Journal Information
Statistics
Follow this link to access the full text of the article
Interesting images
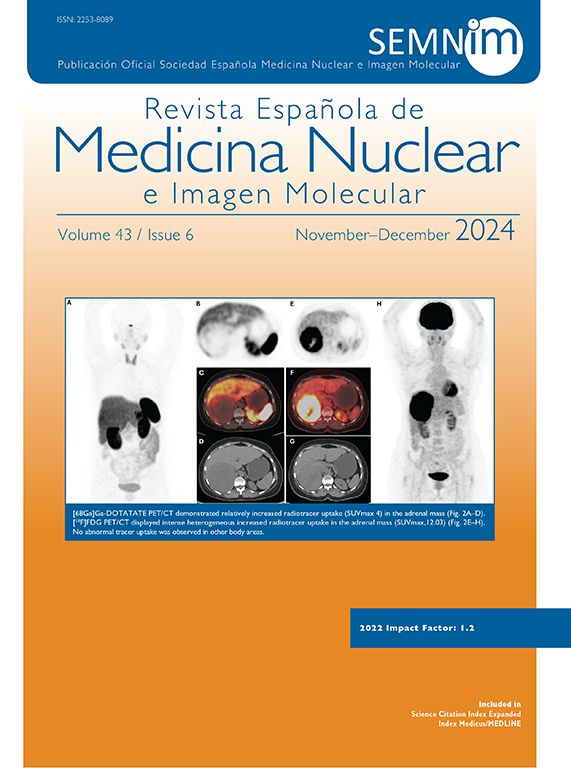
Malignant somatic transformation arising from teratoma in metastatic testicular germ cell tumor detected on 18F-FDG PET/CT
Transformación somática maligna derivada de un teratoma en un tumor testicular metastásico de células germinales detectado mediante PET/TC con 18F-FDG
Rodrigo Cárdenas-Perilla
Nuclear Medicine Department, Clínica Imbanaco (Cali-Colombia), Cra 38bis # 5b2-04, Cali, Colombia