Tuberculosis assumes several clinical forms and can affect almost any part of the human body. Before pharmacological treatment was discovered, half of afflicted subjects died before two years. Tuberculosis can be considered an ancient disease and worldwide strategy to eradicate it has only met with partial success. Presently in Mexico there has been an increase in number of conventional and extra-pulmonary tuberculosis cases. Non pulmonary sites can be found in the gastro-intestinal tract, central nervous system, skin, lymphs, mouth, temporomandibular articulation as well as ganglia at the cervical region. Diagnosis of extra-pulmonary tuberculosis is complicated, this is due to the variety of presentations and multiple differential diagnoses that need to be discarded. There are different diagnostic tests, some of them might even give a false negative. Standard diagnosis is achieved through mycobacterial culture. A systematic analysis of the literature is presented in this study; four clinical cases with tuberculosis cervical-facial manifestations are studied, describing protocol used to corroborate diagnosis and discard other conditions.
La tuberculosis tiene múltiples formas clínicas y puede afectar a casi cualquier parte del cuerpo humano. Antes de encontrarse su tratamiento farmacológico, la mitad de afectados fallecía antes de los dos años. Es una enfermedad antigua con una estrategia mundial para erradicarla con un éxito parcial. Actualmente en México existe un aumento del número de casos convencionales y extrapulmonares. Dichos sitios que no-pulmonares son a nivel del tracto gastrointestinal, sistema nervioso central, piel, linfa, cavidad oral, articulación temporomandibular, así como ganglios en región cervical Cuando se presenta extrapulmonar su diagnóstico es complicado por la variedad de presentaciones y múltiples diagnósticos diferenciales a descartar. Existen diferentes pruebas diagnósticas, algunas que inclusive pueden dar un falso negativo. Su diagnóstico estándar es mediante cultivo de micobacterias. Se presentan un análisis sistemático de la literatura, y se discute cuatro casos clínicos con manifestaciones cervicofaciales de tuberculosis, mostrando el protocolo que se uso para corroborar el diagnóstico y descartar otras patologías.
Tuberculosis (TB) is an infectious, communicable, chronic, granulomatous disease caused by Mycobacterium tuberculosis or Koch bacillus. This disease is generally located in the lung, but has been known to affect other organs.1 According to the World Health Organization (WHO) in 2013, an estimated 9,000,000 subjects were infected with TB; 1,500,000 deaths were attributed to TB, out of which 360,000 were found in HIV positive patients, and 80,000 were under 17 years of age. It has been estimated that 10 million children have been orphaned by parents’ death due to TB. On the other hand, according to WHO figures, 4,800,000 subjects have received timely diagnosis and early treatment.2,3 Large cities increasingly present overcrowding and poverty foci which can foster dissemination of the disease.4 In Mexico tuberculosis is still endemic. According to information used in the prevention and control program of tuberculosis in 2011, 19,445 new cases of all forms were presented. These TB cases were distributed as follows: 81.5% pulmonary, 5.6 ganglionic, 1.6 meningeal, and 11.4 of other types of TB. With respect to TB related cases 20.8% have been related to diabetes, 7.8% to AIDS; 9.3% were pediatric cases; In 2010, 2,414 deaths were related to this disease.5,6
TB is transmitted from one subject to the next by means of inhalation of the mycobacterium discharged by sick individuals while coughing, speaking or sneezing. Lack of detection of existent cases, and more recently appearance of resistance to traditional anti-tuberculosis drugs have rendered tuberculosis an important public health problem in Mexico.6
Initial infection caused by tuberculosis bacillus is transmitted through the air. Since Mycobaterium tuberculosis does not contain enzymes which might allow it to penetrate through mucus, microorganisms must be found in sufficiently small particles (lesser than 5 μ) so as to be able to penetrate into the alveolar space, a mucus free area, . Although the minimum M. tuberculosis dose for human being is still unknown, it has been found that in rabbits and guinea pigs one to three microorganisms might be sufficient.6,7 These first microorganisms will be ingested by alveolar macrophages, and since these are inactive, monocytes arriving to the site will not be able to kill intracellular M. tuberculosis, which will double within macrophages and will rapidly increase in number. During this period, before the onset of specific immunity, is when microorganisms will appear in lymphatic ganglia which drain the region, shortly after, bacteremia of hematogenous dissemination will occur.7,8
