Since the first case descriptions of “dementia praecox” (Diem, 1903), the diagnosis of simple schizophrenia has continued to be controversial. The questioning of its descriptive validity and its reliability, as well as its infrequent use, has led to it being eliminated as a sub-type of schizophrenia in the DSM-III. Criteria for the diagnosis of “simple deteriorative disorder” are currently included in the DSM-IV-TR as a disorder requiring more studies for its possible inclusion.
ObjectivesAn attempt is made, using a clinical case, to perform a historical review of the concept of simple schizophrenia, and at the same what has led to the reflection on the possible reasons for the controversy, and a potential route to resolve it.
MethodologyUsing a controversial clinical case, which meets ICD-10 clinical criteria for simple schizophrenia (and those of the DSM-IV-TR for the simple deteriorative disorder), we reflect on the symptoms and diagnostic difficulties. A literature review and update on the subjects were also performed.
DiscussionOur patient highlights, by the absence in the clinical picture of the most obvious positive psychotic symptoms, the tendency by psychiatrists to identify the diagnosis of schizophrenia with the presence of the same, at least at some time during its evolution. The use of neuroimaging tests was useful to assess the level of deterioration and prognosis of the patient.
ConclusionsConsidering simple schizophrenia in the differential diagnosis of other chronic deteriorative disorders could increase its recognition in the initial phases. The use of neuropsychological function tests, and looking for typical deteriorative patterns of the schizophrenia spectrum, could help to increase the reliability of the diagnosis.
Desde las primeras descripciones de casos de formas simples de “dementia praecox” (Diem, 1903), el diagnóstico de esquizofrenia simple no ha dejado de verse envuelto en controversias. El cuestionamiento sobre su validez descriptiva y fiabilidad, así como su uso infrecuente, llevó a su eliminación como subtipo de esquizofrenia en el DSM-III. En la actualidad se incluyen en el DSM-IV-TR criterios para el diagnóstico del “trastorno deteriorante simple”, como trastorno que requiere de más estudios para su posible inclusión.
ObjetivosSe pretende, a partir de un caso clínico ilustrativo, realizar un repaso histórico del concepto de esquizofrenia simple, a la vez que motivar la reflexión sobre los posibles motivos de controversia en torno al mismo y potencial camino para su resolución.
MetodologíaPartiendo de un caso clínico controvertido, el cual cumple los criterios diagnósticos CIE-10 para esquizofrenia simple (y los del DSM-IV-TR para el trastorno deteriorante simple), reflexionamos sobre la sintomatología y las dificultades diagnósticas. Se realiza una revisión y actualización bibliográfica sobre el tema.
DiscusiónNuestra paciente destaca por la ausencia en el cuadro clínico de los más llamativos síntomas psicóticos positivos, y la tendencia por parte de los psiquiatras a identificar el diagnóstico de esquizofrenia con la presencia de los mismos, al menos en algún momento de la evolución. La utilización de pruebas de neuroimagen, fue de utilidad para evaluar el grado de deterioro y pronóstico de la paciente.
ConclusionesLa consideración de la esquizofrenia simple en el diagnóstico diferencial de otros trastornos deteriorantes crónicos podría incrementar su reconocimiento en las fases iniciales. La utilización de pruebas funcionales neuropsicológicas, buscando patrones de deterioro típicos del espectro esquizofrénico, podría ayudar a aumentar la fiabilidad del diagnóstico.
Diem (1903) described the first few cases of simple forms of dementia praecox, whose development included the insidious erosion of intelligence and affect, but without the positive symptoms involved in psychosis itself. From the time of these first cases, the diagnosis of simple schizophrenia has not been free from controversy. This is perhaps partially due to the fact that the existence and definition of this form of schizophrenia have been anchored more to theoretical developments on the schizophrenic defect than to empirical reality.1
Both Bleuler (1911) and, later on, Kraepelin identified it as one of the subtypes of schizophrenia.2
Bleuler divided schizophrenic symptoms into essential and accessory, including among the first group autism, ambivalence, alogia and affect alterations. He suggested that these essential symptoms were basic and common to all schizophrenic disorders and that the accessory symptoms (hallucinations, delirium and catatonia) were more dramatic but less important.2
The psychiatric classification systems included simple schizophrenia as a diagnostic category: in the International Classification of Diseases (ICD-6) in 1948 and in the DSM-I in 1952. However, the definitions describe a disorder with imprecise limits and confusing symptomology.3
In 1936, Lewis3 criticised the heterogeneity of the syndrome, which invalidated any research on it. A review published by Stone et al.4 in 1968 pointed out that, since 1930, there had only been 1 significant article on the syndrome. They also analysed the diagnosed cases of simple schizophrenia at a state hospital, finding that the diagnosis had rarely been used (only 0.04–0.24% of the cases). This represented 4.5% of all the patients who had been diagnosed with schizophrenia. This last figure is similar to those found in other epidemiological studies: 5.1% by Kant in 1948,5 3.9–9.7% by Morrison in 1974, 3.8% by Carpenter in 1976, 8.2% by Dworkin in 19926 and 3.9% by Kendler in 1994.7 In Stone's opinion, the existing criteria were vague and contradictory, with poor clinical evidence on the existence of the disorder, which could sometimes be assimilated into other diagnoses such as severe personality disorder or chronic schizophrenia. The fruit of their analysis was that the diagnosis should be discarded.4
