Lithium as medication is mainly used in psychiatry as treatment for bipolar disorder and to a lesser extent in neurology (preventative of cluster headache and Kleine-Levin syndrome). Treatment with lithium may give rise to both acute and chronic neurotoxicity.1 The syndrome of Irreversible lithium-effectuated neurotoxicity (SILENT) refers to the persistent neurological sequelae after lithium intoxication. We describe a case of SILENT secondary to heatstroke.
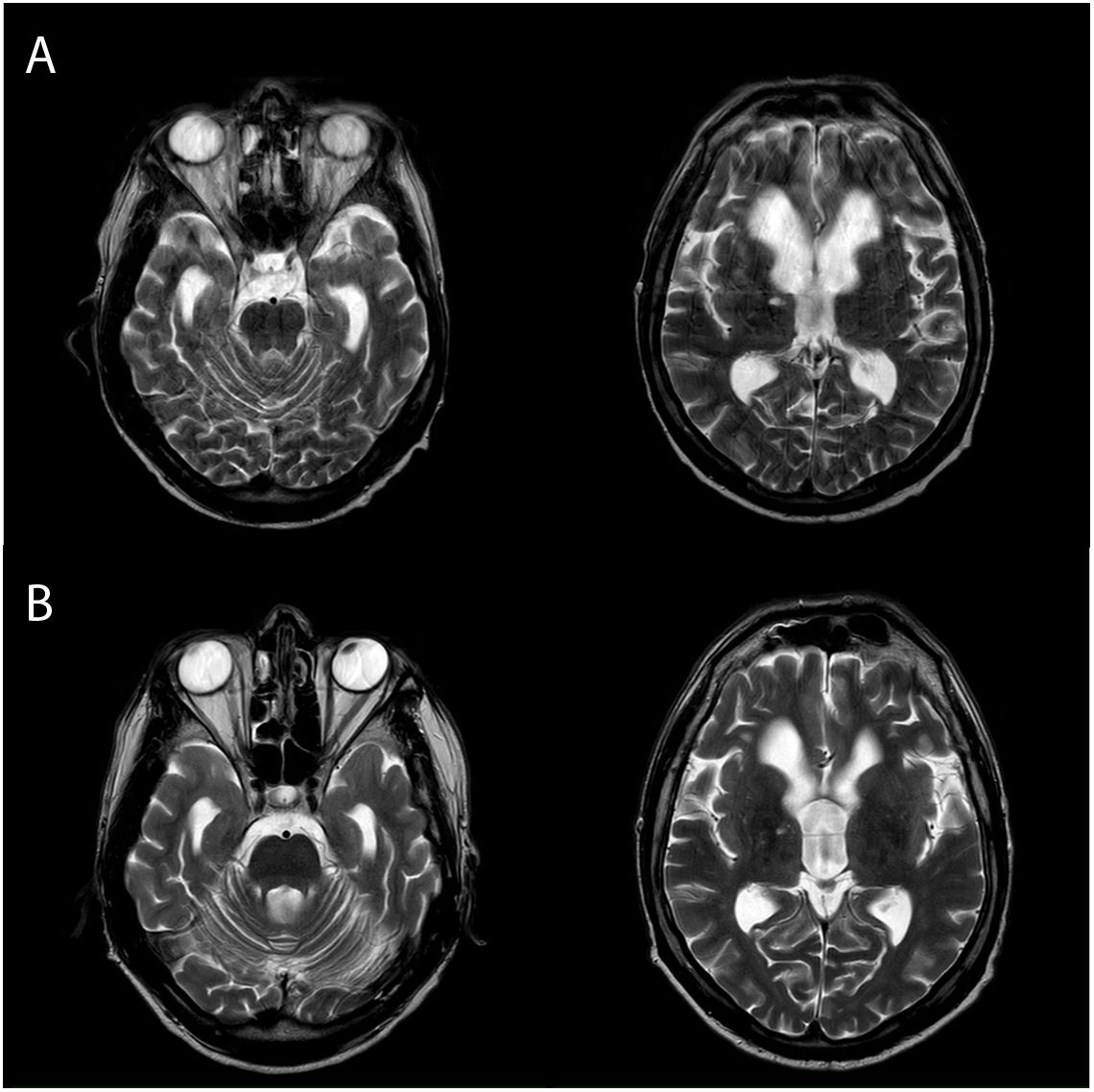
A 42-year old male with a history of type 1 bipolar disorder, chronic oenolism, meningitis as a child, epilepsy and mild intellectual disability was treated with 400-200-400 mg lithium carbonate, 500-500-500 mg valproic acid, 10-10-10 mg olanzapine and 1-1-1 mg. clonazepam. The latest lithaemia (12 days prior to hospital admission) was within therapeutic range (.9 mEq/L). The patient was found on a public highway in the summer of 2018 due to impaired consciousness (Glasgow Coma Scale 6), hyperthermia (40 °C) and low blood pressure (70/40 mmHg), requiring intubation. Analysis highlighted severe hyponatraemia (120 mEq/L) with no rabdomyolysis (CK 317 U/L), with reasonable suspicion of heatstroke and ruling out of malignant neuroleptic syndrome. The other analyses, lumbar puncture and urine toxicants tested normal. Valproate levels were normal but lithaemia was not requested. Computerised axial tomography (CAT) of the brain showed a triventricular hydrocephalus which was already known. After 24 h natraemia was 134 mEq/L. A On the fourth day the patient was extubated, with continuous generalised choreoathetosis movements, scandid dysartheria, broad horizontal-rotatory nystagmus and spastic tetraparesis being observed. Lithium was discontinued and levodopa/carbidopa was started, with slight clinical improvement. Days later, a clear bilateral cerebellar syndrome with appendicular dysmetria and trunk ataxia could be observed. Two nuclear magnetic resonance imaging (NMRI) of the brain were performed, the first nine days after admission and the second at day 24 (Fig. 1A), both without any changes compatible with myelinolysis. After one month of admission the patient had a severe appendicular and axial cerebellar disorder with choreoathetosis movements, mild tetraparesis and pyramidalism. An MRI after eight months (Fig. 1B) showed no alterations other than known hydrocephalus. Given the neurological semiology, the persistence of sequelae more than two months after lithium withdrawal and normal neuroimaging, the patient was finally diagnosed with SILENT.
