Several US studies have investigated the criminal behaviour among homeless individuals with severe mental illness. But to date, no studies have been carried out in Spain.
MethodA retrospective observational study was conducted on a sample of 118 patients selected from a psychiatric care programme for homeless individuals with severe mental illness. Factors associated with criminal behaviour were analysed by comparing 2 groups, with and without criminal records.
ResultsOf the total sample studied, 24.6% had a criminal record, and 58.6% of them had entered prison. Significant differences between groups were found for the variables of gender, pending sentences, duration of homelessness, multiple substance use, disease awareness, and severity of psychotic symptoms.
ConclusionsIn the population of homeless individuals with severe mental illness, regardless of gender, the co-existence of comorbidity with multiple substance use, and a prolonged duration of homelessness, is the most important risk factor for criminal behaviour.
Varios estudios estadounidenses han investigado la conducta delictiva en las personas sin hogar con trastorno mental grave. Pero hasta la fecha ninguno se ha realizado en España.
MetodologíaEstudio observacional retrospectivo, en una muestra de 118 pacientes, seleccionados de un programa de atención psiquiátrica para personas sin hogar con trastorno mental grave. Se analizaron los factores asociados a la conducta delictiva mediante la comparación de 2 grupos, con y sin antecedentes penales.
ResultadosEl 24,6% de la muestra tenía algún antecedente penal y el 58,6% de este grupo había ingresado en prisión. Se encontraron diferencias significativas entre ambos grupos para las variables: sexo, condenas pendientes, duración del sinhogarismo, comorbilidad con politoxicomanía, conciencia de enfermedad y gravedad de los síntomas psicóticos.
ConclusionesEn la población de personas sin hogar con trastorno mental grave, con independencia del sexo, la coexistencia de comorbilidad con politoxicomanía y una duración prolongada del sinhogarismo, constituyen el factor de riesgo más importante para la conducta delictiva.
Lack of housing is a significant social and health problem in Spain. The data obtained in the last survey conducted by the Spanish National Statistics Institute1 showed that the population of homeless individuals (HI) in Spain–attended to at accommodation and catering care facilities–in 2012 was 22,938 people. With population distributed by Autonomous Community, Catalonia (21.3%), Community of Madrid (15.4%) and Andalusia (13.1%) have the highest percentages. And, specifically, in the municipality of Madrid, in December 2014, the “VII Homeless Individuals Night Count”2 was carried out, in which 764 people “without a roof” (i.e., who were spending the night on the street) were detected.
At present, epidemiological studies report that between 20% and 40% of HI suffer from a severe mental illness (SMI).1,3 The social exclusion suffered by this population is a complex phenomenon, which is linked to situations of family and social uprooting, unemployment, severe poverty, personal and social deterioration, etc.; which in turn is associated with greater participation in the criminal justice system (arrests, convictions and imprisonment).3
Increasingly in Spain, media coverage of violent incidents often depicts HI with SMI as perpetrators of crimes. These events continually draw public attention to the complex interaction between homelessness, SMI and criminal behaviour.
In the last 15 years, several studies3 have been carried out to find out about potential criminal behaviour in HI with SMI, in the USA,4–10 and to a lesser extent in the United Kingdom.11
Another phenomenon tangentially related to criminal behaviour is the “criminalisation”3 of HI in general and of the mentally ill, in particular. This phenomenon pertains to the growing social tendency to criminalise disorderly conduct due to mental health, diverting people with mental illness towards the judicial and prison systems.
But, obviously, the data provided in this regard are difficult to transpose to the Spanish reality, both socially (legislation, rules about action procedures of the police and judges, etc.) and culturally (tolerance to deviation from social norms, etc.). And, to date, no study has been conducted on a Spanish sample that analyses this phenomenon in the specific population of HI with SMI.
ObjectivesThe main objective of the study was to analyse the factors associated with criminal behaviour in the HI population with SMI, by comparing 2 groups, with and without criminal records, from a sample of this social group.
