Psycho-COVID: Long-term effects of COVID19 pandemic on brain and mental health
More infoDifferent studies have suggested that psychological, social and economic factors could contribute to an increase in the suicide. That is why the scientific community fear an epidemic of suicides secondary to this crisis. The objective is to evaluate the variables related to suicidal behavior during the two states of alarm and to review if there were sociodemographic or clinical differences with respect to periods prior to the COVID-19 pandemic.
Material and methodsWe compared visits to the emergency room and their characteristics of all patients with suicidal behavior before and after the pandemic in Lérida. Information on sociodemographic status, reason for consultation, diagnosis and characteristics of suicidal behavior was obtained from the electronic medical record.
ResultsNo differences were observed in the percentage of suicidal ideation or attempts in the three periods (p=0.201). The characteristics in the multiple logistic regression associated with suicidal behavior are: being a woman (OR: 1.81 [1.27–2.56]), living with relatives (OR: 1.55 [1.05–2.32]) and have a diagnosis of non-alcohol related substance use disorder (OR: 1.94 [1.09–3.42]). As protective factors, being visited in the emergency room during the second state of alarm (OR: 0.68 [0.48–0.96]) and having depression (OR: 0.67 [0.47–0.96]).
ConclusionsEmergency care for suicidal behavior did not increase during the pandemic and, in fact, in 2020 completed suicides decreased by almost half in the province. Risk factors for suicide attempt were female gender, living with relatives, and having a substance use disorder diagnosis. Instead, depression was a protective factor.
Diferentes estudios han sugerido que factores psicológicos, sociales y económicos podrían aumentar la tasa de suicidio. La comunidad científica teme una epidemia de suicidios secundaria a esta crisis. El objetivo es evaluar las variables relacionadas con la conducta suicida durante los 2 estados de alarma y revisar si hubo diferencias sociodemográficas o clínicas respecto a periodos previos a la pandemia de COVID-19.
Material y métodosComparamos las visitas a urgencias y sus características de todos los pacientes con conducta suicida antes y después de la pandemia en Lérida. La información sobre el estado sociodemográfico, motivo de consulta, diagnóstico y características de la conducta suicida se obtuvieron de la historia clínica electrónica.
ResultadosNo se observaron diferencias en el porcentaje de ideación o intentos suicidas en los 3 períodos (p=0,201). Las características en la regresión logística múltiple asociadas a la conducta suicida son: ser mujer (OR: 1,81 [1,27-2,56]), vivir con familiares (OR: 1,55 [1,05-2,32]) y tener diagnóstico de trastorno por consumo de sustancias no relacionado con el alcohol(OR: 1,94 [1,09-3,42]). Como factores protectores, ser visitado en urgencias durante el segundo estado de alarma (OR: 0,68 [0,48-0,96]) y tener depresión (OR: 0,67 [0,47-0,96]).
ConclusionesLa atención de emergencia por conducta suicida no aumentó durante la pandemia y, de hecho, en 2020 los suicidios consumados disminuyeron casi a la mitad en la provincia. Los factores de riesgo para el intento de suicidio fueron el sexo femenino, vivir con familiares y tener un diagnóstico de trastorno por uso de sustancias. En cambio, la depresión fue un factor protector.
