Ethnic differences have been studied previously in schizophrenia and first episodes. Previous studies in Nethernlands have reported a higher incidence of psychosis in male Moroccan immigrants and more clinical severity. However there is lack of studies in Spain with morocco population and FEP.
AimsThis study aims to determine the clinical differences in a sample of First episode psychosis (FEP) between morocco and Spanish population, recruited in a hospitalisation Unit.
MethodsDescriptive and cross-sectional study of 83 inpatients (FEP). Functionality and symptomatology were evaluated at entry and discharge, the pattern of use of cannabis was evaluated at entry, the dose of antipsychotic and the pattern of side-effects at discharge. Comparisons between native-born population and morocco population was made with univariate analysis and logistic regression was made for evaluating the independence of the associations.
ResultsThe 28.9% of the sample was morocco group. No significance differences were found in clinical characteristics between groups at entry or at discharge. Compared with native –born, the morocco group were more male, with less years of education, worse functionality, reported less use of cannabis, a better pattern of side effects and a tendency of more prescription of LAis.
After the multivariate analysis, just remains a lower functionality (OR 0,93; IC 95% (0,88-0,99); p=0,02) and lower years of education (OR 0,75; IC 95% (0,56-1,01);p=0,05), remain significative with being related with morocco origin.
ConclusionsOur study provides evidence for ethnic differences in morocco population with FEP. Patients with morocco ethnicity have more probability of being males, less years of educations. Have lower functionality and a better profile of side effects.
Las diferencias étnicas han sido estudiadas tanto en esquizofrenia como en primeros episodios psicóticos (PEP). En estudios realizados en los países bajos se ha descrito que en los varones de origen marroquí es más frecuente sufrir un episodio psicótico y presentar mayor severidad en la sintomatología. Sin embargo, no existen estudios en España en PEP en población marroquí comparada con autóctona.
ObjetivosExplorar las diferencias clínicas entre la población inmigrante de origen marroquí y la población autóctona, en una muestra de PEP recogida en una unidad de hospitalización de agudos.
Material y métodosSe evaluó la sintomatología y el funcionamiento al ingreso y al alta, así como el consumo de cannabis y la dosis de tratamiento antipsicótico y perfil de efectos adversos en una muestra de 83 pacientes con PEP. Se compararon los pacientes de origen marroquí con los de la población autóctona mediante análisis univariantes y la independencia de las asociaciones fue evaluada mediante análisis de regresión logística
ResultadosEl 28,9% de la muestra era de origen marroquí. No se encontraron diferencias en cuanto a la sintomatología al ingreso y al alta. Comparado con los autóctonos, los de origen marroquí eran mayoritariamente hombres, tenían menos años de educación, presentaban peor funcionamiento, menor uso de cannabis, mejor perfil de efectos secundarios y una tendencia al mayor uso de LAIS. Tras el análisis multivariante, sólo un peor funcionamiento (OR 0,93; IC 95% (0,88-0,99); p=0,02) y menos años de educación (OR 0,75; IC 95% (0,56-1,01);p=0,05), permanecieron significativamente asociados a ser de origen marroquí.
ConclusionesExisten diferencias sociodemográficas y clínicas entre PEPs de origen marroquí y población autóctona. Nuestros resultados sugieren que debería contemplarse la trascendencia de la competencia cultural en la evaluación y tratamiento de los PEPs.
