Facial emotion recognition (FER) is a fundamental component in social interaction. We know that FER is disturbed in patients with severe mental disorder (SMD), as well as those with a history of childhood trauma.
Material and methodsWe intend to analyze the possible relationship between the existence of trauma in childhood irrespective of a SMD, measured by the CTQ scale and FER, in a sample of 3 types of subjects (n = 321): healthy controls (n = 179), patients with BPD (n = 69) and patients with a first psychotic episode (n = 73). Likewise, clinical and socio-demographic data were collected. The relationship was analyzed by a technique of multivariate regression adjusting for sex, age, IQ, current consumption of drugs and group to which the subject belonged.
ResultsSexual and / or physical trauma in childhood related independently to the existence of SMD with a worse total FER ratio, as well as to a worse rate of recognition in expressions of happiness. Furthermore, the subjects with a history of childhood trauma attributed expressions of anger and fear more frequently to neutral and happy faces, irrespective of other variables.
ConclusionsThe existence of trauma in childhood seems to influence the ability of subjects to recognize facial expressions, irrespective of TMG. Trauma is a preventable factor with specific treatment; therefore, attention should be paid to the existence of this background in clinical populations.
El reconocimiento de las expresiones faciales (REF) es un componente fundamental en la interacción social. Sabemos que dicho REF se encuentra alterado tanto en los pacientes con trastorno mental grave (TMG), como en aquellos que padecen antecedentes de trauma infantil.
Material y métodosPretendemos analizar la posible relación entre la existencia de trauma en la infancia más allá de la presencia de un TMG, medido mediante la escala CTQ y el reconocimiento de las expresiones faciales, en una muestra con 3 tipos de sujetos (n = 321): controles sanos (n = 179), pacientes con TLP (n = 69) y primeros episodios psicóticos (n = 73). Así mismo, se recogieron variables clínicas y datos socio-demográficos. Se analizó dicha relación mediante una técnica de regresión multivariante ajustando por el sexo, la edad, CI, el consumo actual de tóxicos y grupo al que pertenece el sujeto.
ResultadosEl trauma sexual y/o físico en la infancia se relacionó de forma independiente a la existencia de TMG con un peor ratio de REF total, además de con una peor tasa de reconocimiento en las expresiones de felicidad. Además, aquellos sujetos con antecedentes de trauma en la infancia atribuyeron con mayor frecuencia expresiones de enfado y miedo a las caras neutras y felices independientemente de otras variables.
ConclusionesLa existencia de trauma en la infancia parece influir de manera independiente al TMG en la capacidad de los sujetos de reconocer expresiones faciales. Dado que el trauma es un factor prevenible y con un tratamiento específico, se debería prestar atención a la Existencia de este antecedente en las poblaciones clínicas.
Facial emotion recognition (FER) is a social cognition component and is often measured through assessment of the subject’s ability to recognise basic emotions based on facial expression.1 FER learning begins in childhood and continues through adolescence and adulthood.2 Several studies show that the normal development of a FER capacity may be disturbed by the existence of childhood abuse.3,4 A recent review suggests that this type of child demonstrates an overall worse FER and greater reactivity in specific areas of the brain in response to negative facial expression, particularly to anger.5
We know that a history of abuse in childhood is not just related with difficulty in recognition, expression and understanding of emotions,6 but that there is also a higher possibility of developing anxiety, mood disorders, abuse of substances and antisocial behaviour in adult age7 by people suffering from it. A recent study has investigated the long-term effects of abuse and negligence of care during the emotional process, demonstrating that in adulthood the subjects with a history of child abuse are less precise when recognizing emotions than people without a history of abuse.8 Physical abuse has recently been associated with difficulties in recognition of neutral images, whilst emotional negligence and sexual abuse was associated with a poorer recognition of happy expressions.9 Pollak et al.10 reported that recognition of angry faces was altered in children with a recent history of trauma. These alterations exclusively appeared in children who had suffered from emotional or physical negligence, whilst physically abused children did not present with this alteration compared with healthy controls. Similarly, differences were reported between healthy control groups and children who had suffered from emotional and physical negligence in the recognition of expression of anger, sadness and fear. In other studies alternations in the FER of anger and fear were also described in abused children when they were compared with children who had not been abused.11
It is a well-known fact that subjects with severe mental disorders such as psychosis or borderline personality disorder (BPD) present with alterations in their perception of emotions throughout the phases of their disease.12,13 These alterations in emotion recognition may occur not just in patients with psychiatric disorders but also in healthy children and adults with a past of childhood abuse.10 We also know that childhood trauma occurs in a very high percentage of patients with psychosis or BPD.14,15 Although few studies have analysed the existing relationship between the FER and childhood abuse among adult psychiatric groups, there are studies which describe an association between the difficulty in recognizing the expression of distaste and patients with BPD diagnoses and a background of emotional and/or physical abuse in childhood,16 and studies which speak of poorer FER in patients with psychosis and a history of childhood trauma.17
The aim of this study was to analyse the independent relationship of childhood trauma with FER in a sample with three types of subjects: patients with a first psychotic episode (FPE), patients with diagnosis of BPD and healthy control groups. Our initial hypothesis consisted in thinking that subjects with a history of childhood abuse would have a poorer recognition of facial expressions regardless of other variables, including the group to which they belonged. This difficulty in expression recognition could also be accompanied by a bias in the attribution of emotions, most frequently being that the subjects with a history of trauma would recognize negative faces (anger, fear….) in neutral or happy emotions.