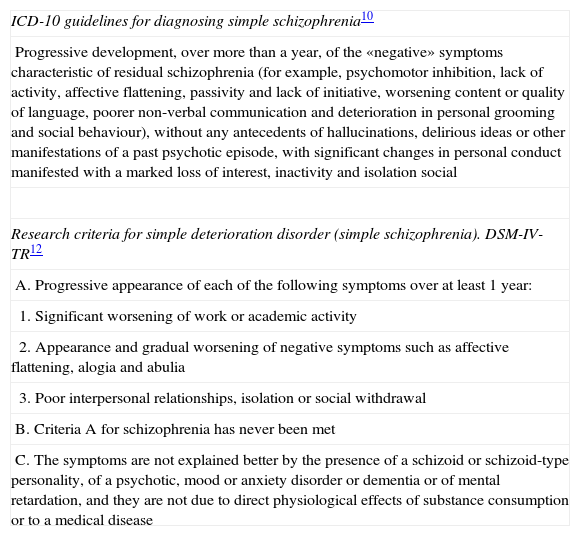
In a desire to standardise psychiatric diagnoses, the DSM-III proposed homogenising the population of patients affected by schizophrenia, among other tasks. It was decided to restrict the concept of this illness to a disorder in which delirium, hallucinations or marked formal disorders of thought had appeared. These are symptoms that clearly conflict with normality and that are easy to identify. Bleuler's essential symptoms–wide and imprecise–which were initially considered as the bedrock of the illness, were rejected as its definitions.3 Questioning the descriptive validity and reliability of the illness, as well as its infrequent use, led to its elimination as a subtype of schizophrenia in the DSM-III (1980).8 What Bleuler9 might have considered, at least theoretically, as the purest form of presentation of schizophrenia was left outside of the diagnostic classification. Meanwhile, it was still being used in other diagnostic systems like the ICD-6 and its later versions. The ICD-10 included it as 1 more subtype of schizophrenia (Table 1).10
ICD-10 guidelines for diagnosing simple schizophrenia.
| ICD-10 guidelines for diagnosing simple schizophrenia10 |
| Progressive development, over more than a year, of the «negative» symptoms characteristic of residual schizophrenia (for example, psychomotor inhibition, lack of activity, affective flattening, passivity and lack of initiative, worsening content or quality of language, poorer non-verbal communication and deterioration in personal grooming and social behaviour), without any antecedents of hallucinations, delirious ideas or other manifestations of a past psychotic episode, with significant changes in personal conduct manifested with a marked loss of interest, inactivity and isolation social |
| Research criteria for simple deterioration disorder (simple schizophrenia). DSM-IV-TR12 |
| A. Progressive appearance of each of the following symptoms over at least 1 year: |
| 1. Significant worsening of work or academic activity |
| 2. Appearance and gradual worsening of negative symptoms such as affective flattening, alogia and abulia |
| 3. Poor interpersonal relationships, isolation or social withdrawal |
| B. Criteria A for schizophrenia has never been met |
| C. The symptoms are not explained better by the presence of a schizoid or schizoid-type personality, of a psychotic, mood or anxiety disorder or dementia or of mental retardation, and they are not due to direct physiological effects of substance consumption or to a medical disease |
While the DSM-IV was being prepared, interest arose in reconsidering the concept of simple schizophrenia: the original view of the syndrome as a non-psychotic illness, with deterioration and accompanied by characteristics indicative of unusual affect, speech or thinking did not fit into any DSM-III-R diagnosis. There were also the historical precedents, the genetic links of these groups of symptoms with other schizophrenia subtypes and the clinical similarities with them to consider.3,7 Patients with simple schizophrenia, diagnosed according the criteria described by Bleuler, presented clinical pictures similar to other more typical forms of schizophrenia in terms of onset age, premorbid social adjustment and negative psychotic symptoms.6 With respect to development, the degrees of functioning of the different schizophrenia subtypes seem to be indistinguishable, as well as their degrees of negative symptoms. However, simple schizophrenia tends to become more chronic (even worse that that of other classic subtypes of schizophrenia),11 which is not surprising considering the greater tendency to negative symptom stability.7 The DSM-IV-TR presently includes criteria for the diagnosis of «simple deteriorative disorder» as a disorder that requires additional studies for its possible inclusion.12 Criticism of the syndrome has arisen from its changeable, unclear definition, its infrequent use as a diagnosis in clinical populations, its lack of reliability and its uncertain descriptive validity. Consequently, these factors needed to be assessed before including it definitively in the diagnostic manual.13 Recent studies, applying multivariate statistical techniques for degree of association analysis, seem to validate simple schizophrenia as a pure clinical subtype within the schizophrenic disorders14 or, if it is not pure, we have a spectrum of subtle differences that range from schizoid reaction (still within the limits of health) to schizophrenic psychosis.
The objectives of this article were: (a) demonstrating, through a clinical case, the current «obscurity» in the use of the diagnosis of simple schizophrenia simple, with the consequent risk of inducing an underdiagnosis that strengthens a feedback loop even more and leading to its disappearance as a clinical entity, and (b) emphasising the importance of early diagnosis to steer these patients towards the appropriate resources and thereby attenuate the deterioration produced by schizophrenic-type processes. We also wanted to highlight the possible use of complementary neuroimaging as anchorage for scant reliability and validity as a clinical entity.
MethodologyAs a basis for our search of the literature, we took a controversial clinical case that met the ICD-10 diagnostic criteria for simple schizophrenia (and those of the DSM-IV-TR for the simple deteriorative disorder). We performed a bibliographical review of articles published on the subject and attempted to consider the symptomatology of the clinical picture and the diagnostic difficulties.