Approximately 3% of the general population will suffer from a psychotic episode during their lives.1 First episodes of psychosis (FEP) usually occur between the ages of 15 and 30, with relevant clinical differences in keeping with ethnicity.2–4 Clinical evolution after a FEP may become a chronic disease and up to 80% will present with a relapse during the following 5 years.5
The study of cultural or ethnic differences and the possible development of a psychiatric disease has been a focus of interest for some years. In an initial study on migration and schizophrenia it was found that there was a higher risk for this psychotic disorder among immigrants.6 In the United Kingdom several authors have described a higher risk of developing a psychosis if the individual’s origin is black Caribbean. A higher risk has also been observed in immigrants of Moroccan origin in the Netherlands.7,8 During the last decade, the study of ethnic differences in cases of FEP has flagged up differential characteristics both in Europe and in the rest of the world.2,4,9,10 However, several inconsistencies have been described, which has indicated a drop in these risk percentages due to the improvement in tools of detection and training for assessment in cultural differences.11–13
Social factors have also been assessed as key factors in onset of psychosis and Morgan et al.14 described the social development theory with consideration of the origin of psychosis as an accumulation of stressful life events.14–16
Protocol and guideline indications for pharmacological doses and treatment criteria are the same for all populations, with no consideration of ethnic differences. However, previous studies indicate that belonging to a minority ethnicity increases the prescription of long-acting injectables (LAI) and decreases the prescription of clozapine.17 With regard to the pattern of substance consumption, several authors have described that native-born patients usually have higher levels of consumption.18,19
Notwithstanding, in many studies the ethnicity variable has been proven to be “minority”, with all types of origins being mixed together in it and with each study using a different proportion of ethnicities. The scarcity of updated and well-designed epidemiological studies in the countries of origin complicate accurate analysis of the before and after migration situation, which has probably resulted in inconsistent or contradictory outcomes.9,20 It would be more logical to carry out separate studies in each specific country and with each immigrant origin, to further support programmes of detection and aid,11 in a similar manner to the ENRICH programme of Birminghman.21
Regarding the Moroccan population, several studies have been conducted in Europe to determine cultural differences. Specifically, in Holland there is some evidence on clinical differences in FEP in the Moroccan population: the most frequent findings were the increase in the risk of developing a psychosis, especially in men, and the higher severity of symptoms.22,23
A series of studies has analysed cultural differences in mental health in Spain,19,24–26 but there are no studies that determine the differences between the Moroccan and the Spanish population with regards to FEP.
ObjectiveTo determine the clinical differences and pharmacological treatment between a Moroccan and Spanish population group in a sample of people who were hospitalised in an acute treatment unit after a FEP.
MethodSubjects: 83 patients consecutively included after being admitted to the acute treatment unit of the Hospital Universitario Pere Mata de Reus in 2017.
Inclusion criteria: aged between 18 and 35 years, affected by psychotic symptoms with sufficient knowledge of the language to complete the questionnaires. Exclusion criteria: presenting with a medical or neurological disease which accounted for the psychosis, or a disorder from toxic substance usage (excluding tobacco or cannabis).
The study was approved by the Research with Medical Products Ethics Committee from the Sanitaria Pere Virgili research institute. All participants signed an informed consent form after the study was described to them.
Tools: the psychiatric diagnosis was undertaken using the OPCRIT checklist v.4.0 (available in http://sgdp.iop.kcl.ac.uk/opcrit/).
Ethnicity classification was carried out by asking the patient for their country of origin, following the previous study model, but without taking into account second generations.27 In keeping with previous studies conducted in Holland and in Spain, we used the following nomenclature to differentiate between the 2 groups: “immigrant population of Moroccan origin” and “native-born population”.19,28
Symptoms of psychosis were assessed on hospital admission and discharge, using the Positive and Negative Syndrome Scale (PANSS) validated into Spanish29 and depressive symptoms were assessed using the Calgary depression scale (CDS) in schizophrenia in its Spanish version.30 Functioning on admission was assessed using the functioning assessment short test (FAST)―in its Spanish version31―and on discharge using the Global Assessment Functioning Scale (GAF). FAST scoring is inversely proportional to the level of functioning.
The duration of untreated psychosis, DUP, was obtained from the patients’ clinical records. Information on medication was obtained from the discharge report and the doses on discharge were used, as in a previous study.32 The antipsychotic dose was converted into equivalent to doses of chlorpromazine (in mg/day)33 and injectable antipsychotic drug doses were converted using the method of the minimum effective dose.34 We assessed the presence of secondary effects using the UKU.35
Stressful life events during the previous 6 months were assessed using the Holmes-Rahe Social Readjustment Scale (HR),36 which is validated into Spanish.37 The HR is a scale which was initially developed to explore the relationship between social adjustment, stress and susceptibility to developing disease and includes 43 life events. From this scale the number of life event variables was obtained.