Material and methodsSampleThe recruitment process of this study has been described previously.18 Data were obtained from a convenience sample of patients with a FPE who had been consecutively admitted into the acute treatment unit of the Hospital Universitario Basurto (HUB). Patients with BPD were recruited from the day hospital of the AMSA Clinic and the HUB. Control groups were recruited from the general population in the same area as the clinical groups through public adverts. The recruitment period was between January 2012 and January 2017. Patients were assessed when the psychiatrist in charge considered that they were clinically stable and could offer their consent. Inclusion criteria were as follows: for the three groups: aged between 18 and 65 years, sufficient knowledge of Spanish and IQ > 70. The patients with a FPE had to meet with the following requisites as well: antipsychotic medication for at least one year; DSM IV-TR diagnostic criteria for affective psychotic or non affective criteria disorder. The exclusion criteria for the three groups were: past or current history of neurological and/or TCE, disabling medical disease and current dependence on any type of substance. The healthy control groups did not have any close family members affected by psychosis. All the subjects signed an informed consent form and accepted to participate in the study. The Operational Criteria Checklist for the psychosis was completed, based on clinical tools and relevant clinical history data to establish the patients’ psychosis diagnoses, using the OPCRIT19 programme. Socio-demographic and clinical variables from the whole sample were collected. The sample patients were clinically stable when assessed. The protocol was administered by psychologists/psychiatrist who had been trained for this purpose.
ToolsThe Childhood Trauma Questionnaire (CTQ-SF) validated into Spanish20 was first used retrospectively to establish the rate of trauma in the three groups. The reduced version of 25 items was used, which derived from the original of 70.21 This questionnaire covers five aspects of the history of physical abuse, emotional abuse, sexual abuse, physical and emotional negligence. Each item uses a 5 point scale to determine the frequency or severity of the traumatic experience. The score of each type of trauma may be calculated separately. This scale may be used both in clinical and non clinical population groups. To define the presence or absence of trauma the following cut-off points were used: emotional abuse ≥ 13; physical abuse ≥ 10; sexual abuse ≥ 8; emotional negligence ≥ 15; physical negligence ≥ 10.22 The shortened version of the CTQ has proven to have a good criteria of validity.23 To increase the statistical power of the sample three trauma variables were created: CTQ1 = existence of abuse or emotional negligence; CTQ2 = existence of any type of physical trauma or sexual abuse, and CTQ3 = existence of any type of abuse. The Benton24 facial recognition test was used to measure the ability to recognize emotions in unfamiliar faces. This test served to eliminate subjects from the sample who scored below normal rates. It was used for Degraded Facial Affect Recognition Task (DFAR)25 to measure the subjects’ emotional facial recognition ability. The test comprised faces of 4 subjects (2 male and 2 female). The faces are presented in a series of photographs which represent different emotional expressions. The three groups were asked to indicate the expression of each face using a button and to respond with the highest possible precision. The photographs of the faces had been previously passed through a filter which faded the images by 30%. This method was adopted to increase the difficulty in recognition and interpretation of facial expressions. The subjects were presented in 64 photographs, formed by 16 presentations of the following options: anger, happiness, fear and neutral affection. During analysis the total proportion of correct answers for the facial expressions were used. High ratings in the DFAR were indicative of a higher capacity to recognize facial expressions. The test was programmed using EPrime 1.1 (Psychology Software Tools, Pittsburgh, Pennsylvania) software.
The short version of the Wechsler adult intelligence scale (WAIS-III)26 was administered to assess the intellectual coefficient. This version includes the following tests: “cubes” (only odd items); “number key”, “arithmetic” (odd items) and “information” (items: 6, 9, 12, 15, 18, 21, 24 and 27).
Statistical analysisFor the descriptive analysis, frequencies and percentages were used for the qualitative variables and mean, standard deviation (SD) and range for the quantitative. The Kolmogorov-Smirnov test was used to confirm the normality of quantitative variables. Socio-demographic differences were analyzed as was the presence of trauma, and the percentage of correct answers in the DFAR test between the three patient groups. To compare quantitative variables the ANOVA test was used or the Kruskal-Wallis test if normality requisites were not complied with. To compare qualitative variables the Chi-square test was used or the exact Fisher test. For multiple comparisons the Bonferroni correction was used. Differences in relation to the percentage of right answers in the DFARtest depending on the type of trauma involved, and the percentage of errors in attribution, were found with the t-test or the Mann-Whitney U non-parametric test. To determine the magnitude of the differences the size effects (SE) were calculated, including the difference of means between the groups divided by the joint SD.27 To classify the magnitude of the differences the thresholds established by Cohen were used: below 0.20 was not significant, between 0.20 and 0.50 was small, between 0.50 and 0.80 was moderate and above 0.80 was large.