Material and methodsA retrospective, naturalistic observational study conducted in a sample of HI with SMI attending the “Psychiatric Care Programme for the Homeless Mentally Ill” in Madrid.12
The aforementioned programme provides social, health and psychiatric care to all HI located in the municipality of Madrid, who are of legal age, who have an SMI and who, due to various circumstances, are not monitored by the Standard Mental Health Network.
The criterion for designating an individual as an HI is established by the European Federation of National Organisations Working with the Homeless (FEANTSA) based on ETHOS (European Typology of Homelessness and Housing Exclusion).13 It states the following: “People who cannot access or retain adequate accommodation that is adapted to their personal situation, that is permanent, and that provides a stable living environment, either due to economic reasons or other social barriers, or because they have personal difficulties with leading an autonomous lifestyle”.
The criterion for designating an individual as having an SMI is established by the United States’ National Institute of Mental Health (NIMH),14 which defines this social group as: “A group of heterogeneous individuals, who suffer from severe psychiatric illnesses, identified by mental illnesses of prolonged duration, which involve a variable degree of disability and social dysfunction, and which have to be attended to with various social and health resources in the psychiatric and social health care network”.
For the purposes of the “Psychiatric Care Programme for the Homeless Mentally Ill” the diagnostic categories (ICD-10)15 included under SMI are: schizophrenic disorders (F20.x), persistent delusional disorders (F22.x), induced delusional disorders (F24.x), schizoaffective disorders (F25.x), other non-organic psychotic disorders (F28 and F29.x), bipolar affective disorder (F31.x), severe depressive episode with psychotic symptoms (F32.3.x), recurrent depressive disorders (F33), obsessive-compulsive disorder (F42.x), schizotypal personality disorder (F21.x) and severe personality disorder (F60.x).
Finally, although it is based on the premise that slightly less than half of the HI who suffer from an SMI may exhibit harmful consumption of alcohol or other substances, the programme does not include those individuals who only present with an abuse and dependence on toxic substances (including alcohol) disorder.
The study sample was chosen from the total number of patients who had undergone psychiatric monitoring in the “Psychiatric Care Programme for the Homeless Mentally Ill” in Madrid (Spain), between 2010 and 2015. A total of 186 medical histories were reviewed, and those that had all the clinical and socio-demographic data filled in for all the items present in the medical history protocol of the programme were chosen. In total, 118 individuals were chosen. From this sample, 2 groups were chosen according to whether or not they had a criminal record mentioned in their history.
The following were used as inclusion criteria for the study: 1) HI with SMI; 2) monitoring initiated in the “Psychiatric Care Programme for the Homeless Mentally Ill” between 2010 and 2015; and 3) all necessary information regarding the main variables of the study available.
The main variable of the study was the existence (or not) of criminal behaviour (at the time of inclusion in the programme), which was identified by the existence, or not, of a criminal record in their medical history (i.e., an official record stating that a person has been sentenced for committing a crime). This is the definition regulated by the Spanish Criminal Code.16
In the case of subjects with a criminal record, the reason for the conviction and seriousness of the crime (“mild” for minor offences and “serious” for crimes classified as serious and less serious) were also included as study variables in accordance with the Spanish Criminal Code.17
In addition, the following socio-demographic and clinical variables were collected from all subjects: gender, nationality, place of origin, type of living environment before homelessness, years of evolution of homelessness, typology of homelessness (according to ETHOS13), educational level reached, best profession reached, existence of pending convictions, victim of crime, co-morbidity with a history of consumption of toxic substances (dependence syndrome; F1x.3 of the ICD-1015), co-morbidity with poly-drug use (disorders due to multiple drug use; F19 of the ICD-1015), main diagnosis (ICD-10),15 years of evolution of the mental illness, form of evolution of the mental illness, previous contact with Mental Health services, previous psychiatric hospitalisation, recognition of the degree of disability, civil incapacity, co-morbidity with infectious disease, co-morbidity with severe somatic disease, disease awareness, attitude towards pharmacological treatment, severity of somatic, psychotic, depressive and anxiety symptoms (Likert-type scale of 7 degrees of intensity: 0=not assessable, 1=normal, 2=unclear, 3=mild, 4=moderate, 5=pronounced, 6=severe, 7=extreme). All the variables corresponded to the time of inclusion in the programme.
