To evaluate the clinical and radiological results in the surgical treatment of moderate and severe hallux valgus by performing percutaneous double osteotomy.
Materials and methodsA retrospective study was conducted on 45 feet of 42 patients diagnosed with moderate–severe hallux valgus, operated on in a single center and by the same surgeon from May 2009 to March 2013. Two patients were lost to follow-up. Clinical and radiological results were recorded.
ResultsAn improvement from 48.14±4.79 points to 91.28±8.73 points was registered using the American Orthopedic Foot and Ankle Society (AOFAS) scale. A radiological decrease from 16.88±2.01 to 8.18±3.23 was observed in the intermetatarsal angle, and from 40.02±6.50 to 10.51±6.55 in hallux valgus angle. There was one case of hallux varus, one case of non-union, a regional pain syndrome type I, an infection that resolved with antibiotics, and a case of loosening of the osteosynthesis that required an open surgical refixation.
DiscussionPercutaneous distal osteotomy of the first metatarsal, when performed as an isolated procedure, shows limitations when dealing with cases of moderate and severe hallux valgus. The described technique adds the advantages of minimally invasive surgery by expanding applications to severe deformities.
ConclusionsPercutaneous double osteotomy is a reproducible technique for correcting severe deformities, with good clinical and radiological results with a complication rate similar to other techniques with the advantages of shorter surgical times and less soft tissue damage.
Evaluar los resultados clínicos y radiológicos en el tratamiento del hallux valgus moderado y grave mediante la realización de una doble osteotomía percutánea.
Material y métodosSe presenta un estudio retrospectivo de 45 pies intervenidos en 42 pacientes diagnosticados de hallux valgus moderado-severo, operados en un solo centro y por el mismo cirujano entre mayo del 2009 y marzo del 2013. Dos pacientes no acudieron a los controles posquirúrgicos. Se registraron los resultados clínicos y radiológicos.
ResultadosSegún la escala de la American Orthopedic Foot and Ankle Society (AOFAS) se obtuvo una mejoría de la puntuación de 48,14±4,79 puntos a 91,28±8,73 puntos. Radiográficamente se obtuvo una disminución en el AIM de 16,88±2,01 a 8,18±3,23 y en el AHV de 40,02±6,50 a 10,51±6,55. Hubo un caso de hallux varus, un caso de seudoartrosis, un síndrome doloroso regional complejo tipo I, una infección que se resolvió con antibióticos y un caso de movilización de la osteosíntesis usada que requirió reintervención abierta.
DiscusiónLas osteotomías percutáneas distales aisladas del primer metatarsiano muestran limitaciones a la hora de enfrentarse a casos de hallux valgus moderado y severo. La técnica descrita añade las ventajas de la cirugía mínimamente invasiva, ampliando las indicaciones a deformidades severas.
ConclusionesLa doble osteotomía percutánea es una técnica reproducible que permite la corrección de deformidades severas con buenos resultados clínicos y radiológicos y con una tasa de complicaciones similares a otras técnicas, con tiempos operatorios más cortos y menor daño de partes blandas.
Elective hallux valgus surgery is indicated in patients reporting pain due to deformity or difficulty to use normal footwear in specific cases. Among the scope of existing techniques to treat hallux valgus, are those considered as minimal-incision or percutaneous techniques.1–14 These techniques are increasingly demanded by patients themselves as their popularity increases, largely due to the esthetic advantage of smaller incisions compared to open techniques.4 However, in addition to the advantages associated with percutaneous surgery, we must also take into account the complications and limitations inherent to their use.15,16 The isolated use of distal osteotomies may not be enough for the treatment of moderate or severe hallux valgus associated to intermetatarsal angles over 16–18° between the first and second metatarsals.3,17 Isolated proximal osteotomies can worsen the distal joint angle of the first metatarsal (distal metatarsal articular angle [DMAA] or proximal articular set angle [PASA]) and increase the risk of elevation and shortening of the first metatarsal.18 The use of combined percutaneous proximal and distal osteotomies increases the surgical indications, enabling their use to correct a large range of angulations.3,18 The advantages of percutaneous surgery would be: a shorter surgery time, reduced tissue dissection, no use of permanent fixation material and a shorter scarring period.4
The purpose of this study is to show that double percutaneous osteotomy can be a reproducible and effective technique for the treatment of moderate to severe hallux valgus.
