Although home hospitalisation has begun to develop widely in recent years there is a notable lack of studies. The following study includes data from the Psychiatric Home Hospitalisation Unit of the Hospital del Mar (HADMar). This programme has been running for 2 years and takes place in a socio-demographically depressed area in Barcelona. It receives patients from community and hospital services. Monitoring is limited in time and at discharge patient are referred to the ambulatory unit.
Material and methodsAll patients visited from 2015 to the present time were selected. A total of 135 patients were included in the sample. A qualitative descriptive study was carried out in order to define the socio-demographic characteristics. The severity of symptoms, suicidal risk and changes in the functionality were considered as clinical outcomes.
ResultsThe mean age of patients was 44.6 years and there were no gender differences. A total of 26 patients had a history of suicidal attempts and 11.1% lived alone; 51.1% were diagnosed with a psychotic disorder. The mean GEP score for the severity of the psychiatric symptoms was 2.39 and the mean risk of suicide was 0.49. There is an increase in the EEAG score from admission to discharge, which means an improvement in the functionality of patients.
ConclusionsThe results obtained in our study are consistent with previous results. Home crisis intervention teams have proved to be an alternative to traditional hospitalisation. However, more studies are needed to support these results.
A pesar del desarrollo de la hospitalización domiciliaria en España durante los últimos años, es llamativa la escasez de literatura. El siguiente estudio pretende exponer los datos obtenidos por la Unidad de Hospitalización a Domicilio de Psiquiatría del Hospital del Mar (HADMar). HADMar es un programa de hospitalización domiciliaria creado hace 2 años, que recibe pacientes procedentes de servicios comunitarios y hospitalarios con un seguimiento limitado en el tiempo. Al alta, el paciente es derivado a la unidad de referencia ambulatoria apropiada para cada caso.
Material y métodosSe seleccionó a todos los pacientes visitados desde 2015 hasta la actualidad. Se llevó a cabo un estudio descriptivo que define las características sociodemográficas de la muestra. Las variables clínicas estudiadas fueron la gravedad de los síntomas, el riesgo de suicidio y los cambios en la funcionalidad.
ResultadosUn total de 135 pacientes fueron incluidos en la muestra. La edad media de los pacientes fue de 44,6 años y no hubo diferencias entre ambos sexos. De ellos, 26 pacientes tenían un historial de intentos autolíticos y el 11,1% vivían solos. El 51,1% fueron diagnosticados de un trastorno psicótico. La puntuación media en la escala GEP en la variable gravedad de los síntomas psiquiátricos fue 2,39 y el riesgo medio de suicidio 0,49. La puntuación de EEAG al alta era mayor que al ingreso.
ConclusionesLos resultados obtenidos en nuestro estudio son consistentes con resultados reportados en estudios previos. Los equipos de hospitalización domiciliaria han demostrado ser una alternativa a la hospitalización tradicional. Sin embargo, se necesitan más estudios que apoyen estos resultados.
Home hospitalisation in cases of mental illness aims to provide care at time of crisis and intensive home treatment as an alternative to admission to hospital. Since the late 1990s, this type of therapeutic model has been implemented in parallel in different areas of Australia, the United States and Europe,1–4 including Spain. Nonetheless, there is a notable absence of studies that provide objective statistical data, and the differences in resources and characteristics of devices in the different regions are notorious.5 This is why it is essential to obtain specific information on the functioning and characteristics of home care teams in our environment. With this in mind, we carried out this study gathering the data from a home hospitalisation unit operating in the Barcelona metropolitan area; specifically, the Psychiatric Home Hospitalisation Unit of the Hospital del Mar (HADMar).