Bibliographical reviewWe introduced the terms «simple schizophrenia» and «simple deteriorative disorder» in the bases PubMed, EMBASE and Índice Médico Español databases and selected all the articles published in English or Spanish up to the end of October 2010 that made explicit reference to this subtype of schizophrenia in their titles. We also reviewed the abstracts of articles that referred to classifying this illness into subtypes, including them in our review if they mentioned the object of our interest. Searching the Cochrane database for articles on simple schizophrenia did not produce any results. Finally, we reviewed the references used in the articles that we considered most relevant, in case we found other articles that met our search criteria.
It was noteworthy that a few more than 26 articles were written in languages other than English or Spanish (18 were Polish or Russian and published before 1988). Initially, we selected 36 articles in all. Of these, 7 were letters to the editor, 1 was a poster presented at a congress, 4 more articles referred to a single clinical case and another 3 contained reflections on the validity of the diagnosis. For our study, we finally used 23 of these articles. The others, up to a total of 36, are indicated in the references31–43 for possible consultation. In short, there are still very few studies on a diagnosis that has been the subject of controversy for so many years.
Clinical caseWe present the case of a 36-year-old single woman, who was admitted to our short-term unit for behavioural problems in the family environment.
A twin to another sister, our case showed good psychomotor development at birth and good language development later on. When she was 3 years old, her father (a 31-year-old army chemical bomb removal expert) took his life by throwing himself under a train. Many details of that period are unknown, but he was admitted to a Madrid hospital and diagnosed with a process of paranoid schizophrenia.
Her mother remembers that when our patient was 7, she would just «go blank» and needed to be calmed down. She had a tonsillectomy at the age of 10. When she was 13, she presented somatic symptomatology of the «dull» head type, minor depressive symptomatology and ideas of death. At that time, the family thought that someone had «put the evil eye on her». The patient and her sister lived without normal rules during this period, while their mother worked as the manager of a gunpowder workshop.
Encouraged by her daughters, the mother went to a marriage agency to find a partner; she met a music teacher and they established a relationship. When the patient was 18, the family moved to Melilla because her stepfather found work in there.
From the time she was 18 until she was 24, she studied music and teaching. She reached the 7th year of piano studies but did not finish her teaching diploma. At that time, she also took accordion classes. The patient had secondary hypoacusis from drugs (she had a history of allergy, or intolerance, to aminoglycosides, diuretics, salicylates, arsenicals, various excipients and lactose). She had right ear surgery at the age of 23 (she currently has an endocochlear prosthesis).
In the patient's opinion, that time of life was turbulent, not only because both sisters were adolescents, but also because of her stepfather's epilepsy problems, her frequent several-day escapes from the house, her compulsive gambling and the multiple rules that she had never had before and that she broke constantly. She remembers her first boyfriends with Moslem men and her first sexual relations, which ended up with her sister's pregnancy and abortion at the age of 24.
Her sister passed a civil exam for schoolteacher and moved to the peninsula, leaving the patient alone with her mother and stepfather. That is when she began to present fainting spells and bulimic behaviour and had her first contact with mental health services, at the age of 25, with a diagnosis of anxiety-depression disorder. In the clinical picture, phobias, fears in general and insomnia stood out.
She began to work with her mother in a centre for immigrants, while the mother's relationship with her stepfather began to deteriorate. At the age of approximately 30, «tired of seeing her mother cry», she went to live with her sister in Almería. Her twin sister is currently married and has a 16-year-old son in treatment with neuroleptics for «manias» and behavioural alterations.
The year after that, the patient had a psychiatric relapse again. She began a pilgrimage of visits to psychiatric physicians from Madrid to Navarra, with different pharmacological formulas that did not work well for her. She came to our region and her mother came along to take care of her.
During these last 6 years, she was admitted many times to different acute psychiatric units, as well as to the Medium Stay Unit at our hospital in 2008. She received multiple pharmacological treatments (neuroleptics, antidepressants and lithium carbonate), which were poorly tolerated, as well as electroconvulsive therapy (ECT) twice, with a very poor response. Under follow-up care in mental health centres, she received many diagnoses: anxiety disorder, psychotic depression, dependent personality disorder, affective paraphrenia, schizoaffective disorder, schizophreniform disorder, etc. and simple schizophrenia more recently.
Her relationship with her mother during the last few years has been one of total exploitation and dependence, making the mother leave her partner continuously to take care of her. She has not worked for years and has had few social relationships. She receives a non-contributing disability pension for hypoacusis and is under partial guardianship, with her mother as the guardian.
At present, her psychopathological situation is stable, with trifluoperazine at low doses, and she goes to an association for family members of mentally ill individuals. She also has hypothyroidism and scalp psoriasis. She has no toxic habits. In general, she has always tended to abandon all the rehabilitation resources proposed. She gives a superficial impression of a clinical picture that is not very serious, which does not correspond with her development or with her true functioning, which is very poor. It is notable that she is incapable of handling simple day-to-day activities, such as catch a bus, go to the supermarket and keep an eye on household affairs.
During the psychopathological examinations in the various admissions to our centre, the patient was always conscious and oriented, approachable and collaborative. Her speech was coherent, appropriate and lucid, but evolving through the successive hospital interventions towards ideative impoverishment, perseverance and childishness. No sensory-perceptual alterations or delirium-related ideas were seen. The patient did express, on numerous occasions, overestimated ideas of guilt for her clinical state, hypochondriacal fears about the somatic anxiety symptoms and ideas of death as a possible escape.
Sometimes displaying hypothymic affects and predominantly anxious at other times, the patient frequently complained of motor inhibition, lifelessness and difficulty in concentrating. The affect symptomatology did not present a circadian rhythm. In the last few months, her affect on contact has sometimes been inappropriate, flat, distant and slightly hostile. Although the patient tends towards overweight, she has no alterations in eating behaviour. She does report problems with insomnia, sometimes with early waking and others with difficulties falling asleep.