Finally, the general lineal model was used to study the relationship regardless of the trauma in childhood with recognition of emotions and the type of error in attribution of the same, adjusted by the group to which the subject belonged, age, sex, IQ and current toxic substance consumption. In the final model only statistically significant variables were considered. The results were presented using parameter β, together with a 95% confidence interval. Also, for each model the R2 coefficient was presented. This was considered a statistically significant result for p < .05. Statistical analyses were carried out with version 12 of the statistical programme STATA.28
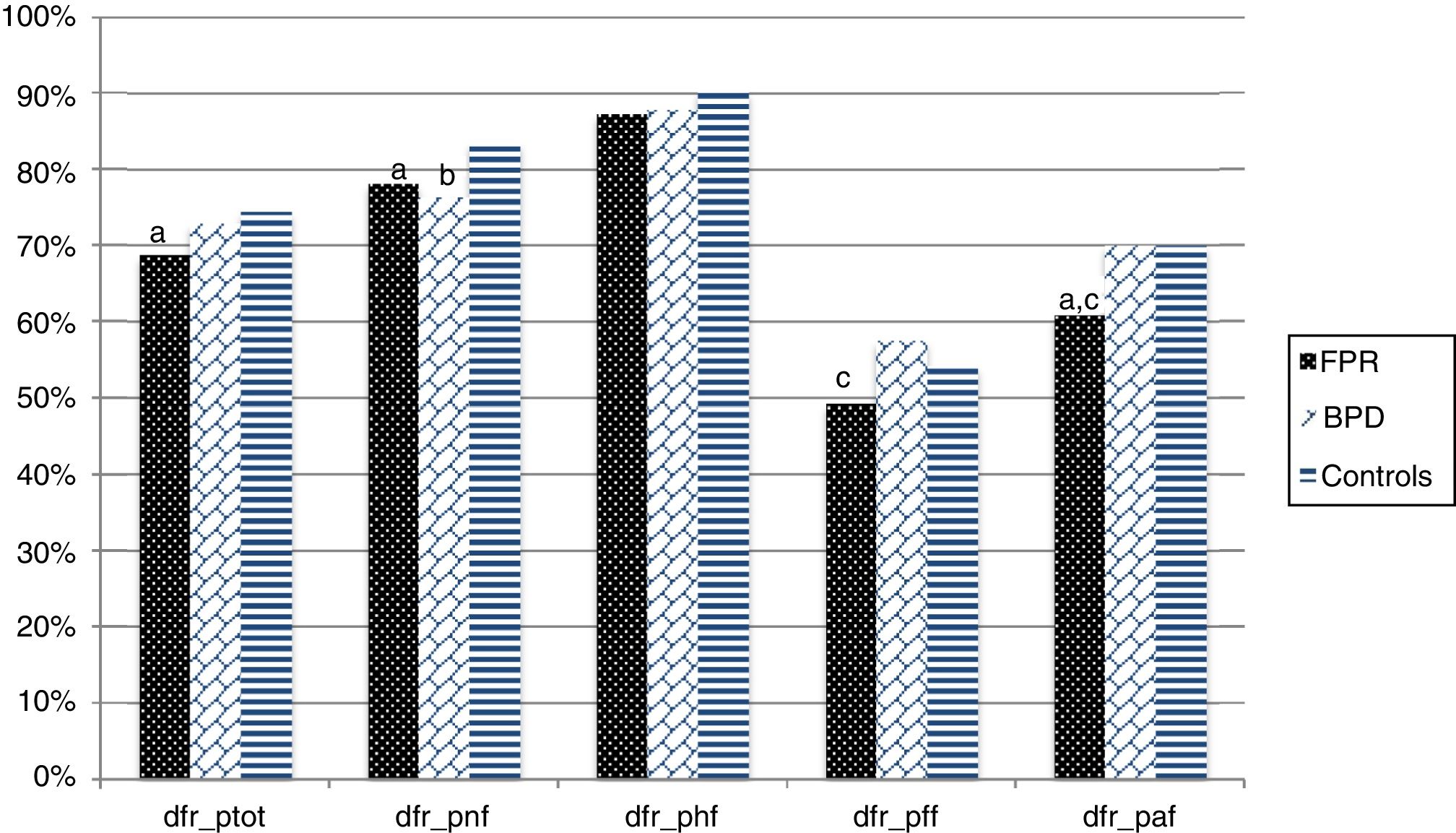
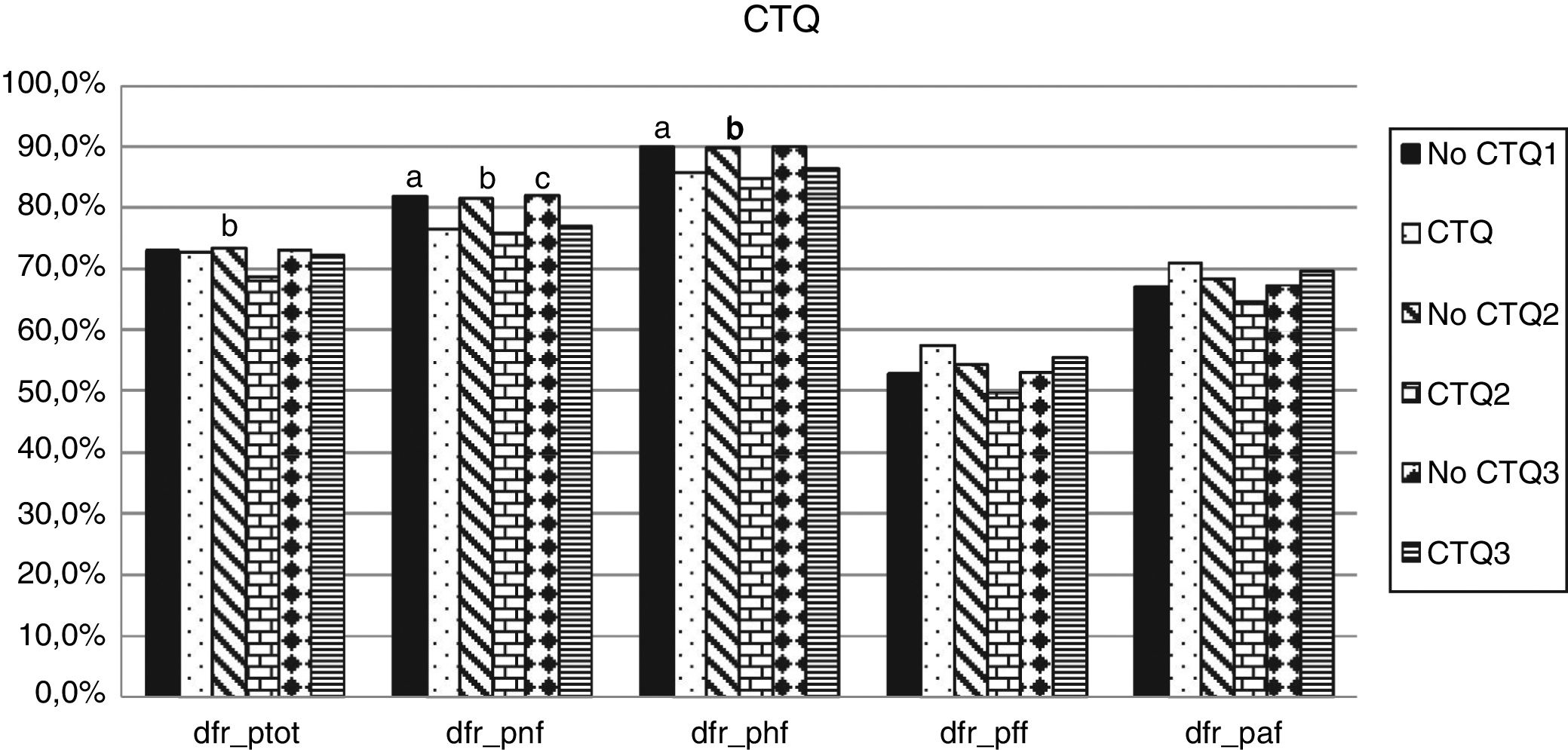
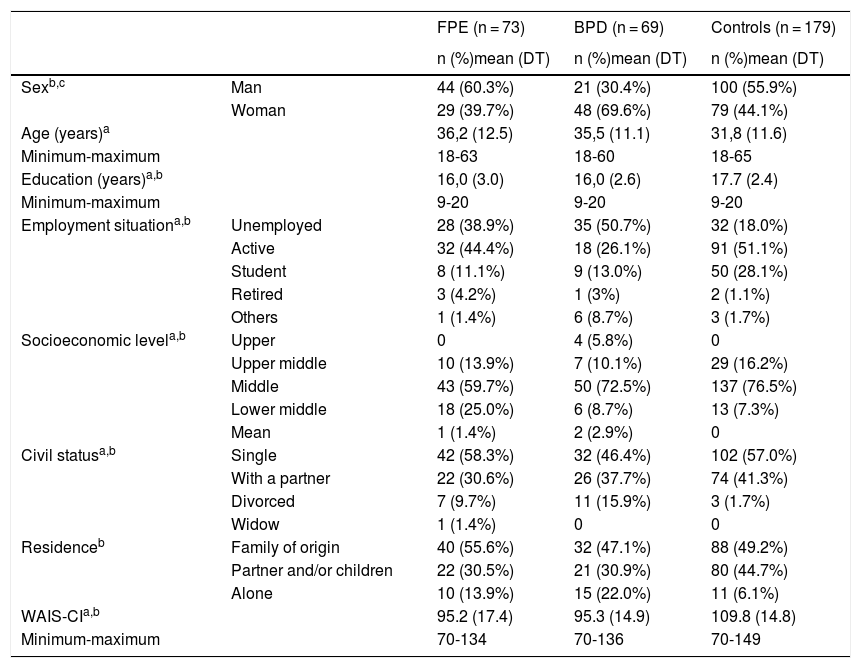
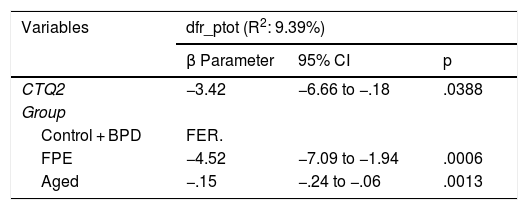
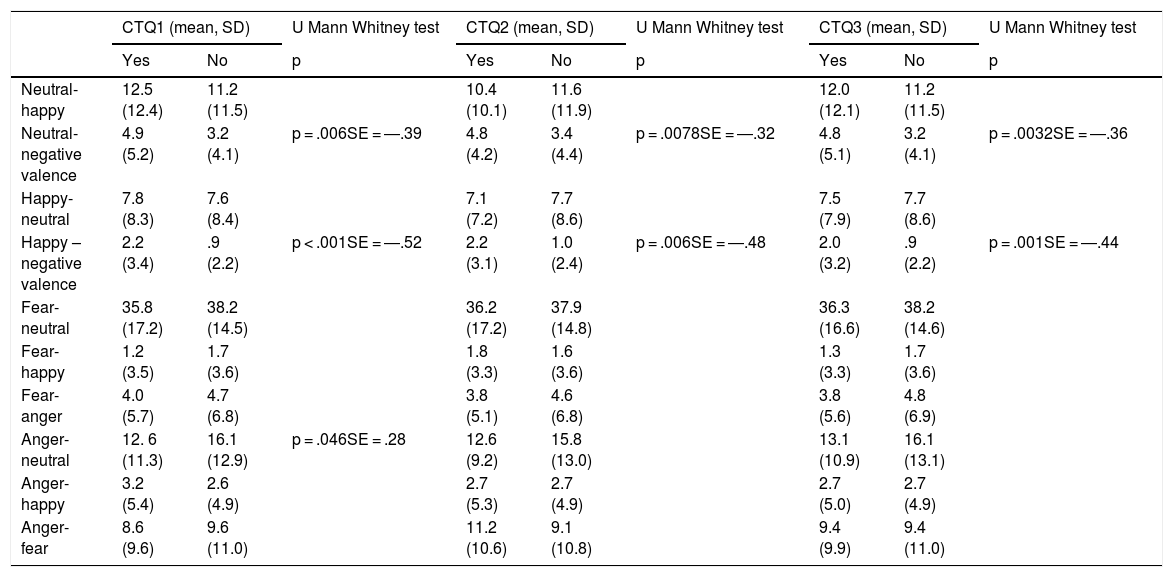
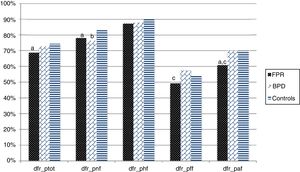
ResultsA sample of 73 FPE, 69 BPD and 179 healthy controls were recruited. The main socio-demographic characteristics together with the differences between groups of the sample are shown in Table 1. 