Little is known about the role of coping in relation to suicidal risk in adolescents with Adjustment Disorder (AD). The present study aimed to assess the relation between suicidal ideation and intention and coping strategies in a clinical sample of adolescents with AD, paying special attention to gender differences.
Material and methodSelf-reported questionnaires about suicidal ideation and intention and coping strategies were administered to 108 adolescents with an AD diagnosis.
ResultsCompared with the normative population, adolescents with an AD diagnosis made more use of Acceptance-Resignation (an avoidance-type coping strategy) and less use of Positive Reappraisal (an approach-type coping strategy). Nevertheless, gender introduced some peculiarities. A relationship was observed between the use of certain coping strategies and suicidal ideation and intention, but with notable differences depending on gender: significant and high correlations were found between these two variables in AD boys, both in the total approach score (r=.53, p<.01) and in the total avoidant score (r=.60, p<.01), with coping strategies explaining 41% of suicidal ideation and intention; in girls, in contrast, the only significant relationship was with an avoidant strategy, Emotional Discharge (r=.25, p<.05), although it had low explanatory power.
ConclusionsCoping strategies must be taken into consideration when assessing and treating adolescents with AD at risk of suicide, especially in the case of boys. The absence of association between coping strategies and suicidal risk in girls is discussed, and some therapeutic proposals are presented.
Existe escasa información sobre la función del afrontamiento en relación con el riesgo suicida en adolescentes con trastorno adaptativo (TA). El presente estudio analiza la relación entre la ideación e intencionalidad suicida y las estrategias de afrontamiento en una muestra clínica de adolescentes con TA, enfatizando diferencias de género.
Material y métodoSe aplicaron cuestionarios autoinformados sobre ideación suicida y sobre estrategias de afrontamiento a 108 adolescentes con diagnóstico de TA.
ResultadosEn comparación con la población normativa, los adolescentes diagnosticados con TA utilizaron en mayor medida la aceptación-resignación (una estrategia de tipo evitativo) y menos la reevaluación positiva (una estrategia de aproximación). Sin embargo, el género introdujo algunas peculiaridades. Se detectó relación entre el uso de algunas estrategias de afrontamiento y la ideación e intencionalidad suicida, pero con importantes diferencias dependiendo del género: en los chicos con TA se encontraron correlaciones altas y significativas entre estas dos variables, tanto con el global de estrategias de aproximación (r=0,53; p<0,01) como de evitación (r=0,60; p<0,01), explicando las estrategias de afrontamiento el 41% de la ideación e intencionalidad suicida. Por el contrario, en las chicas con TA la ideación e intencionalidad suicida solo se relaciona con la estrategia evitativa de descarga emocional (r=0,25; p<0,05), que, además, tiene escaso poder explicativo.
ConclusionesEs importante tener en cuenta las estrategias de afrontamiento cuando evaluamos y tratamos adolescentes con TA con riesgo de suicidio, especialmente en los chicos. Se discute la ausencia de asociación entre las estrategias de afrontamiento y el riesgo suicida en las chicas, y se aportan algunas explicaciones, así como propuestas terapéuticas.
Adolescents have to face many challenges in different areas of their life, and in some cases these challenges can lead to the development of psychological symptoms. When psychopathology emerges in response to a psychosocial stressor and interferes with the individual's functionality, the 5th Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) of the American Psychiatric Association (APA1) defines these symptoms as an Adjustment Disorder (AD). The DSM-5 describes Adjustment Disorder as “the presence of emotional or behavioural symptoms in response to an identifiable stressor(s) occurring within 3 months of the onset of the stressor(s)”. In addition to the exposure to one or more stressors, certain other criteria must be present: (1) the distress experienced is out of proportion to the expected reactions to the stressor, (2) the symptoms must be clinically significant and (3) the distress and impairment are related to the stressor and are not an escalation of an existing mental health disorder or part of normal bereavement.