In some of the admissions, depressive symptomatology has been the most notable. However, this never reached the point of constituting a complete major depressive order. Together with the poor psychopathology displayed on some occasions, what stands out is a great dysfunctionality in several areas of life: professional, interpersonal, love relationships and intimate. The patient abandons all social relationships outside a reduced family circle progressively and has shown herself to be incapable of keeping a job. She maintains an apathetic and non-motivated attitude. The generalised functioning is very poor and very deficient, with predominating somatic symptoms.
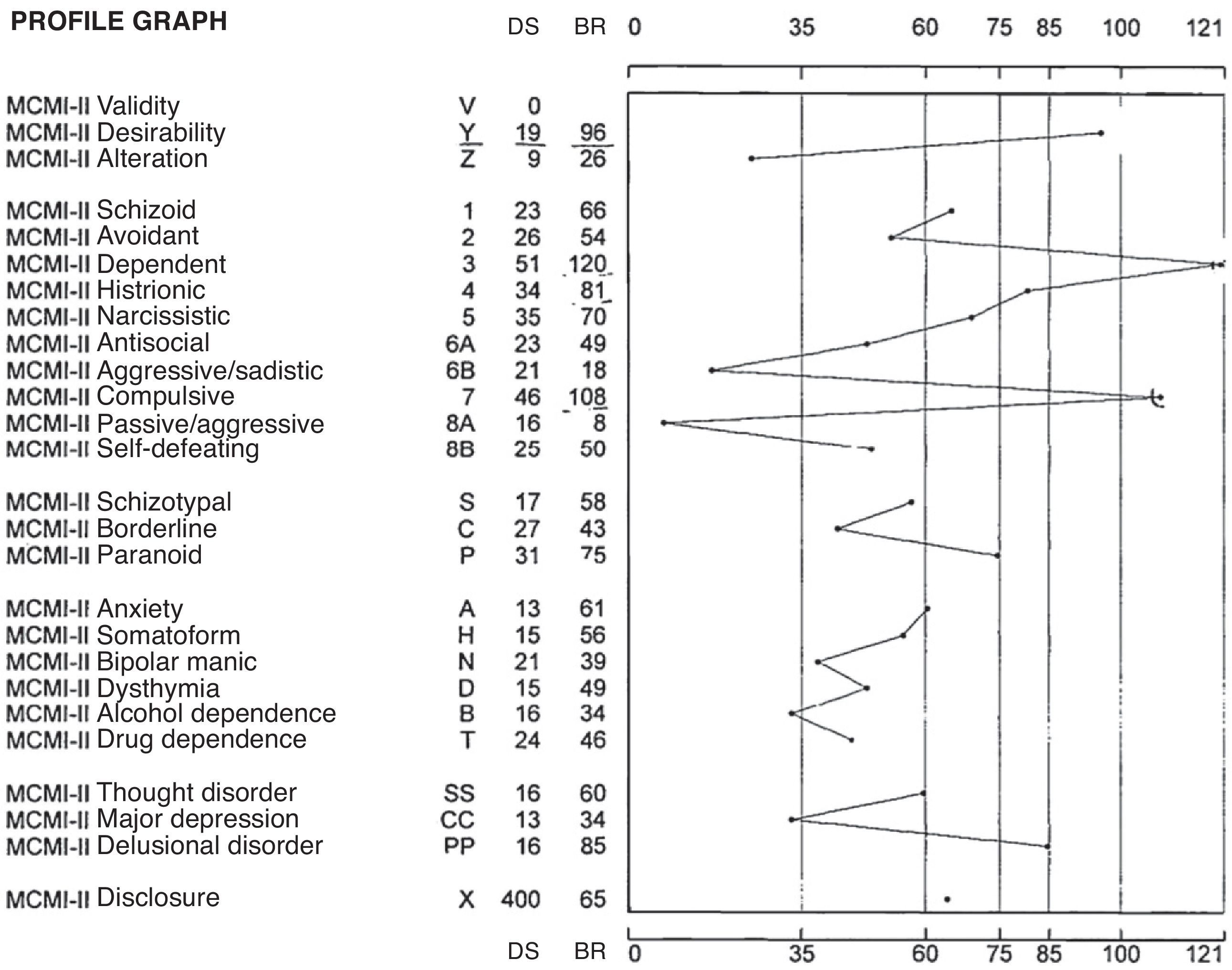
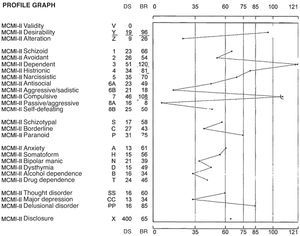
Tests had been given the patient in the past to reach a clearer differential diagnosis, given that the clinical picture was atypical. Among these was the Millon Clinical Multiaxial Inventory-II (Fig. 1).
In the modifying and correcting indexes, she obtained a high score in desirability, which indicated the patient's tendency to present a good image. In the basic personality scales, her highest scores were in the dependent, compulsive and histrionic profile. This profile describes individuals who are orderly and disciplined, with low self-esteem. They are generally friendly and conciliatory, tending to establish strong emotional ties to obtain the support that they need by being complacent. The lack of initiative and autonomy in this personality often stems from parental overprotection. These individuals have generally learned the comfortable posture of adopting a passive role in interpersonal relationships.
In pathological personality scales, the patient obtained an elevated score in paranoid. These individuals show a watchful distrust of other people and a nervously anticipated defence against deception and criticism.
In severe syndromes, the patient obtained a high score in psychotic delirium. This indicated to us that there could be signs of thinking disorders and ideas of reference.