This programme has been in operation since January 2015 and caters for patients in the Sant Martí and Ciutat Vella sectors, socio-demographically depressed areas in Barcelona. It comprises a permanent team of 2 psychiatrists, a psychologist, 2 nurses and a nursing assistant, who work from 8am to 5pm from Monday to Friday. Two telephone numbers are provided for the patient or their family members to contact the team during care hours or outside care hours via voicemail. Also, in the case of emergencies from 5pm to 8am and at weekends, patients are attended by the duty psychiatrist, who has access to the medical records of all home hospitalised patients. Only patients with severe decompensated mental disorders belonging to the catchment area who have agreed to the admission conditions (treatment and therapeutic indications) and with a family member or caregiver acting as a co-therapist are selected. Serious behavioural disorders, absence of appropriate support, suicidal ideation, being under the age of 16, a diagnosis of cognitive impairment, concomitant toxic substance dependence or abuse, exclusive diagnosis of personality disorder or eating disorder are the exclusion criteria. Patients are referred from outpatient mental health centres, the acute hospitalisation unit of the Hospital del Mar, the psychiatry emergency unit of the Hospital del Mar, the crisis unit, or day hospital and outpatient clinics of the Hospital del Mar. Referrals can be made by telephone, fax or e-mail. The nursing assistant receives the patients’ data and the specialist nurse, in agreement with the psychiatrist, assesses the appropriateness of the request and contacts the referring specialist to report whether the case has been either accepted or rejected. Patients who are admitted are assessed by the team in less than 48h, there is no waiting list as yet. Both patients and responsible caregivers sign their informed consent for home admission. Follow-up is time limited, according to the needs of each case, with daily visits a maximum of 3 days apart. During follow-up, contact is maintained with those referring from primary care for assessment of any organic or social problems that may arise. When the patient is discharged, they are contacted and a link visit is coordinated with the relevant ambulatory referral unit and a report is provided. Finally, before the case is closed, it is confirmed that the patient has attended their first outpatient follow-up visit.
Acute home treatment that incorporates Crisis Resolution Programmes (CRP), started in the United Kingdom through the implementation of the National Health Plan 2000, in parallel with other community care services such as early intervention teams and community-based assertive treatment. Like the British CRPs, HADMar seeks to provide a rapid and effective therapeutic response in the community to patients in times of crisis. Follow-up is intensive and ongoing, with frequent home visits until it is possible to link to another follow-up device that is appropriate for each case. it is aimed at people who, in the absence of a CRP, would require hospital admission and it also seeks to facilitate the transfer home of patients already admitted to hospital to reduce their hospital stay. Other similarities between the two services are that the teams are multidisciplinary, carry out coordinated interventions and provide time-limited interventions. Limitations in terms of availability and number of visits should be mentioned as differences, with a higher proportion of patients per professional.
Material and methodsOne hundred and thirty-five patients were included in the sample, which comprised the total number of patients visited by this team from January 2015 to August 2017. A descriptive quantitative study was undertaken to define the socio-demographic features of the target population, and to evaluate the clinical results obtained. To this end, the severity of symptoms measured by the Psychiatric Disease Severity Scale (GEP) and changes in functionality on admission and discharge measured by the Global Activity Assessment Scale (EEAG) were proposed as the main variable. The potential risk of suicide assessed by the item on the GEP scale was put forward as a secondary variable. In the case of patients with a psychotic disorder, changes in the total score of the Positive and Negative Syndrome Scale (PANSS) before and after the intervention were also assessed. In addition, the number of admissions to conventional acute units at 6 weeks and at 6 months after discharge from home hospitalisation were also retrospectively analysed, and the socio-demographic variables of this subgroup of patients were described.
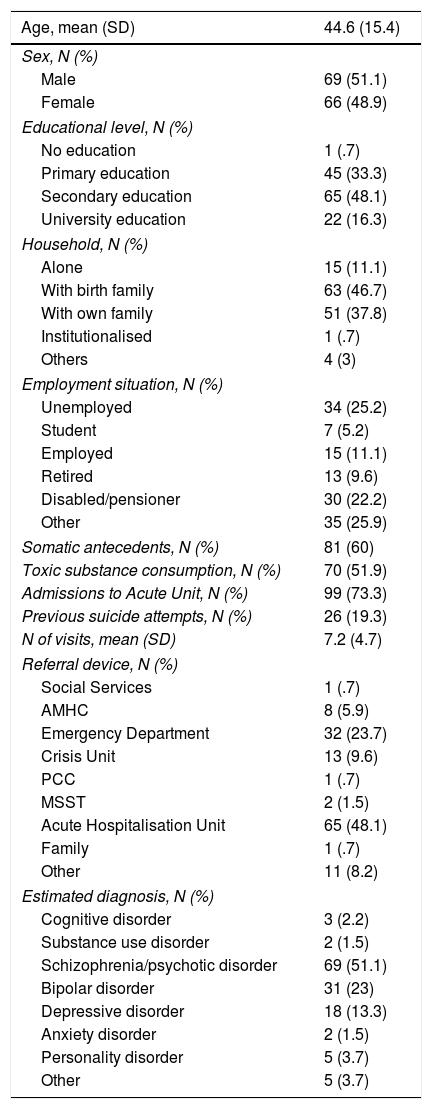
ResultsThe results obtained were collected in the Tables and Figures shown below. Table 1 summarises the socio-demographic features of the sample.