AD is a very common diagnosis in clinical and hospital psychiatric consultation settings, often 50% of cases. In outpatients the incidence ranges from 5% to 20%.1 Other studies have shown that about 30% of young psychiatric inpatients2 and outpatients3 are diagnosed with AD. In the Spanish context, 20% of adolescent mental health outpatients receive an AD diagnosis.4
Numerous studies have established the relationship between AD and suicide risk, since suicidal behaviour (understood as the presence of suicidal thoughts, plans or attempts and the suicide itself5) is linked to an individual's reaction to a stressor or stressors that have triggered the symptom.1,6,7 One fifth of all adolescents who committed suicide could be diagnosed with AD.8 Previous work on almost the same population participating in the current study (Spanish adolescents with AD) established that 27% of girls and 18% of boys presented suicidal ideation (thoughts about intentional self-injury or death) and intention (desire to commit self-harm and suicide).9 A similar percentage (20.6%) was reported in another study10 for Spanish outpatient adolescents. These percentages are higher than those found in Spanish community adolescents (7.4%11 and 6.9%12). Recent studies have shown how the impact of the 2008 economic crisis increased the number of suicides and the use of psychiatric services in young people, including AD patients.13 Thus, it seems important to detect any symptoms of suicide risk in these AD adolescents at an early stage, since suicidal ideation is a frequent precedent of consummated suicide.14,15
AD does not develop without the presence of stress16; it can be considered as an inappropriate response to a stressor, in so far as it interferes with effective coping mechanisms. Therefore, the kind of coping strategies that adolescents deploy is a highly important factor. One of the most widely-accepted definitions of coping is that of Lazarus and Folkman17: “constantly changing cognitive and behavioural efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person” (p. 141). Compas and colleagues18 define coping as the ability to adapt to stress and difficulties, a central goal of human development. Empirical and conceptual research has established the heterogeneity or dimensionality of coping responses, depending on the way in which the individual negotiates the stressful event: either by making constructive attempts to actively manage the stressor, or by attempting to palliate the emotional distress caused. In the first case, terms such as active coping, approach coping, engagement coping, or problem-focused coping are used, and they include strategies such as problem solving, positive reappraisal, logical analysis, seeking information, and so on. In the latter case (attempts to palliate the emotional distress) the terminology used is passive coping, avoidance coping, disengagement coping, or emotion-focused coping. This type of coping includes strategies such as venting feelings, resignation, and seeking rewards.
Studies have shown that certain avoidant and emotion-focused coping strategies are linked with suicidal tendency,7,19–22 with self-harming behaviour,23,24 and self-destructive behaviour in Spanish community adolescents,25 and with non-suicidal self-injury in Chilean community adolescents.26 In contrast, active coping strategies such as hard work and achievement are protective against suicidality.27 But little is known about the coping strategies used by adolescents with AD. It is known that adolescents with a higher level of symptoms tend to use more avoidant strategies and fewer approach strategies when they have to cope with difficulties than adolescents with lower level symptoms.28 Similarly, adult patients tend to apply disengagement strategies more frequently, and humour strategies less frequently, than non-patients.29
Therefore, the appearance and maintenance of symptoms in adolescents with AD be related to an inadequate use of coping strategies. It is particularly interesting to determine which coping strategies are used by adolescents with AD, whether their coping patterns are different from those observed in community adolescents, and whether these patterns are related to an increase in suicidal ideation and intention. This was the purpose of the present study, which had two specific objectives: (1) to study the profile of coping strategies in Spanish AD adolescents according to gender, and to compare it with the coping profile of a normative Spanish adolescent population. Differences between the clinical and normative populations were expected: previous research using populations with a high presence of psychopathology has concluded that young people with a higher level of symptoms tend to use more avoidant strategies and fewer approach strategies when facing difficulties30; (2) to establish, for each gender, both the relationships between coping strategies and suicidal risk in AD adolescents and the explanatory power of coping strategies for suicidal risk. In the light of several previous studies which have shown a relationship between avoidant and emotional coping strategies and suicide symptoms,7,19–21,23 it was expected that this association would be replicated in the current research.
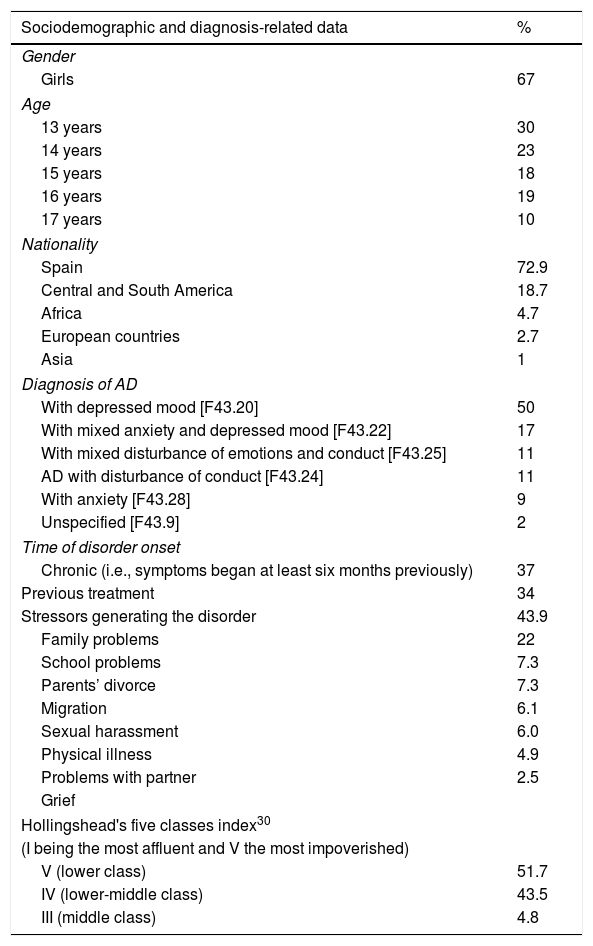
Material and methodParticipantsThe study included 108 adolescents aged 13–17 years old attending a Child and Youth Mental Health Centre in a town near Barcelona (Spain). They were diagnosed with AD according to DSM-5 criteria1 by a clinical psychologist or psychiatrist with at least five years of clinical experience. This centre provides mental health assistance for children and adolescents from 3 to 18 years old referred by paediatric health centres, schools, and social services. Table 1 shows the socio-demographic and diagnosis-related variables.