24.6% of the sample stated they had suffered from some type of abuse in childhood (CTQ3). The group with the highest rate of abuse was that of the BPD (66.7% vs 27.4% in FPE and 7.3% in controls, p < 00001). Regarding emotional abuse (CTQ1), 56.5% of the BPD stated they had suffered from it compared with 5.6% of the control group or 21.9% of the FPE (p < .0001). Regarding physical and/or sexual abuse (CTQ2), up to 37.7% of the BPD of the sample had presented with it, compared with 3.3% of the controls and 13.7% of the FPE (p < .0001). Fig. 1 shows the percentage of correct response in the DFR test according to the group to which the subject belongs, together with their statistical differences. Fig. 2 shows the differences in the percentage of FER between the different types of abuse found in the sample. The existence or emotional abuse or negligence (CTQ1) was related to poorer recognition of neutral faces (81.9% vs. 76.5%, SD = 14.4; ES = .38; p = .006) and happy (90% vs. 85.9%, SD = 10.7; ES = .38; p = .036). Similarly, the existence of physical and/or sexual abuse (CTQ2), which was related to poorer total recognition of facial expressions (73.5% vs. 68.8%, SD = 10.2; SE = .46; p = .0103), of neutral faces (81.6% vs. 75.9%, SD = 14.4; ES = .4; p = .019) and happy faces (89.3% vs. 84.8%, SD = 10.7; SE = .47; p = .024). In this case the size effect is small but is very close to the moderate grade (.5). These significant differences are maintained for the CTQ3 but with a lower effect size, except in total recognition (neutral faces: 82.1% vs. 77%, SD = 14.4; ES = .35; happy faces: 90% vs. 86.6%; DS = 10,7; TE = 0,32). With regard to the relationship between the existence of abuse and the FER adjusted by age, sex, IQ, group to which the subject belongs and current substance consumption (Table 2), we may observe that the percentage of total correct response in the DFAR test are impacted by the group to which the subject belongs, age and physical and/or sexual abuse (CTQ2). This means to say, belonging to the FPE group (related to the reference group, controls and BPD), the existence of this type of trauma and an older age, is related to fewer total correct answers in the DFAR test. Regarding neutral faces, only the group to which the subject belonged was of influence.
