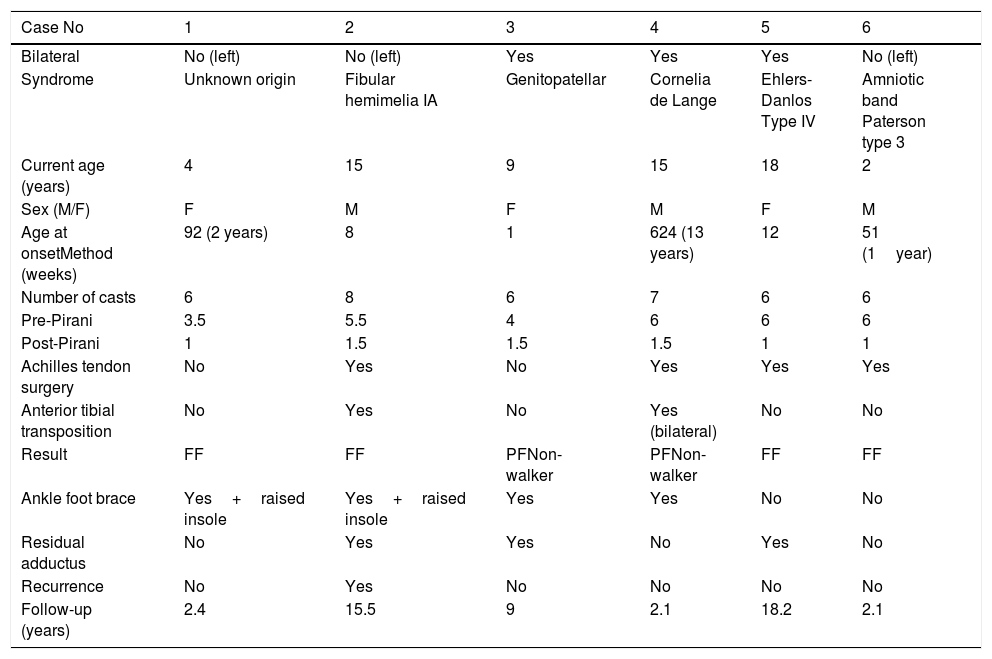
A sample was obtained of six patients (three females and three males), aged between 2 and 18 years, who met the inclusion criteria. Three of them had bilateral involvement and the other three had left laterality, giving a total of nine feet.
Excluding one patient who consulted for the first time at the age of 12 years, the mean age of treatment initiation was 32.8 weeks of life (range 1–92). The follow-up time varied among the patients aged from two years to 18 years, with a median of 5.7 years.
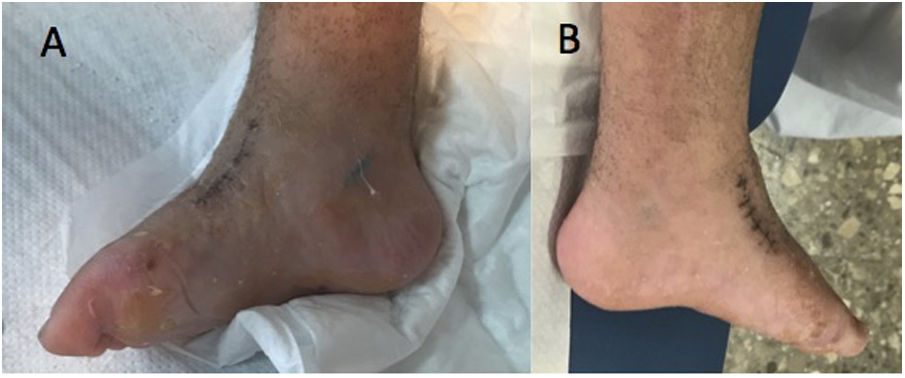
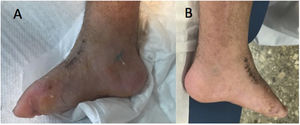
Of the total sample, five patients (83%) had a known syndromic diagnosis: Cornelia de Lange syndrome (Figs. 1 and 2), fibular hemimelia type IA, genitopatellar syndrome, Ehler-Danlos syndrome, type IV or vascular, and amniotic band syndrome. This implied the association of other musculoskeletal developmental disorders, such as digital agenesis, lower limb dysmetria, patellar absence with knee flexion deformity, scoliosis, or fusion of costal arches. Patients with Cornelia de Lange syndrome and genitopatellar syndrome also had associated psychomotor retardation.
All patients were evaluated by a multidisciplinary team of paediatricians, neurologists, geneticists, and paediatric orthopaedic specialists.
