The Weil osteotomy is a common technique used in the treatment of lesser metatarsal deformities of the forefoot. In the last years a large amount of papers have been published showing its effectiveness and the complication rates of the Weil-type osteotomy. Although most of studies have shown an effectiveness in pain reduction close to 80–90%, complication rates are also relatively large in some reports. The present paper is intended to review clinical, radiological and cadaveric studies of the Weil osteotomy in an attempt to make a comprehensive review for the reader regarding all aspects of this common used technique.
La osteotomía de Weil es una técnica quirúrgica comúnmente utilizada para el tratamiento de las alteraciones de los metatarsianos menores en el antepié. En los últimos años se han publicado una gran cantidad de artículos acerca de esta técnica valorando su efectividad y sus posibles complicaciones. Sin embargo, a pesar de que los estudios clínicos han mostrado una efectividad en la reducción del dolor en entre el 80-90% de los pacientes, el índice de complicaciones reportados es relativamente alto en algunas series. El presente artículo revisa los artículos clínicos, radiológicos y de laboratorio o cadavéricos que se han realizado sobre esta técnica para que el lector pueda entender de forma coherente todos los aspectos relacionados con la osteotomía de Weil, especialmente sus indicaciones, efectos mecánicos, modificaciones, posibles complicaciones y resultados de los estudios clínicos.
Surgical treatment of lesser metatarsals has been an ill-defined issue of foot and ankle surgery for decades. Historically, more than 25 different procedures have been described in the literature for the treatment of lesser metatarsals including so different procedures such us plantar condylectomies, osteoclasis, distal shortening osteotomies, distal dorsiflexory osteotomies, metatarsal enclavement (“peg in hole”), proximal dorsiflexory osteotomies, colectomies and, finally, partial or complete metatarsal head resections.1 Lesser metatarsal surgery, by means of metatarsal osteotomies, was historically associated with poor results during years. Most of these techniques were based in the execution of one or more highly unstable metatarsal osteotomies without fixation followed by immediate weightbearing and whose results in the elevation or shortening of the metatarsal heads were often unpredictable.
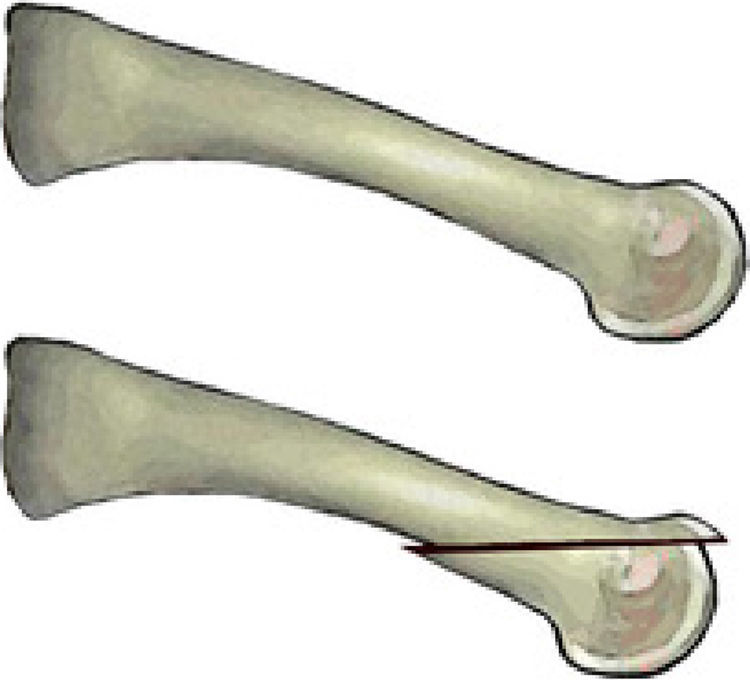
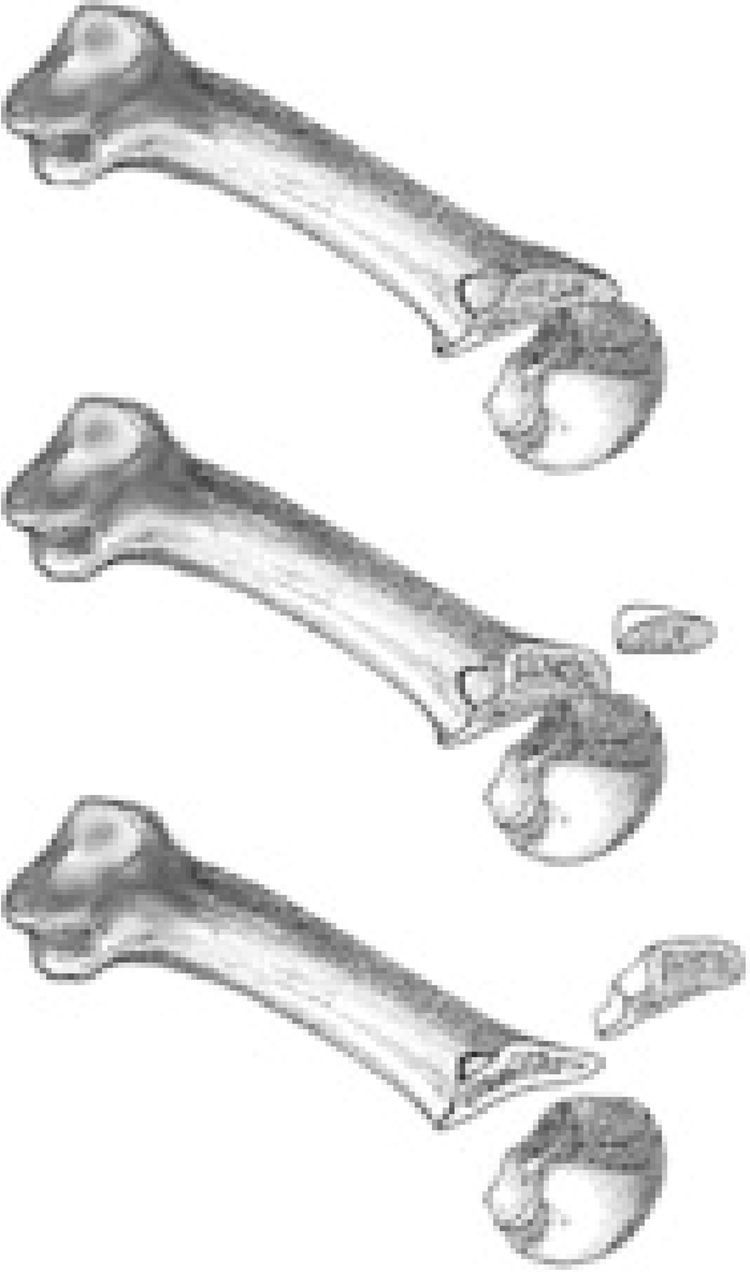
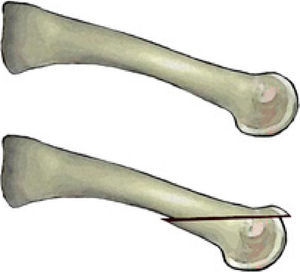
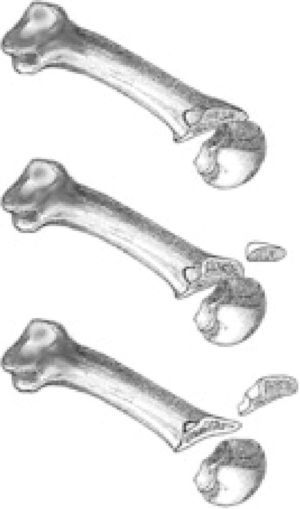
However, the Weil osteotomy has achieved great popularity in the surgical treatment of the lesser rays during the last years. Although there are no formal publications in the literature about the beginning of the technique, it was Lowell Scott Weil, a podiatrist from Chicago, who first performed the technique in a real patient in 1985.2 The osteotomy was initially thought as a cut in the lesser metatarsal, parallel to the weightbearing surface which allows an exact amount of shortening of the metatarsal (Fig. 1). Louis Samuel Barouk, a French orthopedic surgeon settled in Bourdeaux, met LS Weil in a congress in Chicago where they shared experiences and it was then when Weil talked to Barouk about this technique. In 1992, LS Weil was invited by Barouk to a meeting in Bourdeaux about the Scarf osteotomy and in a live surgery case during the meeting, LS Weil performed the osteotomy in Europe for the first time.3 Since then, Barouk hold this technique with enthusiasm and carried it out systematically in his patients. The first formal publication of the technique was published by Barouk in the German journal Orthopade.4 From this publication and from the books written by Barouk about forefoot reconstruction,3,5 the technique was popularized in Europe and nowadays, it is the technique with most papers published in this field, mainly in the orthopedic literature.