At a later time, the MMPI personality test was administered. It showed only a slightly high score on the anxiety scale, border-line scores on the unusually thoughts and perceptions scales and on the aggressive components. However, viewed in relation with the rest of the scales, these results did not allow a clearly pathological interpretation.
In the psychological interview, she did not manifest psychotic symptomatology or severe personality disorders, either. There was only a deterioration that we thought might be due to her family circumstances and the institutional influence and, consequently, reversible.
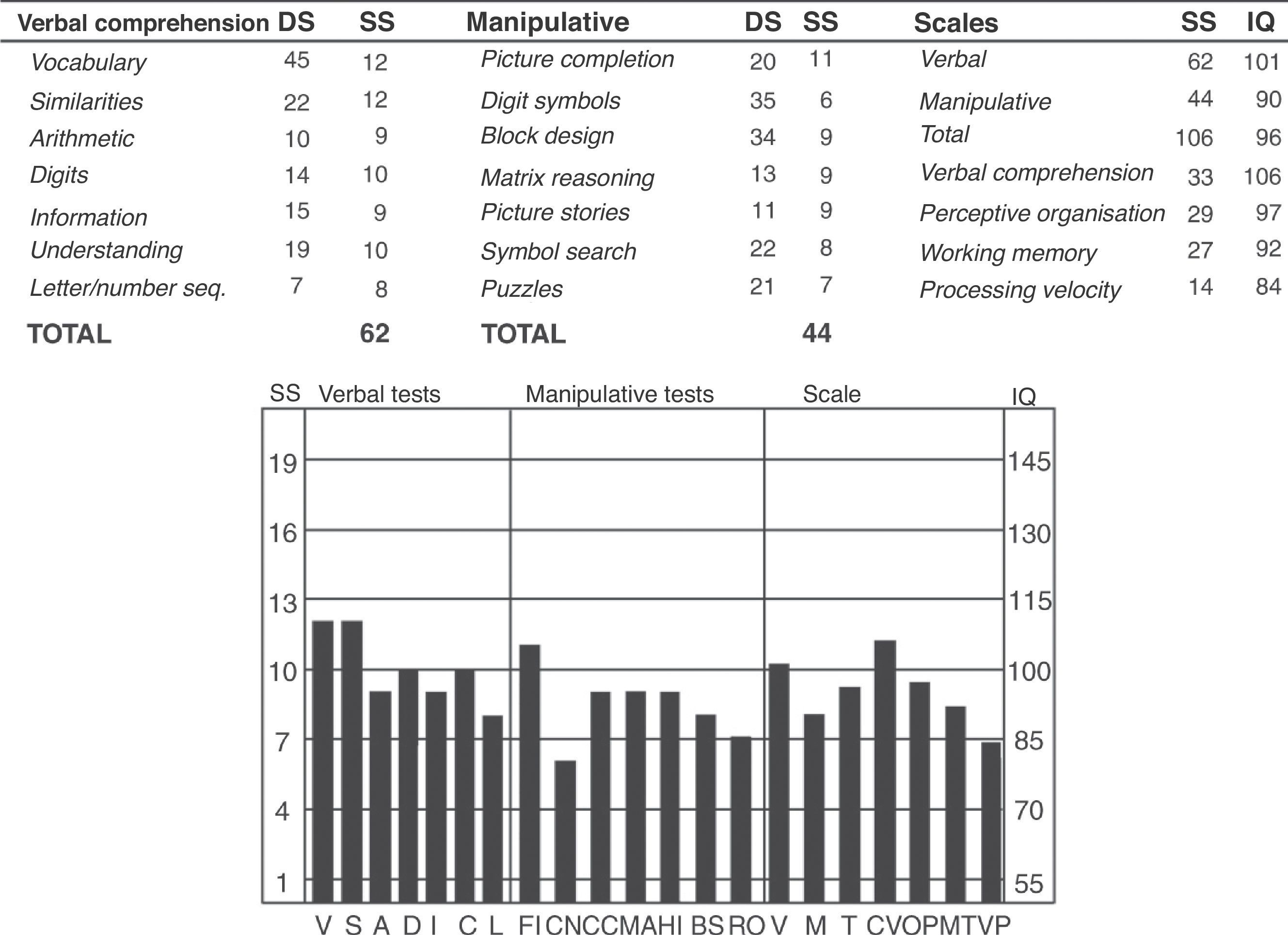
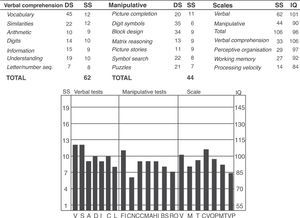
On the patient's last admission to this hospital, from which the idea of this article arose, we decided to administer the Wechsler adult intelligence scale, WAIS III. Various sessions were required, due to the difficulties that she presented in maintaining the attention levels necessary.
It was impossible to administer other tests, given the total lack of posterior collaboration. The patient was characterised by significant impairments in functionality, together with continuous somatic complaints and, above all, psychopharmacological agents; all of these made it extremely difficult to increase her degrees of autonomy and social functioning. Analysing the test results revealed an intellectual functioning level of total IQ of 96, which puts her in an intermediate level of intelligence. With a confidence level of 90%, the patient's true total IQ would lie between 89 (low-normal) and 103 (average). She achieved a verbal IQ score of 101 and a manipulative IQ score of 90. There was a difference of 11 points in favour of the first score, which told us that she showed her intelligence better through verbal comprehension and expression than through a non-verbal form. Upon analysing the points obtained in the various indexes, we could see a significant difference between perceptive organisation (IQ 97) and processing speed (IQ 84). This indicated that she obtained better results on the tasks that measure non-verbal thinking than on those that measure visual-motor processing speed (Fig. 2).