Socio-demographic and diagnosis related data.
| Sociodemographic and diagnosis-related data | % |
|---|---|
| Gender | |
| Girls | 67 |
| Age | |
| 13 years | 30 |
| 14 years | 23 |
| 15 years | 18 |
| 16 years | 19 |
| 17 years | 10 |
| Nationality | |
| Spain | 72.9 |
| Central and South America | 18.7 |
| Africa | 4.7 |
| European countries | 2.7 |
| Asia | 1 |
| Diagnosis of AD | |
| With depressed mood [F43.20] | 50 |
| With mixed anxiety and depressed mood [F43.22] | 17 |
| With mixed disturbance of emotions and conduct [F43.25] | 11 |
| AD with disturbance of conduct [F43.24] | 11 |
| With anxiety [F43.28] | 9 |
| Unspecified [F43.9] | 2 |
| Time of disorder onset | |
| Chronic (i.e., symptoms began at least six months previously) | 37 |
| Previous treatment | 34 |
| Stressors generating the disorder | 43.9 |
| Family problems | 22 |
| School problems | 7.3 |
| Parents’ divorce | 7.3 |
| Migration | 6.1 |
| Sexual harassment | 6.0 |
| Physical illness | 4.9 |
| Problems with partner | 2.5 |
| Grief | |
| Hollingshead's five classes index30 | |
| (I being the most affluent and V the most impoverished) | |
| V (lower class) | 51.7 |
| IV (lower-middle class) | 43.5 |
| III (middle class) | 4.8 |
Consecutive cases were sampled to recruit the participants. Inclusion criteria were the following: (1) AD as the principal diagnosis, (2) age between 13 and 17 years. Exclusion criteria were: (1) inability to properly understand and answer the questionnaires used in the research, due to language, intellectual or sensorial difficulties, and (2) presence of a comorbid bipolar, depressive, psychotic or developmental disorder. The teenagers admitted to the study underwent two assessment sessions with a trained clinical psychologist to determine their psychological characteristics. All families signed an informed consent document authorizing the institution to use their child's assessment and clinical data for scientific purposes. The Ethics Committee of the host institution approved the study, which was conducted in accordance with the Declaration of Helsinki.31
MeasuresPersonal information data sheets and the questionnaires were administered to the participants in a 60-minute individual session. In order to minimize sources of error, all the assessments were carried out by a single Clinical Psychologist trained in psychological assessment. Demographic and clinical data sheets were used to collect information about the adolescent's age, gender, country of birth, educational level, parents’ marital status, parents’ occupational status and educational level, psychiatric diagnosis, type of stressor that triggered the disorder and previous treatment.
To evaluate suicidal risk, the “Inventario de Riesgo Suicida para Adolescentes” (Suicide Risk Inventory for Adolescents – IRISA32) was used. The inventory comprises 50 items scored on a 5-point Likert scale: 1 (“Never/none”), 2 (“rarely/one”), 3 (“sometimes/two”), 4 (“almost always/three”), and 5 (“always/4 or more”). The inventory is organized into three factors: one for Suicidal Ideation and Intention, another for Hopelessness and Depression, and a third for Protective Circumstances. For the purpose of the current study, only the Suicidal Ideation and Intention factor was used. This factor includes 10 items related to suicidal thoughts and behaviour (e.g. “I believe or feel that my death could be a solution to my problems”). Three of these items (25, 49 and 50) are considered critical items, since they are clear indicators of suicide risk, specifically about suicidal ideation (“I have been thinking of committing suicide, of killing myself”), suicide planning (“I have been planning my own death”) and suicide attempts (“I have tried to kill myself by hurting myself, causing myself physical damage, cutting myself, taking pills, asphyxiating myself, or poisoning myself, intentionally and with the purpose of dying)”. For the current study the internal consistency (α=.93) was highly satisfactory and the Cronbach's α for the critical items was .83.