The source of the information was the medical histories of the patients included in the study sample. Based on these histories, an anonymised form was filled in for each patient (generating an anonymised database). The group of patients “with a criminal record” consisted of 29 individuals, and the group “without a criminal record” consisted of 89.
Statistical analysisThe qualitative variables were expressed by their frequency distribution and the quantitative variables (normally distributed) by their mean±standard deviation (SD).
For the comparison between the quantitative variables of the 2 study groups, Student's t-test (or non-parametric Mann–Whitney U test) was used. In the case of qualitative variables, the comparison between groups was assessed using the χ2 test (or Fisher's exact test if more than 25% of the expected values were less than 5).
Subsequently, a logistic regression analysis was carried out with a forward stepwise selection method (Wald) considering the existence, or not, of a criminal record as a dependent variable; and as independent variables those that showed statistical significance in their univariate association with the main variable (criminal record). This technique creates a probabilistic model that allows for estimation of the risk (through odds ratio [OR] provided by the model) that involves the different values of independent variables on a dichotomous dependent variable (existence, or not, of a criminal record). In our case, the use of this technique identifies the factors that may be associated with a criminal record.
For all of these tests, the accepted level of significance was 5%. Data was processed and analysed using the SPSS statistical package version 15.0 for Windows (SPSS, Chicago, IL, USA).
This study was carried out with the approval of the Independent Ethics Committee (IEC) of the Hospital Clínico San Carlos de Madrid, fulfilling all the requirements of the Declaration of Helsinki and Spanish legislation on data protection.
ResultsCriminal recordIn the descriptive analysis of the HI with SMI sample (No.=118) it was found that up to 24.6% (n=29) had some criminal record (at the time of inclusion in the programme), and, of these, 58.6% (n=17) had been to prison at least once.
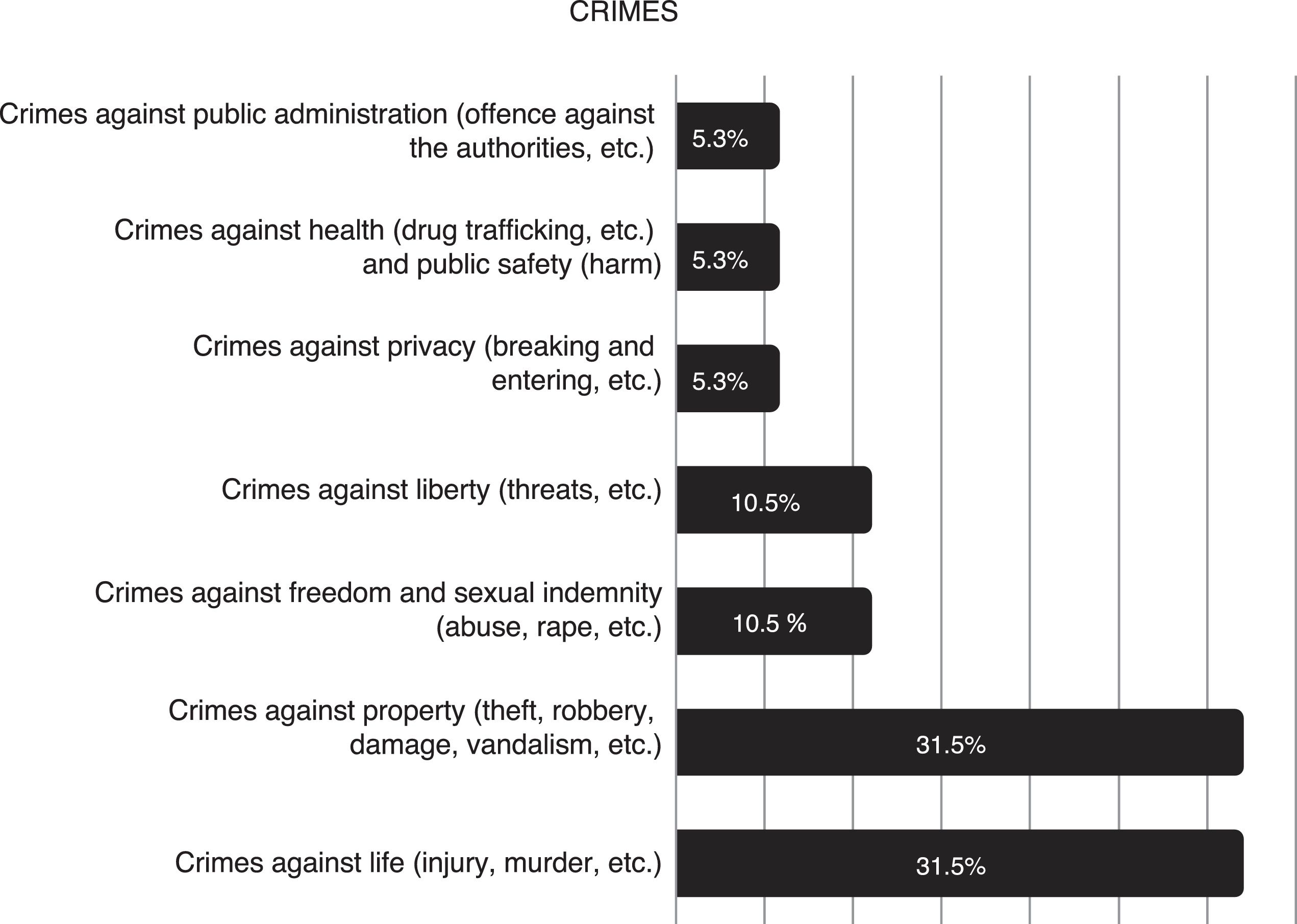