Evolution of brain NMRI.
Bottom of image: Brain NMRI in T2 sequence, cross-sectional slices at protuberance level (A1 and B1) and base lymph nodes (A2 and B2), of our patient. Images A) correspond to the NMRI performed during admission, 24 days after symptom onset and images B) to that performed after 8 months. In both a triventricular hydrocephalus is observed with no evidence of demyelinating lesions characteristic of osmotic myelinolysis either in the protuberance or base lymph nodes.
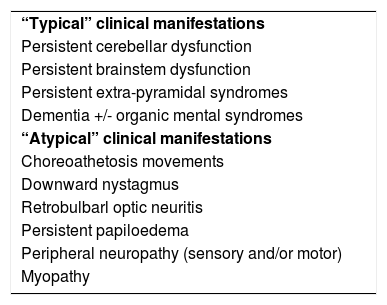
SILENT involves the neurological sequelae resulting from acute lithium carbonate intoxication and is less frequent from chronic use, when they persist two months after ceasing treatment.1,2 Despite of the fact that lithium is still widely used today, SILENT is an uncommon entity.1,3,4 Its physiopathology is as yet unknown, although demyelinisation appears to play a relevant role.1 A loss of cortico-subcortical volume at the cerebellar level and in the subgenual cortex has been described,5 together with the loss of Purkinje cells with glycosis and atrophy of the cerebellar cortex, thus explaining the predominantly cerebellar nature of the condition. The existence of previous neurological sequelae appears to confer a particular susceptibility to the neurotoxic effects of the lithium.1 Also, concomitant consumption of neuroleptics or valproate, fever, dehydration and hyponatraemia were described as risk factors associated with SILENT,1 as occurred in our patient, where dehydration in the context of the heatstroke led to an increase in the plasmatic concentration of the lithium. The therapeutic margin for lithium is narrow and its determination is simple and inexpensive, and should be carried out early in the event of any suspicion of poisoning. In our patient the lithaemia was not determined in the emergency services, which could have impacted posterior patient management and evolution. Inversely, lithium intoxication can give rise to fever and hyponatraemia.1 Typical symptoms of SILENT include cerebellar impairment, extra-pyramidal syndromes or persistent troncoencephallic dysfunction (Table 1).1 choreoathetosis movements, which were prominent in our patient, have been described within the “atypical” manifestations of SILENT (Table 1).1,6,7 Within the differential diagnosis of our patient osmotic myelinolysis was considered after rapid correction of the hyponatraemia and/or through acute lithium intoxication;8 however, early choreoathetosis would be atypical for this entity9 and the normality in the consecutive NMRI finally allowed it to be ruled out. With regard to the therapeutic approach to SILENT, in general, sequelae are persistent and there is no effective treatment. Haemodialysis has been suggested as treatment in the early phase of lithium intoxication, with controls of plasmatic levels during and after the procedure.1,10 In our case treatment with levodopa/carbidopa was started, with partial relief of choreoathetosis movements.
“Typical” and “atypical” manifestations of SILENT.
| “Typical” clinical manifestations |
| Persistent cerebellar dysfunction |
| Persistent brainstem dysfunction |
| Persistent extra-pyramidal syndromes |
| Dementia +/- organic mental syndromes |
| “Atypical” clinical manifestations |
| Choreoathetosis movements |
| Downward nystagmus |
| Retrobulbarl optic neuritis |
| Persistent papiloedema |
| Peripheral neuropathy (sensory and/or motor) |
| Myopathy |
Modified from Adityanjee et al.1
Lithium intoxication and SILENT should be considered in all patients under treatment with lithium who develop neurological symptoms, with haemodyaliysis as emergency treatment in cases of severe intoxication. Myelinolysis may occur after acute lithium intoxication and should be included in differential diagnosis of SILENT.
Conflict of interestsAll authors have no conflict of interest to declare in the publication of this article.
Please cite this article as: Martínez-Martín Á, Sánchez-Larsen Á, Sánchez-Mora C, Sáez-Povedano R, Segura T. Intoxicación por litio: la amenaza SILENTiosa. Rev Psiquiatr Salud Ment (Barc). 2020;14:233–234.