Substance consumption was assessed by urine analysis on hospital admission. To assess the frequency of cannabis consumption detailed questions regarding the last 6 months were asked. Cannabis use was defined as “occasional consumption up to 5 joints weekly”, because the importance of high consumption has been described in onset of psychosis.38,39
Statistical analysisInitially the characteristics of the 2 groups were compared using the Student’s t-test or the Mann-Whitney U test for continuous variables and with the χ2 with Yates correction of the Fisher test for categorical variables. After this binary logistical regression analysis was used to test the magnitude of associations found in univariate analysis. As a result, the group was included as a dependent variable (0 = native-born origin, 1 = Moroccan origin) and all variables with a significance level of p<.10 were included as independent variables in the univariate analysis. The interactions of the included variables were tested against sex and cannabis usage, including those that were significant. To avoid inter-correlational problems correlation analysis was conducted between the continuous variables, with a correlation coefficient of >.70 being considered high. Significance was fixed at p<.05 and the odds ratio (OR) and confidence intervals (CI) were calculated to determine the contribution of each variable.
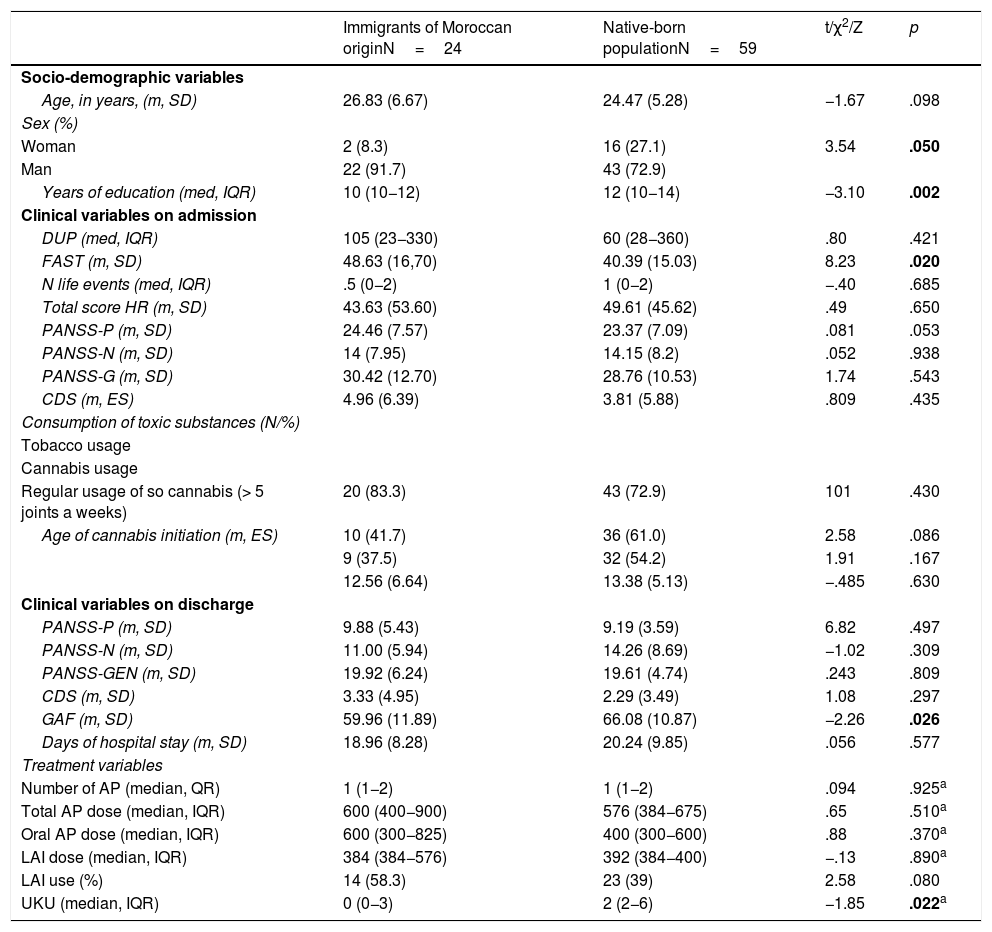
ResultsTwenty eight point nine per cent of the sample were immigrants of Moroccan origin. Table 1 contains the comparison between patients who were of Moroccan origin and the native-born population. In the population of Moroccan origin there was a lower proportion of females (χ2=3.54; p=.05) and fewer years of education (Z=−3.10; p=.002). We found there to be a lower use of cannabis (41.7% compared with 61% of the native-born population), which did not become significant, but a tendency did appear (χ2=2.58; p=.86). No differences were described regarding the severity of the clinical variables. With regard to functionality, those of Moroccan origin presented with higher scores in the FAST on admission (t=8.23; p=.02) and lower GAF on discharge (t=−2.26; p=.02). We did not find any differences regarding the total treatment dose, but there was a tendency in LAI prescription in the Moroccans (χ2=2.58; p=.80) and lower scores in the UKU (Z=−1.85; p=.02).