To evaluate coping strategies, the Moos’ Coping Response Inventory-Youth form (CRI-Y33) was used in its Spanish version.34 In the CRI-Y adolescents describe the most important problem they have had to deal with in the last 12 months and score the 48 test items on a 4-point Likert scale (from 0=‘no, not at all’ to 3=‘yes, fairly often’). The 48 items are distributed across eight scales. Four of them assess approach coping strategies: Logical Analysis (e.g. thinking about different ways to deal with the problem), Positive Reappraisal (e.g. trying to see the positive side of the problem), Seeking Guidance and Support (e.g. talking to someone about the problem), and Problem Solving (e.g. deciding how to do away with the problem). The sum of the four scores provides the global score for approach coping. The other four scales, Cognitive Avoidance (e.g. not thinking about the problem), Acceptance-Resignation, (e.g. accepting the problem as it cannot be solved), Seeking Alternative Rewards (e.g. finding new ways to enjoy life), and Emotional Discharge (e.g. crying or yelling to vent feelings) assess avoidance coping strategies, and the sum of their scores gives the global score for avoidance coping. Measurements of the internal consistency of the Spanish version produced Cronbach's alphas of .77 for the approach scale and .72 for the avoidance scale.
Data analysisStatistical analyses were conducted using SPSS (v.23.0). Means, standard deviations, empirical and theoretical ranges were used to characterize the variables of the study. Four ANOVAs were conducted to test the effect of several socio-demographic- and diagnosis-related variables (SES, type of family, type of AD diagnosis [F43.20], [F43.22], [F43.25], [F43.24], [F43.28], [F43.9]) and trigger stressors of AD on the Suicidal Ideation and Intention Scale of IRISA, since they could be acting as confounding variables. Each one of these four variables was introduced as a factor, and the Suicidal Ideation and Intention Scale of IRISA was the dependent variable. To test the effect of age, Pearson correlation was used.
To test the effect of SES, type of family, type of AD diagnosis ([F43.20], [F43.22], [F43.25], [F43.24], [F43.28], [F43.9]) and trigger stressors of AD on coping strategies two sets of four ANOVAs were conducted for each one. In the first set of ANOVAs, the variables cited above were introduced as factors, and the eight coping strategies of CRI-Y were the dependent variables. In the second set of four ANOVAs, the variables cited above were introduced as factors and the global factors of approach and avoidance of CRI-Y were the dependent variables. MANOVAs could not be used, because the criteria regarding the number of participants were not met. To test the effect of age on coping strategies, Pearson correlation was used.
Student's t-test for independent samples was carried out to test significant differences in means between boys and girls regarding both the Suicidal Ideation and Intention scale of IRISA and the coping strategies of CRI-Y, after applying Bonferroni's correction for multiple contrasts (α<.005) and Levene's test for equality of variances. To test the effect size, Cohen's d was used. Student's t-test for independent samples was employed to test significant differences in means between AD and normative samples on the CRI-Y. To test the effect size, Cohen's d was used. To test significant differences within the same group regarding coping strategies, the paired samples test was employed.
Pearson correlations were used to establish associations between the Suicidal Ideation and Intention scale and coping strategies, and linear regressions (stepwise method) to test the explanatory power of the eight coping strategies of CRI-Y (independent variables) for suicidal ideation and intention (dependent variable). Adjusted R2total, Beta constant, adjusted R2partial, standardized β, 95% CI for B, and variance inflation factor (VIF) were calculated.
ResultsCharacterizing the variables of the studyDescriptive statistics for the Suicidal Ideation and Intention scale of IRISA were calculated separately for boys (mean=12.44, SD=5.19; theoretical range=0–50; empirical range=10–38) and girls (mean=20.26, SD=7.95; theoretical range=0–50; empirical range=10–47). Differences between genders were significant (t=6.01, p<.001). The effect of SES, age, type of family, type of AD diagnosis and trigger stressor of AD on the Suicidal Ideation and Intention scale was calculated. Neither SES (FANOVA=1.31, p>.05), age (r=1.9, p>.05), type of family (FANOVA=2.30, p>.05), type of AD diagnosis (FANOVA=.68, p>.05), nor trigger stressor of AD (FANOVA=1.02, p>.05) was significant. Similarly, the use of coping strategies was independent of SES (FANOVA between 2.34, p>.05 for Logical Analysis and F=.62, p>.05 for Cognitive Avoidance), age (r between −.08 and .13, except for Emotional Discharge: r=.24, p<.01), type of family (FANOVA between 2.26, p>.05 for Problem Solving and F=.40, p>.05 for Seeking Rewards), type of AD diagnosis (FANOVA between 1.33, p>.05 for Acceptance-Resignation and F=.37, p>.05 for Logical Analysis) and trigger stressor of AD (FANOVA between 2.34, p>.05 for Logical Analysis and F=.25, p>.05 for Acceptance-Resignation). Therefore, these socio-demographic- and diagnosis-related variables were not taken into account in the calculations.