Different studies have suggested that psychological, social and economic factors, such as stress due to fear of infection, depression due to isolation and economic crises, such as declining income and unemployment, could contribute to an increase in the suicide rate.1 In situations of previous infection, such as the Spanish flu outbreak or the severe acute respiratory syndrome outbreak in 2003, mortality due to suicide increased.2 That is why the scientific community and political authorities fear an epidemic of suicides secondary to this crisis3 as has already been shown in Spain with an upturn in the number of suicides in 2020, rising to 3941 suicides compared to 3671 in 2019.4
There are multiple studies carried out on the influence of the COVID-19 pandemic on suicidal behavior. A meta-analysis carried out with data from 54 studies with 308,596 participants stands out. Their results suggested higher rates of suicidal ideation events (10.81%), suicide attempts (4.68%), and self-harm (9.63%) during the COVID-19 pandemic when compared to event rates of pre-pandemic studies. The analysis indicated that younger people, women, and people from democratic countries are more susceptible to suicidal ideation during the COVID-19 pandemic.5 Another review involving 12 studies with 120,076 patients reported a prevalence of suicidal ideation of 12.1% (CI 9.3–15.2). The main risk factors for suicidal ideation were: low social support, high physical and mental exhaustion, and self-reported poorer physical health in frontline medical workers, sleep disturbance, quarantine and exhaustion, loneliness, and mental health problems. Thus, it seems confirmed that the rate of suicidal ideation during the COVID pandemic is higher than that reported in studies on the general population before the pandemic and may result in higher suicide rates in the future.6
Although there are projections about the greater probability of suicide and deaths due to despair due to the COVID-19 pandemic,7 it is necessary to carry out local studies according to the care areas that allow a better identification of the situation and care needs. The objective of this study is to evaluate the variables related to suicidal behavior during the two states of alarm and to review if there were sociodemographic or clinical differences with respect to periods prior to the COVID-19 pandemic.
MethodSample and procedureThis study was carried out at the Santa Maria University Hospital in Lleida, Spain. This hospital is the only one providing urgent psychiatric care in the province of Lerida, with an area of influence of 431,183 people.8
The data in this study were obtained through a retrospective review of digital medical records extracting all the patients visited in the Psychiatric Emergency Department of Santa Maria University Hospital in Lerida. The observation periods were: (1) before confinement: from January 13, 2020, until March 14, 2020; (2) during the confinement of the first state of alarm in Spain: from its start on the 15th of March, 2020 until its conclusion on the 20th of June, 2020; (3) during the second state of alarm in Spain: from October 25, 2020 to May 9, 2021.9
MeasurementsThe following information was collected from digital medical records: number of visits to the emergency unit for psychiatric reasons in the periods described, sociodemographic profile of the patients who attended an emergency unit (gender, date of birth and marital status), psychiatric diagnosis (following the criteria in DSM-IV10), reason for consultation and referral upon discharge. For patients who reported suicide attempts, the following data were also collected: method of suicide attempt, lethality and history of suicidal behaviour. We used Silverman et al.’s definition for attempted suicide: a self-inflicted, potentially injurious behaviour with a nonfatal outcome for which there is evidence (either explicit or implicit) of intent to die.11 Following the criteria of Beautrais et al., suicide attempts that required more than 48h of medical attention in the general hospital were considered highly lethal; moderately lethal if they required between 24 and 48h, and of low lethality if they required less than 24h.
Statistical analysisStatistical analyses were performed using the IBM-SPSS v.23 statistical package. Continuous data were expressed as mean±standard deviation while categorical data were presented as percentages. The normal distribution was evaluated using the Shapiro–Wilk test. Chi-square and t-student tests were used for continuous data. As a non-parametric alternative, Fisher's exact test and the Kruskal–Wallis test were used, as appropriate. Univariate analyses were performed to explore whether sociodemographic and clinical variables were associated with suicidal behaviour. Fisher's exact test (FET) provided the significance and the odds ratios (OR) and their 95% confidence intervals (CI) provided the effect size. The significant variables (p<0.05) in the univariate analyses were included in a stepped bivariate logistic regression model. Type I error was set at the usual value of 5% (alpha=0.05) with a two-sided approximation.
The authors state that all the procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the 1975 Declaration of Helsinki, revised in 2008.12 This study was approved by the ethics and clinical research committee of Arnau de Vilanova University Hospital.