All the patients were treated conservatively following the Ponseti method. This technique consists of a specific sequence of foot manipulation and serial casting, with an Achilles tendon tenotomy when the midfoot has been corrected, but the hindfoot has persistent equinus, posterior crease or empty heel. This method should be started as soon as possible after birth. The first step is to correct the cavus by supination of the forefoot in relation to the hindfoot until the longitudinal arch shape of the foot is normal in appearance. Manipulation consists of abduction of the foot in supination under the talus, after stabilisation of the talus with the thumb of the opposite hand. All components of the deformity are corrected simultaneously. After manipulation, the knee is immobilised in a well-moulded inguinopedic cast with the knee in flexion. From the second, third and fourth casts onwards, the cavus, adductus and varus are corrected simultaneously. The equinus deformity gradually improves as the adductus and varus are corrected, but an Achilles tenotomy is usually required for complete correction.11 Prolonged treatment with orthosis is then indicated to maintain the foot in abduction and dorsiflexion. The orthosis is fitted immediately after removal of the last cast. The orthosis is worn 23h a day for the first three months, and after three months for 14−16h a day for up to four years. In our series, in patients with associated psychomotor retardation or pronounced dysmetria, an ankle-foot orthosis was used after removal of the abduction orthosis.
Recurrences were also re-treated using the Ponseti method, with manipulations and serial casting, and Achilles tendon surgery. If the recurrence occurs in children, in whom the lateral cuneiform has already ossified, transposition of the tibialis anterior is combined with the surgery and the abduction orthosis is no longer used.3
The aim of the treatment was to obtain a functional foot for walkers, and to achieve a plantigrade, non-painful foot able to wear a shoe in non-walkers with severe psychomotor retardation.
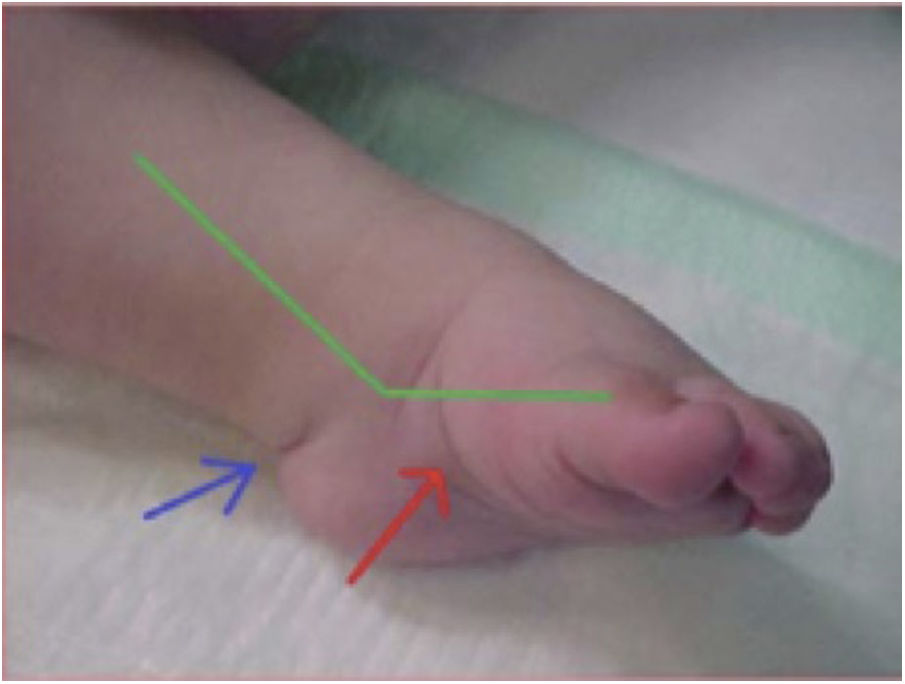
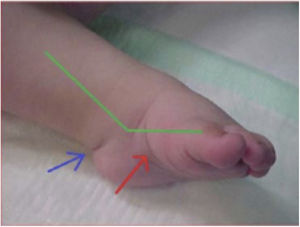
The Pirani classification system3 was used to establish a homogeneous, and as objective as possible, measure of the severity of the deformity. This system is based on six clinical signs of clubfoot which are scored according to degree of deformity as 0 (normal), 0.5 (moderately abnormal) or 1 (severe), with six being the maximum score in case of extreme deformity. The six signs are divided equally into three in the midfoot (curved lateral border, medial crease, and lateral head of talus) and three in the hindfoot (posterior crease, rigid equinus and empty heel) (Figs. 3 and 4).
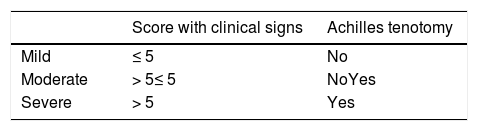
Once the results have been obtained, they are classified according to the score and the need for Achilles tenotomy into mild (≤ 5 points not followed by tenotomy), moderate (> 5 points not followed by tenotomy or ≤ 5 followed by tenotomy) and severe (> 5 points followed by tenotomy) (Table 1).3,18
In our series, the pre-treatment Pirani score was 5.2 (range 3.5–6). Six feet were severely affected (Pirani > 5 requiring Achilles tendon surgery) and the remaining three were mild (Pirani ≤ 5 without requiring Achilles tendon surgery) (Table 2).
Characteristics of the six patients with syndromic clubfoot.
| Case No | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Bilateral | No (left) | No (left) | Yes | Yes | Yes | No (left) |
| Syndrome | Unknown origin | Fibular hemimelia IA | Genitopatellar | Cornelia de Lange | Ehlers-Danlos Type IV | Amniotic band Paterson type 3 |
| Current age (years) | 4 | 15 | 9 | 15 | 18 | 2 |
| Sex (M/F) | F | M | F | M | F | M |
| Age at onsetMethod (weeks) | 92 (2 years) | 8 | 1 | 624 (13 years) | 12 | 51 (1year) |
| Number of casts | 6 | 8 | 6 | 7 | 6 | 6 |
| Pre-Pirani | 3.5 | 5.5 | 4 | 6 | 6 | 6 |
| Post-Pirani | 1 | 1.5 | 1.5 | 1.5 | 1 | 1 |
| Achilles tendon surgery | No | Yes | No | Yes | Yes | Yes |
| Anterior tibial transposition | No | Yes | No | Yes (bilateral) | No | No |
| Result | FF | FF | PFNon-walker | PFNon-walker | FF | FF |
| Ankle foot brace | Yes+raised insole | Yes+raised insole | Yes | Yes | No | No |
| Residual adductus | No | Yes | Yes | No | Yes | No |
| Recurrence | No | Yes | No | No | No | No |
| Follow-up (years) | 2.4 | 15.5 | 9 | 2.1 | 18.2 | 2.1 |
FF: Functional foot; PF: Plantigrade foot.
Clinical follow-up was every four months for the first two years and every six months thereafter. Functional correction of the deformity (plantar foot, painless), Pirani3 score after treatment, relapse and the need for additional surgical procedures were assessed.
ResultsUsing the Ponseti method to treat the patients included in the study, a mean correction according to the Pirani classification of 3.93 points was obtained, decreasing from 5.2 points before treatment to 1.27 points after completion of treatment.
Six to eight serial casts with a mean of 6.5 were required to complete the treatment.
An Achilles tenotomy was performed to correct the clubfoot in over half the patients (six out of nine), following the Pirani classification.
Only one case in this series had two recurrences of the deformity. This patient was the child with fibular hemimelia. In the first recurrence, at three years of age, manipulations and six serial casts were performed, in addition to Achilles Z-lengthening. In the second recurrence, at five years of age, transposition of the tibialis anterior tendon to the lateral cuneiform was combined with the previous treatment. The second case in which this last surgical gesture was combined was the child with delayed treated clubfoot. This patient had Cornelia de Lange syndrome and presented at our centre at 13 years of age.
Forefoot adductus was the most frequently observed residual deformity in the cohort studied, present in three patients (five feet). In these cases, the deformity was not surgically corrected for different reasons related to the pathology associated with their syndromic picture.
An ankle-foot orthosis was used in four of the six patients. Two of them with associated severe psychomotor retardation and the other two with significant lower limb dysmetria.
The established objective was achieved in all cases: five functional feet (of four patients) and four feet suitable for footwear and non-painful, in the patients who were non-walkers due to their underlying disorder.