The descriptive analysis of the group of HI with SMI with a “criminal record” is shown in Table 1. And the typology of the crimes for which they had been convicted is shown in Fig. 1.
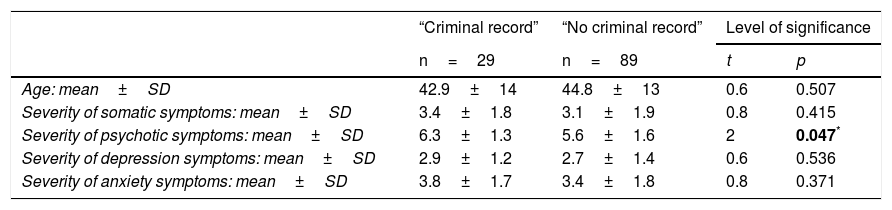
Differences between patients with and without a criminal record for socio-demographic and clinical variables.
| “Criminal record” | “No criminal record” | Level of significance | ||
|---|---|---|---|---|
| n=29 | n=89 | t | p | |
| Age: mean±SD | 42.9±14 | 44.8±13 | 0.6 | 0.507 |
| Severity of somatic symptoms: mean±SD | 3.4±1.8 | 3.1±1.9 | 0.8 | 0.415 |
| Severity of psychotic symptoms: mean±SD | 6.3±1.3 | 5.6±1.6 | 2 | 0.047* |
| Severity of depression symptoms: mean±SD | 2.9±1.2 | 2.7±1.4 | 0.6 | 0.536 |
| Severity of anxiety symptoms: mean±SD | 3.8±1.7 | 3.4±1.8 | 0.8 | 0.371 |
| Count (%) | Count (%) | χ2 | p | |
|---|---|---|---|---|
| Previous prison sentence | 61 | <0.001* | ||
| Yes | 17 (58.6) | 0 (0) | ||
| No | 12 (41.4) | 89 (100) | ||
| Pending convictions | 16.1 | 0.001* | ||
| Yes | 5 (17.2) | 0 (0) | ||
| No | 24 (82.8) | 89 (100) | ||
| Gender | 13.1 | 0.001* | ||
| Male | 27 (93.1) | 50 (56.02) | ||
| Female | 2 (6.9) | 39 (43.8) | ||
| Nationality | 0.4 | 0.527 | ||
| Spanish | 16 (55.2) | 55 (61.8) | ||
| Foreign | 13 (44.8) | 34 (38.2) | ||
| Origin | 1.3 | 0.518 | ||
| Europe | 23 (79.3) | 64 (71.9) | ||
| Africa | 5 (17.2) | 16 (18) | ||
| America | 1 (3.4) | 9 (10.1) | ||
| Type of living environment before homelessness | 2 | 0.373 | ||
| Lived with family | 14 (48.3) | 56 (62.9) | ||
| Lived alone | 6 (20.7) | 14 (15.7) | ||
| Institution (or other) | 9 (31) | 19 (21.3) | ||
| Years of evolution of homelessness | 3.6 | 0.050* | ||
| One year or less | 6 (20.7) | 7 (7.9) | ||
| More than one year | 23 (79.3) | 82 (91.2) | ||
| Typology of homelessness | 1.4 | 0.271 | ||
| Rooflessness | 21 (72.4) | 53 (59.6) | ||
| Homelessness | 8 (27.6) | 36 (40.4) | ||
| Education level reached | 3.6 | 0.157 | ||
| Illiterate | 4 (13.8) | 4 (4.5) | ||
| Basic education | 24 (82.8) | 77 (86.5) | ||
| University education | 1 (3.4) | 8 (9) | ||
| Best profession reached | 1.5 | 0.483 | ||
| No known work | 14 (48.3) | 32 (36) | ||
| Unqualified | 5 (17.2) | 17 (19.1) | ||
| Qualified | 10 (34.5) | 40 (44.9) | ||
| Victim of crime | 0.9 | 0.450 | ||