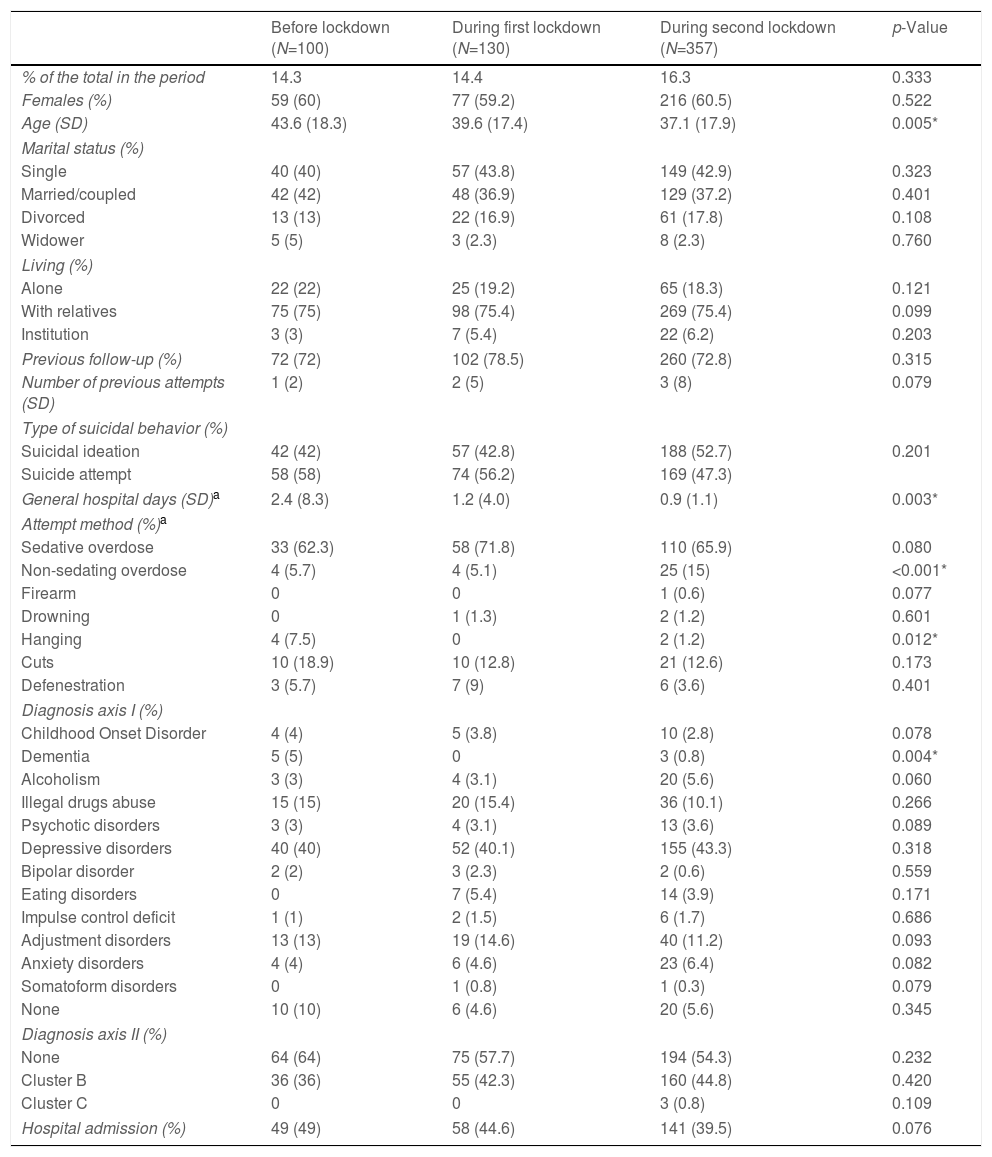
ResultsPatients treated for suicidal behaviorWe recruited 587 patients with suicidal behavior, which represents 15.4% of all psychiatric emergency visits without significant variations in the three periods studied, although their number increased in the second state of alarm (Table 1). No differences were observed in the percentage of suicidal ideation or attempts in the three periods (p=0.201). During the second state of alarm, the patients who attended the emergency room due to suicidal behavior were younger (p=0.005), spent less time in the general hospital due to the lower somatic lethality of the suicide attempt (p=0.003) and regarding the method used in the attempts, an increase in non-sedating drug intakes was observed (p<0.001) and a decrease in hanging in both alarm states. Regarding axis I diagnoses, a reduction was observed in patients with dementias during the two alarm states (p=0.004) without significant variations in the rest of the diagnoses.
