Nowadays periodontal patients are not doomed to not be treated orthodontically. Once periodontal disease is under control, certain orthodontic movements can enhance periodontal health while also improving function and esthetics. This case reports presents a female patient, 28 years of age, skeletal class III with controlled periodontal disease who was refered by the Periodontics Department.
En la actualidad, el paciente con enfermedad periodontal no está condenado a no recibir tratamiento ortodóncico; una vez controlada la enfermedad periodontal puede verse beneficiada con determinados movimientos dentarios específicos que pueden ser favorables para el periodonto contribuyendo a una función y estética adecuada. El presente artículo muestra el reporte de un caso clínico en paciente femenina de 28 años de edad, clase III esquelética con enfermedad periodontal controlada, referida de la Clínica de Periodoncia.
Class III malocclusion is the result of the morphology or lack of position harmony between the maxilla and the mandible during the growth period. Malocclusion and the abnormal position of the teeth are recognized as potential causes of periodontal disease when they are producing occlusal trauma. This is due to the excessive functional stress that may onset inflammatory changes in the periodontium and therefore trigger a destructive bacterial process.1,2 Periodontally compromised patients are treated in an interdisciplinary fashion with the objective of not only improving oral function and aesthetics but also to prevent future problems.3
At present, the orthodontist faces new challenges such as treating periodontally compromised patients whose conditions are often not the most favorable because there may be reduced elements of periodontal support. These conditions are considered to be prevailing in the adult patient but even so it is common belief that they will be more cooperative. Previously it was not considered possible to treat them orthodontically since periodontitis could progress more rapidly. Nowadays, however, these patients are still considered to be at risk of developing a periodontal failure during orthodontic treatment.4–9
When the patient's oral health is good the common objective of both the orthodontist and the periodontist is to preserve it and if possible, improve the longevity and aesthetics of the stomatognathicsystem.3,7–9 Likewise, the periodontally compromised patient can benefit from orthodontic treatment because certain dental movements may be favorable to are duced periodontium.7–9
The characteristics of a class III malocclusion are: mesial position of the mandibular dental arch with respect to the maxilla which produces an anomaly in the incisor relationship (anterior crossbite), presence of a dento-skeletal malocclusion which results from a maxillary hypoplasia, a mandibular prognathism or combination of both.6
Among many considerations, an important point is that dental hygiene is the key factor for treatment success in periodontally compromised patients. The presence of plaque along with orthodontic movement may cause angular defects and significant bone loss but it should be noted that in patients with advanced periodontal disease and good hygiene, orthodontic treatment does not have significant effects on the periodontium or bone level in the long run.10,11 Therefore, before beginning orthodontic treatment it is important that the orthodontist identifies periodontal problems, determines the correct treatment plan and correctly establishes the sequence for orthodontic and periodontal treatment to improve the patient's periodontal health.3,12