| Yes | 1 (3.4) | 8 (9) | ||
| No | 28 (96.6) | 81 (91) | ||
| Toxic substance dependency | 4.2 | 0.054 | ||
| Yes | 20 (69) | 42 (47.2) | ||
| No | 9 (31) | 47 (52.8) | ||
| Poly-drug use | 10.5 | 0.003* | ||
| Yes | 12 (41.4) | 12 (13.5) | ||
| No | 17 (58.6) | 77 (86.5) | ||
| Main diagnosis | 3.6 | 0.443 | ||
| Schizophrenia | 16 (55.2) | 41 (46.1) | ||
| Delusional disorder | 2 (6.9) | 14 (15.7) | ||
| Bipolar disorder | 3 (10.3) | 4 (4.5) | ||
| Personality disorder | 8 (10.3) | 7 (7.9) | ||
| Other (or not related) | 5 (17.2) | 23 (25.8) | ||
| Years of evolution of mental illness | 0.1 | 0.825 | ||
| One year or less | 11 (37.9) | 31 (34.8) | ||
| More than one year | 18 (62.1) | 58 (65.2) | ||
| Form of evolution of mental illness | 1.1 | 0.197 | ||
| Episodic | 14 (48.3) | 33 (37.1) | ||
| Continued evolution | 15 (51.7) | 56 (62.9) | ||
| Previous contact with Mental Health | 2.2 | 0.170 | ||
| Yes | 23 (79.7) | 57 (64) | ||
| No | 6 (20.7) | 32 (36) | ||
| Previous psychiatric hospitalisation | 0.6 | 0.510 | ||
| Yes | 20 (69) | 54 (60.7) | ||
| No | 9 (31) | 35 (39.3) | ||
| Recognition of the degree of disability | 0.1 | 0.744 | ||
| Yes | 4 (13.8) | 10 (11.2) | ||
| No | 25 (86.2) | 79 (88.8) | ||
| Civil incapacity | 0.4 | 0.415 | ||
| Yes | 1 (3.4) | 6 (6.7) | ||
| No | 28 (96.6) | 83 (93.3) | ||
| Co-morbidity with infectious disease | 2 | 0.175 | ||
| Yes | 8 (27.6) | 14 (15.7) | ||
| No | 21 (72.4) | 75 (84.3) | ||
| Co-morbidity with severe somatic disease | 0.7 | 0.690 | ||
| Yes | 13 (44.8) | 34 (34.2) | ||
| No | 16 (55.2) | 55 (65.8) | ||
| Disease awareness | 4 | 0.047* | ||
| No (or unknown) | 29 (100) | 78 (87.6) | ||
| Yes | 0 | 11 (12.4) | ||
| Attitude towards pharmacological treatment | 0.9 | 0.380 | ||
| Totally negative | 8 (27.6) | 33 (37.1) | ||
| Accepting | 21 (72.4) | 56 (62.9) | ||
In the comparative analysis of both groups (Table 1), “with a criminal record” and “without a criminal record”, statistically significant differences were observed in: the existence of pending convictions, gender, years of evolution of homelessness, co-morbidity with poly-drug use, disease awareness and severity of psychotic symptoms. Whereas no significant differences were found for the rest of the variables analysed in the study.