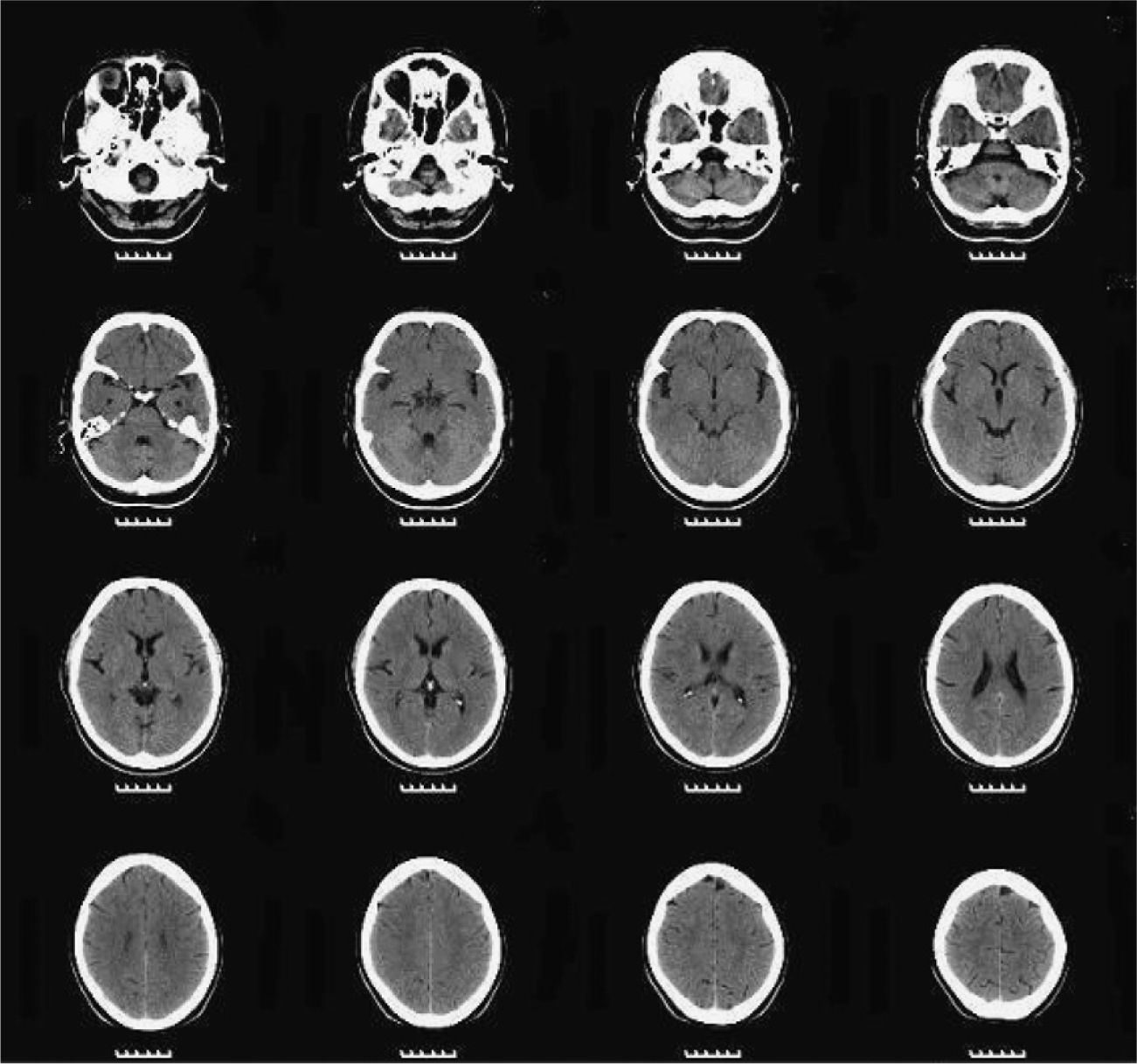
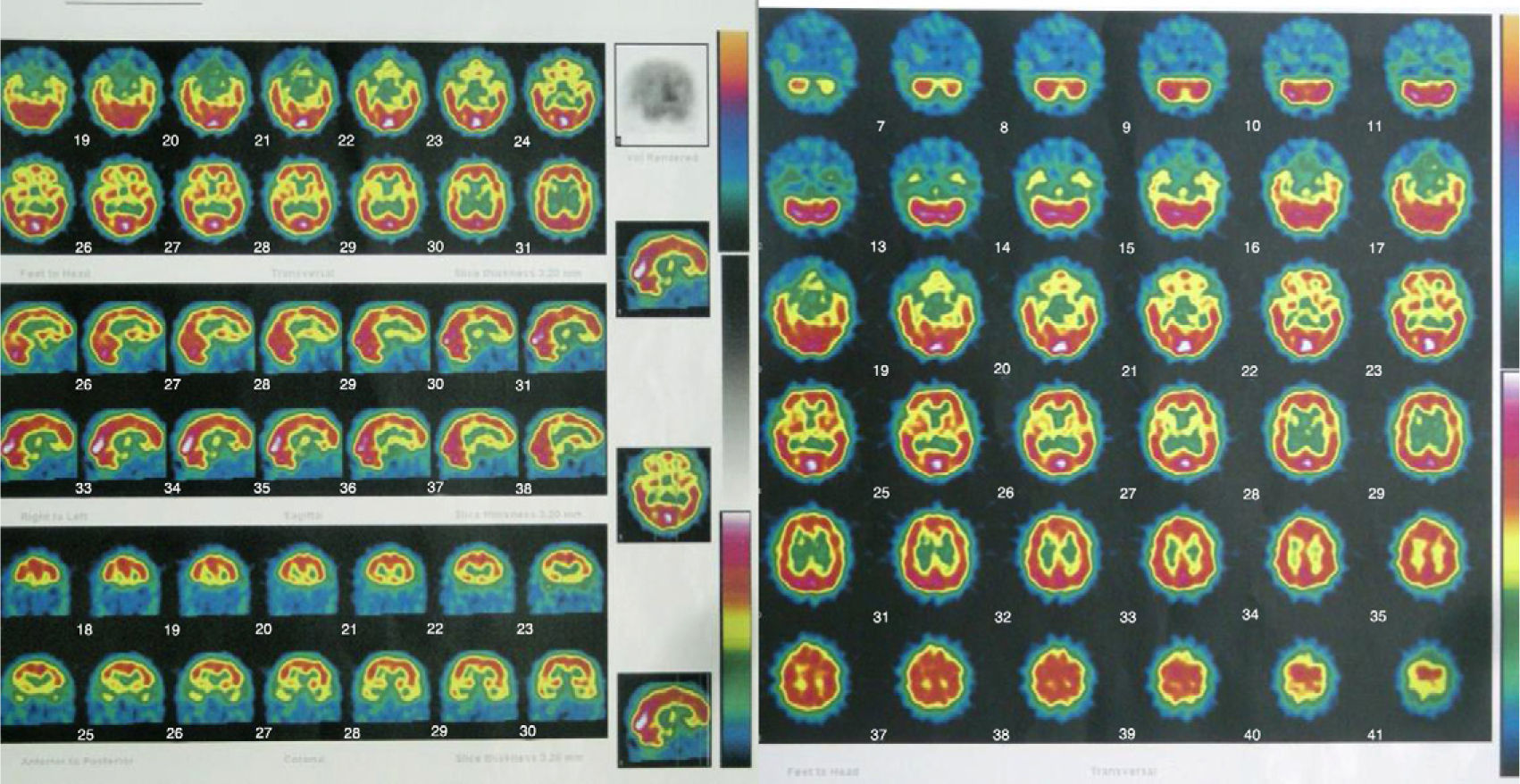
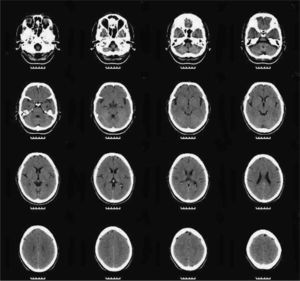
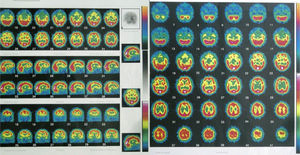
We asked for a magnetic resonance (MR) and a SPECT as complementary tests to see if there were anatomical brain findings of Crow's Type II schizophrenia.15 The patient had already had a brain MR in 2005, without finding any significant alterations. The 2010 MR revealed the presence of slight, predominantly frontal cerebral atrophy (Fig. 3), while a bilateral temporal hypoperfusion was observed in the SPECT (Fig. 4).
In the autonomous community of the Murcia region, the number of patients diagnosed with schizophrenia attended during 2008 in the mental health centres of the health network of the Murcia Health Service was 1895. Of these, only 15 (less than 0.8%) received the diagnosis of simple schizophrenia.16 These figures are very low, even compared with those obtained in other epidemiological studies published.4–7
The clinical case we present, that of a 36-year-old woman, shows that the absence of the striking positive psychotic symptoms associated with the diagnosis of schizophrenia makes it more difficult to keep this family of disorders in mind to explain the symptoms of functional deterioration suffered. It is also possible that, in normal clinical practice, the main orientation of psychopathological examination towards the rapid appearance of symptoms that are «new», disruptive and evident masks the interpretation of the gradual loss of previously acquired capabilities when this loss cannot be attributed to the other symptoms.