Socio-demographic characteristics of the sample.
| Age, mean (SD) | 44.6 (15.4) |
|---|---|
| Sex, N (%) | |
| Male | 69 (51.1) |
| Female | 66 (48.9) |
| Educational level, N (%) | |
| No education | 1 (.7) |
| Primary education | 45 (33.3) |
| Secondary education | 65 (48.1) |
| University education | 22 (16.3) |
| Household, N (%) | |
| Alone | 15 (11.1) |
| With birth family | 63 (46.7) |
| With own family | 51 (37.8) |
| Institutionalised | 1 (.7) |
| Others | 4 (3) |
| Employment situation, N (%) | |
| Unemployed | 34 (25.2) |
| Student | 7 (5.2) |
| Employed | 15 (11.1) |
| Retired | 13 (9.6) |
| Disabled/pensioner | 30 (22.2) |
| Other | 35 (25.9) |
| Somatic antecedents, N (%) | 81 (60) |
| Toxic substance consumption, N (%) | 70 (51.9) |
| Admissions to Acute Unit, N (%) | 99 (73.3) |
| Previous suicide attempts, N (%) | 26 (19.3) |
| N of visits, mean (SD) | 7.2 (4.7) |
| Referral device, N (%) | |
| Social Services | 1 (.7) |
| AMHC | 8 (5.9) |
| Emergency Department | 32 (23.7) |
| Crisis Unit | 13 (9.6) |
| PCC | 1 (.7) |
| MSST | 2 (1.5) |
| Acute Hospitalisation Unit | 65 (48.1) |
| Family | 1 (.7) |
| Other | 11 (8.2) |
| Estimated diagnosis, N (%) | |
| Cognitive disorder | 3 (2.2) |
| Substance use disorder | 2 (1.5) |
| Schizophrenia/psychotic disorder | 69 (51.1) |
| Bipolar disorder | 31 (23) |
| Depressive disorder | 18 (13.3) |
| Anxiety disorder | 2 (1.5) |
| Personality disorder | 5 (3.7) |
| Other | 5 (3.7) |
PCC: Primary Care Centre; AMHC: adult mental health centre; MSST: multidisciplinary specialist support team.
Most of the patients treated were in middle adulthood, although the sample also included the geriatric population. All the patients visited were over 18 years of age. There were no differences between sexes, and the educational level was representative of the population. The majority lived with their birth or own family, and fewer than 12% lived alone. A quarter remained economically inactive. The presence was noteworthy of somatic antecedents other than psychiatric illness and toxic substance use, which affected more than half the sample. Of the cases, 73% had a history of at least one admission to an acute psychiatric unit, and 20% reported suicide attempts in the past. Regarding the type of psychiatric illness, 51% were diagnosed with psychotic disorders and 36% with affective disorders. In terms of the characteristics of clinical care in HADMar, the average follow-up is 7 visits per patient. The main source of patient referral is the acute hospitalisation unit, followed by psychiatric emergencies.
The mean obtained on the GEP scale for the severity of the psychiatric symptoms of the patients visited was 2.39 (SD .7), and the mean potential risk of suicide was GEP1=.49 (SD .75). In both subscales the results are measured from 0 to 3; the greater the number the greater the risk and severity of symptoms.
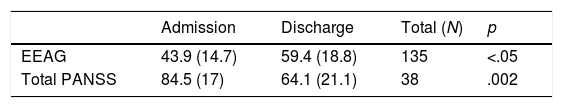
Table 2 lists the changes in functionality and severity of symptoms before and after the intervention. There is an increase in the EEAG score from admission to discharge. This increase is almost 15 points and represents a significant and clinically relevant improvement in the functionality of patients receiving home treatment. In addition, 38 of the 69 individuals in the subgroup of patients with psychotic disorders were measured for symptom severity using the PANSS scale. In the study, the total PANSS values were collected on admission and on discharge in this group of patients. The results obtained were a decrease of 21 points on the scale, which implies an improvement in the severity of the symptoms.