An immunological reaction takes place several weeks after uninhibited growth of M. tuberculosis, this has the result of interrupting bacterial growth. Microorganisms can be totally eliminated in the initial infection site, (primary infection), nevertheless, in sites of bacillary dissemination through the blood, microorganisms might persist for months or even years; microorganisms then begin to rapidly reproduce and result in the development of symptomatic tuberculosis. Although these lesions might be found in any location of the body, they are more frequently found in pulmonary apexes, bones, lymph nodes, meninges and kidneys. Initial contact with M. tuberculosis takes place at the periphery of the lung, where the bacillus has been deposited through inhalation. The tuberculosis bacillus establishes a localized infection which, initially results in few or even no clinical signs.9,10
Local dissemination towards hilar lymph nodes is frequent; from there, microorganisms enter the bloodstream and disseminate towards other parts of the body. This microorganism dissemination results in pulmonary and extra-pulmonary foci which are responsible for the main clinical manifestations of tuberculosis. Initial X rays can reveal an increase in size of lymph nodes and occasionally, at a later point, there is calcification of lymph nodes and parenchymal lesion; this constitutes the classic Ghon complex (Figure 1) and suggests not only a previous tuberculosis infection, but also presence of disease such as histoplasmosis.10 At initial bacteremia stages, in most patients, no additional tuberculosis signs develop, because local and general defenses curb the infection. Post-primary or reactivation pulmonary tuberculosis is frequently developed after a latency period, it originates from the hematogenous dissemination sites; initial infection due to tuberculosis bacillus frequently lacks clinical importance and is overlooked. In most patients, the disease is preserved latent for an indefinite time or even for years, and reveals itself at an episode of immunodeficiency.4,10
Pulmonary tuberculosis is the most frequent and most contagious form of tuberculosis, it represents about 80 to 85% of total cases. It first appears with respiratory signs such as dry cough, expectoration with or without hemoptysis, thoracic pain and general symptoms such as anorexia, asthenia, adynamia, night sweats, loss of weight and sometimes prolonged fever. In tuberculosis patients, examination of respiratory system oftentimes yields normal results, in spite of extensive radiologic compromise.
Extra-pulmonary tuberculosis: It comprises 15 to 20% of all tuberculosis cases, and affects organs located outside the lung.3,11,12
Pleural and ganglionar extra-pulmonary tuberculosis are the most frequent forms, followed by genitourinary tuberculosis, symptoms of extra-pulmonary tuberculosis depend on the affected organ. The first lesion produced by the bacillus upon entering the system is a lung pulmonitis, and ulceration at the last portion of the ileum, or an inflammatory focus in the tonsil. Parenchymal process, lymphangitis and adenitis constitute primary tuberculosis and are known as Ranke's primary complex.13 This condition clears in almost all cases, only leaving a relative immunity detected through thorax X-rays.
Comprehensive evaluation of a patient suspected of having contracted TB includes clinical history, physical exploration, thorax x-rays and microbiological cultures. It might also include tuberculin test (TST) and serological tests. Tuberculin test (TST) with a purified protein derivative plays a limited role in active TB diagnosis, especially in older patients identified with latent TB. A negative test does not discard active TB diagnosis in elderly patients in cases when epidemiological, clinical and radiographic characteristics are present which might support the diagnosis. TST might be negative in approximately 20% of cases at the time of active disease. Tests with gamma g interferon have been introduced for TB detection in peripheral blood, this test is conducted by means of stimulation of mononuclear cells exposed to M tuberculosis specific antigens in order to identify this bacillus. Sensitivity is 80% although specificity for active disease is lesser, differing in this aspect from latent infection.4