Sociodemographic variables.
| FPE (n = 73) | BPD (n = 69) | Controls (n = 179) | ||
|---|---|---|---|---|
| n (%)mean (DT) | n (%)mean (DT) | n (%)mean (DT) | ||
| Sexb,c | Man | 44 (60.3%) | 21 (30.4%) | 100 (55.9%) |
| Woman | 29 (39.7%) | 48 (69.6%) | 79 (44.1%) | |
| Age (years)a | 36,2 (12.5) | 35,5 (11.1) | 31,8 (11.6) | |
| Minimum-maximum | 18-63 | 18-60 | 18-65 | |
| Education (years)a,b | 16,0 (3.0) | 16,0 (2.6) | 17.7 (2.4) | |
| Minimum-maximum | 9-20 | 9-20 | 9-20 | |
| Employment situationa,b | Unemployed | 28 (38.9%) | 35 (50.7%) | 32 (18.0%) |
| Active | 32 (44.4%) | 18 (26.1%) | 91 (51.1%) | |
| Student | 8 (11.1%) | 9 (13.0%) | 50 (28.1%) | |
| Retired | 3 (4.2%) | 1 (3%) | 2 (1.1%) | |
| Others | 1 (1.4%) | 6 (8.7%) | 3 (1.7%) | |
| Socioeconomic levela,b | Upper | 0 | 4 (5.8%) | 0 |
| Upper middle | 10 (13.9%) | 7 (10.1%) | 29 (16.2%) | |
| Middle | 43 (59.7%) | 50 (72.5%) | 137 (76.5%) | |
| Lower middle | 18 (25.0%) | 6 (8.7%) | 13 (7.3%) | |
| Mean | 1 (1.4%) | 2 (2.9%) | 0 | |
| Civil statusa,b | Single | 42 (58.3%) | 32 (46.4%) | 102 (57.0%) |
| With a partner | 22 (30.6%) | 26 (37.7%) | 74 (41.3%) | |
| Divorced | 7 (9.7%) | 11 (15.9%) | 3 (1.7%) | |
| Widow | 1 (1.4%) | 0 | 0 | |
| Residenceb | Family of origin | 40 (55.6%) | 32 (47.1%) | 88 (49.2%) |
| Partner and/or children | 22 (30.5%) | 21 (30.9%) | 80 (44.7%) | |
| Alone | 10 (13.9%) | 15 (22.0%) | 11 (6.1%) | |
| WAIS-CIa,b | 95.2 (17.4) | 95.3 (14.9) | 109.8 (14.8) | |
| Minimum-maximum | 70-134 | 70-136 | 70-149 |
Percentage of correct answers in the DFR test depending on the subject group.
*Statistical significance (p < .05); dfr_tot: percentage of total right answers; dfr_pnf: percentage of right answers for neutral facial expressions; dfr_phf: percentage of right answers for happy facial expressions; dfr_pff: percentage of right answers for fearful facial expressions; dfr_paf: percentage of right answers for angry facial expressions.
aThe differences are statistically significant (p < .05) between the control group and the FPE group.
bThe differences are statistically significant (p < .05) between the control group and the BPD group.
cThe differences are statistically significant (p < .05) between the FPE group and the BPD group.
Percentage of correct answers in the DFR test according to type of trauma suffered from.
* Statistical significance. dfr_tot: percentage of total right answers; dfr_pnf: percentage of right answers for neutral facial expressions; dfr_phf: percentage of right answers for happy facial expressions; dfr_pff: percentage of right answers for fearful facial expressions; dfr_paf: percentage of right answers for angry facial expressions.
aThe differences are statistically significant (p < .05) between the group with CTQ1 and the one not suffering from it.
bThe differences are statistically significant (p < .05) between the group with CTQ2 and the one not suffering from it.
cThe differences are statistically significant (p < .05) between the group with CTQ3 and the one not suffering from it.
Relationship between the existence of trauma in childhood and the FER adjusted to age, sex, IQ, group to which the subject belongs and substance consumption.