Description of patients seen in psychiatric emergencies for suicidal behavior during the three periods studied.
| Before lockdown (N=100) | During first lockdown (N=130) | During second lockdown (N=357) | p-Value | |
|---|---|---|---|---|
| % of the total in the period | 14.3 | 14.4 | 16.3 | 0.333 |
| Females (%) | 59 (60) | 77 (59.2) | 216 (60.5) | 0.522 |
| Age (SD) | 43.6 (18.3) | 39.6 (17.4) | 37.1 (17.9) | 0.005* |
| Marital status (%) | ||||
| Single | 40 (40) | 57 (43.8) | 149 (42.9) | 0.323 |
| Married/coupled | 42 (42) | 48 (36.9) | 129 (37.2) | 0.401 |
| Divorced | 13 (13) | 22 (16.9) | 61 (17.8) | 0.108 |
| Widower | 5 (5) | 3 (2.3) | 8 (2.3) | 0.760 |
| Living (%) | ||||
| Alone | 22 (22) | 25 (19.2) | 65 (18.3) | 0.121 |
| With relatives | 75 (75) | 98 (75.4) | 269 (75.4) | 0.099 |
| Institution | 3 (3) | 7 (5.4) | 22 (6.2) | 0.203 |
| Previous follow-up (%) | 72 (72) | 102 (78.5) | 260 (72.8) | 0.315 |
| Number of previous attempts (SD) | 1 (2) | 2 (5) | 3 (8) | 0.079 |
| Type of suicidal behavior (%) | ||||
| Suicidal ideation | 42 (42) | 57 (42.8) | 188 (52.7) | 0.201 |
| Suicide attempt | 58 (58) | 74 (56.2) | 169 (47.3) | |
| General hospital days (SD)a | 2.4 (8.3) | 1.2 (4.0) | 0.9 (1.1) | 0.003* |
| Attempt method (%)a | ||||
| Sedative overdose | 33 (62.3) | 58 (71.8) | 110 (65.9) | 0.080 |
| Non-sedating overdose | 4 (5.7) | 4 (5.1) | 25 (15) | <0.001* |
| Firearm | 0 | 0 | 1 (0.6) | 0.077 |
| Drowning | 0 | 1 (1.3) | 2 (1.2) | 0.601 |
| Hanging | 4 (7.5) | 0 | 2 (1.2) | 0.012* |
| Cuts | 10 (18.9) | 10 (12.8) | 21 (12.6) | 0.173 |
| Defenestration | 3 (5.7) | 7 (9) | 6 (3.6) | 0.401 |
| Diagnosis axis I (%) | ||||
| Childhood Onset Disorder | 4 (4) | 5 (3.8) | 10 (2.8) | 0.078 |