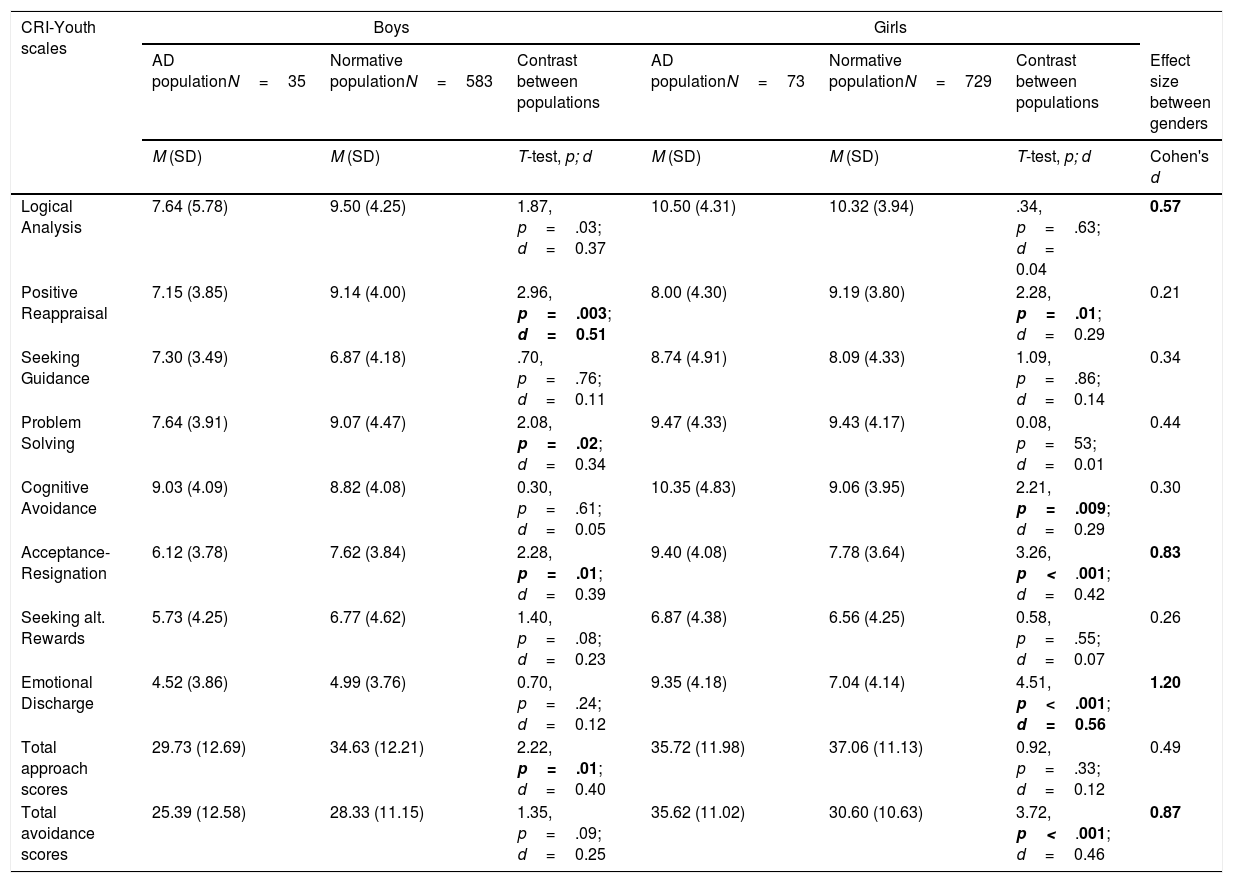
Coping strategies in AD adolescentsMeans and standard deviations on the CRI-Y for girls and for boys in the AD population were calculated and differences between genders were tested (see Table 2). Girls obtained significantly higher mean scores than boys in Acceptance-Resignation (t=3.87, p<.001), Emotional Discharge (t=5.59, p<.001), and in total avoidance scores (t=4.19, p<.001) with high effect sizes (see Table 2). The intra-group comparison indicated that in boys the most frequently used coping strategy was Cognitive Avoidance, which differed significantly from the remaining strategies except for Logical Analysis (p<.01 in all t-tests between related group contrasts). There were no significant differences between the total scores for approach and avoidance coping (p>.05). Among girls, the most used coping strategies were Logical Analysis, Cognitive Avoidance, Problem Solving and Acceptance-Resignation, with no significant differences between them (p>.05 in all t-tests between related group contrasts). There were no significant differences between total scores of approach and avoidance coping (p>.05).