Materials and methodsWe operated on 44 hallux valgus in 41 patients during the period between 1st May 2009 and 27th March 2013. We included deformities considered from moderate to severe, that is, with a hallux valgus angle (HVA) of 30° and an intermetatarsal angle (IMA) of 14° between the first and second metatarsals, according to the classification of Mann and Coughlin.19 The respective upper limit intervened recorded in this study was an IMA of 20° and an HVA of 58°. We lost 2 cases who did not attend follow-up controls.
We excluded from the study all those cases of hallux valgus considered as mild, which according to our algorithm were treated through isolated distal osteotomies, patients with previous Keller–Brandes type interventions, arthrosis of the first metatarsophalangeal joint, as well as the 2 patients mentioned who did not attend review in outpatient consultation.
The indication for surgery was only established in patients who reported pain and significant involvement for leisure and daily living activities.
We operated on a total of 36 females and 5 males, with a mean age of 61 years at the time of the intervention (range: 20–75 years). Of these, 3 patients underwent bilateral interventions in deferred procedures. Patients were referred to our unit after having received conservative treatment with modification of footwear, orthesis, etc., with no improvement and with an evolution of pain of at least 1 year. Only 5 did not undergo Weil type osteotomies of the lesser metatarsals. We believe it advisable to carry out this procedure both in case of transfer metatarsalgia and shortening of the first ray after conducting osteotomies. In 25 patients we also percutaneously corrected any deformities of the lesser toes which could coexist at the time of surgery, through osteotomies or tenotomies. All surgical procedures were conducted by the same orthopedic surgeon at the same center.
Postoperative evolution was controlled clinically and radiographically at 6 weeks, 3 months, 6 months, 1 year and 2 years after the intervention, with the frequency of visits being increased in case of complications. The mean evolution of recorded cases was of 24.02 months (range: 12–51 months), with 16 operated feet presenting an evolution of 2 years or more and 27 feet a minimum evolution of 1 year. Preoperatively, we observed the IMA, HVA and DMAA values in an anteroposterior radiograph whilst under load, as well as the postoperative results of the angles 6 months after the intervention.
We recorded the scores in the American Orthopedic Foot and Ankle society (AOFAS) scale pre- and postoperatively.20
The recorded data underwent statistical analysis consisting in a Student t test for paired data, using the statistics software package SPSS Statistics version 22 (IBM, Armonk, USA).
Surgical techniquePatients were placed in the supine position with both lower limbs projecting from the lower part of the table, in order to use the minifluoroscope, essential for the percutaneous procedure. The anesthetic technique consisted in distal sensory block of the ankle or a block at the level of the popliteal fossa depending on the judgment of the anesthesiologist. All patients received a dose of 2g cefazolin as antibiotic prophylaxis in an interval between 1h and 30min before starting the procedure. We did not use ischemia in any of the procedures.