It is difficult to establish TB diagnosis in pediatric population, since a practical method to achieve this is still lacking. Sputum is positive in less than 10% of all tests, bacteriological culture is positive in only 30% of all cases. In TB patients, thorax X-rays play an important role in the detection, diagnosis and responses to treatment, nevertheless, they can be normal or show non-specific mild signs in patients with active disease. Thorax X-ray constitutes the main diagnostic support, nevertheless, normal radiological findings will be encountered in 15% of all TB patients.3
Computerized tomography (CT) is more sensitive than thorax x-rays in the detection and characterization of local or disseminated subtle parenchymal disease and mediastinal lymphoadenopathy. Radiologic diagnosis of TB is only correct in 49% of cases, 34% in primary TB and 59% in TB reactivation. Differing from CT, where pulmonary TB diagnosis is correct in 91% of patients and TB is correctly excluded in 76% of cases. High resolution CT is useful to detect small cavitation foci in areas of confluent pneumonia, areas of dense nodularity and scarring. CT is also useful in the evaluation of complications, it can reveal a pleural disease which is not evident in thorax X rays. It plays an important role in complicated multi-drug resistant TB, since multiple cavities increase expectoration of a large number of bacteria as well as endobronchial dissemination in previously unaffected areas of the lung-.12
Post Emission Tomography (PET) with carbon 11 Colina (11C-Colina) might be useful to differentiate between pulmonary cancer and tuberculosis. Standardized uptake value (SUV-max) is high in malignant masses and low in tuberculosis with C11 Colina; in patients with pulmonary cancer, SUV-max with 18-fluoro-2-deoxyglucose (FDG) and C-Colina are high. Limited penetration of drugs within cavities that lodge a great number of mycobacteria contributes to drug resistance. Therefore, surgery might be an adjuvant in the treatment of MDR TB; nevertheless chemotherapy is considered the most reliable treatment for MDR TB. CT can locate cavitation site as well as extension of active disease and provide a mapping for surgical treatment planning.10,11 In classical descriptions, when an established diagnosis is presented, an excision of adenopathies is conducted to obtain diagnosis. This procedure frequently elicits complications such as torpid healing or fistula formation which can end in requiring a new intervention.14,15
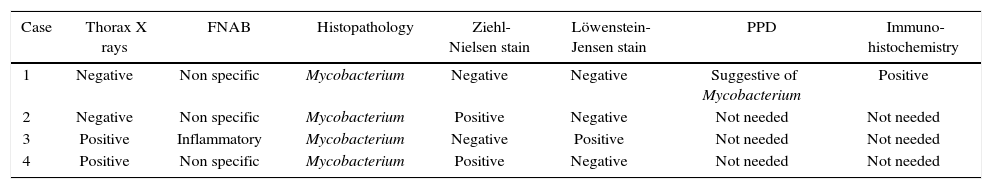
MATERIAL AND METHODSA convenience selection of patients treated in 2012-2014 at the Regional Hospital «Ignacio Zaragoza» (ISSSTE) was conducted. Patients had been diagnosed with tuberculosis and were residing in the eastern area of Mexico City. These four cases were selected due to diagnosis controversy. In selected cases, FNAB (fine needle aspiration biopsy) diagnostic tests were conducted as well as thorax X-rays, tomograms, Ziehl-Neelsen test, Lowenstein- Jensen culture and positive immunohistochemistry to Mycobacterium tuberculosum. Definite diagnosis was achieved with three out of the six positive tests. In anamnesis, patients of this selected sampling informed of middle social and financial status, practice of adequate hygiene habits, lack of crowding, and absence of related hereditary familial history.
CLINICAL CASESCase 1: 11 year old femaleLeft submandibular tumor of 2 year evolution. Lesion measured 12 × 22mm, was mobile, indurated, adhered to deep planes (Figures 1 and 2) History of varicella (chickenpox).
Presence of local pain, 38° C fever, with repeated episodes. Thorax x ray revealed negative results, local tomographic study confirmed presence of lymphadenopathy. FNAB tests revealed non-specific results. An incision biopsy was performed which provided an unspecific histopathological result suggestive of mycobacterium granulomatous infection. Ziehl-Neelsen test was negative, Löwenstein-Jensen culture was negative, PPD (purified protein derivative) test suggested mycobacterium infection. A sample was sent to be subjected to immunohistochemical study; it revealed positive to Mycobacterium tuberculosum.
After a one year control period, evolution was adequate without presence of any other lesion. Patient was transferred to the infectious diseases department.
