The correct closure of the surgical wound is an important step in the procedure of a total hip prosthesis implantation, which aims to a correct healing of the wound and minimize the risk of complications.
The objective of our study is to determine if the use of a bidirectional barbed suture decreases the closing time after PTC, in the fascial and subcutaneous plane, when compared to the conventional suture polyglactin 910. The hypothesis is that there is no difference in closing time when comparing both sutures.
Material and methodProspective single blind randomized study comparing 2 groups: study group with the use of bidirectional continuous barbed suture (Quill®) (Gr.Q) and a control group (Gr.V) using discontinuous polyglactin 91 suture (Vicryl®). Closure was performed in 2 planes (fascia and subcutaneous) simultaneously by 2 surgeons. The exclusion criteria were: previous surgeries on the same hip, revision surgeries, major deformities and allergies to suture components.
The variables under study were: 1) fascia closure time, subcutaneous and global, 2) surgical wound infection, and 3) dehiscence.
Results82 patients (39 GrQ, 43 GrV) were included. The global closing time was shorter in Gr.Q (5 min 59 s) compared to Gr.V (7.01 min); (p < 0.04). They showed differences in subcutaneous closure; Gr.Q shorter time with a 37 s difference (p = 0.048). Differences in fascial plane were not observed.
Superficial infection was observed in 1 GrQ patient and 1 in GrV; 1 case of deep infection in Gr.Q (p = 0.29). One patient presented dehiscence of the wound in Gr.Q (p = 0.3). However, these differences did not show statistical significance.
ConclusionsThe use of a barbed suture allows a shorter closing time compared to the conventional one. However, despite this decrease in time, no differences were found in terms of the appearance of infection or wound dehiscence.
En cirugía protésica de cadera, el correcto cierre de la herida quirúrgica supone un elemento importante del proceso, que tiene como objetivo la rápida curación de las partes blandas así como minimizar el riesgo de complicaciones.
El objetivo del presente estudio es determinar si la utilización de una sutura barbada bidireccional (Quill®) disminuye el tiempo de cierre tras PTC, en el plano fascial y subcutáneo, al ser comparado con la sutura discontinua convencional de poliglactina 910. La hipótesis es que no hay diferencia en tiempo de cierre al comparar ambas suturas.
Material y métodoSe trata de un estudio prospectivo aleatorizado simple ciego que compara un 1 r grupo estudio con uso de sutura barbada continua bidireccional (Quill®; Ethicon- Johnson & Johnson, Miami, Florida, EUA ) (Gr.Q) y 2° grupo control (Gr.V) sutura discontinua tipo poliglactina 91 (Vicryl® Ethicon- Johnson & Johnson, Miami, Florida, EUA). Sutura realizada en 2 planos (fascia y subcutáneo) simultánea por 2 cirujanos. Antecedente de cirugías previas en la misma cadera, cirugías de revisión, grandes deformidades y alergias a componentes de la sutura fueron criterios de exclusión del estudio.
Las variables a estudio fueron : 1)Tiempo de cierre de fascia,subcutáneo y global, 2) infección herida quirúrgica, y 3)dehiscencia.
ResultadosSe incluyeron 82 pacientes (39 GrQ,43 GrV). El tiempo de cierre global fue menor en Gr.Q (5 min 59seg) respecto Gr.V(7,01 min);(p < 0.04). Mostraron diferencias en cierre subcutáneo; Gr.Q menor tiempo con 37 seg.de diferencia (p = 0,048).No mostraron diferencias en plano fascial.
Se observó infección superficial en 1 paciente de GrQ y 1 en GrV;1 caso de infección profunda en Gr.Q(p = 0,29). Un paciente presentó dehiscencia de la herida en Gr.Q(p = 0,3).
ConclusionesLa utilización de una sutura barbada permite un menor tiempo de cierre respecto la convencional. No obstante, a pesar de esta disminución de tiempo no se han encontrado diferencias en cuanto a aparición de infección o dehiscencia de la herida.
In total hip arthroplasty (THA) correctly closing the surgical wound has the aim of ensuring that the soft tissues cure rapidly, minimising the risk of complications such as dehiscence or the formation of seroma/haematoma, with an acceptable cosmetic result. Likewise, reducing the time taken for surgery is associated with a reduced risk of infection, as well as reducing the costs of treating this complication.1–4
Different suture techniques have been used to date to close the surgical wound after prosthetic surgery. Typically, discontinuous stitches of absorbable polyglactin have been used in the fascial and subcutaneous planes. Some authors point out that this heterogeneous distribution of tension may favour suture failure and the resulting appearance of complications.5,6 Due to this, some surgeons prefer a continuous polyglactin suture closure, with the potential risk of dehiscence if the knotting of the same fails. However, there are no prospective studies which demonstrate the superiority of one technique or the other.