Comparison of the socio-demographic and clinical characteristics of patients of Moroccan origin with native-born patients.
| Immigrants of Moroccan originN=24 | Native-born populationN=59 | t/χ2/Z | p | |
|---|---|---|---|---|
| Socio-demographic variables | ||||
| Age, in years, (m, SD) | 26.83 (6.67) | 24.47 (5.28) | −1.67 | .098 |
| Sex (%) | ||||
| Woman | 2 (8.3) | 16 (27.1) | 3.54 | .050 |
| Man | 22 (91.7) | 43 (72.9) | ||
| Years of education (med, IQR) | 10 (10−12) | 12 (10−14) | −3.10 | .002 |
| Clinical variables on admission | ||||
| DUP (med, IQR) | 105 (23−330) | 60 (28−360) | .80 | .421 |
| FAST (m, SD) | 48.63 (16,70) | 40.39 (15.03) | 8.23 | .020 |
| N life events (med, IQR) | .5 (0−2) | 1 (0−2) | −.40 | .685 |
| Total score HR (m, SD) | 43.63 (53.60) | 49.61 (45.62) | .49 | .650 |
| PANSS-P (m, SD) | 24.46 (7.57) | 23.37 (7.09) | .081 | .053 |
| PANSS-N (m, SD) | 14 (7.95) | 14.15 (8.2) | .052 | .938 |
| PANSS-G (m, SD) | 30.42 (12.70) | 28.76 (10.53) | 1.74 | .543 |
| CDS (m, ES) | 4.96 (6.39) | 3.81 (5.88) | .809 | .435 |
| Consumption of toxic substances (N/%) | ||||
| Tobacco usage | ||||
| Cannabis usage | ||||
| Regular usage of so cannabis (> 5 joints a weeks) | 20 (83.3) | 43 (72.9) | 101 | .430 |
| Age of cannabis initiation (m, ES) | 10 (41.7) | 36 (61.0) | 2.58 | .086 |
| 9 (37.5) | 32 (54.2) | 1.91 | .167 | |
| 12.56 (6.64) | 13.38 (5.13) | −.485 | .630 | |
| Clinical variables on discharge | ||||
| PANSS-P (m, SD) | 9.88 (5.43) | 9.19 (3.59) | 6.82 | .497 |
| PANSS-N (m, SD) | 11.00 (5.94) | 14.26 (8.69) | −1.02 | .309 |
| PANSS-GEN (m, SD) | 19.92 (6.24) | 19.61 (4.74) | .243 | .809 |
| CDS (m, SD) | 3.33 (4.95) | 2.29 (3.49) | 1.08 | .297 |
| GAF (m, SD) | 59.96 (11.89) | 66.08 (10.87) | −2.26 | .026 |
| Days of hospital stay (m, SD) | 18.96 (8.28) | 20.24 (9.85) | .056 | .577 |
| Treatment variables | ||||
| Number of AP (median, QR) | 1 (1−2) | 1 (1−2) | .094 | .925a |
| Total AP dose (median, IQR) | 600 (400−900) | 576 (384−675) | .65 | .510a |
| Oral AP dose (median, IQR) | 600 (300−825) | 400 (300−600) | .88 | .370a |
| LAI dose (median, IQR) | 384 (384−576) | 392 (384−400) | −.13 | .890a |
| LAI use (%) | 14 (58.3) | 23 (39) | 2.58 | .080 |
| UKU (median, IQR) | 0 (0−3) | 2 (2−6) | −1.85 | .022a |
CDS: Calgary Depression Scale; SD: standard deviation; Oral AP dose: total dose of antipsychotics equivalent to chlorpromazine; DUP: duration of untreated psychosis; FAST: Functioning assessment short test; GAF: Global Assessment Functioning Scale ; HR: Holmes Rahe; IQR: interquartile range; LAI: long acting injectable; PANSS: Positive and Negative Syndrome Scale; UKU: antipsychotic side effect scale.