It is the opinion of the authors of this review that the technique has inherent advantages that have speed up its dissemination. On one hand, the osteotomy is technically easy to perform and do not have a long learning curve. Several of the metatarsal osteotomies described in the literature were technically complex and frequently the surgery failed because of technical problems of the technique. On the other hand, Weil osteotomy produces a predictable and programmed shortening of the metatarsal being at the same time so stable, that allow immediate weightbearing. This immediate weightbearing helps to compress of the osteotomy and do not distract it. For the first time, surgeons could apply a precise and predictable shortening of the metatarsal with immediate weightbearing avoiding associated problems of distraction of the osteotomy that could dorsiflex or shorten the metatarsal head in an uncontrolled fashion. This aspect avoided the main problem for foot and ankle surgeons in metatarsal correction which was the loss of control of the shortening or elevation of a metatarsal under immediate weightbearing.6 Mainly for these reasons, the osteotomy is nowadays the most common technique applied for the treatment of lesser metatarsals around the world.
The technique and its indicationsWeil osteotomy is designed to make a controlled shortening of the length of the metatarsal in the transverse plane and its main indication is referred to an excessively long metatarsal with an abnormal metatarsal parabola.7 However, in the last years the indications of the technique have been “expanded”, being used for the treatment of digital deformities associated to metatarsophalangeal joint subluxation or luxation3,5 and for transverse plane deformities of the digits.8,9 These indications are associated to the indirect relaxation that the osteotomy produces in the soft tissues which improves the digital contracture. At the same time, Ernesto Maceira, a Spanish orthopedic surgeon, has used this technique for the treatment of mechanically induced propulsive metatarsal pain in what he termed as “third rocker” metatarsal pain.10,11 This concept encompasses the mechanical study of the foot during gait and is referred to lesser metatarsal pain induced by abnormal biomechanics during the propulsive phase of the gait cycle or “third rocker”. This is differentiated from metatarsal pain produced in other phases of the gait cycle such as midstance or “second rocker” metatarsal pain. In the third rocker, the heel lifts the ground and body weight is concentrated on the metatarsal area till the opposite foot contacts the ground. Is during this exact moment, when length abnormalities of the metatarsals are more potentially harmful. A controlled shortening of the involved metatarsals can help to reduce plantar pressure in the propulsive phase which is the main reason for its indication in cases of mechanically induced propulsive metatarsal pain or “third rocker” metatarsal pain.
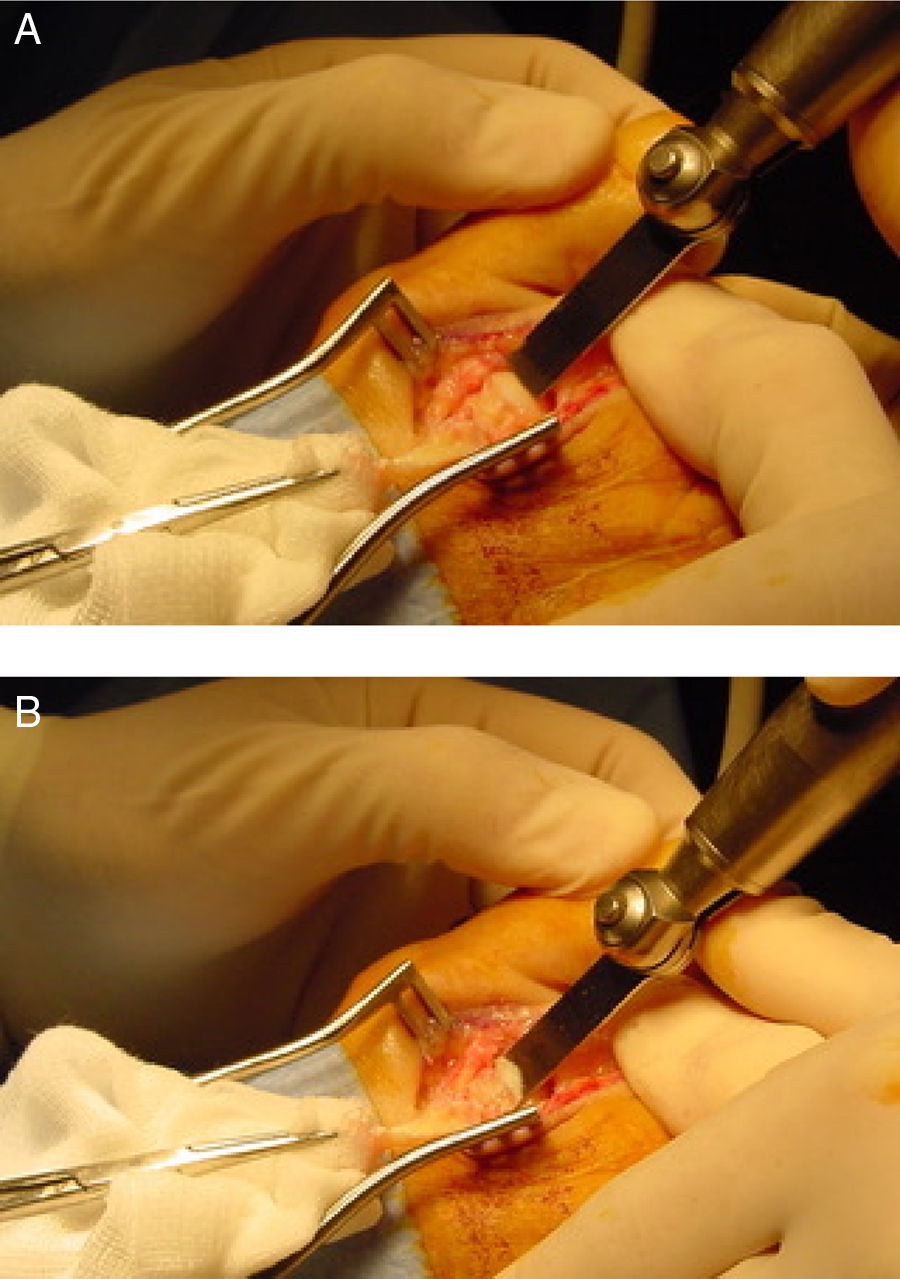
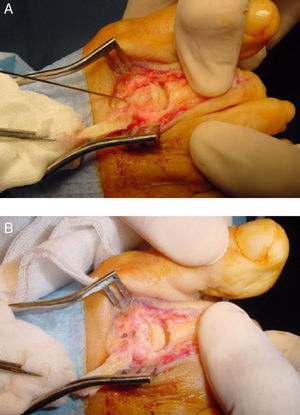
The technique begins with the patient lying supine. Local anesthesia is usually employed depending on the surgeon preference with sedation of the patient. An ankle tourniquet is usually employed unless concomitant procedures in the lower leg such us gastrocnemious recession are also planned. A dorsal approach is performed with a direct incision just over the metatarsal or in the metatarsal spaces when the technique is going to be performed in adjacent metatarsals. A transverse incision can also be used when the osteotomy is going to be performed in several metatarsals (usually three or more),12 although it can also be performed with longitudinal incisions in the intermetatarsal spaces (second intermetatarsal space incision for 2° and 3° metatarsals and fourth intermetatarsal space incision for 4° and 5° metatarsals).3 In case of use the transverse incision, it is wise to perform the incision proximal to the metatarsophalangeal joint line to allow easy exposure of the metatarsal heads which will facilitate the fixation after the shortening of the metatarsals (Fig. 2).
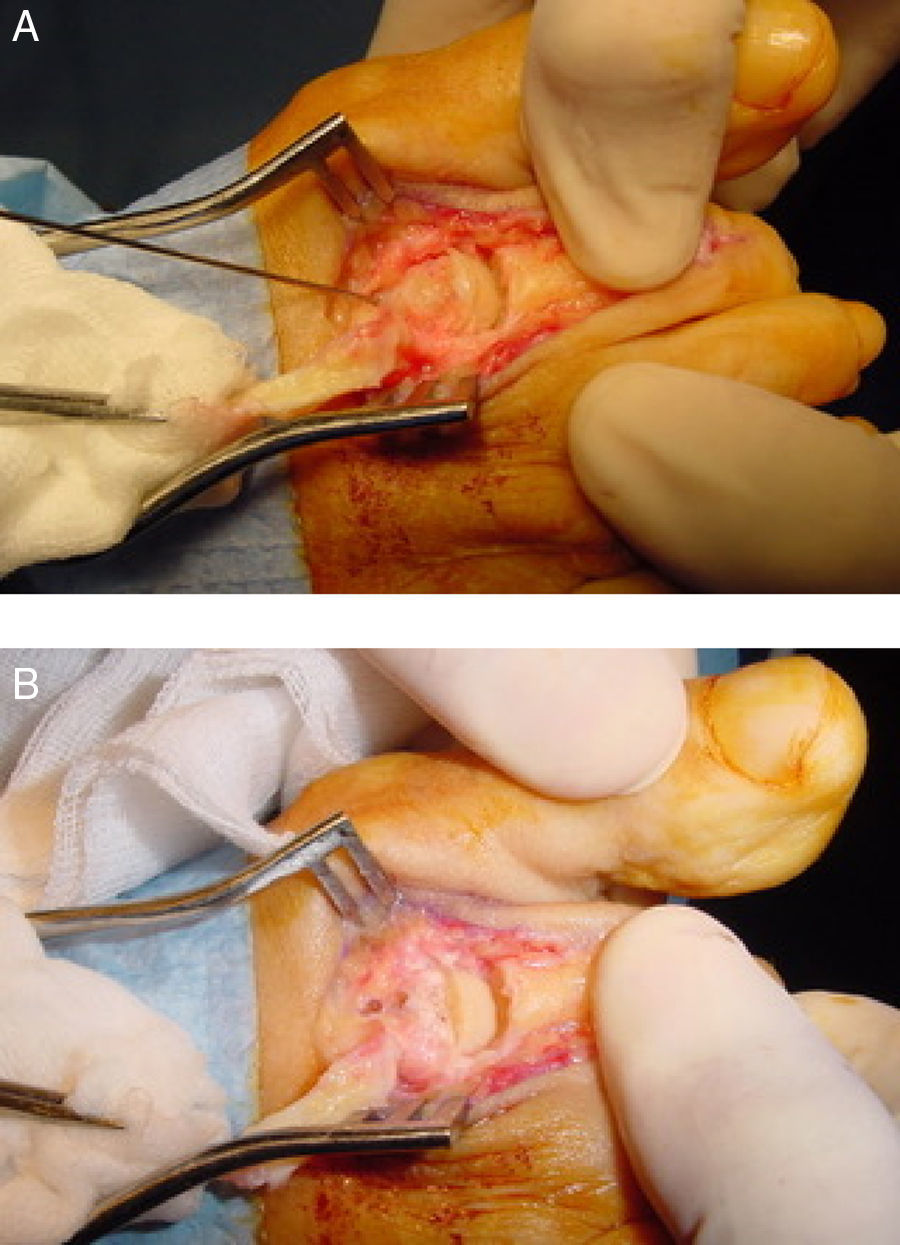
Once the incision is performed, it is deepened till deep fascia is reach avoiding damage to the neurovascular structures. Deep fascia is identified by the extensor digitorum longus and extensor digitorum brevis tendons over the metatarsophalangeal joint. At this point, the surgeon can use different maneuvers to open the joint. It can be done by a longitudinal incision medial to the extensor digitorum longus tendon, lateral to the extensor digitorum brevis tendon or between both tendons. With this incision the joint is opened and collateral ligaments are released to fully exposed the metatarsal head. Other maneuver consists in a “Z” lengthening of the extensor tendons at the metatarsophalangeal joint releasing the hood ligament and exposing metatarsophalangeal joint capsule. Afterwards joint capsule can be opened with a transverse incision or a “T” incision with the vertical arm oriented proximally over the metatarsal head. Collateral ligaments are also released and the metatarsal head is also exposed. This maneuver is also indicated when a procedure of arthroplasty or arthrodesis of the interphalangeal joints of the digit is performed concomitantly. The proximal extensor tendon end cut at the interphalangeal joint can be pull back proximally exposing the metatarsophalangeal joint capsule.
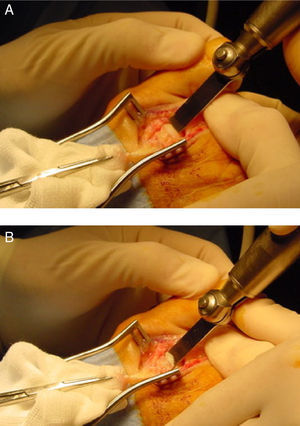
Once the joint is fully exposed, the assistant protects the medial and lateral soft tissues to avoid damage of the neurovascular structures with the saw blade and the surgeon plantarflex the digit which allow easy visualization of the metatarsal head. An end-to-end bone cut is performed starting 1–2mm below the dorsal border of the articular cartilage of the metatarsal head intraarticularly. Saw blade is oriented as much parallel as possible to the weightbearing plane (Fig. 3). For the orientation of the blade is important to visualize and/or palpate the plantar aspect of the heel and the metatarsal area at the same time. A critical point of the osteotomy is the saw blade inclination that should be adequate to avoid the uncontrolled progression of the osteotomy in the proximal metatarsal diaphysis without completing the osteotomy. This usually requires the use of a long saw blade that is inclined 10–15° in the relation of the weightbearing surface. At the completion of the osteotomy a hard resistance in the saw can be felt which correspond to the plantar cortex of the metatarsal diaphysis. Once the osteotomy is completed, the metatarsal head is “settled” proximally in a decompression zone. The degree of shortening planed preoperatively is checked in the dorsal fragment of the osteotomy and the relative position with the other metatarsals are also checked fluoroscopically or by careful palpation intraoperatively. If more than 3mm of shortening is required (especially in the 2° and 3° metatarsals) it is recommended to extract a small slice of bone preferably from the head fragment because it is much wider and easy to manage that the metatarsal shaft which would difficult posterior fixation. This modification was termed by Barouk as “the second layer”.3 As the cut of the osteotomy is almost never strictly parallel to the weightbearing plane and it is usually angulated 10–15°, proximal translation of the metatarsal head is associated with some degree of plantarflexion. This plantarflexion is usually not important clinically if the displacement is small. However, with big displacements (usually more than 3mm) the second layer produce elevation and compensate for the plantarflexion associated with big displacements of the metatarsal head.
Once the metatarsal head has reached the desired position, fixation of the osteotomy can be achieved with several methods such us 2 parallel or crossed smooth Kirschner wires (absorbable or not absorbable), one threatened Kirschner wire or different screws such us 2.0mm (minifragment set) non-lagged screw, 2.4mm Herbert type cannulated screw or “click-off” screws designed specifically for fixation of the osteotomy. Because of the inherent stability associated with the osteotomy, any of the fixation methods mentioned gives adequate stability.13 For the fixation technique, the surgeon should plantarflex the metatarsophalangeal joint with one hand and making force at the same time with the proximal phalanx from plantar to dorsal on the metatarsal head to compress the osteotomy. In this position fixation is easily achieved from dorsal to plantar with any of the methods available. It can also be used a Kirschner wire located proximally as a temporal fixation before the use of the final fixation, although in the authors experience this is not absolutely essential. Finally, the dorsal bone prominence is eliminated with a Rongeur-type instrument to achieved a smooth and anatomical metatarsal head that allow metatarsophalangeal joint dorsiflexion without restrictions (Fig. 4).
After washing with saline, sequential closure of the wound is performed. The capsulotendinous plane over the joint can be closed with 3-0 absorbable suture or leave without suture with superimposed tendon ends in the authors experience. In case of suturing that plane, it is important to overcorrect the toe in a plantarflexed position during the suture. Subcutaneous and skin layers are closed as surgeon preferences. Absorbable 4-0 and 5-0 sutures are good options for subcutaneous and dermal sutures which allow early bathing without the necessity of suture removal.
ModificationsSeveral modifications to the original technique have been described in the last years such us the triple Weil osteotomy or Weil in three steps,14 “tilt up”, “tilt down”2 or the medial or lateral translation of the metatarsal head.9,15 The “tilt up” modification makes a “second layer” angulated as a wedge with the apex located distally and the base proximally. The most important indication is metatarsal head elevation in cases of prominent plantar condyles or IPK lesions when the metatarsal parabola is correct. The “tilt down” modification consists in making a wedge exactly opposite to that described for the “tilt up” modification, with a proximal apex and a distal base. The idea of this modification is rotation of the effective cartilage of the metatarsal head to prevent digital dorsiflexion contractures and floating toes postoperatively.3
The medial or lateral translation of the metatarsal head is indicated for the correction of digital deformities in the transverse plane such us abduction or adduction. Once completed the osteotomy, the metatarsal head is translated one third or half of its wide to correct the deformity.8 If the deformity of the digit is in adduction, the metatarsal head is translated medially. If the deformity of the digit is in abduction, the metatarsal head is translated laterally. The main idea is to shorten the metatarsal and translate the metatarsal head under the base of the phalanx to correct the deformity in the same manner of hallux valgus correction with translating osteotomies to close the intermetatarsal angle such us Austin or Scarf procedures9 (Fig. 5).
(A and B) Pre- and postoperative X-rays of a case of Weil osteotomies of 2nd to 5th metatarsals with medial translation of the metatarsal head to correct adduction deformity of the digits with a flexor digitorum brevis transposition.51
One of the most common modification used in Europe is that proposed by Maceira, known as triple Weil osteotomy of Weil in three steps.14 This modification consists in making three cuts over the metatarsal to extract a bone cylinder of the distal metaphysis–diaphysis area. Once the metatarsal head is exposed in a standard fashion, a complete end-to-end bone cut is performed starting just proximal to the cartilage of the metatarsal head extraarticularly. The orientation of the first cut is much more inclined to the weightbearing surface than in the standard Weil osteotomy. This more oblique orientation is finished plantarly without damaging the plantar condyles of the metatarsal head. Exact orientation can vary individually depending on the metatarsal inclination and morphology of the metatarsal head. Next, a second bone-to-bone cut is performed perpendicular to the ground, from dorsal to plantar, with the idea of extraction an exact amount of bone measured preoperatively. Finally, a third bone-to-bone cut is performed starting at the same point of the second cut but with the same inclination of the first cut. With these three cuts a cylinder of bone is extracted and fragments are pushed together (Fig. 6). Fixation of the osteotomy is performed with any of the methods described above although it is technically more complex with this modification. Firstly, the proximal cuts on the bone give a narrow diaphysis which makes the area for dorsal fixation much narrower, and secondly, the obliquity of the cut makes more difficult to put the screw or the wire perpendicular to the osteotomy. This modification of the osteotomy produces a controlled shortening with elevation of the metatarsal head. Because of the extraction of a bone cylinder of the metatarsal, metatarsal head is shortened and elevated regarding its initial position. This elevation is coaxial to the longitudinal axis of the metatarsal which makes the amount of elevation dependent on the cylinder length and the metatarsal inclination with respect to the ground which can be different in patients with pes planus or pes cavus.
Complications and mechanical analysis of the osteotomySince the technique was popularized in the 2000 and its use was massively expanded, complications also appear such us floating toes, transfer metatarsalgia, recurrence of the deformity or pain or no unions. In 2011, Highlander et al.16 published a systematic review regarding Weil osteotomy complications from clinical studies in the literature till that date. Complications found by the authors in order of appearance were: 36% of floating toes, 15% of recurrence, 7% of transfer metatarsalgia and 3% delayed union and no union (reported together). Because of its ample contact surface and the stability created by fixation systems and the weightbearing of the patient, the reported index of no unions or delayed unions is quite low (0–2%) and even a paper did not find differences in postoperative clinical results between fixation and not fixation of the osteotomy.17
However, the other complications reported can be explained by a mechanical analysis of the osteotomy. The effect of different combined variables such us cut orientation, amount of shortening and modifications used are critical aspects to understand the final mechanical effect that the osteotomy has on the metatarsal or metatarsals with respect to the weightbearing surface.
Lowet Scott Weil described the osteotomy parallel to the weightbearing surface such us the proximal displacement of the metatarsal head would produce shortening without plantarflexion/elevation respect to the other metatarsals. For that reason, the osteotomy is started intraarticularly 2mm below the dorsal border of the articular cartilage of the metatarsal head (Fig. 3). If the osteotomy is performed extraarticularly (dorsal to the cartilage), a cut parallel to the ground will progress through the metatarsal diaphysis without exiting the osteotomy plantarly. However, the idea of the cut parallel to the weightbearing surface has been discussed extensively and has promoted the appearance of modifications. In, 2001, Trnka et al.18 published one of the first in vitro studies of the osteotomy by performing it on 2 specimens and in several osseous models to observe its mechanical effect. This study highlighted two important aspects of the Weil osteotomy. The first one was the impossibility to complete the osteotomy plantarly with an orientation of the blade less than 25° with respect to the metatarsal diaphysis. These authors needed to angulate the saw blade at least 25° in the osseous models to allow the saw blade to exist the osteotomy in the plantar diaphysis of the metatarsal. Less than 25° of angulation made the saw blade to progress through the metatarsal diaphysis. As the average value of inclination of the second metatarsal is 15°,5 it would be impossible to perform the osteotomy parallel to the weightbearing surface and in the case of the second metatarsal the final inclination of the osteotomy would be 10° at minimum. This inclination predicts a plantarflexion effect of the osteotomy that would increase with bigger proximal displacements and with less inclination of the metatarsal, which could be more important in the third, fourth and fifth metatarsals whose inclination is usually less than 15°.
In summary, the study of Trnka et al. showed the inherent plantarflexion associated with the procedure as the metatarsal head is displaced proximally. This plantarflexion seems to have minimally or no effect when the displacement is small, usually 3mm or less, although some authors have stated than 5mm can be performed without changes in plantar pressures.19 However, it seems that shortenings greater than 3mm could lead to a plantarflexion deformity of the metatarsal head that could be clinically relevant.2,5 In those cases, modifications such us the “second layer” or Triple Weil osteotomy could be done to compensate the associated plantarflexion.3,14,20 The “second layer” produces a coaxial elevation of the metatarsal head that compensates the plantarflexion associated with big displacements of the osteotomy whereas the Triple Weil osteotomy produces both, shortening and elevation, so in the latter cases it is not necessary to displace more the osteotomy in a shortening direction.14 Garg et al.21 preformed the Triple Weil osteotomy in 48 patients and observed that a shortening bigger than 2mm produced an unacceptable rate of transfer metatarsalgia to the adjacent metatarsals that required to operate adjacent metatarsals. Authors stated that the transfer was produced by the shortening and elevation created by the osteotomy leaving a shortened and elevated metatarsal head respect to the others metatarsal heads. The main problem with this approach is derived from the difficulty of knowing the exact amount of millimeters needed in the “second layer” or in the triple Weil osteotomy to produce elevation without jeopardizing the other metatarsal heads. Till now, this is a not clear aspect of the technique that needs more clarification in future studies, especially with big displacements of the osteotomy or when the osteotomy is performed in several metatarsals. Those aspects are discussed thoroughly in the next section of the manuscript.
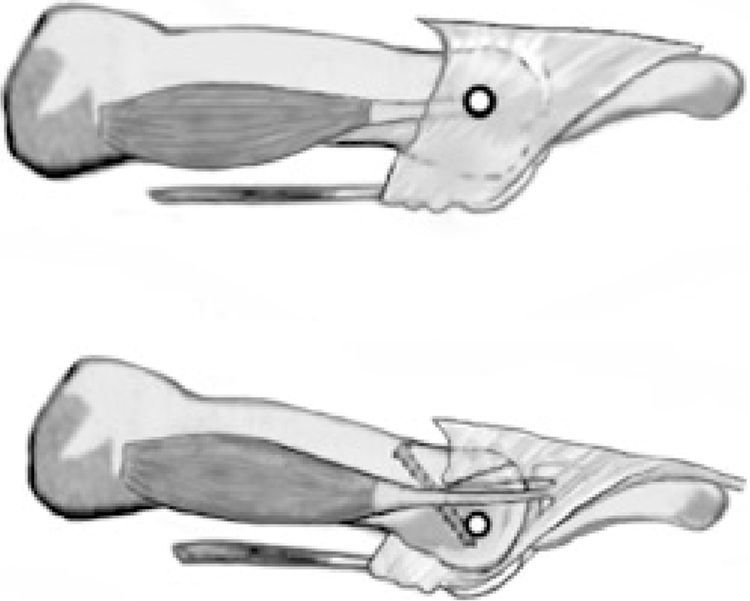
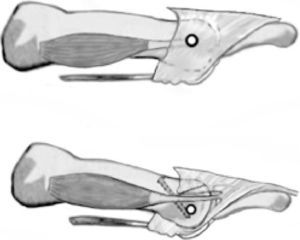
The second important point noted by Trnka et al.18 explained the most common complication reported of the Weil osteotomy: postoperative floating toes. For those authors, the proximal displacement of the metatarsal head and its associated plantarflexion makes a change in location of the axis of the metatarsophalangeal joint in relation to the tendon of dorsal interosseous muscles. In this new situation, they noted that the tendon changed from a position inferior to the axis (which produce a plantarflexion of the digit) to a position superior to the axis (which produce a dorsiflexion of the digit) and that change would contribute to the extension deformity seen after the osteotomy (Fig. 7). This explanation has been used extensively in the orthopedic community22 to explain the high index of floating toes reported after the osteotomy.
Mechanical effect of the osteotomy over the axis orientation of the metatarsophalangeal joint in relation to the position of the dorsal interosseous muscles tendon described by Trnka et al.18
However, the presence of floating toes after the Weil osteotomy seems to be a more complex, and not very well understood, aspect of the technique. Garg and colleagues21 published a study on 48 patients with a triple Weil osteotomy in which the axis position of the metatarsophalangeal joint do not change in relation to the interosseous tendons. They showed a similar rate of floating toes postoperatively (27.1%) that those reported in other studies with a simple Weil osteotomy. At the same time, those authors observed that the floating toe deformity decreased postoperatively in the long run. Patients with less evolution time from the surgery had bigger rate of floating toes that patients with less evolution time (41.2% vs. 17.6%). The authors recognized that this finding is contrary to the explanation reported by Trnka et al. regarding the possible etiology of floating toes.18 At the same time, Pascual Huerta et al.23 carried out a retrospective analysis of 25 operated cases with either simple Weil (8 cases) or triple Weil osteotomy (17 cases) and did not find differences in the rates of floating toes in both groups.
Other authors have suggested relaxation of plantar soft tissues as a possible etiology for the toe extension deformity after the osteotomy.24 It is important to note that the main plantarflexory force of the metatarsophalangeal joint is the plantar fascia with its attachment in the plantar plate of the metatarsophalangeal joint which produces the inverted Windlass mechanism.25,26 In fact, it has been reported extension digital deformities of the toes after plantar fascia release.27 Shortening of the metatarsals by means of Weil osteotomy, primarily in shortenings bigger than 5mm, produces an indirect soft tissue relaxation that weakens the plantarflexion pull of the plantar fascia over the metatarsophalangeal joint. This decrease in the plantarflexion moments over the metatarsophalangeal joint in the shortened metatarsals allow for a dorsiflexion displacement of the digit in the early postoperative period. Pérez et al. confirmed this hypothesis in a study with specimens showing that Weil osteotomy produced an immediate deformity of the metatarsophalangeal joint into dorsiflexion that was also immediately corrected with tightening of the plantar plate.24 Authors of the present review are in agreement with this explanation and, in their experience the deformity of floating toes after Weil osteotomy tend to reduce with time (6–12 months) and most of times disappear in the long run. This could be viewed as an adaptive shortening process of plantar fascia after the shortening of the metatarsal.
There are two more considerations to be aware regarding floating toes deformities after Weil osteotomy. The first one is that the surgeon should be alert to the presence of preoperative floating toes that probably would not be corrected by only performing the Weil osteotomy alone. Lots of cases in which this technique is applied have metatarsophalangeal joint subluxation or luxation with the digit in a floating toe position in the preoperative period. The Weil osteotomy produce a shortening of the metatarsal or shortening with elevation, but has no effect on the plantarflexion forces of the metatarsophalangeal joint that are usually distorted in these cases by rupture or attenuation of the plantar plate. If a technique to plantarflex the digit such us flexor digitorum longus transfer28,29 or plantar plate repair30–32 is not applied, the natural outcome of these cases is that the digit will have a dorsiflexion deformity after the surgery that was also present preoperatively. Probably, is in this cases in which Weil osteotomy “leaves” permanent floating toes deformities that do not improve with time.
The second consideration is related to concomitant procedures performed in the interphalangeal joint such us arthroplasty or arthrodesis. Migues et al. published a case series report of 70 Weil osteotomies in 26 patients33 in which they found a statistically significant association between floating toes in patients in which Weil osteotomy was performed together with procedures in the proximal interphalangeal joint compared to cases with Weil osteotomy alone (50% vs. 15%). The Weil osteotomy performed together with an arthrodesis procedure of the proximal interphalangeal joint is a common procedure in cases of digital deformity with metatarsophalangeal joint luxation, subluxation of transverse plane deformity. On one hand, the arthrodesis stabilizes the interphalangeal joint correcting the digital position and, at the same time, it converts the plantarflexory force of the flexor digitorum brevis over the interphalangeal joint into plantarflexory force over the metatarsophalangeal joint which also add stability to the latter plantarly. However, to achieve those objectives it is necessary to sacrifice the mobility of the proximal interphalangeal joint. Many times, a floating toe can be compensated with plantarflexion of the proximal interphalangeal joint making the tip of the toe to touch the ground. With a proximal interphalangeal joint arthrodesis, the digit usually is in a more rectus position and loses its ability to compensate the floating toe deformity. This could explain why the Weil osteotomy associated with proximal interphalangeal joint arthrodesis is more likely to produce a rigid toe that collaborate to a floating toe deformity of the digit.
After reviewing all these ideas, it is evident that the biomechanical behavior of the metatarsophalangeal joint after the Weil osteotomy need to be more studied. Although the change of interosseous muscle action from plantarflexors to dorsiflexors with the Weil osteotomy could have an effect in the development of floating toes, it is possible that other factors such us plantar fascia relaxation with shortening of the metatarsals, presence of floating toes preoperatively or combination of the Weil osteotomy with proximal interphalangeal joint arthrodesis of the digit could play an important role in the development of floating toes postoperatively.
Longitudinal decompression, multiple Weil osteotomies and metatarsal parabolaProbably, Barouk has been the surgeon who best understood the indications and who best applied the osteotomy in the treatment of moderate and severe deformities of the forefoot. For this author, the Weil osteotomy of the lesser metatarsals has a critical importance in the treatment of severe deformities of the forefoot with subluxations and/or complete luxation of the metatarsophalangeal joints. In this sense, the concept of “longitudinal decompression” of the forefoot is one of the major pillars in which forefoot reconstruction is based as Barouk and Weil stablished.3
It is the opinion of the authors of the present manuscript that the most common deformities of lesser rays such us claw toes or hammer toes, specially when they are accompanied with subluxation or luxation of the metatarsophalangeal joint has an important component of shortening of the soft tissues (tendon, ligaments, skin, etc.) over bone segments that are functionally “too long”. The component of tension or shortening of the soft tissues is key to understand the etiopathogenesis of forefoot deformities and gets worse with time and with deformity progression. The imbalance of length in the forefoot between soft tissues and bone segments helps to maintain the deformity in cases of subluxation or luxation of the metatarsophalangeal joint. At the same time, the base of the phalanx makes a retrograde plantarflexory force on the metatarsal head increasing its plantar pressure on the ground. Although it can be a more controversial point, it is also the opinion of the authors of the present work that the deformities of the first ray such us hallux valgus and hallux limitus share the same etiology of the lesser metatarsals with a component of shortened soft tissues over a functionally long osseous segments. With these ideas in mind and simply put, treatment of forefoot deformities could be approached by two different perspectives: lengthening of soft tissues (ligament release, tenotomies, tendon lengthenings, lengthening skin plasties, etc.) or shortening of bone segments. A third perspective would combine both, lengthening of soft tissues and shortening of bone segments. Regardless of which is the best approach, is in this context when the idea of “longitudinal decompression” of the forefoot with multiple Weil osteotomies proposed by Weil and Barouk acquire relevance.
To carry out this concept, Barouk developed the idea of “ms point” which represent the point of maximum deformity.3 It consists in the identification of the most proximal point of the base of the phalanx in the metatarsophalangeal joint with most deformity into subluxation/luxation in the weightbearing X-ray of the patient (Fig. 8). This point indicates the maximal contracture deformity of the soft tissues of the forefoot and indicates the amount of decompression needed to fix the problem. Once the “ms point” has been identified, the distance between the most distal part of the metatarsal head to the “ms point” is measured. This distance gives the exact amount of shortening needed in the osteotomy to correct the deformity of the joint. This concept is quite relevant in the treatment of luxation and subluxation of metatarsophalangeal joints because it allows a precise calculation of the shortening needed to reduce the deformity in a specific metatarsal ray.
(A) Preoperative view of a patient with a luxation deformity of the second metatarsophalangeal joint. Note the “ms point” as the point of maximum deformity in the base of the phalanx over the metatarsal head. This point is used as a reference of the amount of shortening needed to correct the deformity. (B) From the “ms point” a new metatarsal parabola is constructed.
However, shortening of an isolated metatarsal can distort the metatarsal parabola and the shortened metatarsal can loose its hability to support weight in the propulsive phase of gait (“third rocker”). For this reason, this approach of “longitudinal decompression” to metatarsal surgery requires to perform surgery also in asymptomatic metatarsals to reestablish imbalances of the metatarsal parabola (Fig. 8). So, the basic idea is to perform a programmed shortening of the lesser metatarsals (symptomatic and no symptomatic) with the objective of restoring a correct metatarsal parabola taking the “ms point” in the worst subluxed metatarsophalangeal joint as the initial reference point. This is probably the most difficult point to be understood by surgeons, clinicians and foot specialists in general. The universal tendency in surgery is to think that “less is more”, so it is not easy to understand that for the correction of the deformity of one metatarsophalangeal joint, it is necessary to perform multiples osteotomies in the forefoot to produce a longitudinal decompression. Although this approach can be seen as a more aggressive surgery that can extend the postoperative recovery of the patients, it is an established idea for several foot surgeons and for the authors of this revision that this approach gives more reliable and predictable results in the correction of severe forefoot deformities in the long run. On one hand, it resolves the contracture of all the metatarsophalangeal joints including those with a luxation/subluxation process of the joint and those that do not have problems but could probably developed them in the future. On the other hand, asymptomatic metatarsals would acquire a correct length in relation to the neighbor metatarsals that has been shortened to avoid transfer metatarsalgia in the future.
However, which is the right metatarsal parabola that need to be reconstructed? Basically all the orthopedic literature is centered on the work of Maestro et al.34 to define the concept of correct or “harmonious” metatarsal parabola that need to be achieved in the surgical reconstruction of the forefoot. In 2003, Maestro et al. published a paper in Foot and Ankle Clinics of North America trying to identify an ideal morphotype of metatarsal parabola as a planning method in cases of patients with severe forefoot deformities that require a forefoot reconstruction.34 Firstly, the paper explains an initial study that the authors carried out in 1995 in which they analyze the anteroposterior view (A-P) of 40 “normal” feet (they do not specify in how many patients) with a mean age of 55. In this study they found that the lesser metatarsal lengths were in a geometrical progression by factor two. Specifically, Maestro et al. found second metatarsal head 3.37mm longer than third metatarsal head, third metatarsal head 6.54mm longer than fourth metatarsal head and fourth metatarsal head 12mm longer than fifth metatarsal head. With this first study, the authors described the results of a second study with 84 “normal” feet again (neither specify in how many patients). Of the 84 “normal” feet, they used 34feet of the first study (with a mean age of 55.2) and added 50feet with a mean age of 30.3 years. With the X-rays of the 84feet, the authors identify 4 main morphotypes of metatarsal parabola. The first morphotype was termed as normal or “harmonious” and it was characterized by a geometric progression of metatarsal lengths by factor two (i.e. 2-4-8, 3-6-9, etc. with a tolerance of 20%). The other 3 morphotypes were considered as “no harmonious” and were characterized by: (a) excessively long second and third metatarsals (30%), (b) hypoplasia of fourth and fifth metatarsals (37%), and (c) excessively long first metatarsal (2.4%). Maestro et al. finally recommended the first morphotype or “harmonious” for the preoperative planning of the cases that require a complete reconstruction of the metatarsal parabola.34
Barouk embraced this idea of Maestro et al. and currently it is an accepted preoperative planning for forefoot reconstruction that first and second metatarsals should be equally in length and lesser metatarsals with an “harmonious” geometric progression by factor two as Maestro et al. described.3 However, although the work of Maestro et al. has been consolidated as a reference globally, the idea of correct or “harmonious” metatarsal parabola proposed by those authors, has several conflicting points. One of them is that the described morphotypes are all based in a sample of “normal” feet with no pain and no diagnosed deformities of the forefoot. It is evident that the preoperative planning of a forefoot reconstruction is quite important to avoid problems such us recurrence or transfer metatarsalgia, but the authors of the present review have not find any evidence supporting the idea that the first morphotype described by Maestro et al. should be followed discarding the other three. Although trying to replicate the “harmonious” metatarsal parabola could be a good option for several cases it massive use is not supported by the evidence. In fact, the transverse design of the work of Maestro et al. do not allow to observe if some of the described morphotypes (including the “harmonious”) developed pain or deformity in a medium or long time.
Some authors have noticed this aspect. Bevernage and Leemrijse35 published a case series of 73feet in 63 patients with a Weil osteotomy in which the method of Maestro et al. was used to plan the “armonious” metatarsal parabola preoperatively. Firstly, those authors showed the difficulty of achieving an “armonious” metatarsal parabola as only 23% of the 71 reconstructed cases had all criteria proposed by Maestro et al. to be considered as “armonious” postoperatively. At the same time, the authors did not find a significant association between reaching an “armonious” parabola postoperatively with a geometric progression by factor two and the development of recurrence or transfer metatarsalgia postoperatively. The authors of the present paper also published a clinical case of forefoot reconstruction36 in which the patient developed a transfer metatarsalgia of the third metatarsal plantarly prominent in spite of following the criteria of “armonious” metatarsal parabola described by Maestro et al. questioning the utility of this planning method in all cases.
So, it seems that the study of the metatarsal parabola as the only method of preoperative planning do not exclude the possibility of recurrence or transfer metatarsalgia in cases that require a forefoot reconstruction. It is obvious that this planning method only take into consideration the position of the metatarsal heads in the transverse plane and not in the frontal plane. Recurrence and transfer metatarsalgia are commonly related to imbalances of the metatarsal heads in the frontal plane.37 Kirby38,39 gave a good mechanical approach to understand forefoot behavior in this context. Although it is not the scope of this review it is interesting to note that from a mechanical view, the forefoot can be modeled as 5 independent rays with different and independent stiffness coefficients and with different responses to ground reaction forces. Each ray has a unique load-deformation curve (which determines its stiffness into dorsiflexion) that determines the amount of pressure that each metatarsal head support in weightbearing conditions. A good example of this is the intraoperative picture showed in Fig. 2. In this figure, the surgeon is making plantarflexion of all the metatarsophalangeal joints and, at the same time, making force in the proximal bases in a dorsal direction to simulate weightbearing. If we can imagine that all metatarsal heads are receiving the same dorsiflexion force (as it is supposed to be), we can also see that the mechanical behavior of each ray is quite different. First and fifth rays have lower stiffness (they get more dorsiflexion compared to the other rays with the same amount of force into dorsiflexion) and second and third rays have highest stiffness (they get less dorsiflexion compared to the other rays with the same amount of force into dorsiflexion). This behavior of the forefoot has been described in previous studies,40,41 and is critical to understand the plantar pressure under the metatarsal heads in weightbearing conditions. For the authors of this paper, this is a good approach to understand the forefoot mechanical behavior but in their experience the individual stiffness of each ray is variable from some subjects to others (i.e. although usually second metatarsal has higher stiffness, some cases can have a more flexible second ray compared to first or third rays). A more detailed description of the idea is given in the literature.38,39
This is a critical aspect to understand problems of recurrence or transfer metatarsalgia after multiple Weil osteotomies for “forefoot decompression”. Shortenings associated to “longitudinal decompression” are usually long enough (usually bigger than 5mm) that are unavoidable associated with plantarflexion of the metatarsal head during its proximal translation. This plantarflexion can produce plantar prominences that can be fixed with the extraction of a slice of bone (“second layer”) to elevate the metatarsal head. The extraction of this piece of bone is thought to avoid imbalances in the frontal plane of the metatarsal heads but, as has been discussed earlier in this paper, the main problem with this modification is the difficulty to know exactly the amount of bone needed to remove in order to avoid a plantar prominence of the metatarsal head. In the authors experience, in cases of imbalances in the frontal plane of the metatarsal heads, those are much worse tolerated in rays with higher degree of stiffness (second and third rays) than when they occur in more flexible rays (fourth and fifth rays). At the same time, if second and third rays have the same stiffness coefficient they would require the same amount of “second layer” extracted from the bone (or the same amount of shortening with a triple Weil osteotomy). Otherwise, the metatarsal with less amount of shortening or “second layer” extracted would present with a plantar prominence that would not be compensated. Although some authors have tried to identify this problem and to quantify it with axial projection of the metatarsal heads intraoperatively,37 the assessment of this position and stiffness of each ray is a clinical aspect that is almost impossible to quantify in a exact way currently with the technology currently available. This is an obvious obstacle for a complete assessment of all parameters that are implicated in the surgical reconstruction of the forefoot.
In summary, it can be stated that the osteotomy has a good design and seems to work well for modifications of the metatarsals in the transverse plane (metatarsal parabola), but its effect in the frontal plane is much less known. Surgeons need to be aware that the alignment of the metatarsal heads in the frontal plane after multiple Weil osteotomies is the final result of several variables such us type of osteotomy (simple vs. triple) and inclination of the cut, amount of shortening, the presence and amount of “second layer” and individual stiffness of each ray. This is sometimes a complicated equation and it is obvious that more studies are necessary for a better understanding of the effect that multiple Weil osteotomies has on the transverse and frontal plane alignment taking into consideration the stiffness of each ray individually. The preoperative planning of “longitudinal decompression” by means of multiple Weil osteotomies for control the transverse and frontal plane alignments of the metatarsal heads is still a problem difficult to resolve.
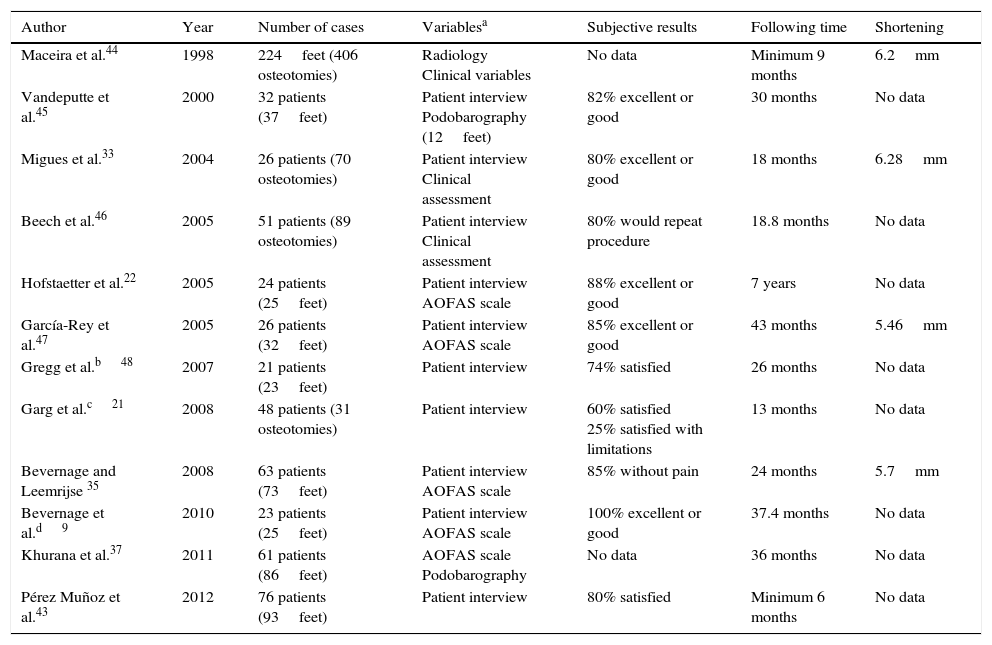
Clinical studiesIn the last years, there have been an explosion of clinical studies of the Weil osteotomy, mainly in form of cases series. Table 1 summarizes studies of the Weil osteotomy with a subjective or objective satisfaction assessment reported by patients. Most of clinical studies with the osteotomy have reported a result of 80–85% of “good” or “excellent” results.9,21,22,33,35,37,42–48 This data shows that the index of complications reported with this technique do not match with the index of “fair” or “poor” results referred subjectively by the patients. In this sense, it seems that complications associated with the osteotomy such us floating toes or joint stiffness are mainly reported by the clinicians and they are not usually seen as relevant problems for patients as long as they can do daily live without pain in most cases. However, other complications such us recurrence or transfer metatarsalgia are usually referred by the patient as serious or debilitating problems. Those latter complications occur usually between 10% and 15% in most studies and perfectly match with a “poor” or “fair” reporting of surgery as most of these cases do require a new surgery.
Subjective results reported in clinical studies performed over the Weil osteotomy in the last years.
| Author | Year | Number of cases | Variablesa | Subjective results | Following time | Shortening |
|---|---|---|---|---|---|---|
| Maceira et al.44 | 1998 | 224feet (406 osteotomies) | Radiology Clinical variables | No data | Minimum 9 months | 6.2mm |
| Vandeputte et al.45 | 2000 | 32 patients (37feet) | Patient interview Podobarography (12feet) | 82% excellent or good | 30 months | No data |
| Migues et al.33 | 2004 | 26 patients (70 osteotomies) | Patient interview Clinical assessment | 80% excellent or good | 18 months | 6.28mm |
| Beech et al.46 | 2005 | 51 patients (89 osteotomies) | Patient interview Clinical assessment | 80% would repeat procedure | 18.8 months | No data |
| Hofstaetter et al.22 | 2005 | 24 patients (25feet) | Patient interview AOFAS scale | 88% excellent or good | 7 years | No data |
| García-Rey et al.47 | 2005 | 26 patients (32feet) | Patient interview AOFAS scale | 85% excellent or good | 43 months | 5.46mm |
| Gregg et al.b48 | 2007 | 21 patients (23feet) | Patient interview | 74% satisfied | 26 months | No data |
| Garg et al.c21 | 2008 | 48 patients (31 osteotomies) | Patient interview | 60% satisfied 25% satisfied with limitations | 13 months | No data |
| Bevernage and Leemrijse 35 | 2008 | 63 patients (73feet) | Patient interview AOFAS scale | 85% without pain | 24 months | 5.7mm |
| Bevernage et al.d9 | 2010 | 23 patients (25feet) | Patient interview AOFAS scale | 100% excellent or good | 37.4 months | No data |
| Khurana et al.37 | 2011 | 61 patients (86feet) | AOFAS scale Podobarography | No data | 36 months | No data |
| Pérez Muñoz et al.43 | 2012 | 76 patients (93feet) | Patient interview | 80% satisfied | Minimum 6 months | No data |
Although most of the clinical studies used subjective tools to assess the effectiveness of the technique and patient satisfaction, studies that used more objective scales to measure its effectiveness such us the AOFAS scale, has also showed a significant improvement in their postoperative values related to pain, function and ambulation.9,22,35,37,47 The average improvement reported in the AOFAS scale varies between 35 and 50 points.
From the result of the studies, is that it seems that the Weil osteotomy works well for cases of metatarsal pain with luxation or subluxation of the metatarsophalangeal joint, specially in the long run. The longer follow up period reported in the studies is the Hofstaetter et al.22 study, that was 7 years. This study showed the highest percentage of “good” or “excellent” results reported subjectively by the patients (88%). Interestingly, those authors interviewed the patients at 1 year and at 7 years postoperatively and the results were better at 7 years that at 1 years. One year after surgery patients reported subjectively their results as “excellent” in 60% and “good” in 24%, whereas at 7 years the same patients reported their results subjectively as “excellent” in 76% and “good” in 12%. So, it seems that some of these patients improved with time. Hofstaetter et al. pointed out in their paper that cases that do not improved were mainly because of an insufficient shortening which stopped the favorable progression of those cases.
Finally, and comparing with other osteotomies, authors have found only one randomized clinical trial in the literature that compared the Weil osteotomy (33 cases) with a minimal incisional surgery (MIS) or percutaneous osteotomy DMMO (39 cases).49 The study showed better results in the Weil osteotomy group in metatarsal pain and postoperative edema at 3 months. However, the results in the last follow up (14.8 months) did not show differences between both groups regarding pain, mobility and function. Another nonrandomized study that compared the same techniques (20 cases with Weil osteotomy vs. 13 cases with DMMO) did neither find differences regarding pain in the AOFAS scale at 6 months postoperatively.50
ConclusionsThe Weil osteotomy is currently the most common technique used for the treatment of diverse metatarsal problems of the forefoot. It can be used in the treatment of excessively long metatarsals with imbalance of the metatarsal parabola, digital deviations in the transverse plane and also for correction of lesser metatarsophalangeal joint subluxation or complete luxation. Most clinical studies have showed a high satisfaction index reported subjectively by the patients that usually is closed to 80–85%. However, complications related to the osteotomy such us floating toes (36%), recurrence (15%), transfer metatarsalgia (7%) and delayed union or no union (3%) are relatively high. Although some of this complications are not referred as real problems by patients, such us floating toes, others, such us recurrence of transfer metatarsalgia, are referred as a more relevant problem by the patients that frequently will require a new intervention or surgery.
It has been described several modifications of the osteotomy being the “second layer” and the triple Weil osteotomy (Maceira modification) the most used nowadays. Those modifications allow a programmed shortening of the metatarsal with coaxial elevation of the metatarsal head in the sagittal plane which can compensate for inherent plantarflexion associated with the technique, specially with bigger shortenings. Performing multiple osteotomies for forefoot reconstruction have an important role in the treatment of severe forefoot deformities that require a “longitudinal decompression”. However, the ideal parameter to guide the reconstruction of the forefoot such us metatarsal parabola and the effect of the osteotomy in the frontal plane alignment of the metatarsal heads when osteotomies are performed in several metatarsals at the same time are not completely understood. The alignment of the metatarsal heads in the frontal plane after multiple Weil osteotomies is the final result of several variables such us type of osteotomy (simple vs. triple) and inclination of the cut, amount of shortening, the presence and amount of “second layer” and individual stiffness of each ray. More studies are needed to fully understand this aspects and to guide the preoperative planning of those patients.
Authors acknowledge Dr. Rafael Benegas Rekondo for his help in the development of the historic perspective of this paper and to D. Ramón Vaillo for his assistance with Figs. 1, 6 and 7.