The periodontist and the orthodontist must work together to make sure that inflammation and occlusal trauma are not present during the treatment of periodontally compromised patients, since these factors may lead to an increase in the insertion loss.3,5 Likewise, interdisciplinary orthodontic treatment may improve the gingival and bony level, the occlusal trauma and infrabonydefects.3
This article presents the case report of a female patient of 28 years of age, skeletal class III with controlled periodontal disease who was referred from the Periodontics Clinic for the purpose of improving her periodontal health and aesthetics.
CASE REPORTFemale patient, 28 years of age, with controlled periodontal disease, who was admitted to the Orthodontics Department Clinic at the Division of Post-Graduate Studies and Research (DEPeI) of the National Autonomous University of Mexico (UNAM), referred from the Periodontics Department.
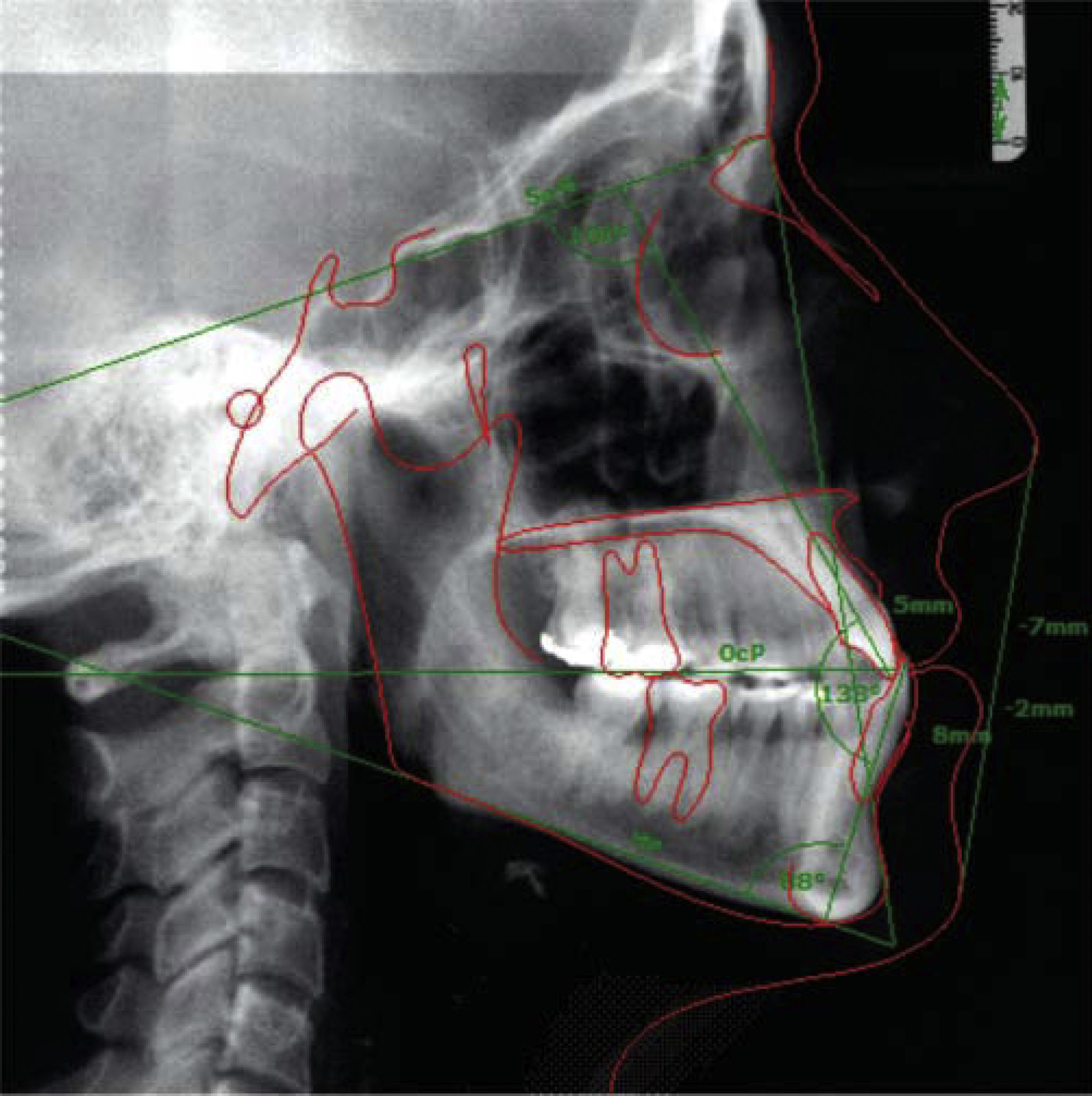
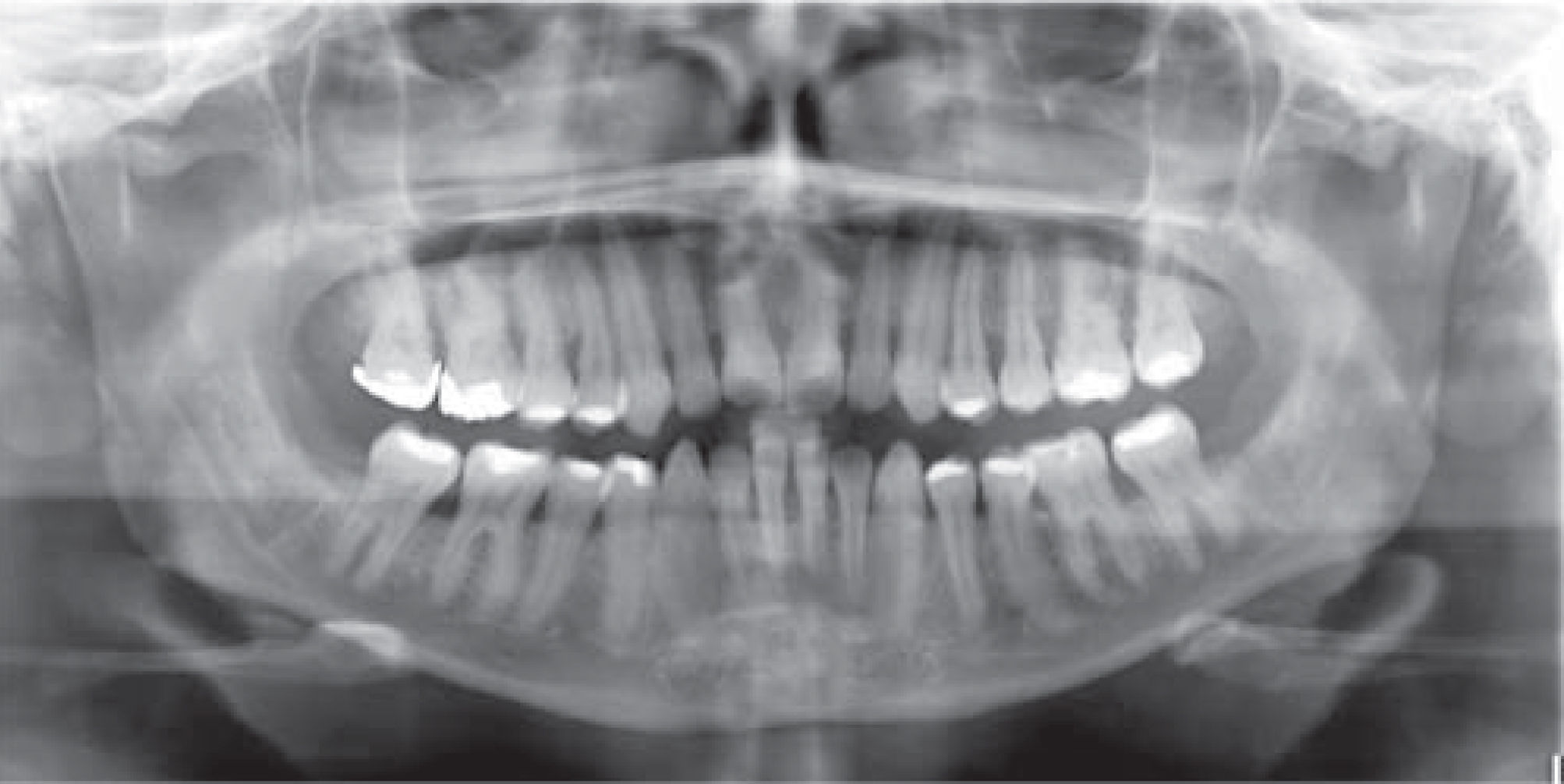
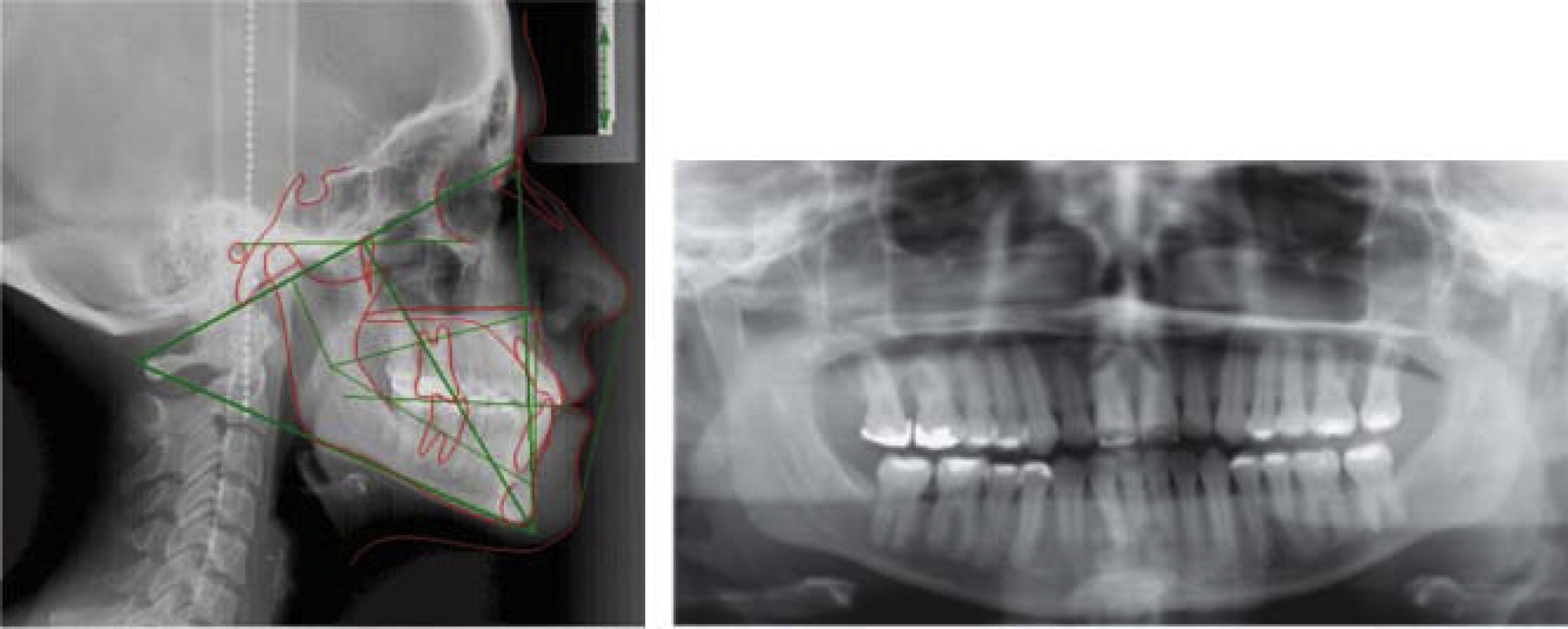
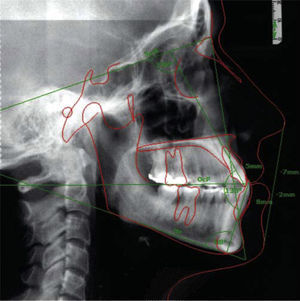
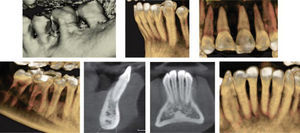
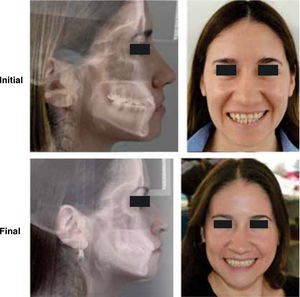
In the cephalometric analysis she was a skeletal class III, mesocephalic, with a concave profile, neutral growth and lower lip protrusion (Figure 1). In the panoramic radiograph she presented 28 erupted permanent teeth, loss of alveolar crests and a root-crown ratio of 3:1 (Figure 2).