Means, standard deviations (SD) and theoretical range of coping strategies for boys and for girls. Student's t test between clinical adolescents with Adjustment Disorder (AD) and normative Spanish adolescents. Cohen's d effect size between populations and between genders.
| CRI-Youth scales | Boys | Girls | |||||
|---|---|---|---|---|---|---|---|
| AD populationN=35 | Normative populationN=583 | Contrast between populations | AD populationN=73 | Normative populationN=729 | Contrast between populations | Effect size between genders | |
| M (SD) | M (SD) | T-test, p; d | M (SD) | M (SD) | T-test, p; d | Cohen's d | |
| Logical Analysis | 7.64 (5.78) | 9.50 (4.25) | 1.87, p=.03; d=0.37 | 10.50 (4.31) | 10.32 (3.94) | .34, p=.63; d= 0.04 | 0.57 |
| Positive Reappraisal | 7.15 (3.85) | 9.14 (4.00) | 2.96, p=.003; d=0.51 | 8.00 (4.30) | 9.19 (3.80) | 2.28, p=.01; d=0.29 | 0.21 |
| Seeking Guidance | 7.30 (3.49) | 6.87 (4.18) | .70, p=.76; d=0.11 | 8.74 (4.91) | 8.09 (4.33) | 1.09, p=.86; d=0.14 | 0.34 |
| Problem Solving | 7.64 (3.91) | 9.07 (4.47) | 2.08, p=.02; d=0.34 | 9.47 (4.33) | 9.43 (4.17) | 0.08, p=53; d=0.01 | 0.44 |
| Cognitive Avoidance | 9.03 (4.09) | 8.82 (4.08) | 0.30, p=.61; d=0.05 | 10.35 (4.83) | 9.06 (3.95) | 2.21, p=.009; d=0.29 | 0.30 |
| Acceptance-Resignation | 6.12 (3.78) | 7.62 (3.84) | 2.28, p=.01; d=0.39 | 9.40 (4.08) | 7.78 (3.64) | 3.26, p<.001; d=0.42 | 0.83 |
| Seeking alt. Rewards | 5.73 (4.25) | 6.77 (4.62) | 1.40, p=.08; d=0.23 | 6.87 (4.38) | 6.56 (4.25) | 0.58, p=.55; d=0.07 | 0.26 |
| Emotional Discharge | 4.52 (3.86) | 4.99 (3.76) | 0.70, p=.24; d=0.12 | 9.35 (4.18) | 7.04 (4.14) | 4.51, p<.001; d=0.56 | 1.20 |
| Total approach scores | 29.73 (12.69) | 34.63 (12.21) | 2.22, p=.01; d=0.40 | 35.72 (11.98) | 37.06 (11.13) | 0.92, p=.33; d=0.12 | 0.49 |
| Total avoidance scores | 25.39 (12.58) | 28.33 (11.15) | 1.35, p=.09; d=0.25 | 35.62 (11.02) | 30.60 (10.63) | 3.72, p<.001; d=0.46 | 0.87 |
Note: Theoretical range for CRI-Y scales=0–18. Theoretical range for approach and avoidance total scores=0–72. In bold, significant differences and effect size.
Compared with the normative Spanish female sample for the CRI-Y30,31 girls with AD obtained significantly higher mean scores in avoidance strategies, especially Acceptance-Resignation, Cognitive Avoidance and Emotional Discharge, and significantly lower mean scores in Positive Reappraisal. Nevertheless, except for Emotional Discharge, the effect sizes were low. Boys with AD obtained significantly lower mean scores in Positive Reappraisal, Problem Solving, Acceptance-Resignation and in the total approach scale than the normative male population. Nevertheless, except for Positive Reappraisal, the effect sizes were low (see Table 2).
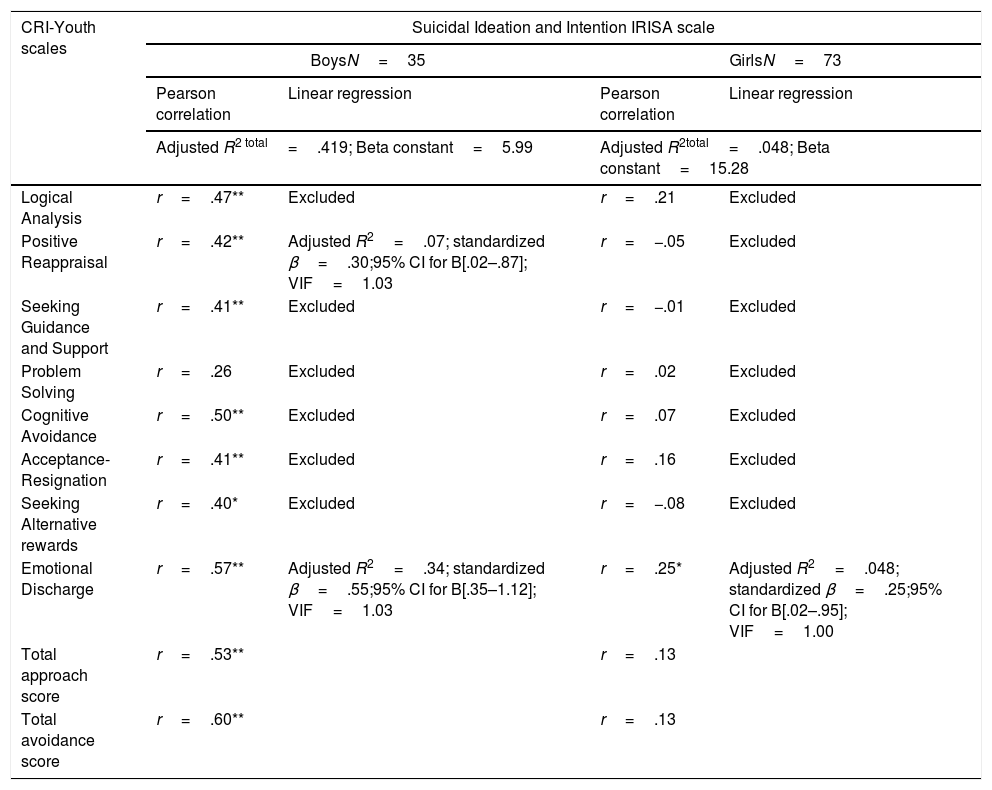
Relationship between coping strategies and Suicidal Ideation and IntentionCorrelations between coping strategies and Suicidal Ideation and Intention scores were conducted for each gender. As can be seen in Table 3, in boys suicidal risk showed positive and significant associations with all coping strategies except for Problem Solving. In boys, the explanatory power of coping reached 41%. The two scales included in the model were Emotional Discharge and Positive Reappraisal. The remaining scales of CRI-Youth were excluded from the regression model. In girls, suicidal risk only showed an association with the Emotional Discharge scale, and its explanatory power was low. The remaining scales of CRI-Youth were excluded from the regression model.
