Journal Information
Share
Download PDF
More article options
Clinical report
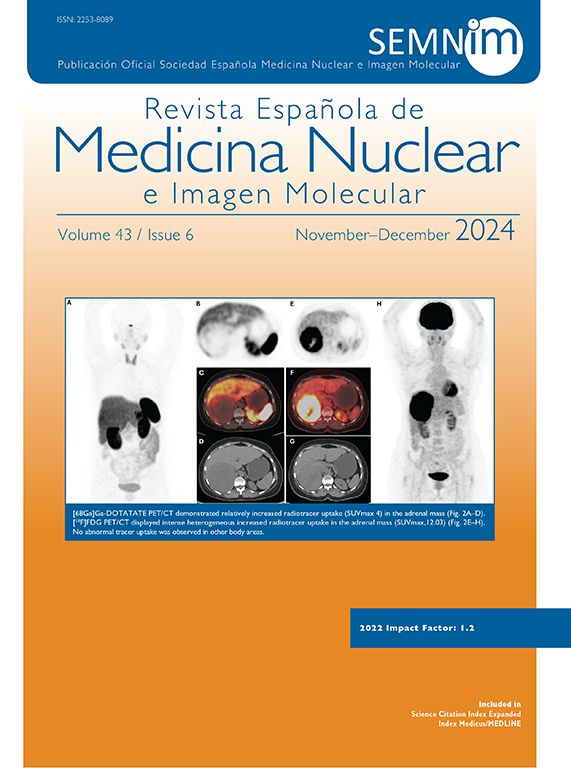
Is it possible NET-redifferentiation after chemotherapy? Ga68 DOTA-peptide imaging as a game-changer in therapy management
¿Es posible la rediferenciación de NET tras la quimioterapia? Captación de imágenes de DOTA-Péptidos marcados con Ga68 como cambio de estrategia en el tratamiento terapéutico
a Clinic of Nuclear Medicine, Istanbul Training and Research Hospital, Kasap İlyas Mah. Org. Abdurrahman Nafiz Gürman Cd., 34098 Fatih, Istanbul, Turkey
b University of Health Sciences, Clinic of Nuclear Medicine, Istanbul Training and Research Hospital, Kasap İlyas Mah. Org. Abdurrahman Nafiz Gürman Cd., 34098 Fatih, Istanbul, Turkey
c Clinic of Pathology, Istanbul Training and Research Hospital, Kasap İlyas Mah. Org. Abdurrahman Nafiz Gürman Cd., 34098 Fatih, Istanbul, Turkey