| Variables | dfr_ptot (R2: 9.39%) | ||
|---|---|---|---|
| β Parameter | 95% CI | p | |
| CTQ2 | −3.42 | −6.66 to −.18 | .0388 |
| Group | |||
| Control + BPD | FER. | ||
| FPE | −4.52 | −7.09 to −1.94 | .0006 |
| Aged | −.15 | −.24 to −.06 | .0013 |
| Variables | dfr_pnf (R2: 5.01%) | ||
|---|---|---|---|
| β Parameter | 95% CI | p | |
| Group | |||
| Control | FER. | ||
| FPE | −5.58 | −9.42 to −1.74 | .0045 |
| BPD | −.21 | −11.13 to −3.29 | .0003 |
| Variables | dfr_phf (R2: 2.46%) | ||
|---|---|---|---|
| β Parameter | 95% CI | p | |
| CTQ2 | −4.99 | −8.44 to −1.53 | .0049 |
| Variables | dfr_pff (R2: 3.55%) | ||
|---|---|---|---|
| β Parameter | 95% CI | p | |
| Age | −.31 | −.48 to −.13 | .0007 |
| Variables | dfr_paf (R2: 4.86%) | ||
|---|---|---|---|
| β Parameter | 95% CI | p | |
| Group | |||
| Control + BPD | FER. | ||
| FPE | −8,52 | −14.04 to −3 | .0026 |
| Age | −.22 | −.42 to −.03 | .0246 |
95% CI: 95% confidence incidence; FER.: reference group; dfr_tot: percentage of total right answers; dfr_pnf: percentage of right answers for neutral facial expressions; dfr_phf: percentage of right answers for happy facial expressions; dfr_pff: percentage right answers for fearful facial expressions; dfr_paf: percentage of right answers for angry facial expressions.
The CTQ2 continues to be a fact which is correlated with the recognition of happy faces, so that subjects who have suffered from this type of abuse have the greatest difficulty in recognizing this type of expression. Age impacts facial expression recognition for anger and fear (the higher the age the worse the recognition), whilst belonging to the FPE group meant having greater difficulty in recognizing angry faces.
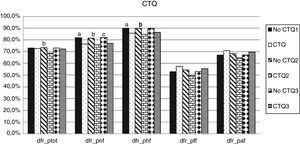
In order to increase statistical power, we combined emotions of anger and fear in the so-called negative valence. With regard to the direction of the most frequent error in FER, we saw that subjects who had suffered from some type of trauma tended to find more faces with negative valence (anger or fear) among the neutral and happy ones, than those who had not had traumatic experiences. Subjects without experiences of emotional abuse perceived neutral expressions more frequently in angry faces, than those who had a history of abuse, although in this case the ES was low (Table 3).
Comparison of attribution error percentage in FER according to type of trauma suffered from. Analysis adjusted and without adjustment.
| CTQ1 (mean, SD) | U Mann Whitney test | CTQ2 (mean, SD) | U Mann Whitney test | CTQ3 (mean, SD) | U Mann Whitney test | ||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | p | Yes | No | p | Yes | No | p | |
| Neutral-happy | 12.5 (12.4) | 11.2 (11.5) | 10.4 (10.1) | 11.6 (11.9) | 12.0 (12.1) | 11.2 (11.5) | |||
| Neutral-negative valence | 4.9 (5.2) | 3.2 (4.1) | p = .006SE = ―.39 | 4.8 (4.2) | 3.4 (4.4) | p = .0078SE = ―.32 | 4.8 (5.1) | 3.2 (4.1) | p = .0032SE = ―.36 |
| Happy-neutral | 7.8 (8.3) | 7.6 (8.4) | 7.1 (7.2) | 7.7 (8.6) | 7.5 (7.9) | 7.7 (8.6) | |||
| Happy –negative valence | 2.2 (3.4) | .9 (2.2) | p < .001SE = ―.52 | 2.2 (3.1) | 1.0 (2.4) | p = .006SE = ―.48 | 2.0 (3.2) | .9 (2.2) | p = .001SE = ―.44 |
| Fear-neutral | 35.8 (17.2) | 38.2 (14.5) | 36.2 (17.2) | 37.9 (14.8) | 36.3 (16.6) | 38.2 (14.6) | |||
| Fear-happy | 1.2 (3.5) | 1.7 (3.6) | 1.8 (3.3) | 1.6 (3.6) | 1.3 (3.3) | 1.7 (3.6) | |||
| Fear-anger | 4.0 (5.7) | 4.7 (6.8) | 3.8 (5.1) | 4.6 (6.8) | 3.8 (5.6) | 4.8 (6.9) | |||
| Anger-neutral | 12. 6 (11.3) | 16.1 (12.9) | p = .046SE = .28 | 12.6 (9.2) | 15.8 (13.0) | 13.1 (10.9) | 16.1 (13.1) | ||
| Anger-happy | 3.2 (5.4) | 2.6 (4.9) | 2.7 (5.3) | 2.7 (4.9) | 2.7 (5.0) | 2.7 (4.9) | |||
| Anger-fear | 8.6 (9.6) | 9.6 (11.0) | 11.2 (10.6) | 9.1 (10.8) | 9.4 (9.9) | 9.4 (11.0) | |||
p = statistical significance; SE = size effect.
Adjusting this ratio to possible variables such as age, sex, IQ, the group to which the subject belongs and current substance consumption, we found a statistically significant relationship between the fact of more frequently attributing negative expressions to neutral faces (CTQ3; R2 = 2.69%; CI 95%: .57-2.79; β = 1.68; p = .0032) and happy (CTQ3; R2 = 6.69%; CI 95%: .36-1.63; β = .99; p = .0022) in subjects who had suffered from some type of trauma.