Pearson correlations between IRISA Suicide Ideation and Intention scale and CRI-Y coping strategies in AD sample. Linear Stepwise regression. Adjusted R2total, Beta constant, adjusted R2partial, standardized β, 95% CI for B, and variance inflation factor (VIF).
| CRI-Youth scales | Suicidal Ideation and Intention IRISA scale | |||
|---|---|---|---|---|
| BoysN=35 | GirlsN=73 | |||
| Pearson correlation | Linear regression | Pearson correlation | Linear regression | |
| Adjusted R2 total=.419; Beta constant=5.99 | Adjusted R2total=.048; Beta constant=15.28 | |||
| Logical Analysis | r=.47** | Excluded | r=.21 | Excluded |
| Positive Reappraisal | r=.42** | Adjusted R2=.07; standardized β=.30;95% CI for B[.02–.87]; VIF=1.03 | r=−.05 | Excluded |
| Seeking Guidance and Support | r=.41** | Excluded | r=−.01 | Excluded |
| Problem Solving | r=.26 | Excluded | r=.02 | Excluded |
| Cognitive Avoidance | r=.50** | Excluded | r=.07 | Excluded |
| Acceptance-Resignation | r=.41** | Excluded | r=.16 | Excluded |
| Seeking Alternative rewards | r=.40* | Excluded | r=−.08 | Excluded |
| Emotional Discharge | r=.57** | Adjusted R2=.34; standardized β=.55;95% CI for B[.35–1.12]; VIF=1.03 | r=.25* | Adjusted R2=.048; standardized β=.25;95% CI for B[.02–.95]; VIF=1.00 |
| Total approach score | r=.53** | r=.13 | ||
| Total avoidance score | r=.60** | r=.13 | ||
The aim of the study was to analyze the profile of coping strategies in adolescents diagnosed with AD and its association with suicidal tendencies. Regarding the first objective of this study (to analyze the coping profile in AD adolescents compared with the normative Spanish sample) the most significant features were the diminished capacity in both genders to give a positive sense to their experiences. Furthermore, girls presented a tendency towards passive resignation when faced with negative events, avoiding thinking about the problem, and the venting of emotions. Nevertheless, in general the effect sizes were low; for this reason, the results should not be overestimated. Another peculiarity of the AD sample, compared with the normative Spanish sample, was the negligible difference between the use of approach and avoidance strategies. This phenomenon is uncommon in non-clinical adolescent populations, which tend to prioritize the use of approach strategies over those of avoidance, but has been found in community adolescents with high levels of symptoms.28
Regarding gender differences, girls with AD deployed more coping strategies to face stressors than boys with AD, especially those pertaining to the avoidant type. It might be argued that girls used a larger number of strategies to cope with stressors, although these strategies were not adaptive. Similar results were found by other authors.35
Use of coping strategies and suicidal riskRegarding the second objective of this study, in the literature avoidant strategies have been linked to suicidal risk.6,18,20 However, in the current study there were notable differences regarding gender: In boys suicidal risk showed positive and significant associations with all coping strategies (except for Problem Solving), and coping explained 41% of the suicidal risk; in girls, on the other hand there was hardly any relationship between these two variables, except for Emotional Discharge (crying, shouting, and the venting of feelings) which had only negligible explanatory power. This result is unexpected but it highlights the importance of studying gender independently, in order to be able to make more precise statements. Following Mangnall and Yurkovich36 it might be hypothesized that girls use suicidal ideation, planning, and attempts as a maladaptive coping strategy to deal with the stressful events that have triggered the disease and thus relieve distress. Along the same lines, thinking and planning suicide could be both a way to alleviate the suffering triggered by the stressor and a way to avoid thinking about it and evading the stressor. Training girls in the use of more effective coping strategies may have a protective effect, as some studies have shown that resilient poly-victimized adolescents were more likely to use more positive reappraisal and to seek family support than non-resilient poly-victimized adolescents.37
In the case of boys with AD, there are several possible explanations for the link between Cognitive Avoidance, Acceptance-Resignation and Emotional Discharge and suicide risk. For instance, it might be argued that Acceptance-Resignation reflects a feeling of helplessness that may persuade adolescents that suicide is a valid way to solve their problems. Emotional Discharge is an emotion-focused coping strategy that has been associated in the literature with suicide symptoms in adolescents.20,23 Cognitive avoidance, which has been linked with suicidal risk by other studies,23 can be understood as a denial response to external problems. The link between denial and suicide has previously been noted in the literature.6,38 It could also be hypothesized that adolescents use cognitive avoidance to disengage from external problems but still feel emotional suffering; they may be unable to think of positive solutions and may believe that suicidal behaviour or a suicide attempt is a way to resolve their psychological distress. Furthermore, Pettit and colleagues39 found that the tendency to suppress unwanted thoughts was related to suicide ideation, because, paradoxically, the effort made to suppress painful thoughts merely increases their severity.