In bold if the level of significance <0.05.
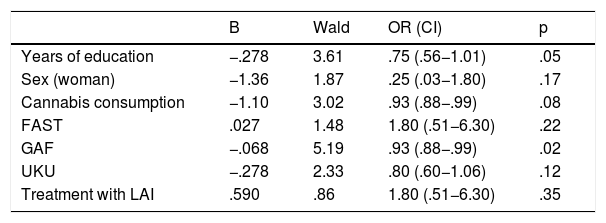
Table 2 shows the results after multivariate analysis. Gender, cannabis consumption, treatment with LAI, years of education, FAST, UKU and GAF are included as independent variables. We found no >.70 correlations between the continuous variables and they were therefore all included in the analysis. Interactions were tested between the different variables without finding any statistically significant interaction. Lastly, the results which were statistically significantly associated with being of Moroccan origin were: fewer years in education (OR 0.75; 95% CI: .56−1.01; p=.05), lower GAF (OR 0.93; 95% CI: .88−.99; p=.02) and a tendency towards a lower cannabis consumption (OR 0.93; 95% CI: .88−.99; p=.08).
Logistic regression model.
| B | Wald | OR (CI) | p | |
|---|---|---|---|---|
| Years of education | −.278 | 3.61 | .75 (.56−1.01) | .05 |
| Sex (woman) | −1.36 | 1.87 | .25 (.03−1.80) | .17 |
| Cannabis consumption | −1.10 | 3.02 | .93 (.88−.99) | .08 |
| FAST | .027 | 1.48 | 1.80 (.51−6.30) | .22 |
| GAF | −.068 | 5.19 | .93 (.88−.99) | .02 |
| UKU | −.278 | 2.33 | .80 (.60−1.06) | .12 |
| Treatment with LAI | .590 | .86 | 1.80 (.51−6.30) | .35 |
Dependent variable, being an immigrant of Moroccan origin.
FAST: Functioning assessment short test; GAF: Global Assessment Functioning Scale; CI: confidence interval; LAI: long acting injectable; OR: odds ratio; UKU: antipsychotic side effect scale.
The main findings from our study are a greater prevalence of men and fewer years of education in the group of immigrants of Moroccan origin compared to the native-born population. There were no differences regarding the intensity of symptoms but the group of Moroccan origin did have poorer functioning and a lower tendency of cannabis usage. In turn, we found there was greater use of LAI, but with a lower profile of side effects in the Moroccan population. Up until now, this is the first study to focus on the ethnic differences in patients with FEP in Spain.
The distribution of ethnicities in our region is similar to that represented by studies in the Netherlands, where the main immigrant ethnicity is Moroccan.23,40 The differences of gender described in the Moroccan ethnicity (8.3% women; p<.05) has also been described in previous studies, which show that the risk of suffering from a psychotic episode is greater in males.41
We found that the Moroccan population were in education for fewer years but the figures should be regarded with caution since education systems differ in each country, as described in a recent study conducted in Norway on the immigrant population and the probability of admission into the general hospital.42
With regard to clinical differences, we found there were no differences in the DUP, the psychotic symptoms or the depressive symptoms in the 2 groups. In contrast, a longer DUP had previously been described in immigrant patients of diverse origins,20,22 although the need for further studies to validate these findings was highlighted.