| Dementia | 5 (5) | 0 | 3 (0.8) | 0.004* |
| Alcoholism | 3 (3) | 4 (3.1) | 20 (5.6) | 0.060 |
| Illegal drugs abuse | 15 (15) | 20 (15.4) | 36 (10.1) | 0.266 |
| Psychotic disorders | 3 (3) | 4 (3.1) | 13 (3.6) | 0.089 |
| Depressive disorders | 40 (40) | 52 (40.1) | 155 (43.3) | 0.318 |
| Bipolar disorder | 2 (2) | 3 (2.3) | 2 (0.6) | 0.559 |
| Eating disorders | 0 | 7 (5.4) | 14 (3.9) | 0.171 |
| Impulse control deficit | 1 (1) | 2 (1.5) | 6 (1.7) | 0.686 |
| Adjustment disorders | 13 (13) | 19 (14.6) | 40 (11.2) | 0.093 |
| Anxiety disorders | 4 (4) | 6 (4.6) | 23 (6.4) | 0.082 |
| Somatoform disorders | 0 | 1 (0.8) | 1 (0.3) | 0.079 |
| None | 10 (10) | 6 (4.6) | 20 (5.6) | 0.345 |
| Diagnosis axis II (%) | ||||
| None | 64 (64) | 75 (57.7) | 194 (54.3) | 0.232 |
| Cluster B | 36 (36) | 55 (42.3) | 160 (44.8) | 0.420 |
| Cluster C | 0 | 0 | 3 (0.8) | 0.109 |
| Hospital admission (%) | 49 (49) | 58 (44.6) | 141 (39.5) | 0.076 |
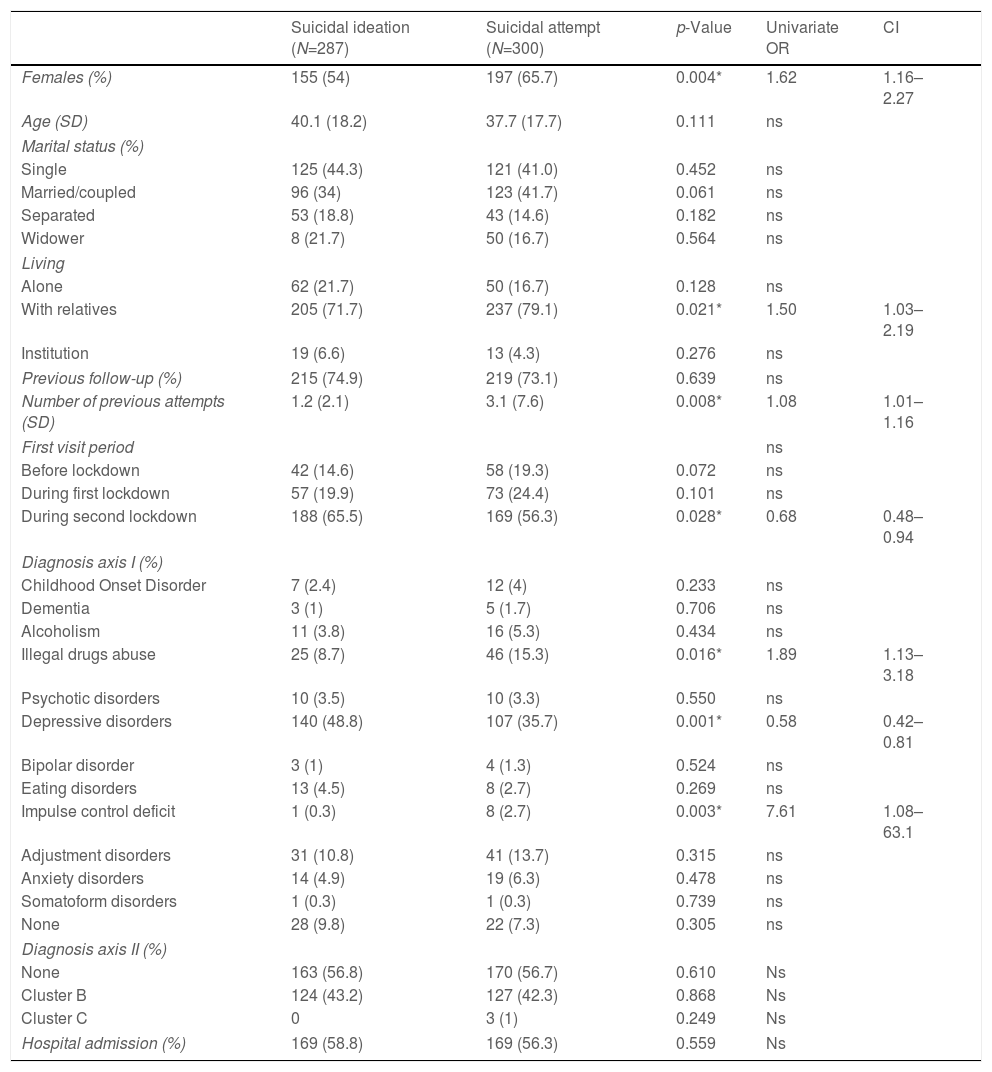
Of all patients with suicidal behavior, 287 (49.9%) presented suicidal ideation and 300 (51.1%) attended after making a suicide attempt (Table 2). When comparing both groups, we found that in the group of patients who had made a suicide attempt there was a higher percentage of women (p=0.004), a higher percentage of patients who lived with relatives (p=0.021), the patients had made more attempts (p=0.008) and had more diagnoses of Non-Alcohol Substance Use Disorder (p=0.016) and Impulse Control Disorder (p=0.003). On the contrary, in this group the patients had been visited less frequently during the second alarm state (p=0.028) and presented less diagnosis of the depressive spectrum. The other variables did not show significant differences between both groups.
Bivariate and multivariate logistic regression of patients who consulted for suicidal behavior.
| Suicidal ideation (N=287) | Suicidal attempt (N=300) | p-Value | Univariate OR | CI | |
|---|---|---|---|---|---|
| Females (%) | 155 (54) | 197 (65.7) | 0.004* | 1.62 | 1.16–2.27 |
| Age (SD) | 40.1 (18.2) | 37.7 (17.7) | 0.111 | ns | |
| Marital status (%) | |||||
| Single | 125 (44.3) | 121 (41.0) | 0.452 | ns | |
| Married/coupled | 96 (34) | 123 (41.7) | 0.061 | ns | |
| Separated | 53 (18.8) | 43 (14.6) | 0.182 | ns | |
| Widower | 8 (21.7) | 50 (16.7) | 0.564 | ns | |
| Living | |||||
| Alone | 62 (21.7) | 50 (16.7) | 0.128 | ns | |
| With relatives | 205 (71.7) | 237 (79.1) | 0.021* | 1.50 | 1.03–2.19 |
| Institution | 19 (6.6) | 13 (4.3) | 0.276 | ns | |
| Previous follow-up (%) | 215 (74.9) | 219 (73.1) | 0.639 | ns | |
| Number of previous attempts (SD) | 1.2 (2.1) | 3.1 (7.6) | 0.008* | 1.08 | 1.01–1.16 |
| First visit period | ns | ||||
| Before lockdown | 42 (14.6) | 58 (19.3) | 0.072 | ns | |
| During first lockdown | 57 (19.9) | 73 (24.4) | 0.101 | ns | |
| During second lockdown | 188 (65.5) | 169 (56.3) | 0.028* | 0.68 | 0.48–0.94 |
| Diagnosis axis I (%) | |||||
| Childhood Onset Disorder | 7 (2.4) | 12 (4) | 0.233 | ns | |
| Dementia | 3 (1) | 5 (1.7) | 0.706 | ns | |
| Alcoholism | 11 (3.8) | 16 (5.3) | 0.434 | ns | |
| Illegal drugs abuse | 25 (8.7) | 46 (15.3) | 0.016* | 1.89 | 1.13–3.18 |
| Psychotic disorders | 10 (3.5) | 10 (3.3) | 0.550 | ns | |
| Depressive disorders | 140 (48.8) | 107 (35.7) | 0.001* | 0.58 | 0.42–0.81 |
| Bipolar disorder | 3 (1) | 4 (1.3) | 0.524 | ns | |
| Eating disorders | 13 (4.5) | 8 (2.7) | 0.269 | ns | |
| Impulse control deficit | 1 (0.3) | 8 (2.7) | 0.003* | 7.61 | 1.08–63.1 |
| Adjustment disorders | 31 (10.8) | 41 (13.7) | 0.315 | ns | |
| Anxiety disorders | 14 (4.9) | 19 (6.3) | 0.478 | ns | |
| Somatoform disorders | 1 (0.3) | 1 (0.3) | 0.739 | ns | |
| None | 28 (9.8) | 22 (7.3) | 0.305 | ns | |
| Diagnosis axis II (%) | |||||
| None | 163 (56.8) | 170 (56.7) | 0.610 | Ns | |
| Cluster B | 124 (43.2) | 127 (42.3) | 0.868 | Ns | |
| Cluster C | 0 | 3 (1) | 0.249 | Ns | |
| Hospital admission (%) | 169 (58.8) | 169 (56.3) | 0.559 | Ns | |
| Multivariate logistic regression model | |||||
|---|---|---|---|---|---|
| Variable | Wald X2a | p-Value | OR corrected | CI | |
| First step | Female | 11.15 | 0.001* | 1.81 | 1.27–2.56 |
| Living with relatives | 5.04 | 0.025* | 1.55 | 1.05–2.32 | |
| Number of previous attempts | 3.65 | 0.056 | 1.07 | 0.98–1.14 | |
| Visit during second state of alarm | 4.68 | 0.030* | 0.68 | 0.48–0.96 | |
| Illegal drugs abuse | 5.17 | 0.023* | 1.94 | 1.09–3.42 | |
| Depressive disorders | 4.73 | 0.030* | 0.67 | 0.47–0.96 | |
| Impulse control deficit | 3.69 | 0.053 | 7.89 | 0.98–64.94 | |
In bivariate logistic regression, the following variables were associated with suicide attempt: being female, living with relatives, the number of previous attempts, being visited in the second state of alarm, having a diagnosis of substance use disorder not related to alcohol, a diagnosis of affective disorder, and a diagnosis of impulse control disorder. When analyzing the characteristics in the multiple logistic regression, being a woman (OR: 1.81 [1.27–2.56]), living with relatives (OR: 1.55 [1.05–2.32]) and having a diagnosis of