DiscussionThe Ponseti method has become the gold standard in the treatment of idiopathic clubfoot due to its excellent results and the marked decrease in surgery rates.4,9,12,13 Thanks to the consolidation of this technique, surgery has gone from first-line treatment to a secondary option to complement correction already achieved with conservative treatment.14
There are fewer publications on non-idiopathic clubfoot, with arthrogryposis and myelomeningocele being the aetiologies that appear most frequently in these studies.6,15,16
In our case, arthrogryposis was not included because it is a phenotypic manifestation that can be associated with more than 300 diseases with very different aetiologies, and whose common characteristic is congenital joint contracture presenting in at least two different areas of the body.17,18 Myelomeningocele was excluded because the deformity is the result of intrauterine flaccid paralysis, which causes an imbalance in the forces, resulting in foot deformity.19
Myotonic dystrophy is another disorder with muscle involvement that is repeated in three of the reviews.1,6,15 Genetic disorders also play an important role, among which trisomies 18 and 21 and Larsen, Toriello-Carey and DiGeorge syndromes are noteworthy due to their prevalence. Finally, amniotic band syndrome appears in four of the cohorts.1,6,15,20
However, of the five disorders with an established diagnosis in this study, only Ehlers-Danlos syndrome and amniotic band syndrome appear in the cohort of the other articles reviewed.1,6,16 Despite the existence of case reports linking fibular hemimelia with clubfoot, the only study we reviewed that uses the Ponseti method to treat this condition is the same case that we review here.10 However, there is one case of tibial hemimelia described in Moroney's sample.16
The studies by Gurnett,15 Janicki6 and Moroney16 compare the use of the Ponseti method in patients with idiopathic vs. non-idiopathic clubfoot (including myelomeningocele and arthrogryposis). These studies conclude a good clinical outcome, but with more casts and a greater need for surgical intervention. However, this surgery is less aggressive after the initial orthopaedic treatment.
Finally, in 2018, Matar1 published the first article on the treatment of syndromic clubfoot, excluding myelomeningocele and arthrogryposis. From his experience he states that the Ponseti method is an effective first-line treatment and that the main challenge currently is to maintain correction. Even so, he confirms that already mentioned previously in the literature, as these syndromic feet will require a greater number of casts and will have a higher risk of recurrence. In our series, we only recorded one case of recurrence. However, this data cannot be considered definitive, as two patients were under five years old at the end of the study follow-up and therefore might recur in the future. On the other hand, three of the six patients were over 14 years of age at the end of the study, therefore, recurrence of the deformity would not be expected in these patients.
Ponseti states in his original technique that four to five serial casts are usually sufficient for correction of the deformity.3 However, in the case of syndromic clubfeet, the average number of casts is higher.6,15,16 In the present series, there was a mean of 6.5 casts (range 6–8), which supports the statement that a higher mean number of casts is needed in the treatment of syndromic clubfoot.
The Pirani scale was used to assess the improvement of the treated feet. The deformity was measured before treatment, with a mean score of 5.2 points (out of a maximum of 6), and at the end of treatment, where a mean score of 1.27 was obtained. In other words, the average deformity of the sample was reduced by 3.93 points. These results are in line with those obtained by Moroney,16 who, starting from a pre-treatment score of 5.8, achieved a reduction to 3.7 points post-treatment, with a mean improvement of 2.1. Both reviews support a remarkable mean decrease in Pirani score, demonstrating the usefulness of the treatment using an objective scale.
Adductus was observed in three of the six patients (five feet). Parsa et al.21 state that forefoot adductus is the most common residual deformity in the treatment of paediatric clubfoot, as was the case in our series. However, none of the patients who presented the deformity required treatment for different reasons. One of the cases had Ehlers-Danlos syndrome, type IV or vascular, which meant that surgery, although minor, could be life-threatening for the patient. In another case, the operation was rejected by the patient’s own relatives because the patient’s foot was functional and he had undergone several previous operations (due to recurrence of the equinus, varus, adductus, and dysmetria associated with fibular hemimelia). The last case is that of a patient with genitopatellar syndrome, which is associated with significant psychomotor retardation, therefore a plantar foot, able to wear a shoe and not painful, was the main objective.
A limitation of the sample studied is that it is a small and heterogeneous group of syndromes that have in common the presence of an equinus varus and adductus deformity of the foot. This deformity can be treated following the Ponseti method, but the final goal of treatment is determined by the other disorders associated with the syndromic picture. Thus, in two of the patients in our series, the goal was to obtain a plantigrade foot that was pain-free and able to wear a shoe. In our opinion, it is important that the medical team treating the patient establishes a real goal and informs the parents of this goal.
This review provides information on a topic on which the literature is scant. The results found in this study support those obtained by the other authors presented above and confirm the hypothesis that the Ponseti method is also suitable to treat syndromic clubfoot, thus avoiding multiple and complicated surgical interventions; the only difference being that more casting is required compared to idiopathic clubfoot. Furthermore, residual adductus is usually noted as the most frequent residual deformity.
Level of evidenceLevel of evidence IV.
Presented as a poster at the XIII Annual Congress of the Spanish Pediatric Orthopedics Society (SEOP) in Madrid on June 5, 6 and 7, 2019.
Please cite this article as: Ferrando Meseguer E, Roig Sánchez S, Pino Almero L, Romano Bataller A, Mínguez Rey MF. Pie zambo sindrómico más allá de la artrogriposis y el mielomeningocele: tratamiento ortopédico con el método de Ponseti. Rev Esp Cir Ortop Traumatol. 2021;65:180–185.