The prevalence of cannabis usage of the sample is high (53%), but similar to that found in studies with FEP samples.43,44 However, in keeping with previous studies, we found there to be a lower prevalence of cannabis consumption in the immigrant population. This concept is clearly stigmatised by our society, which erroneously considers the Moroccan population to be the main consumer.19,28
We found there to be no significant differences in the number of life events, which is at variance with previous studies.3 One possible explanation to our finding would be that the HR only assesses life events from the last 6 months. The migratory process and belonging to a different culture hinder comparison between groups even further, which would promote stress leading to the onset of psychosis or some other psychopathology.13
Regarding patient functioning, we found there was poorer functioning in the Moroccan population both before hospital admission and on discharge. Being female has already been described as a predictor of good functioning both prior to the disorder and during the course of it,45 although our Moroccan sample lacked women. However, in the logistic regression model controlling gender, the GAF remained lower as a significant variable of the Moroccan origin population.
No differences were present in the total antipsychotic drug doses, but there was a tendency for higher prescription of LAI in the Moroccan population. Regarding total doses of antipsychotic drugs, lower exposure was described in the immigrant population, particularly in Moroccan women in a previous study in Spain.25 Our findings coincided with the latest studies which have compared antipsychotic doses in immigrant populations.46,47 In the Connoly and Taylor46 study, conducted in United Kingdom, distinction was made between patients of black and white races, whilst in that of Hassan et al.,47 distinction was made between white Caucasian Europeans and non Europeans. There is a wide variation of origin grouping, although further research into pharmacological doses is required.13 Regarding the use of the LAI, there has been a tendency for higher use in Moroccan ethnicity. This coincides with Das-Munshi et al.17 in a study conducted in the United Kingdom which describes higher prescription of injectables in patients of minority ethnicity. On occasions, the LAI may be considered as an imposed treatment, which is periodically administered, without much consideration for the patient’s will. Other previous studies have already described that belonging to a minority ethnicity increases the risk of receiving an obligatory community treatment.9,48
The side effect profile with UKU is poorer in the Spanish population. No evidence has been described on the side effects in the Moroccan population but in a recent work on adverse effects a higher side effect profile was reported in women. In our sample there were very few women.49
Study limitations and advantagesThe main limitation was the difficulty posed by a cross-sectional design where causality was not possible to establish. Also, due to the relatively small sample size, with few women, it was not possible to make sub-groups, and studies with larger samples are required to confirm these differences. Furthermore, the sample was taken in a hospitalisation unit and therefore did not include any patients who had never been hospitalised and among whom more women would probably have been present. It was also not possible to include the socio-economic level of the groups nor assess this difference.
Regarding PANSS, we were not able to undertake a sub-analysis of the items, since the small size of the sample limited this aspect, and we were unable to distinguish between whether any symptoms were more prevalent in any group.50 Another limitation of our study was the lack of cultural mediators in the interviews with the Moroccan population, who could have lowered the language barrier and improved clinical uptake.
Despite the small sample size, the study was conducted systematically and phenotyping of the patients was accurately undertaken with the appropriate tools. Also, unlike other previous studies with a multi-ethnic focus, we used only the immigrant population of Moroccan origin and compared it with the native-born population.
ConclusionsAlmost 30% of our sample was of Moroccan origin, with socio-demographic and functioning differences between the Moroccan population and the Spanish population.
Today’s Spain, which is evolving towards an increasingly multicultural society, should consider the essential nature cultural competence in introducing interventions to help palliate the difficulties it faces regarding cultural and ethnic differences. On consideration of our findings, social measures for helping immigration in early intervention programmes in early psychosis should be designed, similarly to those already present in the United Kingdom.
FinancingThis research study did not receive any specific grants from public sector, commercial or non-profit making agencies.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Arranz S, Camacho J, Andrés C, Niubó I, Sanchez Gistau V. Diferencias en la presentación clínica de primeros episodios psicóticos entre población de origen marroquí y población autóctona. Rev Psiquiatr Salud Ment (Barc.). 2019. https://doi.org/10.1016/j.rpsm.2019.03.004