suicide remain as risk factors for suicide attempt. non-alcohol related substance use disorder (OR: 1.94 [1.09–3.42]); As protective factors, being visited in the emergency room during the second state of alarm (OR: 0.68 [0.48–0.96]) and having a diagnosis of depression (OR: 0.67 [0.47–0.96]) are maintained. Although having a diagnosis of Impulse Control Disorder was the greatest risk factor for suicide attempt individually (OR: 7.61 [1.08–63.1]), when adjusting the model with the rest of the variables, this characteristic loses statistical significance.
DiscussionIn this sample, unlike other studies that warned of an increase in suicidal behavior,13 we did not find a significant increase in emergency care for suicidal behavior compared to the situation prior to the pandemic. Some studies considering only 2020 reported no difference or reduced emergency department attendances for suicidal behaviour.14 Relative to a similar period in 2019, the number of emergency department attendances for suicide attempts remained stable among American youngs during summer 2020 and winter 2021.15 And lose to our territory under study, a recent study that reviewed suicidal behavior attended to and included in the Barcelona Suicide Risk Code (CRS) platform revealed a 43.20% increase in the monthly incidence of suicidal ideation and suicide attempts during the pandemic compared to the period 2018–2019, reaching a maximum increase of 573.8% in young people under 18 years of age in the month of May 2021.16 It also highlights that, in our province of study, Lérida, there was no increase in suicides compared to the previous year, since that in 2020, 24 suicides were reported and in 2019, 41 deaths were recorded. In the autonomous community of Catalonia, on the other hand, there was an increase in deaths by suicide since 556 people committed suicide in 2020 while in 2019 there were 535 deaths by suicide.4
In this sense, a study that analyzed visits to the emergency room or hospitalizations for suicidal behavior of 1,690,733 adolescents and young adults is relevant, where they showed that a 15-month period of the COVID-19 pandemic was associated with a relative decrease of self-harm or overdose.17 But this information must be interpreted with caution, since preliminary reports on suicide mortality at the beginning of the pandemic indicated that suicide rates would not increase (Massachusetts, USA; Victoria, Australia; England) or would decrease (Japan, Norway) in the first months of the pandemic.13 In Austria, for example, during the first 6 months of the pandemic, there was a relative decrease in suicide among all adults.18 Nevertheless, it must be reiterated that some fatal or non-fatal cases of self-harm or overdose may have been missed due to failure to attend an emergency room, or incomplete recording of any of them as a fatality.17 Any change in suicide risk associated with covid-19 is likely to be dynamic. The 20% decline in Japan at the beginning of the pandemic appeared to reverse in August, when an increase of 7.7%19 was reported. Evidence from previous epidemics suggests that a short-term decline in suicide may initially occur.20
In our work, there are three risk factors associated with suicidal behavior after carrying out logistic regression: female sex, living with relatives and presenting a substance use disorder.