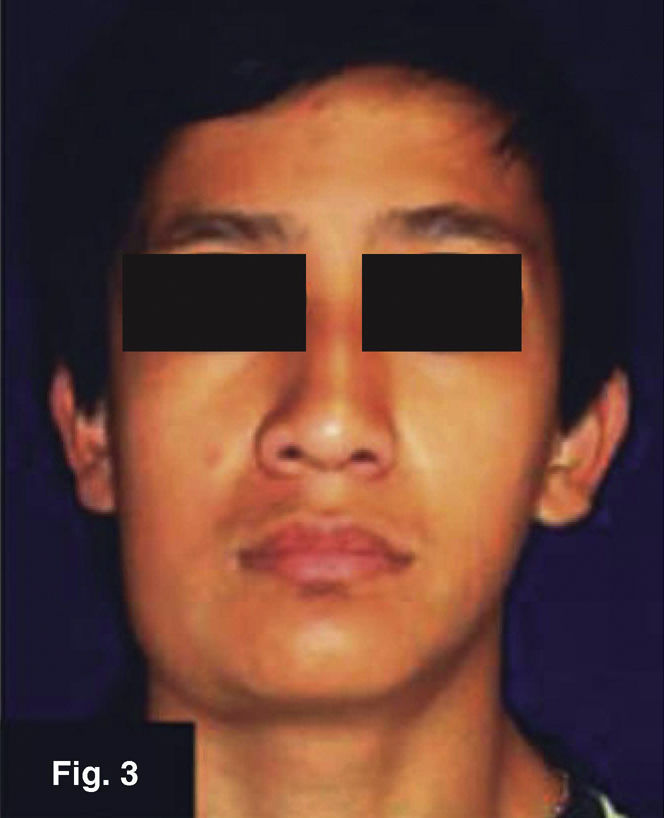
Case 2: 16 year old maleRight submandibular tumor of 10 month evolution. Lesion measured 14 × 32mm, was mobile, indurated and adhered to deep planes (Figures 3 and 4) history of contusion was reported in the right mandibular region with asymptomatic volume increase. Treatment with anti-inflammatory drugs elicited no results. Patient denied presence of pain or fever peaks. He exhibited a thorax X-ray protocol study with negative results. Lymphoadenopathy confirmed by tomogram. FNAB yielded unspecific results. Excision biopsy was undertaken, it yielded histopathological results of Mycobacterium tuberculosum granulomatous infection. Ziehl- Neelsen test yielded positive, Löwenstein-Jensen culture yielded negative.
At a one year control visit it was observed that evolution was adequate, no other lesion was present. The case was transferred to the infectious diseases department.
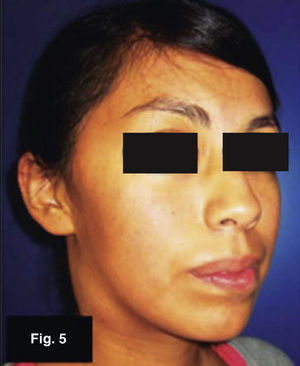
Case 3: 19 year old femaleTumor in the region of the right carotid triangle of three month evolution. Lesion measured 35 × 20mm, was mobile, indurated and adhered to superficial planes (Figures 5 and 6). Patient denied presence of trauma, infections or change of habits. No pain or fever peaks were reported. Thoracic X-ray study yielded positive, FNAB yielded non specific inflammatory results. Tumor was excised resulting in mycobacterium tuberculosum granulomatous infection. Zeihl-Neelsen test was negative, Löwenstein-Jensen test was positive.
At the one year control visit it was observed that evolution was adequate and no other lesions were present. The case was transferred to infectious diseases department.
Case 4: 52 year old maleThe patient exhibited mandibular ridge fistula and tumor in the right oral region of four months evolution. Lesion measured 20x21mm, was mobile, indurated, adhered to deep planes with erythematous color (Figures 7 and 8). The patient reported noncontributory history, and denied presence of pain or fever peaks. FNAB was conducted and yielded non specific results. Excision biopsy was performed, which yielded histopathological results of granulomatous infection. Ziehl Nielsen test yielded positive results for microbaterium tuberculosum, Löwenstein-Jensen yielded negative results.
The lesion evolved to a scrofula which was drained and closed, constant infections were present. After two months, lesion healed with treatment of dicloxacillin and rinses. This enabled adequate evolution and transfer to Infectious Diseases Department.
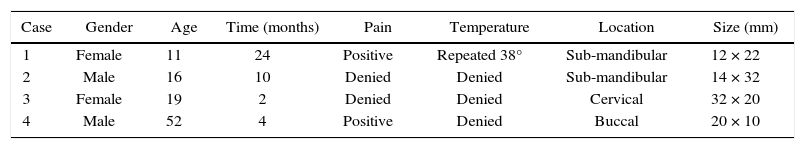
ANALYSISPatient's records and results are recorded in Tables 1 and 2. The fact that tuberculosis patients’ age does not show predilection for a specific stage of life hinders diagnosis.
Resume of specific studies.
| Case | Thorax X rays | FNAB | Histopathology | Ziehl-Nielsen stain | Löwenstein- Jensen stain | PPD | Immuno- histochemistry |
|---|---|---|---|---|---|---|---|
| 1 | Negative | Non specific | Mycobacterium | Negative | Negative | Suggestive of Mycobacterium | Positive |
| 2 | Negative | Non specific | Mycobacterium | Positive | Negative | Not needed | Not needed |
| 3 | Positive | Inflammatory | Mycobacterium | Negative | Positive | Not needed | Not needed |
| 4 | Positive | Non specific | Mycobacterium | Positive | Negative | Not needed | Not needed |
Assessment of thoracic x-rays reveals that there is no definite correlation between extra-pulmonary TB and Ghon complex . Patient 1 (Figure 9). Sputum bacilloscopy and fine needle aspiration biopsy were non specific and failed to provide contributory results.