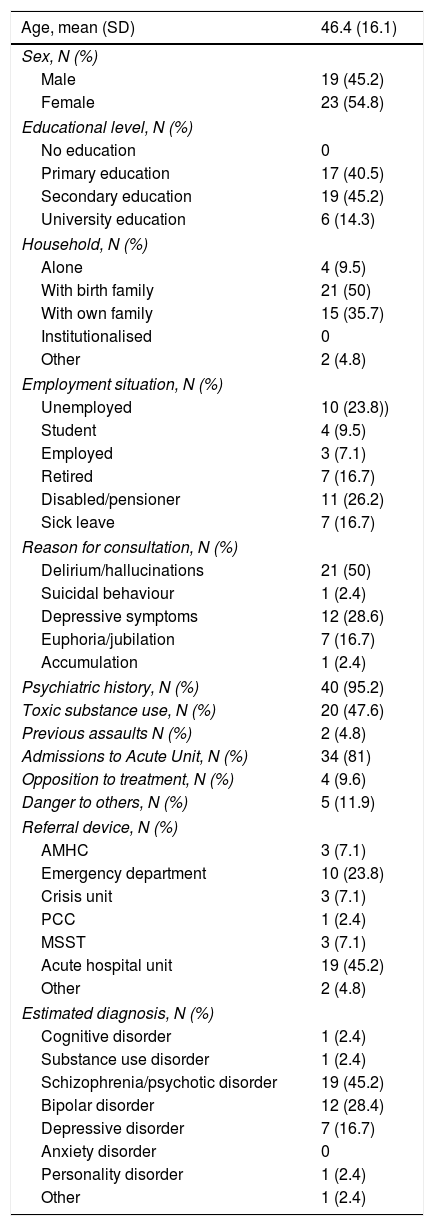
Of the 135 patients initially included in the sample, follow-up was not possible of 2 patients due to a change in sectorisation, but it was possible to obtain information for the remaining 133 patients following discharge. During follow-up, 12 readmissions and 5 suicide attempts were collected; none resulted in accomplished suicide. After discharge, 42 (31.6%) patients required one or more admissions to conventional acute hospitalisation units. A total of 57 episodes of acute admission were found, of which 25 (43.9%) were during the first 6 weeks following discharge and, of these, 16 (64%) occurred in under 24h. Between 6 weeks and 6 months a total of 13 (22.8%) episodes of admission were counted, and 19 (33.3%) were after 6 months. Table 3 describes the main socio-demographic characteristics of this subgroup of patients. A greater number of women were admitted, unlike other samples, in which being male was associated with an increased risk of admission to hospital. Less than 10% of the cases showed significant active opposition to treatment, and there was hetero-aggressive risk in only 5–12%.6,7 With regard to the remaining variables studied, the results were similar to findings reported in these studies. In 50% of cases the reason for consultation was the presence of delusions or hallucinations, and referrals mostly came from the hospital emergency department and the acute ward. Forty-five percent had a diagnosis of psychotic disorder, and 81% had one or more previous admissions to acute hospital units.
Socio-demographic characteristics of the patients readmitted to acute hospital units.
| Age, mean (SD) | 46.4 (16.1) |
|---|---|
| Sex, N (%) | |
| Male | 19 (45.2) |
| Female | 23 (54.8) |
| Educational level, N (%) | |
| No education | 0 |
| Primary education | 17 (40.5) |
| Secondary education | 19 (45.2) |
| University education | 6 (14.3) |
| Household, N (%) | |
| Alone | 4 (9.5) |
| With birth family | 21 (50) |
| With own family | 15 (35.7) |
| Institutionalised | 0 |
| Other | 2 (4.8) |
| Employment situation, N (%) | |
| Unemployed | 10 (23.8)) |
| Student | 4 (9.5) |
| Employed | 3 (7.1) |
| Retired | 7 (16.7) |
| Disabled/pensioner | 11 (26.2) |
| Sick leave | 7 (16.7) |
| Reason for consultation, N (%) | |
| Delirium/hallucinations | 21 (50) |
| Suicidal behaviour | 1 (2.4) |
| Depressive symptoms | 12 (28.6) |
| Euphoria/jubilation | 7 (16.7) |
| Accumulation | 1 (2.4) |
| Psychiatric history, N (%) | 40 (95.2) |
| Toxic substance use, N (%) | 20 (47.6) |
| Previous assaults N (%) | 2 (4.8) |
| Admissions to Acute Unit, N (%) | 34 (81) |
| Opposition to treatment, N (%) | 4 (9.6) |
| Danger to others, N (%) | 5 (11.9) |
| Referral device, N (%) | |
| AMHC | 3 (7.1) |
| Emergency department | 10 (23.8) |
| Crisis unit | 3 (7.1) |
| PCC | 1 (2.4) |
| MSST | 3 (7.1) |
| Acute hospital unit | 19 (45.2) |
| Other | 2 (4.8) |
| Estimated diagnosis, N (%) | |
| Cognitive disorder | 1 (2.4) |
| Substance use disorder | 1 (2.4) |
| Schizophrenia/psychotic disorder | 19 (45.2) |
| Bipolar disorder | 12 (28.4) |
| Depressive disorder | 7 (16.7) |
| Anxiety disorder | 0 |
| Personality disorder | 1 (2.4) |
| Other | 1 (2.4) |
PCC: primary care centre; AMHC: adult mental health centre; MSST: multidisciplinary specialist support team.