DiscussionIn our sample, the existence of any type of childhood abuse is associated with a worse rate of FER in adulthood. There is particularly poorer recognition of faces with expressions of happiness and neutral faces. Also, this association remains statistically significant for recognition of happy faces and the rate of total FER regardless of other factors, such as belonging to the study group, when the subjects mentioned a history of physical and/or sexual abuse (CTQ2). Furthermore, the subjects of the sample with some type of childhood abuse most frequently attributed negative expressions to the neutral and happy faces than the subjects without said abuse, regardless of other factors. Lastly, subjects with a history of emotional abuse in childhood recognized happy faces less frequently in angry expression than those subjects without these histories, although these differences were not maintained after adjusting the model through other variables.
The difficulty in recognizing certain facial expressions, particularly in positive expression, has been broadly described in children with a history of childhood abuse.10,29 These alterations also appear to remain in adulthood.16,30 In our sample we clearly saw that subjects with a history of childhood abuse presented with a poorer recognition of facial expressions, and especially with neutral and happy expressions. Probably the fact that they had lived in an environment of abuse and deprivation could have led to fewer opportunities to learn to recognize other emotion of others by using their own sensory motor experiences.10,31 Poor recognition of emotion in abused children may therefore originate in less experience of positive emotions.
Particularly interesting is the bias shown by abused children in favour of expressions of anger in some studies, because these expressions are recognized based on lower sensory and external stimuli11 and fewer expressive clues32 than other negative emotions. This phenomenon is understood as an adaptive form of learning of victims as a reaction to an environment of this type.33 Although in our sample there was better FER of anger in patients who had suffered emotional, physical or sexual abuses (Fig. 2), these differences were not statistically significant. We did find a greater attribution frequency of happy faces to angry faces, although this result loses its significance when we analyzed it together with other variables) and of negative valence faces to neutral and happy ones.
This suggests major confusion in discernment of negative emotions in these subjects.
Given the exploratory nature of this work, no chance conclusions may be drawn from them. It is also obvious that to explain the bias in the FER many other variables would be necessary. However, and given that there appears to be a relationship between emotional process alterations and FER, we may speculate that a traumatic experience in childhood may lead to a vulnerability in the development of an emotional disorder and that this involves an aberrant emotional process coinciding with the beginnings of a mental disorder in adulthood.
Further studies are required so that the interaction between childhood abuse and vulnerability in the development of emotional processing alterations may be understood.
Several hypotheses have been formulated. On the one hand, it could be that the children who have experienced negligence in care during their childhood have experienced an emotionally deprived environment which may have impacted their FER.34 Another possibility is that exposure to the trauma in childhood could have impacted their neurodevelopment in such a way that it subtly changes emotional processes. Some data suggest that an increased activity exists in response to sad faces in depressive patients35 and to negative faces (fear, anger, sadness) in healthy individuals with a history of childhood abuse.36 This change in FER could impact the later development of a mental pathology, since this type of alteration is more frequently seen in clinical population groups (especially in FPE).
We would also mention the Research Domain Criteria (RDoC), focused on the search for dimensional psychological concepts which are relevant to human behaviour and mental disorders, proposing a change in psychiatric classification.37 The idea would be to “develop, for research purposes, new forms of classifying mental disorders based on dimensions of behaviour and observable neurobiological measuresments.”38 A dimensional focus was incorporated in contrast to the standard categorical classification. The process consists in determining a mechanism used for functional behaviour and linking its inappropriate functioning to different clinical problems. At present there are five RDoC domains: negative valence, positive valence, cognitive systems, social processes, systems of activation and regulators. Inside each domain there is a series of constructs. The FER could be included within the construct called social processes (social communication: reception of facial communication ― ability to perceive of an emotional state of someone based on verbal facial non verbal expressions). Our study could provide information to this area of research.
As already mentioned, this study is limited to making a cross-sectional evaluation of the FER, which would prevent any conclusions being reached on causality. A limitation to our study could be that we did not examine the possible effects of psychotropic medication in the FER. Although there are several studies which offer information on the mild effects of psychoactive medication in the FER,39 recent literature does not report on any significant impact of antispychotics40 or antidepressant medication in the FER.41 Furthermore, it is true that patients with BPD often present with other comorbid pathologies which may also affect the FER, a fact that was not analysed in the sample. However, it is also true that, in general, the existence of other psychiatric pathologies in this group is not definitive for making a BPD diagnosis.
One strength could be to highlight that the sample is representative of the environment in which we find ourselves and is proof of the importance of the childhood trauma in the FER regardless of other factors analysed, including the diagnostic group to which the subject belonged. Also, all results obtained are separate from IQ which implies that other cognitive aspects of emotional intelligence are involved in the FER process.
To conclude, the existence of trauma in childhood appears to have a separate influence in the sample subjects’ ability to recognize facial expressions. Since trauma is an avoidable factor and has a specific treatment, attention should be paid to the existence of this background precedent in clinical population groups.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Catalan A, Díaz A, Angosto V, Zamalloa I, Martínez N, Guede D, et al. ¿Influye el trauma infantil en el reconocimiento de las emociones faciales independientemente del diagnóstico de trastorno mental grave? Rev Psiquiatr Salud Ment (Barc.). 2020;13:140–149.