Our results are consistent with others that have already reported more suicide attempts in women, such as a study conducted in Asia in which the number and proportion of emergency care related to suicide attempts increased in 2020 compared to the previous 2 years, especially among women and people from 25 to 49 years old.21
Regarding the nucleus of coexistence, it is surprising that the aspect of living with relatives was a suicidal risk factor since loneliness has been described in multiple works as a high suicidal risk factor.22-24 In fact, a group of French researchers highlighted the need for specific strategies to address loneliness, as well as improve access to care, including telepsychiatry to prevent depression and suicide.25 Specifically, a study carried out in New Zealand reported that living with relatives during confinement was a source of hope for individuals.26
We observed an increased risk of suicide in patients with a history of substance use disorder. It should be noted that up to 40% of patients with substance dependence report a history of previous suicide attempts27 and that this diagnosis has been associated with greater recidivism in suicidal behavior.28
Although not significant in our multivariate logistic regression model, prior suicide attempts were associated with suicidal behavior during the pandemic. The literature that identifies previous suicidal behavior as a high risk factor for subsequent recidivism is robust29,30 which is why secondary prevention has been described as essential in this risk group.31 In terms of suicide attempts lethality, we observed a decrease of general hospital days in the second state of alarm, indicating a decrease of lethality in this period. These results are not supported by previous literature in the acute phase of the pandemic describing low-recue suicide attempts and therefore with greater potential somatic lethality. Moreover, these results also contrast with those observed in more chronic phases of the pandemic1: a recent French study on hospitalizations for suicide in the country revealed that the severity and use of violent methods increased during the second and third quarters of 2020 compared to 2019 and 2018, and this was more evident in those under 60 years of age.32
Paradoxically, in our sample the diagnosis of depression turned out to be protective for suicide attempt. This fact is controversial since classically 10–15% of people with a major depressive disorder commit suicide, and between 60 and 70% of suicide victims suffered a depressive episode.33 This finding of ours is not consistent with the literature, since several studies report that there was a general worsening of mental health throughout the confinement, with prevalence estimates ranging between 9 and 46% among those who report data on symptoms. depressive34,35 and some studies indicate factors such as hopelessness and depression as aspects closely related to suicide attempts during the pandemic.36
Finally, in our study we observed that hospital admissions for suicidal behavior decreased during the pandemic, especially in the second state of alarm. These findings, although not significant, are consistent with the results from France, which indicate that hospital admissions for suicide decreased during the pandemic.32
Strengths and limitationsThese results must be interpreted with some limitations in mind. First, the data presented here come from the digital medical records and, we have relied on the clinical diagnosis made by different psychiatrists. However, as this is a single-center study, there is a common clinical criterion among all psychiatrists working in our emergency department supporting internal validity of the results. Second, we did not employ validated symptom severity measures but lethality measured in hours of medical attention in the general hospital and hospital admission was used as a logical measure of illness severity. This real-world measure increases the clinical transferability of our results, but they may be affected by hospital logistics during the pandemic. Third, this sample is representative of a population seeking secondary care services and results may not be generalizable to patients seeking primary care services. Finally, this is a cross-sectional study based on a single center emergency department and causal inference cannot be made. Therefore, prospective studies would be interesting.
As a strength of the study, we have been able to obtain a sample that represents all the psychiatric emergencies dealt with in the province, related to suicide behaviour, during the two states of alarm. In addition, having data on deaths by suicide in 2020 allows for a broader perspective of suicidal behavior in the territory.
ConclusionsIn our study, we did not observe an increase in emergency care for suicidal behavior during the pandemic and, in fact, in 2020, completed suicides decreased by almost half in our province. Risk factors for suicide attempt were female gender, living with relatives, and having a diagnosis of substance use disorder. Instead, it was a protective factor to have depression.
Conflict of interestAll authors declare that they have no conflict of interest in relation to the performance of this work.