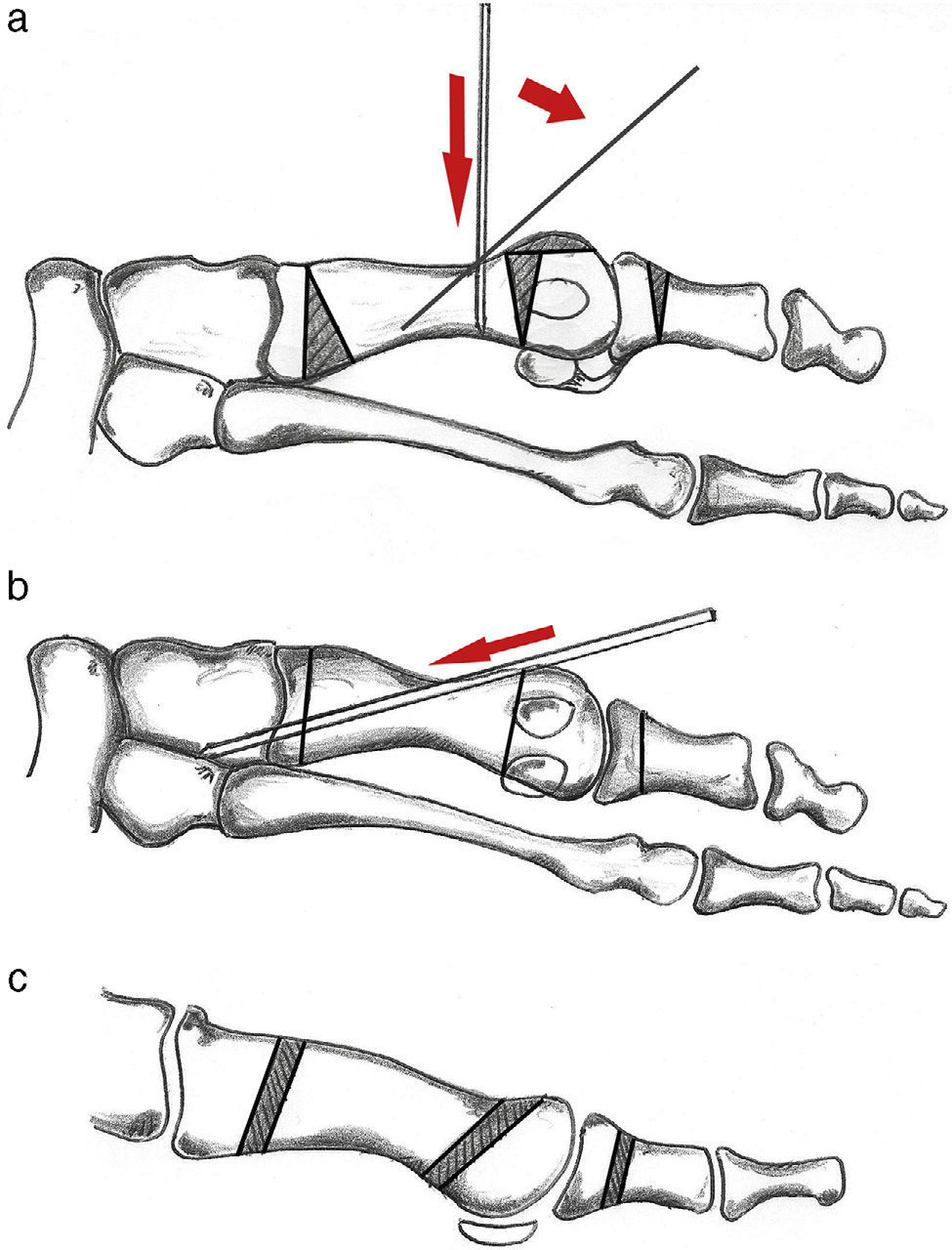
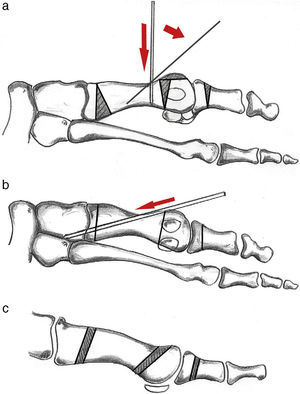
Following the technique described by De Prado et al.,21 we initially carried out a cutaneous incision 3mm in length with a percutaneous surgery scalpel with a Beaver 64 (Waltham, USA) blade, proximal and plantar to the bunion. After creating a working space by opening a cavity between the bone and capsule, we used the motorized drill at a speed no higher than 5000rpm in order to prevent bone necrosis during the buniectomy. Next, we assessed the possibility of conducting a Reverdin-Isham type distal osteotomy to correct DMAA (PASA), making an incision with the drill from distal dorsal to proximal plantar, behind the sesamoids, at an angle of 45° (Fig. 1a). We performed a percutaneous tenotomy of the abductor hallucis with lateral capsulotomy and Akin osteotomy in all patients.
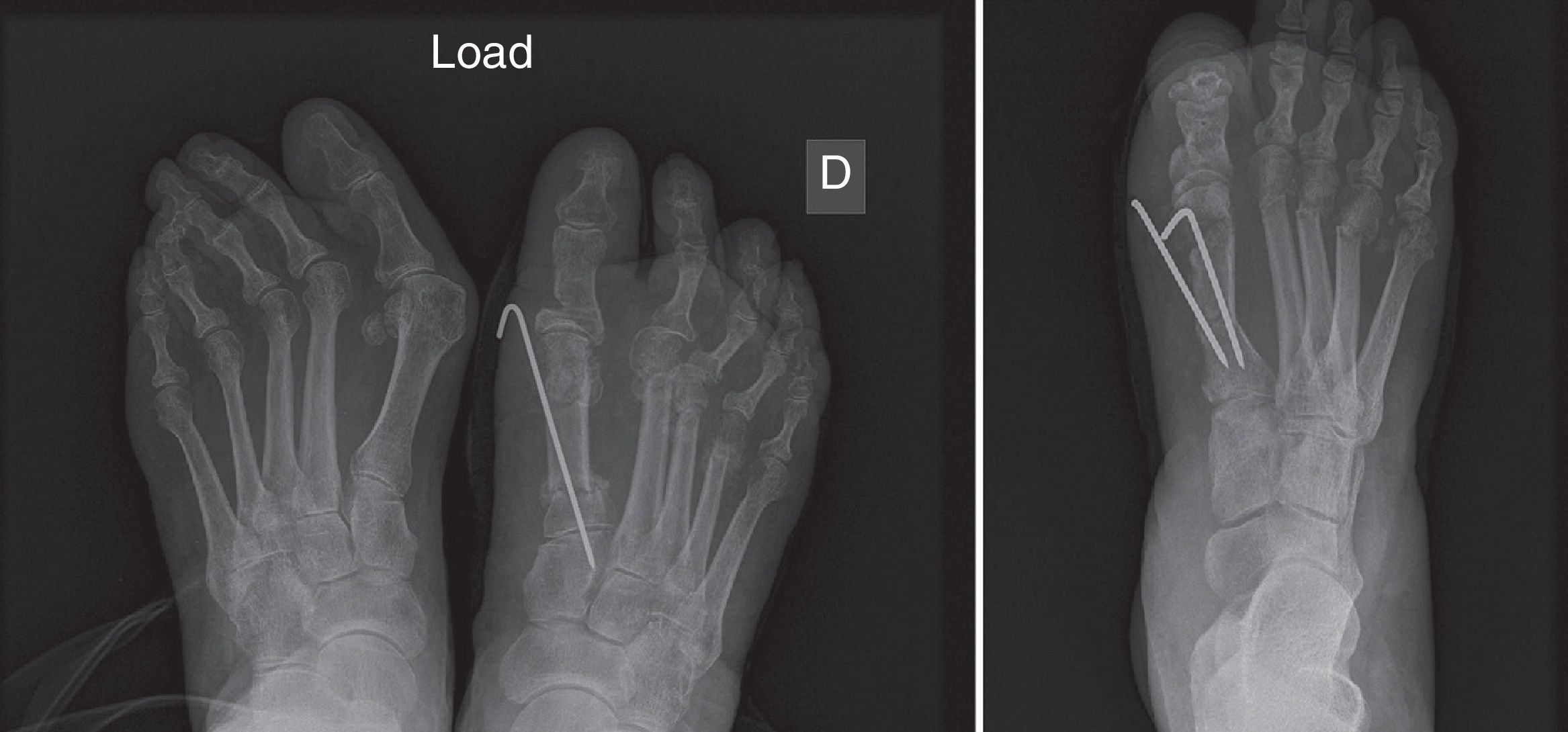
To perform the osteotomy of the base of the first metatarsal, we palpated the extensor hallucis longus tendon and, laterally to it, used the fluoroscope to find a point located approximately 1.5cm from the base of the metatarsal, where we made an incision with a Beaver 64 scalpel. Next, we slid a scraper through the lateral aspect of the metatarsal to remove the periosteum and began to cut the bone with a Shannon 44 drill (Vilex Inc., McMinnville, TN, USA). We made the cut in an intermediate plane between the plane which would be the floor in a position of load and that corresponding to the axial of the first metatarsal. We attempted to respect the medial cortical. Next, using a Wedge Burr type drill (Vilex Inc., McMinnville, TN, USA), we drilled a sufficiently large cavity to allow closure and achieve correction of the IMA. We distally introduced a Kirschner wire 2mm in diameter perpendicularly to the diaphysis, and then brought it closer converging on the angle to the axis of the metatarsal, in an intramedullary direction from distal to proximal (Fig. 1b) whilst at the same time pressing on the metatarsal closing the wedge and bringing it closer to the second metatarsal. Lastly, we crossed the site of the osteotomy with the Kirschner wire and fixed to the base of the metatarsal or to the first wedge (Figs. 1 and 2). Optionally, depending on the quality of the fixation, we introduced another Kirschner wire to provide additional stability (Fig. 2). Subsequently, depending on the shortening of the first metatarsal which was necessary to correct the angle or the presence of metatarsalgia in the previous clinical assessment, we carried out percutaneous Weil osteotomies and corrections in the lesser toes. After suturing the surgical incisions, we placed a functional bandage with hypercorrection of the hallux valgus to maintain alignment of the osteotomies which were not fixed, and this was maintained for 6 weeks with weekly changes in our outpatient consultation by the nursing staff. Load with postoperative footwear was authorized from the first day. The use of normal, comfortable footwear was authorized after 6 weeks. All patients received 10 days of low molecular weight heparin as antithrombotic prophylaxis, and we did not detect any case of deep vein thrombosis. Postoperative analgesia consisted in etoricoxib 120mg once per day for days 4 associated to a combination of 37.5mg tramadol hydrochloride and 325mg paracetamol with 1–3 daily doses depending on the pain.
After 6 weeks, the Kirschner wires were removed by the nursing staff in outpatient consultation after ensuring the start of bone callus in radiographs under load and the use of normal footwear was authorized, reminding patients to perform mobilization exercises for the metatarsophalangeal joint and contrast baths to reduce edema.
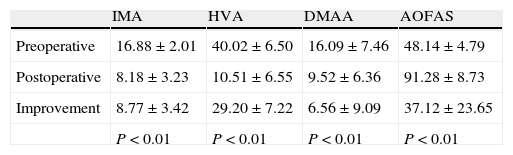
ResultsRegarding the radiographic results (Fig. 3), we observed an improvement in the IMA from 16.88±2.01 to 8.18±3.23 and in the HVA from 40.02±6.50 to 10.51±6.55 with statistically significant values, applying a 95% confidence interval. The value of the DMAA showed a mean improvement of 6.56±9.09 (Table 1). The measurements were made in radiographs whilst standing, 6 months after the procedure. Consolidation of the osteotomies was confirmed radiographically in all patients except for 1 case within 6 months. In general, it was possible to observe the start of a fracture callus radiographically after 6–8 weeks evolution.
Radiographic and American Academy of Foot and Ankle Surgery (AOFAS) scale results, along with mean pre- and postoperative values.
| IMA | HVA | DMAA | AOFAS | |
| Preoperative | 16.88±2.01 | 40.02±6.50 | 16.09±7.46 | 48.14±4.79 |
| Postoperative | 8.18±3.23 | 10.51±6.55 | 9.52±6.36 | 91.28±8.73 |
| Improvement | 8.77±3.42 | 29.20±7.22 | 6.56±9.09 | 37.12±23.65 |
| P<0.01 | P<0.01 | P<0.01 | P<0.01 |
AOFAS: American Orthopedic Foot and Ankle Society scale; DMAA: distal metatarsal articular angle; HVA: hallux valgus angle; IMA: intermetatarsal angle between the first and second metatarsals.
Regarding complications, 3 patients suffered recurrence of the deformity (HVA>20°). We registered 3 cases of elevation of the metatarsal in the sagittal plane regarding the previous radiographs, both cases with a follow-up of 2 years and with no clinical significance. There were no cases of necrosis of the metatarsal head. There was 1 case of mobilization of the osteosynthesis in the immediate postoperative period, which required reintervention through open surgery, and another one required reintervention through open surgery due to pseudoarthrosis of the osteotomies, both in the base and Weil type after 1.5 years follow-up. We also detected 1 case of mild hallux varus with good tolerance by the affected patient, who refused another intervention. Lastly, we registered 1 deep infection which responded adequately to antibiotic treatment. The postoperative AOFAS score was 91.28±8.73 (range: 65–100), recorded after 1 or 2 years of the intervention (Table 1).