An unexpected finding of the current study is that in boys the use of approach coping strategies (specifically Logical Analysis, Positive Reappraisal and Seeking Guidance and Support) was also associated with suicidal ideation and intention. Although the majority of studies associate approach strategies with greater psychological adjustment, the use of approach strategies is not always as beneficial as might be assumed (see Compas et al.,18 and Clarke,40 for a review). In this regard, a relationship between the use of Logical Analysis and both suicidal risk23 and psychopathology28 has been found in previous research. Adolescents who focus on their problems and who are prone to ruminate and analyze their causes may suffer longer episodes of depression than those who adopt distraction strategies. Another explanation for the relation between approach coping strategies and suicidal ideation and intention is based on research findings that emphasize that the use of approach strategies to deal with stressors appraised as uncontrollable can actually increase the level of psychopathology,40 since trying to solve a non-solvable problem can increase the level of stress and frustration on seeing that one's efforts have been futile. One solution to this unmanageable problem might be suicide.
More difficult to explain is the relationship between Positive Reappraisal and suicidal tendencies observed in boys. This strategy, as assessed by CRI-Y, contains items related to believing that things will get better, that things could have been worse, or that the subject's life can change for the better. This type of thinking would be expected to restrain suicidal ideation and attempts. Perhaps in boys with AD psychological suffering can make this inner dialogue more a desideratum than a genuine reappraisal of the situation. One might also conjecture that this relationship indicates the underlying presence of a morbid thought: “things will go better ... because I have thought about taking my life”; “my life will change for the better .. because I have planned my own death”. Perhaps a thorough analysis of the specific items that compose the IRISA ideation/intention scale and their correlations with CRI-Y could shed some light on these results and support this explanation.
The present study has a number of limitations that need to be considered. Firstly, more studies with larger samples should be carried out in order to replicate these results, especially the gender differences that appeared when analysing the relation between suicide and coping strategies. Another limitation is the use of self-inventories to assess the suicide risk, which some studies have questioned.41 It should also be stressed that although the IRISA inventory is a methodologically and clinically sound Spanish-language instrument, no normative population sample is currently available for Spain. Nevertheless, the IRISA has been used by researchers in countries in Central America, and the results of their studies have shown high correlations with the original sample.42 In addition, a previous study using a contrasting group of Spanish community adolescents found the IRISA to be a good instrument for detecting suicide symptoms9 and their relationships with personality patterns.43 Despite these limitations, to our knowledge, this is the first study to have analyzed the relations between coping strategies and suicidal ideation and intention in AD adolescents, and it provides valuable information for the prevention and treatment of suicidal tendencies in this population.
ConclusionGirls with AD reported higher levels of suicidal ideation and intention than boys. Adolescents with AD used more avoidance-type coping strategies than community adolescents. The relationship between coping and suicide in adolescents with AD was influenced by gender: in boys, a strong relationship between coping strategies – both approach and avoidance – and suicidal ideation and intention was observed, with coping strategy explaining 41% of suicidal behaviour. In girls, only the Emotional Discharge strategy was related to suicidal ideation and intention. Suicidal ideation and intention may be a misadjusted coping strategy in itself for girls. There is a clear need to train adolescents with AD to make better use of coping strategies to face the stressor that has triggered their disease.
Funding sourceThis study was partially funded by the Agency for the Management of University and Research Grant (AGAUR) of the Government of Catalonia (2017 SGR-1681).
Conflict of interestNone.