The presence of affect-related, non-specific symptomatology, with anxiety, low frame of mind, anergia, apathy and anhedonia, together with the repeated occasions in which the patient expressed suicidal ideation, were the reason that the initial diagnoses shifted towards affective disorders.
Although the patient did not present positive psychotic symptoms (hallucinations and delirium) in any of the times she was in our hospital, these symptoms could have been present briefly in some of the episodes of worsening she underwent. That would explain the diagnoses of psychotic depression, affective paraphrenia and schizoaffective disorder that the patient received at one time or another of her medical history. However, we assume that the intensity and duration of these symptoms was short (depressive delirious ideas more than authentic delirium, occasional auditory pseudo-hallucinations) and, consequently, gave insufficient grounds for maintaining the diagnosis. In contrast, as both the family and the patient herself explained, weeks before her last psychiatric admission she was urged by another psychiatrist to abandon drug therapy completely, in the interpretation that what she had was a personality disorder.
The doubts that arose in the diagnosis of this patient have contributed to how erratic her treatment was. She had consultations at many clinics and numerous clinical trials, sometimes based on contradictory approaches, without the idea of including her in a comprehensive rehabilitation programme that could prevent or slow her deterioration being considered. All these vacillations or uncertainties also contributed to increasing the anguish experienced by the patient and her family.