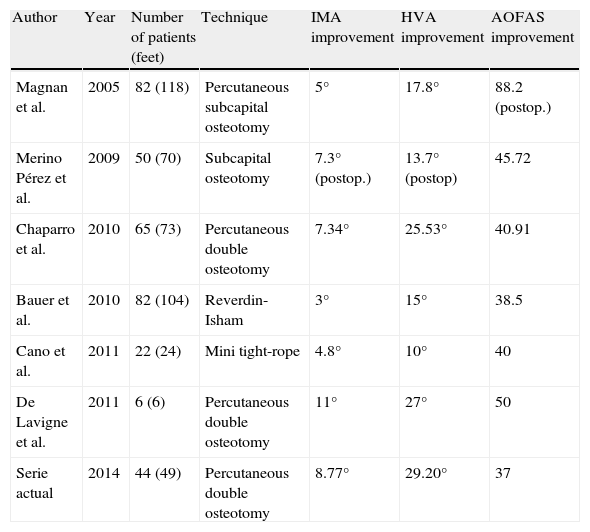
DiscussionThe result of 91.28±8.73 points obtained in the postoperative AOFAS (Table 1) demonstrates similar results to those with other percutaneous1–9,13,22,23 (Table 2) and open techniques.6,10,12,14,24 Double osteotomy for the correction of hallux valgus was first described by Logroscino in 1948. Other authors, like Peterson and Johnson, reported double osteotomies in adolescents en 1993.22 In 1999, Coughlin published results of 18 feet intervened through open double osteotomy of the first metatarsal for hallux valgus with increased DMAA, fixed with Kirschner wires and cannulated screws. He did not use the AOFAS scale, but reported that 14 out of 18 patients were satisfied with the surgical result. Regarding the angles, he achieved mean corrections of 34–12° for the HVA and 15–6° for the IMA. As complications, he registered 1 case of deep vein thrombosis, 1 loss of internal fixation in osteotomy of the base and 1 case of hallux varus which required reintervention. In cases where an Akin osteotomy was added, the technique is described as “triple osteotomy”.23
Comparison with published studies which used a percutaneous double osteotomy or percutaneous distal osteotomy in moderate or severe cases of hallux valgus.
| Author | Year | Number of patients (feet) | Technique | IMA improvement | HVA improvement | AOFAS improvement |
| Magnan et al. | 2005 | 82 (118) | Percutaneous subcapital osteotomy | 5° | 17.8° | 88.2 (postop.) |
| Merino Pérez et al. | 2009 | 50 (70) | Subcapital osteotomy | 7.3° (postop.) | 13.7° (postop) | 45.72 |
| Chaparro et al. | 2010 | 65 (73) | Percutaneous double osteotomy | 7.34° | 25.53° | 40.91 |
| Bauer et al. | 2010 | 82 (104) | Reverdin-Isham | 3° | 15° | 38.5 |
| Cano et al. | 2011 | 22 (24) | Mini tight-rope | 4.8° | 10° | 40 |
| De Lavigne et al. | 2011 | 6 (6) | Percutaneous double osteotomy | 11° | 27° | 50 |
| Serie actual | 2014 | 44 (49) | Percutaneous double osteotomy | 8.77° | 29.20° | 37 |
AOFAS: American Orthopedic Foot and Ankle Society scale; HVA: hallux valgus angle; IMA: intermetatarsal angle between the first and second metatarsals.
At present, several open techniques have been described, both distal (Hohmann, Wilson, Mitchell and Chevron) and proximal, as well as Mann,12 Ludloff or scarf osteotomies, with results which are comparable to the technique described. In 2000, Trnka et al.24 carried out the Chevron technique on 66 feet with a follow-up of 2–5 years and an AOFAS score of 90–92 points, as he divided the patients into age groups over and under 50 years. As complications, 3 patients suffered non-union with deformity of the osteotomy, 1 deep infection and 1 case of type I RSD (reflex sympathetic dystrophy).