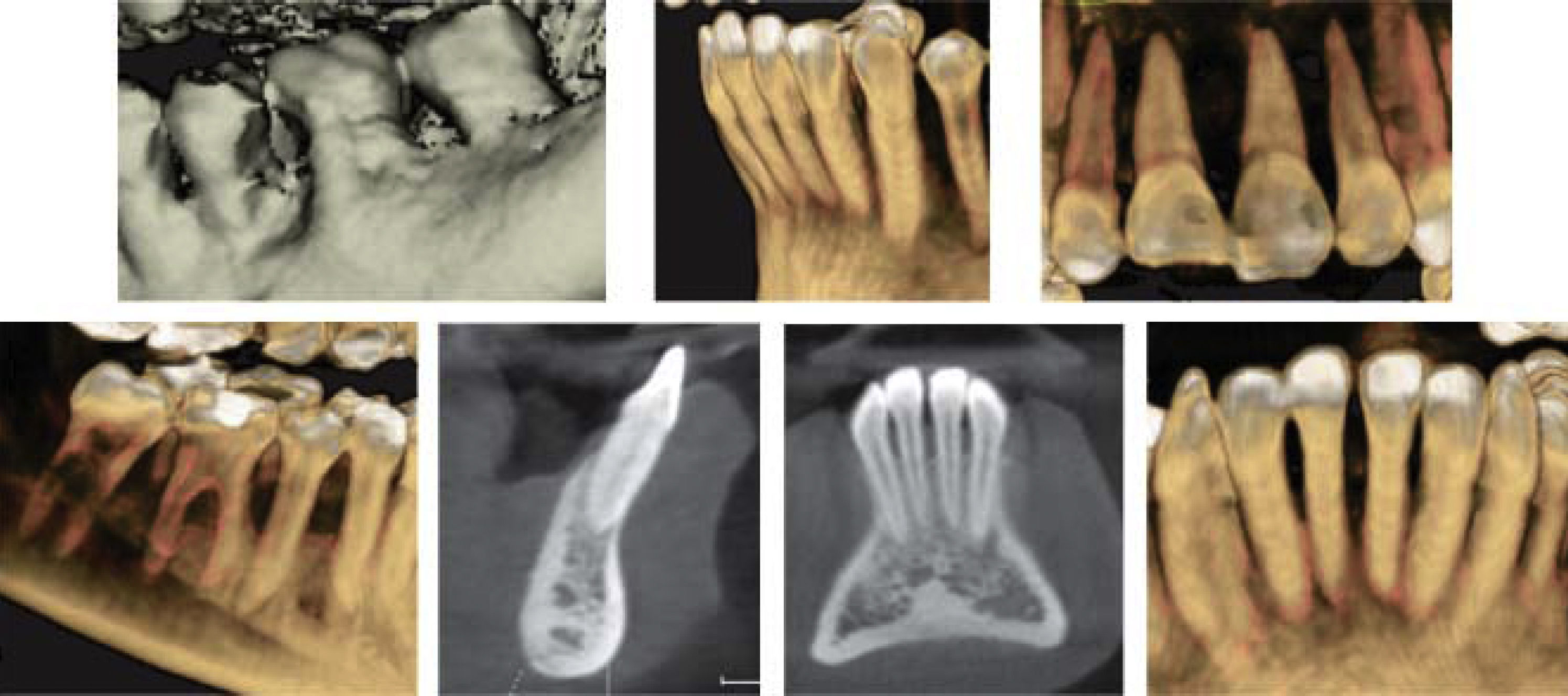
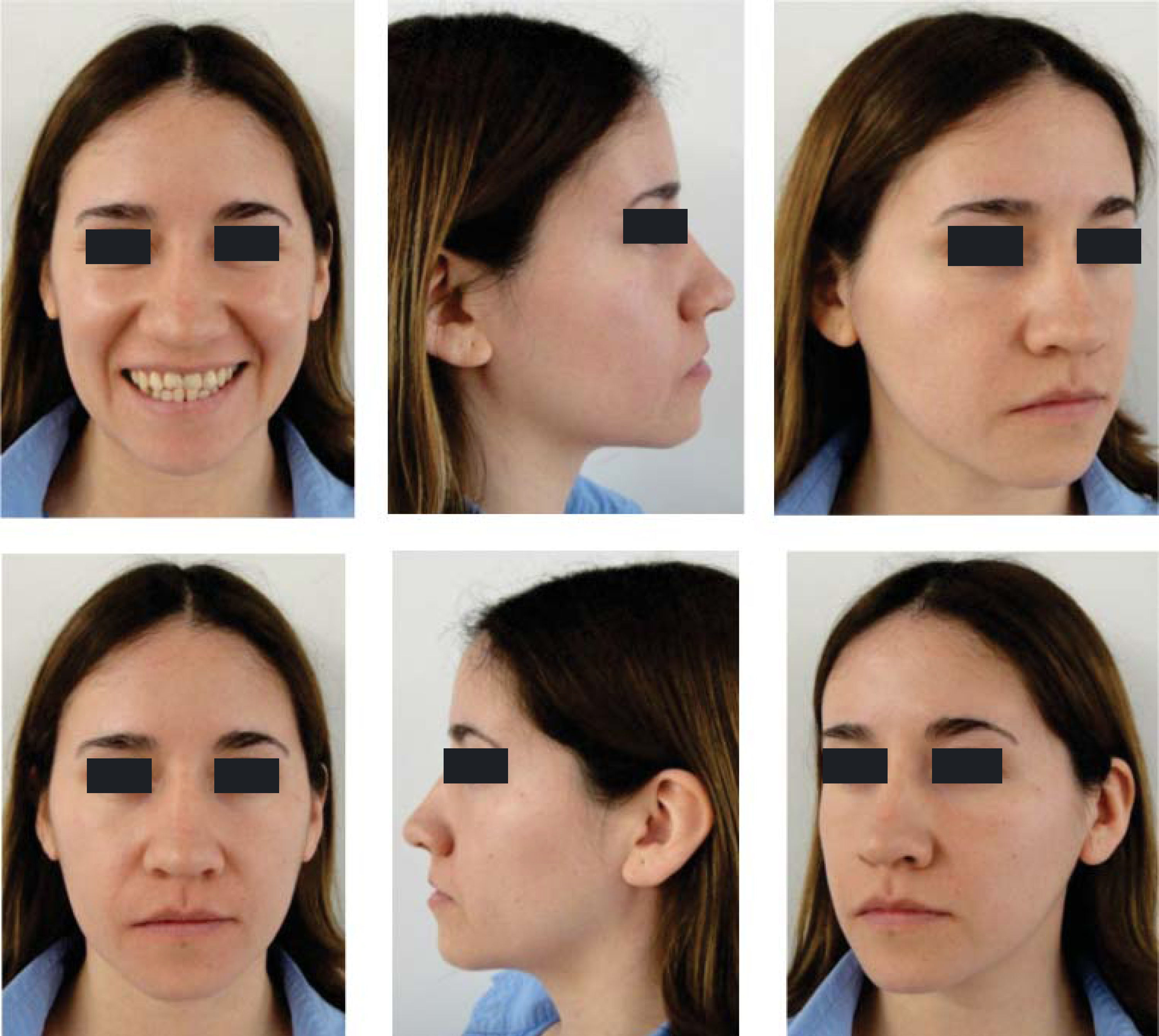
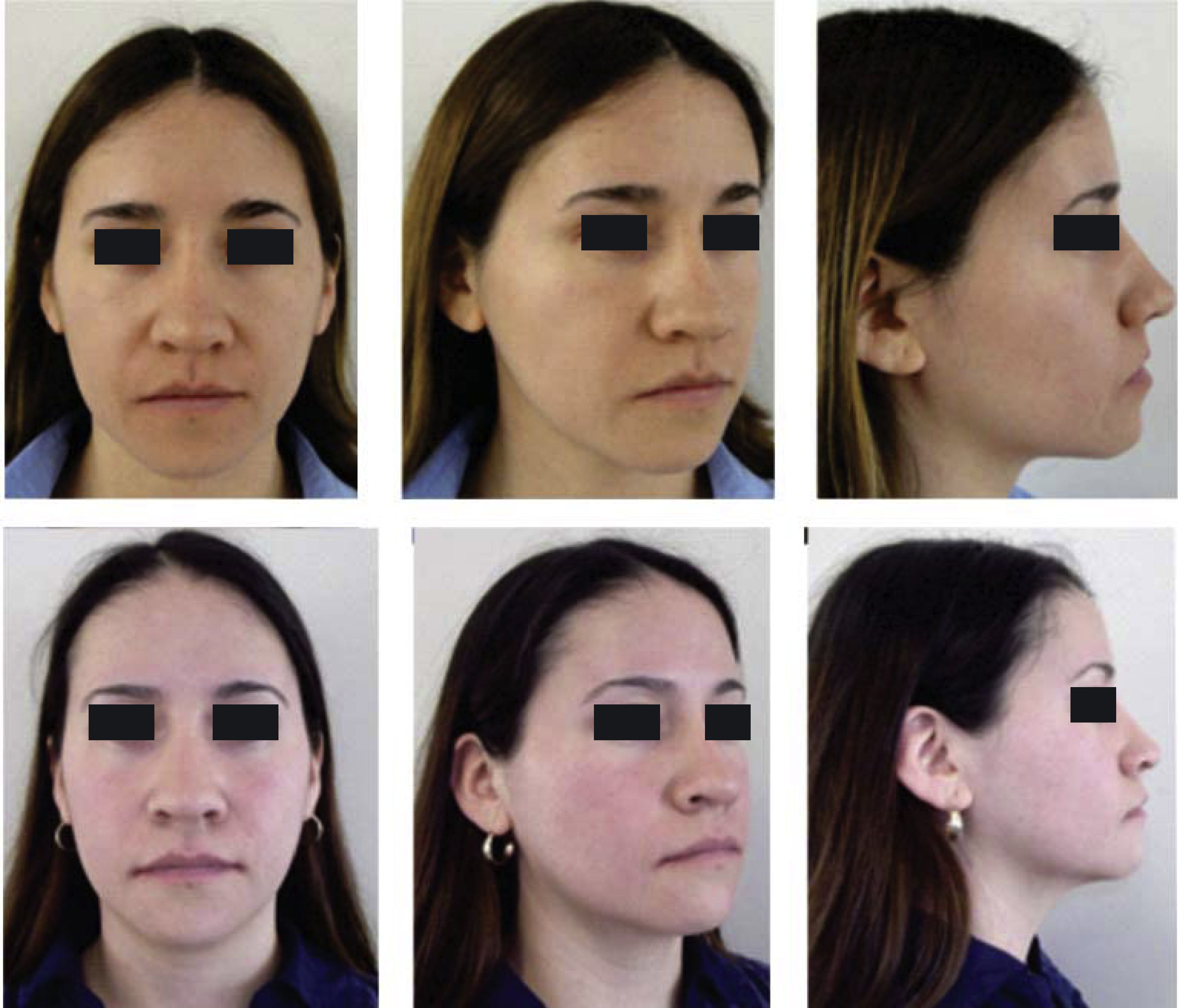
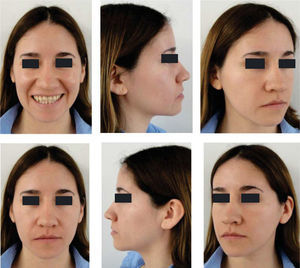
Facially, she presents a concave profile, mesofacial pattern, decreased upper facial third, asymmetry, neutral smile, lip competence and a slightly everted lower lip. Upon clinical examination and intraoral analysis, it was observed bilateral molar class III, a canine class III, a 3mm overbite, -2mm overjet, moderate lower dental crowding, dental midline deviation, ovoid upper and lower arch form, unilateral anterior and posterior crossbite and controlled generalized chronic periodontitis (Figures 3 at 5).
TREATMENT OBJECTIVESThe treatment objectives were: to improve the occlusal relationships in order to promote the conditions of periodontal health and aesthetics of the patient, to maintain the skeletal class or correct it surgically depending on the case evolution, to maintain the vertical dimension, to improve as much as possible the profile, correct the crossbites, achieve a molar and canine class I, obtain anterior and canine guidance, to align and correct the midline deviation. Thus a stable occlusion would be achieved and the dental inclinations would be corrected in order to improve the aesthetic and functional conditions.