Logistic regression modelThe model obtained with the logistic regression showed a good fit (χ2 Hosmer–Lemeshow=0.324; gl=; p=0.956), correctly classifying 82.2% of the sample with a sensitivity of 97.4% and a specificity of 20.7% with a cut-off value of 0.5 in the regression equation. The 3 variables included in the model were: gender (χ2 Wald=8.27; gl=1; p=0.004); years of evolution of homelessness (χ2 Wald=.17; gl=1; p=0.023) and history of poly-drug use (χ2 Wald=8.46; gl=1; p=0.003).
The ORs for these variables showed that being male as opposed to female increased the risk of having a criminal record ninefold (OR=9.31; 95% CI=2–42.7). A duration of homelessness of more than a year increased the risk up to fivefold (OR=5.03; 95% CI=1.2–20.1). And co-morbidity with poly-drug use quadrupled said risk (OR=4.37; 95% CI=1.2–11.7).
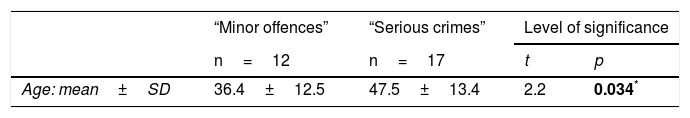
Serious crimes and minor offencesFinally, it was observed that of the HI with SMI who had a criminal record, 58.6% (n=17) had been convicted for “serious crimes” (which corresponded to 14% of the total sample); as opposed to 41.4% (n=12) for “minor offences”.
In the comparison of both groups (“serious crimes” and “minor offences”), statistically significant differences were found in (Table 2): age (p=0.034; t=2.2); in the “serious crimes” group the mean age was 47.5±13.4 years, while in the “minor offences” group it was 36.4±12.5 years. And nationality (p=0.008; χ2=9.7); with 17.6% (n=3) foreigners in the “serious crimes” group as opposed to 75% (n=9) foreigners in the “minor offences” group. And, although it was not statistically significant, a significant trend was found (p=0.08; χ2=12.1) (Table 2) of a greater frequency of “crimes against life (injuries, murder, etc.)” (23.5%; n=4) in the “serious crimes” group; and a greater frequency of “crimes against property (theft, robbery, damage, vandalism, etc.” in the “minor offences” group (33.3%; n=4). Finally, no significant differences were found between the two groups for the rest of the variables: gender (p=0.218; χ2=1.5), place of origin (p=0.123; χ2=4.1), type of living environment before homelessness (p=0.125; χ2=7.3), years of evolution of homelessness (p=0.289; χ2=2.5), typology of homelessness (p=0.793; χ2=0.1), level of education (p=0.430; χ2=1.7), profession (p=0.374; χ2=1.9), pending convictions (p=0.286; χ2=1.1), victim of crime (p=0.393; χ2=1.7), co-morbidity with consumption of toxic substances (p=0.822; χ2=0.1), co-morbidity with poly-drug use (p=0.460; χ2=0.5), main diagnosis (p=0.904; χ2=1), years of evolution of mental illness (p=0.260; χ2=1.2), form of evolution of mental illness (p=0.876; χ2=0.1), previous contact with mental health (p=0.158; χ2=1.9), previous psychiatric hospitalisation (p=0.555; χ2=0.3), recognition of the degree of disability (p=0.141; χ2=2.1), disability (p=0.226; χ2=1.4), co-morbidity with severe infectious or somatic disease (p=0.394; χ2=5.1 and p=0.534; χ2=0.1; respectively), disease awareness (p=0.119; χ2=2.4), attitude towards pharmacological treatment (p=0.793; χ2=0.1) and severity of somatic, psychotic, depressive and anxiety symptoms (p=0.161; t=2.1; p=0.823; t=0.2; p=0.225; t=1.2 and p=0.179; t=1.3, respectively).