Barbed sutures (BS) started to be commercialised recently, and they have been studied in several published works. They are characterised by certain “barbs” which give rise to a unidirectional anchorage once the thread has passed through a tissue, permitting a suture that is continuous and knot-free, with the same strength as conventional suture.6–8
Several works have been published on the efficacy of suture of this type in prosthetic hip and knee surgery. The results describe a reduction in closure time8–10 that generally leads to a fall in expenses, in spite of the cost of the suture material.3,11 The majority of these studies are retrospective, and only an isolated few are randomised and prospective.
The hypothesis of this study is that the use of barbed suture reduces the time taken for the surgical wound to close after THA in comparison with normal suture. The aim is to compare whether the use of bidirectional barbed suture reduces closure time after THA in the fascial and subcutaneous planes in comparison with conventional discontinuous polyglactin 910 suture. Secondarily, we will analyse the secondary variables: the presence of acute infection (superficial and deep), dehiscence and surgical wound complications.
Material and methodStudy populationA simple, blind, randomised prospective study was performed in the period from February to July 2016 in a single hospital. It was approved by the Ethics Committee of the Institution (2015/6529). After they had given their informed consent, patients with coxarthrosis were included who had undergone primary hip arthroplasty (cemented/uncemented/hybrid). The exclusion criteria were: previous surgery on the same hip, revision surgery, major deformities or allergies to suture components.
Surgical techniqueThe lateral decubitus position and an anterolateral approach were used in all of the patients. A total hip prosthesis was implanted (cemented/uncemented/hybrid) following the standard procedure, with the primary surgery implants habitually used in our hospital. The models of prosthesis implanted were the ones we habitually use: the Furlong CSF Plus® cup (JRI Orthopedics®), the Metabloc Allofit® cup (Zimmer Biomet®) and, for hybrid prostheses, the Metabloc Allofit®. Following the protocol of our hospital, intravenous tranexamic acid was administered preoperatively to all of the patients except those with a medical contraindication against this use for anaesthesia due to allergy to this compound, a history of thrombotic events or coagulation pathologies, among others).
Finally a suture was made in two planes (fascial and subcutaneous) simultaneously by two surgeons, from the centre of the wound to its edges. The type of suture used depended on the results of randomisation: a control group with discontinuous polyglactin 910 suture, or the study group with continuous barbed suture (Quill®).
Closure in the control group followed the usual procedure, simultaneously by two surgeons who made discontinuous stitches in both planes. The type of suture studied is characterised by the presence of “barbs” which give rise to a unidirectional anchorage from the centre of the suture towards its ends, which means that closure has to commence at the centre of the wound and proceed towards the edges of the same. Once the thread has passed through tissue, the barbs make it possible to make a continuous and knot-free suture.7 A subfascial 10 mm silicon drainage channel with a vacuum reservoir was fitted in all of the patients and removed from 24−48 hrs. after the operation (after 24 h. by default and 48 h in the case of abundant discharge > 200 cc in 24 h). The skin was closed using staples in all cases.
All of the patients followed the same postoperative protocol. They started active and passive mobilisation exercises on the first day after the operation and commenced sitting on the first day and walking on the second day after surgery, increasing their activity every day until they were discharged on about the fourth day after the operation. All of the patients followed at least 10 sessions of out-patient rehabilitation, and loading was permitted from the first, without distinguishing between cemented or uncemented prostheses. Antithrombotic prophylaxis was maintained with subcutaneous enoxaparin at 40 mg/24 h for 30 days.
RandomisationPatients were assigned at random to one of two groups: the study group (Gr. Q) with continuous bidirectional barbed suture (Quill®) or the control group (Gr. V) with discontinuous polyglactin 910 (Vicryl®) type suture. This was done by using a system of sealed envelopes prior to surgery. Suturing was performed simultaneously in two planes (fascial and subcutaneous) by two surgeons, working from the centre of the wound to its edges. To correct the influence on time of using a new suture, all of the surgeons underwent a learning period, using the suture on at least 12 patients before the start of this study.
Discontinuous polyglactin 910 suture (Vycrill®, Ethicon, Somerville, NJ) was used in the control group. The study group used continuous barbed suture (Quill®, Angiotech, Vancouver, British Columbia, Canada). Size two suture was used to close the fascial plane and size zero was used for the subcutaneous plane in both groups.