It was only after many years of illness, as a conclusion to the patient's evolution, the results from the psychometric tests described above and the findings from the 2 neuroimaging tests helped us to reach the conviction that everything supported the diagnosis of simple schizophrenia.17
The prevalence obtained for simple schizophrenia, as has been indicated, could be too low for 2 reasons: some patients with simple schizophrenia may not seek psychiatric assistance, with this being more probable than in the case of other schizophrenia subtypes because of the less dramatic clinical presentation in simple schizophrenia7; and the individuals affected by simple schizophrenia can present a loss of insight and initiative, with it being improbable that they would seek psychiatric help for themselves.8 It is also possible that some patients with simple schizophrenia receive other diagnoses once they have been seen in health centres.7 The absence of the most dramatic positive psychotic symptoms and the tendency to identify the schizophrenic disorder with their presence, at least during some moment of the evolution, can be a contributing factor in keeping simple schizophrenia a relegated diagnosis.
Doubts as to its diagnostic validity and the controversy around its concept have undoubtedly lead to the scant number of studies on this disorder.18,19 However, as we have demonstrated with this case history, there continue to be patients who fulfil the criteria proposed for this disorder.
If, as clinical observations indicate, the negative and positive symptoms of schizophrenia can be present in different combinations, with there being patients who show sets of positive symptoms with negligible negative symptomatology, there is no reason why there cannot be patients in whom the disease is characterised solely, or almost exclusively, by negative symptoms.17,19,20 These include nuclear traits such as an insidious onset, abulia, affective flattening and a deteriorating course, without the presence of abnormal experiences and behaviour phenomena indicative of positive symptoms of schizophrenia. However, the fact that they do not reach the intensity of those seen in the typical forms of this illness (by being symptoms that are minor, brief or not of a clearly psychotic nature), does not have to invalidate the diagnosis of simple schizophrenia.17,19 Ey indicated that it is almost always possible to find forms of delirious or hallucinatory phenomena so discrete in these patients, that they could be unnoticed by those who lived with them.21 The existence of such symptoms could really be indicating the continuity of simple schizophrenia with other subtypes of schizophrenia, which would also constitute a continuum among themselves and would not always remain stable over time.17 For all of these reasons, some authors have defended the position that the newest nosological systems for schizophrenia should be more dimensional (poor psycho-motor skills, disorganisation and reality distortion) than categorical.18
These symptoms typical of simple schizophrenia might be more evident in the context of a functional assessment than within a psychopathological description of the patient. The extension and intensity of the difficulties presented by the patients can be assessed better by batteries of neuropsychological tests.18,22 Such tests can detect intellectual impairment, with deficits in executive functions and memory, just as other schizophrenic patients present.17
Although not always, in various studies on neuromorphological anomalies of patients diagnosed with simple schizophrenia, there are anomalies typical of other schizophrenia subtypes, such as greater ventricular and subarachnoid space volumes, as well as further alterations in brain development.23–25 Studies on visual evoked potentials show alterations in various subtypes of patients with schizophrenia, including those who received the diagnosis of simple schizophrenia.26 Functional neuroimaging tests like the SPECT can demonstrate a deficit of perfusion in the frontal regions, associated with aspects of schizophrenia such as chronicity, presence of a negative clinical syndrome and cognitive deterioration17. This hypoperfusion of the prefrontal grey matter has also been found in more recent studies, such as Suzuki's.27
The delay in recognition, because this is an illness with an insidious onset and deteriorating chronic course, has serious consequences with respect to providing appropriate medical, psychiatric and social interventions, with the consequent negative effect on the prognosis.8 Given that these patients do not present the positive symptoms of schizophrenia, with their disruptive and troublesome nature, it is more likely that their families or primary health centres will not initially recognise them to be mentally ill individuals.8,21 Various authors emphasise that these patients tend to present, above all in the initial phases, multiple somatic discomforts that bring to mind neurotic disorders, if not simple laziness, as the first diagnosis.21 All of these circumstances help to make simple schizophrenia a diagnosis that is often forgotten.28
Increasing the acknowledgement of this subtype of schizophrenic disorder would help to provide the patients with appropriate medical and psychiatric treatment.8,29,30 The number of studies published on treatment for these patients are practically incidental; however, based on the possible improvement in the negative symptoms of the disorder, some authors have proposed the use of neuroleptics even in doubtful clinical cases or when simple schizophrenia is only suspected.29,30
This is a disorder that, psychopathologically speaking, can present with a low symptom profile (in the case we describe, the personality test results oscillated from very pathological, in 2005, and normal, in 2010). Consequently, using tests for functional and neuropsychological deterioration, as well as functional neuroimaging tests, can be very useful for diagnosing it.18
ConclusionsIn spite of the controversy around it, we consider that the diagnosis of simple schizophrenia responds to a nosological reality in which patients who cannot be assimilated into the diagnostic criteria of other mental disorders can be fitted. The general lack of interest about simple schizophrenia has contributed to the fact that the literature on it still remains scant, especially with respect to the underlying neuromorphological alterations and to treatment. Even though the DSM-IV-TR included it in the criteria for research on simple deterioration disorder, the majority of the articles published (like this one) involve isolated clinical cases. The oversight with which this diagnosis has been treated among the scientific community seems to put its permanence in the clinical imagination in danger. In consequence, it runs the risk of being an underdiagnosed disorder, with the damage that a delay in identifying it can cause the individuals affected.
Including simple schizophrenia in the differential diagnosis of other chronic deteriorating disorders could increase its recognition in the initial phases. Using neuropsychological functional tests and looking for patterns of deterioration typical in the schizophrenic spectrum could help to increase the reliability of the diagnosis. There should be epidemiological studies, both among the general population and in clinical populations, to make it possible to estimate the true prevalence of this illness.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Martínez Serrano J, et al. En defensa del diagnóstico de esquizofrenia simple: reflexiones a propósito de un caso. Rev Psiquiatr Salud Ment (Barc). 2012;5(1):53-62.