Significant differences between patients with “minor offences” and “serious crimes”.
| “Minor offences” | “Serious crimes” | Level of significance | ||
|---|---|---|---|---|
| n=12 | n=17 | t | p | |
| Age: mean±SD | 36.4±12.5 | 47.5±13.4 | 2.2 | 0.034* |
| Count (%) | Count (%) | χ2 | p | |
|---|---|---|---|---|
| Age range | 6.2 | 0.04* | ||
| Between 18 and 35 years of age | 8 (66.7) | 3 (17.6) | ||
| Between 36 and 55 years of age | 3 (25) | 10 (58.8) | ||
| Aged over 55 years | 1 (8.3) | 4 (23.5) | ||
| Nationality | 9.7 | 0.008* | ||
| Foreign | 9 (75) | 3 (17.6) | ||
| Spanish | 3 (25) | 14 (82.4) | ||
| Type of crime | 12.2 | 0.080 | ||
| Against life | 2 (16.7) | 4 (23.5) | ||
| Against property | 4 (33.3) | 2 (11.8) | ||
| Against sexual indemnity | 1 (8.3) | 1 (5.9) | ||
| Against liberty | 2 (16.7) | 0 (0) | ||
| Against privacy | 1 (8.3) | 0 (0) | ||
| Against safety and public well-being | 0 (0) | 1 (5.9) | ||
| Against public administration | 1 (8.3) | 0 (0) | ||
| Other, multiple or unknown | 1 (8.3) | 9 (52.9) | ||
The main finding of this study is that in the population of HI with SMI, regardless of gender, the coexistence of poly-drug use with a duration of homelessness greater than a year is the most significant risk factor for criminal behaviour, unlike these conditions independently and other social and clinical factors.
Duration of homelessnessIn this sense, in our sample, a duration of homelessness of greater than one year increased the risk of criminal behaviour up to fivefold. This finding is very relevant since, typically, there has been a tendency to pay less attention to contextual factors than to clinical risk factors in studies on the relationship between mental illness and criminal behaviour.3 While it is true that in a previous study conducted in the United States3,11 it has been suggested that in terms of participation in the criminal justice system (arrests, convictions and imprisonment), HI with SMI tend to be more similar to the general HI population than to the general population of individuals with SMI. And this may be due to the fact that when people with SMI have no home, and are therefore visible in the public space, they are more likely to attract the attention of the public and of the security forces and, therefore, to be arrested more frequently.18 However, all conclusions should be considered tentative given the scant available studies.3
Poly-drug useFurthermore, in our sample, co-morbidity with poly-drug use quadrupled the risk of criminal behaviour. So, just as has been consistently replicated in all the previous scientific literature in this regard,3 poly-drug use is a differential factor between both groups (“with a criminal record” and “without a criminal record”). In fact, many studies on the general population of adults with SMI have found that substance abuse is the main cause of crime and not mental illness in itself.19–23 And, in this sense, it is possible that for the HI population with SMI, several causal pathways underlie the relationship between poly-drug use and the existence of a criminal record; such as, for example, that the disinhibition effect of drug and alcohol abuse may cause some HI with SMI to exhibit problematic behaviour on the street, thereby increasing the risk of criminal altercations.3,18
Criminal behaviour ratesAnother finding that our study draws attention to is that almost a quarter of the HI with SMI in the municipality of Madrid (up to 24.6%) had a criminal record; these rates are lower than those observed in other international studies with the same population (mainly in the USA), where rates range between 28.1 and 80.0%.3 And, although the lowest rates found in other studies conducted in the United States are close to those found in our study, it should be noted that, in the case of the lowest rate19 (28.1%), it only represents convictions for serious crimes, which in the study of our sample would be considerably lower – i.e. 14.4%. This observed difference was expected, and is explained by the fact that the previous studies published refer to cities in the US states (New York,10 California,7 Washington,8 Florida4 and Missouri5), where criminalisation of the homeless mentally ill comes from having been a socio-health and legal problem for a few decades.