The minimum follow-up time was one month (average duration 36 + -3.6 days). The main variables recorded were the time taken to close the wound in minutes (the fascia, subcutaneous plane and overall). Cases of suture breakage were also recorded (interruption of the suture with the continuous closer, which required finishing the closure with discontinuous stitches of conventional suture).
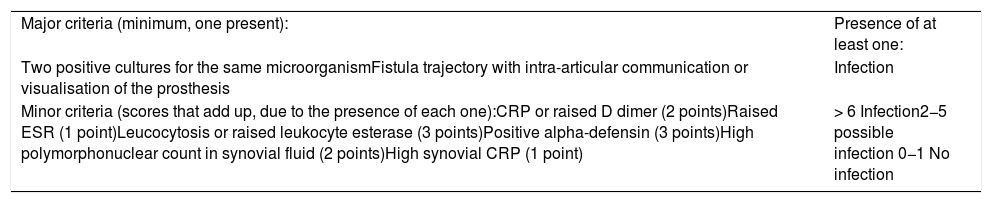
The secondary variables recorded were demographic data (age, sex, weight and height), coxarthrosis aetiology and type of prosthesis. The presence of surgical wound infection was also recorded (following the updated 2018 infection criteria of the Musculoskeletal Infection Society) (Table 1).
Updated Musculoskeletal Infection Society 2018 infection criteria.
| Major criteria (minimum, one present): | Presence of at least one: |
| Two positive cultures for the same microorganismFistula trajectory with intra-articular communication or visualisation of the prosthesis | Infection |
| Minor criteria (scores that add up, due to the presence of each one):CRP or raised D dimer (2 points)Raised ESR (1 point)Leucocytosis or raised leukocyte esterase (3 points)Positive alpha-defensin (3 points)High polymorphonuclear count in synovial fluid (2 points)High synovial CRP (1 point) | > 6 Infection2−5 possible infection 0−1 No infection |
CRP: C-reactive Protein; ESR: Erythrocyte sedimentation rate.
The exclusion criteria specified above were applied (previous surgery on the same hip, revision surgery, major deformities or allergies to suture components).
Statistical studyA previous statistical power study was performed, assuming 10% probable losses during follow-up. The sample size was calculated based on the results of previous studies2,9–14 and considering a sample of 33 patients to be the minimum for each group to achieve consistent results. Both groups were compared using the Student t-test for quantitative variables and χ2 for qualitative variables. A P value of < .05 was considered to be statistically significant. The SPSS v22® program was used for statistical analysis.
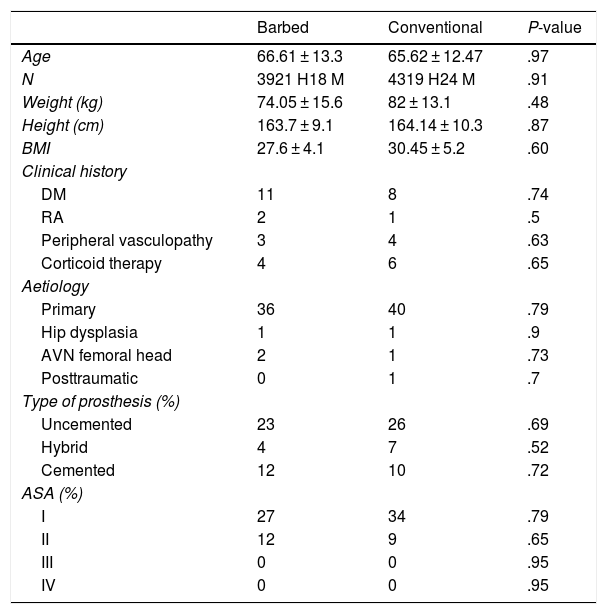
ResultsA total of 82 patients operated for THA (40 men/42 women) were included, 39 patients in the Quill® group (Gr. Q) and 43 in the Vycrill® group (Gr. V). Both groups were comparable for the variables studied (Table 2). For Gr. Q/Gr. V respectively the demographic variables recorded were: average age 66.6/65.2 years; weight 74.05/82 kg; height 163.7/164.14 cm; BMI 27.6/30.45. Regarding the aetiology of the coxarthrosis, in both groups the main cause was primary arthrosis (36 patients in Gr. Q, 40 in Gr. V), followed by dysplasia (one case in each group), avascular necrosis (AVN) (2 in Gr. Q, 1 in Gr. V) and posttraumatic (1 in Gr. V). An uncemented prosthesis was implanted in 23 cases in Gr. Q/26 in Gr. V, followed by a cemented prosthesis in 12 patients in Gr. Q/10 in Gr. V, and a hybrid prosthesis in four patients in Gr. Q/7 in Gr. V. Nor were differences detected between Gr. Q and Gr. V found respecting basal pathology/surgical risk, with 27 and 34 ASA i patients and 12 and 9 ASA ii patients, respectively.