TREATMENT PLAN0.022” slot Roth System appliances with bands in the first and second upper and lower molars would be placed. An interconsultation would be made with the Periodontics Department where scaling and root planning in the lower anterior area would be performed and subsequently, a free gingival graft would be placed. The patient was kept in a maintenance phase of periodontal treatment to continue with the orthodontic treatment.
Orthodontic treatment Phase I of alignment and leveling would begin by placing 0.014”-0.016” NiTi archwires. During Phase II-1, light 2nd and 3rd order movements would be performed with an archwire sequence from 0.016” × 0.016” NiTi- 0.017” X 0.025” SS. In Phase II-2 retraction of the lower anterior segment would be performed with a 0.019” × 0.025” DKL archwire. At this point of treatment, the case would be re-assessed to determine whether the treatment continued with orthodontics or orthodontics and orthognathic surgery.
TREATMENT PROGRESSTreatment was begun with the placement of fixed appliances, 0.022” slot Roth system, in the upper arch. The Department of Periodontics conducted the scaling and root planning in the lower anterior area and subsequently, placed a free gingival graft. A month later fixed appliances were placed in the lower dental arch thus beginning the leveling and alignment with the corresponding archwires (Figure 6). Three segments were formed throughout this phase: one anterior segment and two posterior ones. After the segments were formed a single keyhole loop (SKL) archwire was placed in the lower arch maintaining a segment with ligature wire from lower first molar to canine on both sides. The archwire was activated in the following appointment with a Suzuki retroligature to begin space closure (Figure 7A).
Once the spaces were closed, the archwire was tied with ligature wire to form a block of teeth from second premolar to second premolar on the upper and lower arch and began to use 3.5oz, 5/16” class III elastics with a vertical vector (Figure 7B). Subsequently, the teeth # 11 and 21 were rebuilt with composite to recover their form and aesthetics as well as to maintain what had been achieved.
A panoramic radiograph was obtained to reposition the brackets accordingly. The brackets form teeth #42 and 35 were repositioned to achieve root parallelism.
After bracket repositioning, a space opened between the lower right lateral incisor and canine and reseated so the SKL archwire was placed again to close that space (Figure 7C); four months after, the fixed appliances were removed (Figure 8). As retention a circumferential retainer was placed in the upper arch, while a fixed retainer made with a 0.0175” braided wire and bonded with fluid resin was placed in the lower (Figure 9).