There currently persists an imbalance in the mental health system between the care needs of patients and the provision of community services for the treatment of acute and severe psychiatric illness. The efforts of the World Health Organisation and European institutions to promote community-based policies have facilitated the creation of new types of crisis intervention that have, however, been unevenly implemented.8,9 In recent decades, movements based on early intervention in mentally ill patients have emerged exponentially, seeking not only to reduce symptoms but also to preserve patient autonomy and functionality. Home care constitutes an indispensable requirement for the implementation of these models.10,11
According to the data reviewed in our study, the home care model deployed in the Hospital del Mar obtained positive results in terms of significant improvement in psychiatric symptoms and, more discreetly, on levels of functionality. It is difficult to know whether these results are comparable to the benefits that would be obtained with hospitalisation, as there are not yet sufficient studies comparing both interventions.12
In terms of socio-demographic characteristics, the findings reported indicate a profile of patients with severe mental illness and frequent decompensation, consistent with the results obtained on the GEP scale. However, these data contrast with results obtained by other groups. Ness et al.,13 in a descriptive article on a Norwegian home care team, found that one third of patients had no significant mental problems and one fifth were reactive responses to stress. Hasselberg et al.2 published similar results in a sample of predominantly female patients with mild-moderate chronic psychiatric illness. The authors argue that in countries like Norway, patients at higher risk of self-harm and in vulnerable situations are preferentially referred to hospital.
Despite the severity and complexity of the patients attended by the HADMar unit, there is a relatively low risk of suicide (mean <.5 on the GEP subscale), with an incidence of suicide attempts after discharge of less than 4%. In some specific groups of patients, such as patients living alone, this risk may be greater and, therefore, patient safety must be prioritised and a specific profile defined for individuals who may benefit from this type of intervention.14
Study of the follow-up following discharge of patients provided results comparable to those obtained in the Islington studies,15,16 in which the rate of return to the acute ward at 6 weeks following discharge was less than 50%, and approximately 30% at 6 months: this latter figure is significant only in the case of voluntary admissions. As in our sample, Cotton et al. report in their article a very high percentage of patients (70%) readmitted in under 24h. This could be explained by improper referral of patients who, after an initial assessment by the home care team, were considered not to meet the inclusion requirements and who required therapeutic intervention on a hospital ward. Given that the referred patients principally came from the emergency department and acute wards, it is logical to consider that care and management pressure plays a fundamental role in the high number of readmissions during these initial hours.
It is worth mentioning that among the limitations of the study is that it is an observational analysis and therefore, no definitive conclusions can be drawn from it. Moreover, it is a relatively small sample that analyses the results of a pilot programme, therefore no quantitative details were gathered from the reference population. In terms of the severity of the symptoms in the subgroup of patients with psychotic disorders, no reasons were found to justify the considerable number of losses. Furthermore, the scales used to measure the risk of suicide and the severity of psychiatric illness are used in routine clinical practice, but not in research, and therefore it would be advisable to replicate the results with methods of measurement of higher specificity. Given that the study is aimed at a very restricted patient population, the level of external validity it provides is questionable. Moreover, the heterogeneity of operation and the resources available in each team make the results even more difficult to generalise.
In summary, despite its limitations, this study provides relevant data regarding improvement in patients’ symptoms and functionality, with low risk of associated suicide, and proposes home hospitalisation as an effective alternative to conventional hospitalisation in patients with severe decompensated mental illness. However, more studies are required to support these data and, above all, cost-benefit and qualitative studies to study other important factors such as the effects of this type of care on the family burden
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Alba Palé L, León Caballero J, Córcoles Martínez D, González Fresnedo AM, Bellsolà Gonzalez M, Martín López LM, et al. Unidad de Hospitalización Domiciliaria del Hospital del Mar. Equipo de atención psiquiátrica domiciliaria en el área de Barcelona. Rev Psiquiatr Salud Ment (Barc). 2019;12:207–212.