GenderWith regard to gender, it was foreseeable that being male (compared to being female) markedly increased the risk of having a criminal record, as has been described in all the previous literature on this matter.24
Associated psychopathologyFrom the psychopathological point of view, it was observed that the group of HI with SMI and “with a criminal record” presented a greater apparent severity of psychotic symptoms in relation to the group of HI with SMI “without a criminal record”. These findings would be in line with other studies on criminal behaviour, where the presence and intensity of psychotic symptoms has been related to a pattern of delinquency associated with situations of homelessness, mainly when it is linked to the consumption of toxic substances.25
This psychopathological context consequently explains that criminal behaviour is also associated with a lower awareness of illness; with none of the patients in the “criminal record” group having an adequate awareness of their illness. Although, paradoxically, 72.4% of them agreed to undergo pharmacological treatment, which is explained because a large part of them were complying with involuntary outpatient treatment as a safety measure.
Open criminal justice casesAnother difference found in the “criminal record” group was the coexistence of pending (or open) criminal justice cases; which would support the existence of the “revolving door” phenomenon. This consists of the mentally ill subjected to safety measures being recidivists in the commission of criminal acts (usually minor), so that they come and go (often almost unceasingly) to and from the penal/prison system.26 In this regard, in the relevant scientific literature it has also been found that the number of previous convictions is one of the most common predictors of recidivism among offenders with and without SMI.3
CriminalisationFinally, in the study on the type of crime, the analysis of the “minor offences” group, which involved just under half of the patients with a criminal record, can provide information about the phenomenon of criminalisation. It appears that an HI with SMI is more susceptible to being accused of a minor offence3 compared to the general population. And, accordingly, it appears that foreign nationality and youth is associated with more frequent minor offences, as has also been described in other studies.
ConclusionsIn the population of HI with SMI, regardless of gender, the coexistence of poly-drug use with a prolonged duration of homelessness is the most significant risk factor for criminal behaviour, unlike these conditions independently and other social, as well as clinical, factors.
A greater severity of psychotic symptoms, as well as a lower awareness of illness in HI with SMI and “with a criminal record” indicates (as a minimum) the need to establish adequate medical-psychiatric treatment in this population.
Of particular importance is the coexistence of pending criminal justice cases, which highlights the current prevailing problem of the “revolving door” phenomenon of the mentally ill (and specifically those who are socially excluded) in the judicial/prison system.
Finally, foreign nationality and youth are emerging as possible factors in addition to criminalisation of the HI with SMI social group, and these factors should be taken into account in future studies.
All these results implicitly reveal the need for an integral and multidisciplinary, socio-health approach to this stigmatised social group of HI with SMI, as well as closer coordination with the criminal justice and prison domains.
Limitations of the studyThis is a retrospective study with a sample selection based on quality of data from medical records, which means that these results cannot be easily generalised.
This retrospective nature implies that there may be an under-recording of data relative to criminal records, although the selection of the sample based on the completion of all the items of the medical history would partially limit this bias.
FundingThis study has been done by our own means with no external funding.
Conflicts of interestThe authors state that there are no conflicts of interest.
To Dr María Vázquez Souza, the psychiatrist who launched and developed the “Psychiatric Care Programme for the Homeless Mentally Ill” in Madrid.
In memory of Dr Cristina García-Andrade Domínguez, a forensic doctor with extraordinary and admirable talent, both professionally and with regard to humanity.
Please cite this article as: Fernández García-Andrade R, Serván Rendón-Luna B, Medina Téllez de Meneses E, Vidal Martínez V, Bravo Ortiz MF, Reneses Prieto B. Conducta delictiva en las personas sin hogar (PSH) con trastorno mental grave (TMG). Rev Esp Med Legal. 2018;44:55–63.