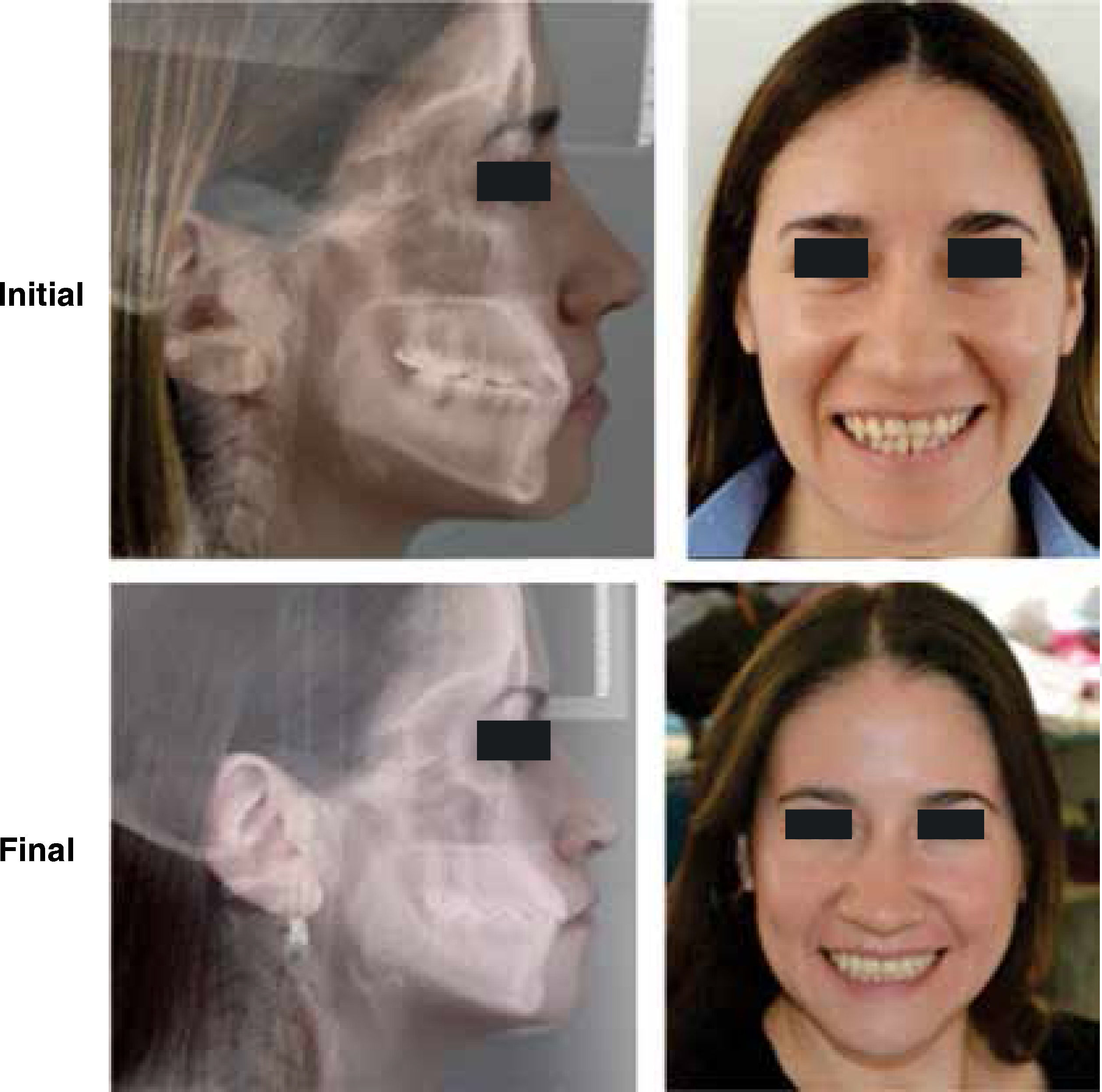
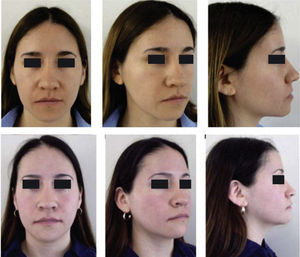
RESULTSThe arches were successfully correlated by eliminating the crossbite, the crowding was solved and the spaces were closed thus improving occlusal relationships and achieving molar and canine class I. The resulting overbite and overjet were adequate and remained under control. Periodontal status, aesthetics and function were favored (Figure 10) so the oral health and facial status of the patient was improved (Figure 11), emphasizing the harmony of a beautiful smile (Figure 12).