Demographic variables and characteristics of the groups. Both were found to be comparable.
| Barbed | Conventional | P-value | |
|---|---|---|---|
| Age | 66.61 ± 13.3 | 65.62 ± 12.47 | .97 |
| N | 3921 H18 M | 4319 H24 M | .91 |
| Weight (kg) | 74.05 ± 15.6 | 82 ± 13.1 | .48 |
| Height (cm) | 163.7 ± 9.1 | 164.14 ± 10.3 | .87 |
| BMI | 27.6 ± 4.1 | 30.45 ± 5.2 | .60 |
| Clinical history | |||
| DM | 11 | 8 | .74 |
| RA | 2 | 1 | .5 |
| Peripheral vasculopathy | 3 | 4 | .63 |
| Corticoid therapy | 4 | 6 | .65 |
| Aetiology | |||
| Primary | 36 | 40 | .79 |
| Hip dysplasia | 1 | 1 | .9 |
| AVN femoral head | 2 | 1 | .73 |
| Posttraumatic | 0 | 1 | .7 |
| Type of prosthesis (%) | |||
| Uncemented | 23 | 26 | .69 |
| Hybrid | 4 | 7 | .52 |
| Cemented | 12 | 10 | .72 |
| ASA (%) | |||
| I | 27 | 34 | .79 |
| II | 12 | 9 | .65 |
| III | 0 | 0 | .95 |
| IV | 0 | 0 | .95 |
ASA: American Society of Anaesthesiologists; RA: Rheumatoid Arthritis; DM: Diabetes mellitus; BMI: Body Mass Index; AVN: Avascular necrosis.
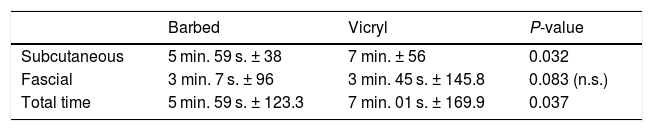
For the main variable studied the total duration of wound closure was found to be shorter in Gr. Q (5 min. 59 s.) than it was in Gr. V (7.01 min.), (P < .04). Nor were significant differences found in the time taken for subcutaneous closure: this was shorter in Gr. Q with 37 s difference (P = .048). No differences were found in fascial plane closure (Table 3).
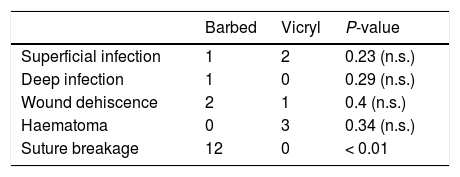
Respecting the secondary variables (Table 4), two cases of dehiscence were found in Gr. Q and one in Gr. V (defined as defective closure in > 2 cm following the removal of staples), with one case of superficial infection in Gr. Q and two in Gr. V. Only one patient in Gr. Q had a deep infection. These differences were not statistically significant.
Of the other incidents that were recorded, it should be pointed out that four cases of haematoma occurred in Gr. V with none in Gr. Q (P < .05). None of these cases went on to suffer an infection.
DiscussionAlthough the correct closure of the wound has been studied beforehand, the majority of works are retrospective studies on reducing closure time and the possible resulting advantages of this. Nevertheless, interpreting these results shows the limitation intrinsic to retrospective analysis of the results. This study analyses the results of using a barbed suture prospectively with closure time as the main variable and, secondarily, the appearance of complications.
The main finding of this study is that barbed suture significantly reduces the time taken to close the wound in hip surgery (1 min. 2 s. overall closure time). Other prospective studies published beforehand report the efficacy of this suture in reducing the said closure time in hip surgery,4,8,12,13 showing greater differences that those found in this work. The meta-analysis in 2015 by Borzio et al.4, which included four prospective studies with a total of 588 THA (290 in the Quill® study group and 298 in the Vicryl® group), found a closure time that was 5.4 min faster with barbed suture (where the total closure time was approx. 9.6 min. in gr. Q and 15 min. in gr. V). The work by Smith et al.14 shows similar results to the aforementioned one, with a saving of 9.72 min in comparison with traditional suture. The said studies indicate that if the fact that three surgical operations tend to be performed per day, the saving would amount to about 29 min, and this could be enough time to permit carrying out another procedure on the same day.
It could be thought that the marked difference between our times and those reported in the literature may be due to the closure technique. While in our study a bidirectional suture was performed simultaneously by two surgeons in both groups, in other works this procedure was only used for the Quill® suture. In these groups the traditional closure was made by a single surgeon who closed the wound from proximal to distal, giving rise to a slower closure as it was made by a single person.4
A controversial point arises in terms of the clinical significance of the limited saving of time observed in our study (about one minute. The authors of this study do not consider this shorter time in the implantation of THA will affect the result of this procedure. Based on our experience, it would not have the clinical importance expressed in other studies.4,8,14
The complications that could be attributed to the type of suture were analysed as a secondary objective. Factors such as the characteristics of the sample were analysed (age, sex, BMI and ASA), coxarthrosis aetiology, type of prosthesis and rehabilitation protocol and postoperative antithrombotic prophylaxis. No case of haematoma was found in Gr. Q in this study, while three cases were found in Gr. V. Although the differences were no significant, this tendency towards the less frequent appearance of haematomas would lead to considerations in favour of increasing the tension and better closing the planes.
Another secondary finding in this study was the theoretical advantage attributed to the barbed suture in terms of the incidence of dehiscence. In case of the failure or breakage of this type of suture, the “barbs” will function as anchors, resisting traction forces and keeping the suture under tension and in place. Regarding this point, in our experience this suture was not sufficient to prevent dehiscence (with two cases of dehiscence with a Quill® closure and one with conventional suture).
Another secondary variable in this study was the appearance of wound infection, which was similar in both groups. There was one case of superficial infection and one of deep infection in the study group, and these were treated by debridement and antibiotic therapy. Two cases of deep infection were found in the Vycrill® group, and these were treated in the same way. As is the case in earlier publications, we found no significant differences in terms of the development of wound infection depending on the use of one suture or the other.3,8,10,12 Nevertheless, in the study by Thacher et al.5 which analyses a broad sample (162 patients closed with barbed suture and 429 patients closed with Vycrill®), the barbed suture group was associated with a lower incidence of superficial infections compared to the conventional suture (0% vs 5.4%, respectively), as well as a higher incidence of dehiscence (3.1% vs 0.7%). Although this study is retrospective, it is characterised by its large sample in comparison with other prospective studies. Future prospective studies with larger samples may add to the evidence for this finding.
Lastly, the intraoperative incidents recorded with the use of barbed suture should be mentioned. The majority of these were breakage of the suture when closing the subcutaneous plane (10 subcutaneous and two fascial, P < .001). When the Quill® suture broke, the closure was terminated using the remnant until the plane was properly closed. If this was not possible, discontinuous Vycrill® stitches were added, which occurred in very few patients. Suture breakage was underlined in the meta-analyses by Borzio et al.4 and Gililland et al.9, in which 6% of sutures broke during the operation. The frequency of breakage observed in our study (31%) is higher. This may be due to less familiarity with the suture in question, even though each surgeon had been able to use it in at least 12 patients before commencing the study. The authors found that barbed suture has stronger closing power in more consistent tissue such as the fascial plane tissue, where the “barbs” are able to provide a more effective anchorage. However, this was not the case in the subcutaneous plane, where the connective tissue is less consistent and an effective closure cannot be ensured in case of suture breakage.
LimitationsThis study is not free of limitations. Although the limited size of the sample stands out in comparison with other studies, its strength lies in its prospective/randomised nature in making it possible to evaluate the benefits of using this new suture.
A limitation that should be underlined is the number of sutures used for each plane, as this was not recorded. In general, one Quill® suture or two Vycrill® ones were used for each plane in each patient. Nevertheless, cost analysis was included in our objectives.
As not only were two different types of suture used, because two different techniques were also employed, the real aim of the study was to confirm whether Quill® suture could offer any advantage over using traditional forms of closure in our hospital. Another limitation was patient follow-up, which was for a limited time. However, we consider it to be sufficient to observe the comparative results of the sutures, as well as any complications. Likewise, the presence of more than three different surgeons may be a distortion, although it also improve the external validity of the study.
ConclusionUse of a barbed suture slightly shortens the time taken for closure in comparison with conventional discontinuous suture. In spite of the shorter time for surgery that was observed, no differences were found in the presence of superficial or deep infections, wound dehiscence or haematoma, when closure with Quill® or Vycril® sutures were compared. These similar results would not justify recommending the use of one type of suture or the other.
Level of evidenceLevel of evidence
Please cite this article as: Serrano Chinchilla P, Gamba C, León García A, Tey Pons M, Marqués López F. Utilización de sutura barbada en prótesis total de cadera. Estudio prospectivo aleatorizado. Rev Esp Cir Ortop Traumatol. 2021;65:63–68.