In the 11 year old female, the results of the anatomical and pathological study, although very precise, were not able to identify the bacillus, thus corroboration with immunohistochemistry and tuberculin was required.
In most cases TB proved positive in histopathological study which confers this study greater diagnostic effectiveness.
Identification of alcohol acid resistant bacilli was positive in 75% of cases, this was the case for males: for females it was non specific or not assessable.
In all cases, tomography only provided confirmation of lymphoadenopathy, for this reason it was not taken into account in the analysis; FNAB and sputum bacilloscopy results were non specific in cases of chronic inflammation.
DISCUSSIONBefore discovering treatment, mortality rate of this disease was 50% in the two first years. Present treatment is pharmacological.16 Tuberculosis, (TB) can appear under many forms, and affects almost any part of the human body. When it appears in sites outside the lungs it is known as extra pulmonary tuberculosis, these sites can be those involving gastrointestinal tract, central nervous system, skin, lymph mouth or cervical region.1,13
For the onset of the disease in the mouth there are systemic and local predisposing factors. These can be local factors such as poor oral hygiene, local trauma, pre-existing lesions such as leukoplakia, periapical granuloma, cysts, abscesses and periodontitis. There are also systemic predisposing factors such as resistance to immunosuppression or nutritional deficiencies which increase a patient's susceptibility to a tuberculosis infection in the facial region.2
WHO reports that extrapulmonary tuberculosis (ETB) accounts for 10-20% of the total worldwide TB cases. Nevertheless, this frequency notably increases in subjects afflicted with some degree of immunodeficiency. Severely immuno-depressed subjects afflicted with TB and AIDS might present extra-pulmonary locations in up to 60% of the cases. No literature was found at the Regional Hospital Ignacio Zaragoza with reports of statistical indicators of extra-pulmonary tuberculosis prevalence or incidence.2
With exception of pleural involvement, the most frequent location is found in ganglia, followed by genitourinary and osteoarticular locations; remaining locations are very infrequent.1,2 TB cases, although initially in the lung, can or cannot be visible in thorax X-rays. It has been acknowledged that from this primary pulmonary focus dissemination might occur. This can be produced either by contiguity, via the lymphatic system, or haematogenously. This latter conduct causes most cases of extra-pulmonary TB cases.13
The four cases of extra-pulmonary TB here presented show the difficulties existing in emitting accurate diagnosis as well as the multiple negative results obtained from ETB common tests. There is therefore a clear need to corroborate with the help of multiple diagnostic tests so as to avoid the aforementioned false negatives.4 With the advent of efficient chemo-therapeutic agents, the need for surgical treatment of TB in all its forms has practically disappeared. Presently, surgery in ETB treatment is only indicated in two special situations: harvesting valid samples for the diagnosis (biopsies) and as a therapeutic option in rare situations of sequels and complications of this disease.17,18
According to Basgoz, extrapulmonary TB exhibits negative bacilloscopy, therefore, its transmission potential is practically non-existent, as well as the diagnostic ability of the sputum test; this is consistent with our study, where in all four ETB cases, nonexistent bacilloscopy was found.19
CONCLUSIONSTuberculosis cases demand accurate diagnosis since there is no 100% accurate diagnostic test, and results must always be corroborated with clinical tests. A diagnosis protocol must include tuberculosis in all cervical adenopathies, especially in unilateral adenopathies, where some type of immunosuppression is involved. New cases must be reported to the institution in order to feed national statistics and approach the problem in a comprehensive manner. In order to discard TB from these alterations, excisional biopsy of cervical-facial adenopathies must be accompanied by an evaluation as well as bacteriological culture.
An accurate diagnosis favors suitable resolution of the disease, thus preventing drug-resistant tuberculosis. Thorax X-rays, although suitable as an initial study, do not totally dismiss presence of TB in a patient's system.
Fourth year student, Maxillofacial and Oral Surgery Master's Program, National School of Dentistry, National University of Mexico (UNAM), Regional Hospital «General Ignacio Zaragoza» ISSSTE, Mexico City.
Este artículo puede ser consultado en versión completa en http://www.medigraphic.com/facultadodontologiaunam