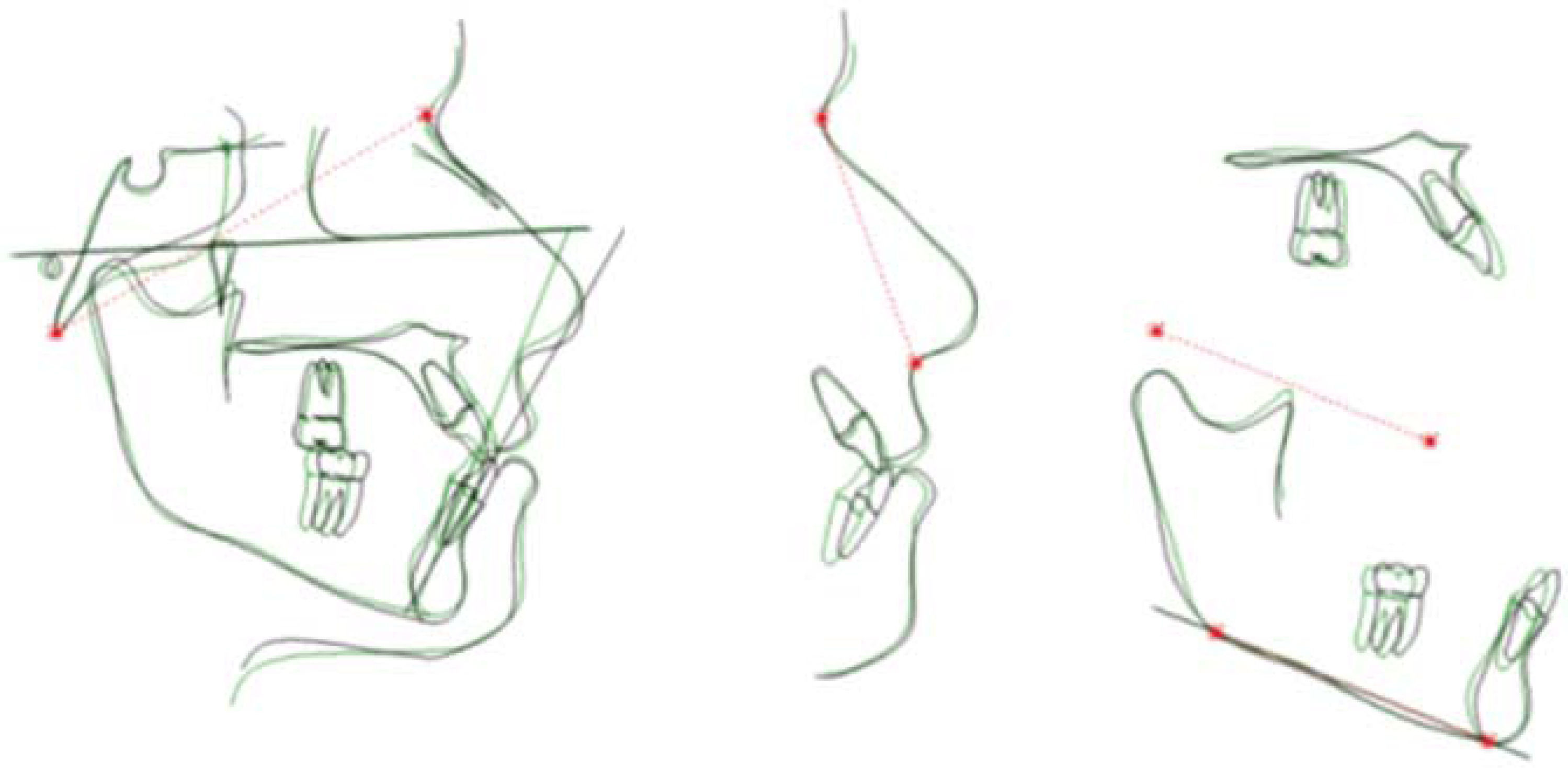
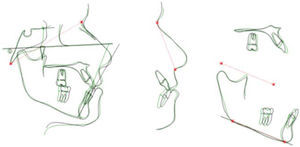
In the final cephalometry and in the superimposition, the skeletal changes were: initial facial depth: 94°, final: 92°; initial maxillary depth: 94°, final 95.4°; initial convexity: 0mm, final: 3.2mm; initial facial axis: 89°, final: 92.6°; initial Gn-GN/L1: 88°, final: 89°; initial SN/ U1: 100°, final 115° (Figure 13). It may be observed that a conservative treatment was performed since no surgical procedure was needed to correct the skeletal problem in addition to controlling periodontal health and improving the patient's esthetic conditions. However in order to achieve these results, the upper incisors were proclined (Figure 14).
Super impositions. Initial: red, final: blue
Color image available atwww.medigraphic.com/ortodoncia.
In spite of the periodontal conditions, it has been shown that orthodontic treatment is no longer a contraindication in the therapy of controlled periodontitis and may even improve the possibilities to save and restore the affected teeth.2,7–9
Interdisciplinary cooperation and that of the patient can transform the dental and periodontal problems into smiles and aesthetic and healthy dentitions. It is recommended that the orthodontist includes a periodontal evaluation during the patient's initial consultation and if a problem is detected in the stomatognatic system, it is important to refer the patient to the specific specialty for a more detailed diagnosis.3,4,12
It is considered that in patients with class III malocclusion, the discrepancy lies between centric relation and centric occlusion with reference to the sagittal plane and that many of these patients have a functional mandibular displacement that may result from a premature functional interference in the occlusion as presented in this case.13
It is important to emphasize that the use of fixed retainers in patients with a history of periodontal disease may be favorable because these type of retainers decrease secondary teeth movements and thus allows a positive environment for bone repair mechanisms. Interdisciplinary control remains important. In addition to the above-mentioned factors, a good retention can help achieve better results and a functional change for periodontally compromised patients with Class III malocclusion.2,13
CONCLUSIONSA proper assessment, a correct interdisciplinary diagnosis, a good treatment plan, proper orthodontic follow-up, good information for the patient and good patient cooperation are important factors for clinical management thus providing integrity of the periodontium, oral and facial aesthetics in addition to comprehensive health care for the patient.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia