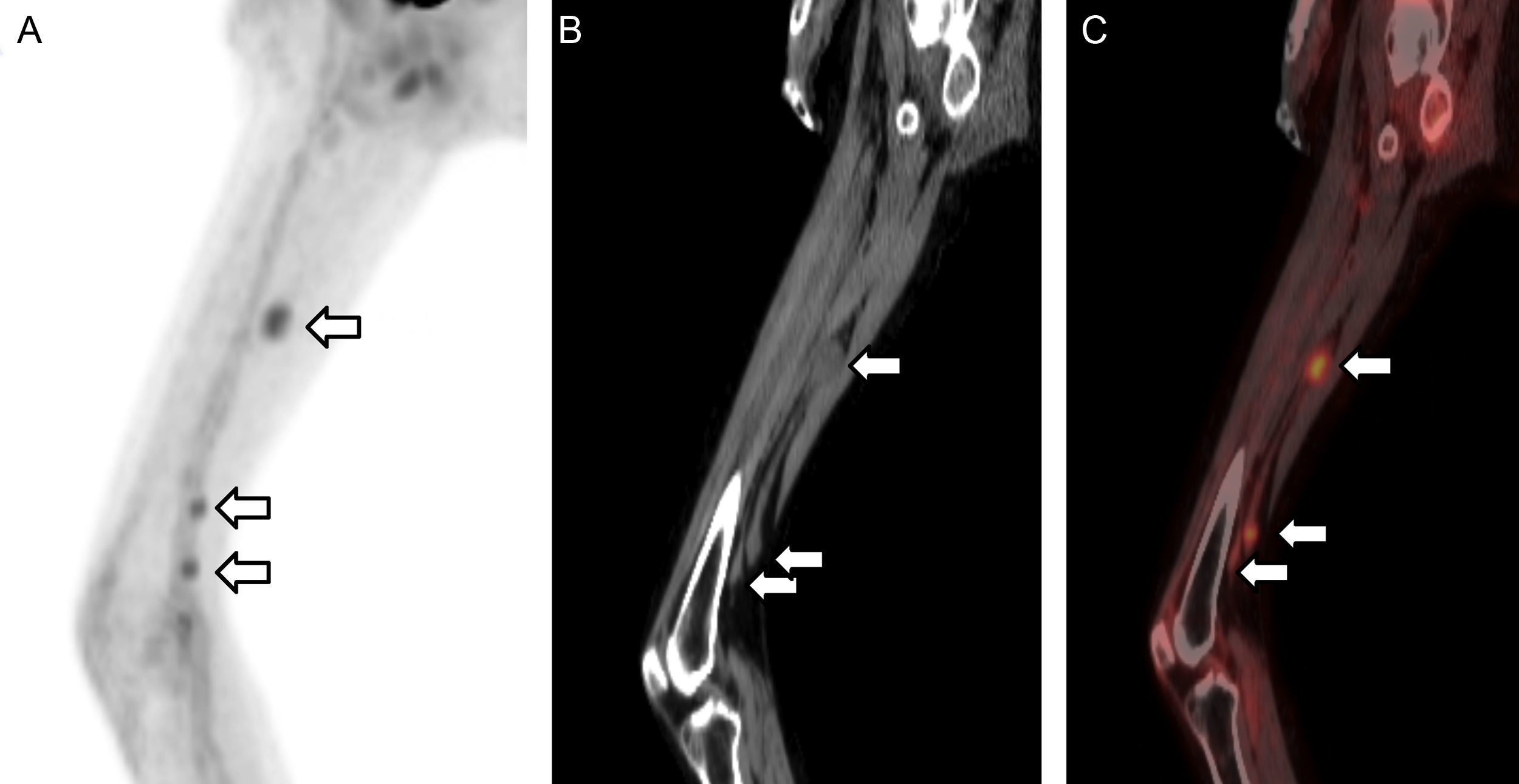
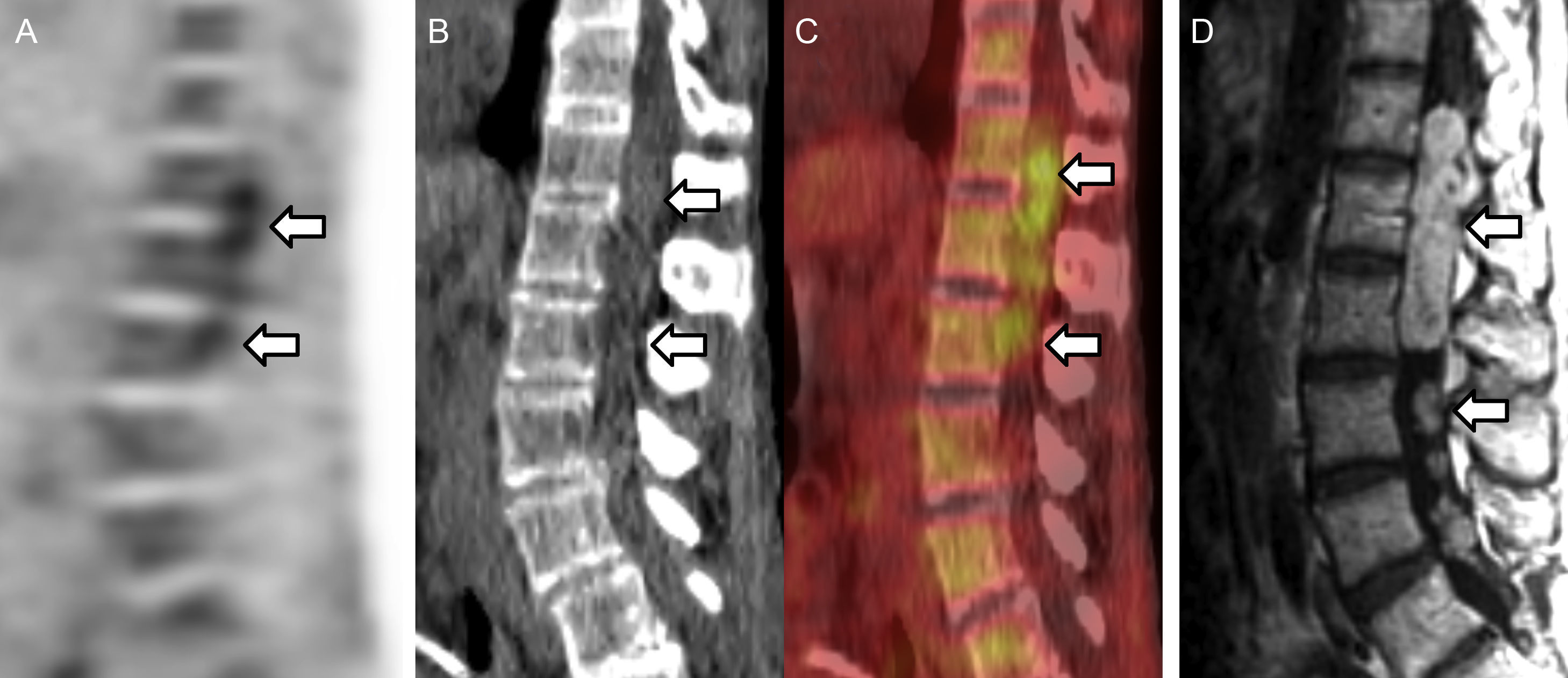
We present a patient with neurocutaneous syndrome, status prior resections for cervical schwannomas and median as well as radial nerve schwannomas. This is a 57-year-old female with neurocutaneous syndrome presenting at 42 years of age with unilateral vestibular schwannoma. Genetic testing was negative but on clinical criteria neurofibromatosis-2 (NF-2) or schwannomatosis were considered.1 She underwent FDG PET/CT 85min after intravenous injection of 11.3mCi (418.1MBq) FDG, for recent onset of severe left back pain with suspected cauda equina compression. Whole-body FDG PET/CT showed multiple FDG avid soft tissue foci overlying the sciatic nerve, consistent with multiple schwannomas (Fig. 1). It also demonstrated heterogenous uptake corresponding to multiple lesions visualized on MRI (Fig. 2).
Whole-body FDG PET/CT showed (A–C) a series of FDG avid lesions overlying the left sciatic nerve (arrows) confirmed on MRI measuring up to 2.7cm×2.2cm and SUVmax whole body weight of 3.3, 3.2 and 3.1. In addition, hypermetabolic lesions were seen in left axilla and right shoulder (SUVmax of. 4.6 and 4.3, respectively), consistent with schwannomas on MRI (data not shown).
Schwannomatosis can be hard to differentiate from NF-2 and some authors suggested that vestibular schwannomas utilized in the Manchester criteria,1 should not be an exclusion criterion for the diagnosis of schwannomatosis. NF-2 is a rare autosomal dominant syndrome that may have MERLIN gene mutation and/or characterized by vestibular schwannomas, and other schwannomas, multiple meningiomas, ependymoma and lens opacities. Neurofibromatosis type 1 (NF-1), on the other hand, is a different disease with a few overlapping features.1 In contrast to NF-2 where malignant transformation is rare, NF-1 has 10% cumulative incidence of malignant transformation2 thus several reports have described the use of FDG in NF-1 to differentiate between benign peripheral nerve sheath tumors (PNST) and malignant PNST.
Our report is unique in showing histologically proven intra spinal canal schwannomas associated with neurocutaneous syndrome related to NF-2 or schwannomatosis. FDG uptake was in the range described for benign PNST and some malignant PNST. In our patient, given that there are multiple sites with same intensity of FDG uptake malignant transformation of any lesion was unlikely. This rare case also illustrates why close attention should be paid to the spinal canal (Fig. 2A–D) in these patients, since these lesions can easily be mistaken for physiologic uptake in the distal spinal cord. Furthermore FDG may detect other sites of schwannomas, as seen in this patient's sciatic nerve.
A single case report of FDG uptake in an intraspinal canal schwannoma has been reported.3
Because these lesions were consistent with her pain distribution, she underwent T11-L2 partial laminectomy and removal of histologically confirmed benign intradural schwannomas, with resolution of pain symptoms.
Please cite this article as: Beylergil V., et al. Schwannomatosis/neurofibromatosis tipo 2 en FDG PET/TC de un paciente con múltiples schwannomas. 2013. http://dx.doi.org/.