In 2000, Zettl et al.25 intervened 114 feet through crescentic type osteotomy of the base of the first metatarsal with an open technique and distal reefing of soft tissues in moderate to severe hallux valgus (IMA>15° and HVA>30°) with good results in 91% of patients but with 8 cases of hallux varus and 5 cases of failure of the osteosynthesis material.
Focusing on percutaneous techniques, Isham proposed a double osteotomy when the IMA exceeded 18°26 and De Prado proposed carrying out percutaneous double osteotomies in moderate or severe hallux valgus, without specifying their angular measurements.1,21 In 2010,22 Chaparro et al. presented 73 feet intervened through a double percutaneous osteotomy, fixing the proximal osteotomy with a cannulated screw and a mean reported result of 90.8 points in the AOFAS scale. The indication for a double osteotomy was established from 15° IMA. As complications he reported 2 failures of the osteosynthesis with iatrogenic fracture at the site of introduction of the screws, 2 cases of type I RSD, and 1 case of mobilization of the distal osteotomy. De Lavigne et al.3 published a prospective study in 6 patients with IMA between 18° and 29° with good results (postoperative AOFAS of 84 points). As a surgical technique he employed a distal Chevron osteotomy and a proximal subtraction osteotomy, with both performed percutaneously.
Double osteotomy enables the correction of moderate–severe IMA and DMAA (PASA).3
Other percutaneous techniques based only on distal osteotomies have been reported. However, some negative results have also been published in connection with these kinds of techniques.15 Magnan et al.2 published corrections of preoperative IMA of up to 20° using an isolated percutaneous subcapital osteotomy, modifying the technique described initially by Bösch et al.9
Regarding the more consolidated open techniques, the results have been similar.
In our case, the technique popularized in our country by De Prado is more reproducible and only requires provisional fixation with Kirschner wires and a functional bandage to maintain the distal osteotomies. The perforation to allow introduction of a screw in the base of the metatarsal can be associated to perioperative fractures,22,26 in addition to implanting a foreign material, with the complications that this may cause.
As contraindications for this technique, we considered the presence of arthrosis or various grades of hallux rigidus.
The radiographic and clinical results obtained with a follow-up period of between 1 and 2 years have achieved satisfactory corrections in the deformities described.
The theoretical problems faced include the possibility of elevation of the first metatarsal, osteonecrosis of the head of the first metatarsal, metatarsophalangeal joint rigidity, non-union (pseudoarthrosis) and the technical difficulty of carrying out a 3D osteotomy based on 2D imaging. Regarding the possible elevation of the metatarsal, the intraoperative use of the fluoroscope with a lateral image whilst standing and achieving a stable fixation with 1 or 2 Kirschner wires should be enough to avoid this complication. Osteonecrosis of the head of the first metatarsal was not detected in our series. Non-union and skin burn problems can be prevented by a careful technique and avoiding high-speed drilling when conducting the osteotomies. Loss of mobility in the metatarsophalangeal joint is observed frequently and can be related to the release of the lateral capsule, non-compliance by patients regarding postoperative exercises, and the presence of intraarticular bone debris particles.
Given the shortening of the first metatarsal when conducting a closure double osteotomy, in most cases we recommend carrying out Weil osteotomies of the lesser rays to achieve a correct metatarsal formula and thus avoid transfer metatarsalgias.
ConclusionsThis study demonstrates that the technique described can be considered as a valid alternative to currently existing techniques, both open and percutaneous. The indication for percutaneous techniques can be extended to severe hallux valgus. The use of Kirschner wires as osteosynthesis material can represent an economic advantage, in addition to avoiding the permanent implantation of material.
We conclude that, with adequate training, it is possible to achieve shorter surgical times, less soft tissue damage entailing less scarring time of the surgical wounds and the advantage of being able to perform the procedure on an outpatient basis by increasing the range of indications of percutaneous hallux valgus surgery to moderate and severe cases.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Díaz Fernández R. Tratamiento del hallux valgus moderado y severo mediante doble osteotomía percutánea del primer metatarsiano. Rev Esp Cir Ortop Traumatol. 2015;59:52–58.