The conceptualization of schizophrenia has changed from its initial conception in the 19th century to the recent publication of the ICD-11. The changes incorporated in this latest version were made based on the evaluation of the current ICD, the available scientific evidence, and the consensus reached by its developers. In this paper we describe the conceptualization changes (diagnostic criteria and specifiers) of ICD-11 schizophrenia with respect to those of ICD-10 and DSM-5. The changes found are discussed based on the scientific literature published in Medline, Scopus and Scielo until July 2019 and the information on the WHO and APA websites. Given that the diagnosis of schizophrenia is based on the diagnostic criteria of the diagnostic classification systems, it is important to know the changes made in its conceptualization and the evidence supporting such modifications.
La conceptualización de la esquizofrenia ha cambiado desde su concepción inicial en el S. XIX hasta la reciente publicación de la CIE-11. Los cambios incorporados en esta última versión se han realizado en base a la evaluación de la CIE vigente, la evidencia científica disponible y los consensos logrados por sus desarrolladores. En el presente trabajo se describen los cambios en la conceptualización (criterios diagnósticos y especificadores) de la esquizofrenia de la CIE-11 respecto a aquella de la CIE-10 y del DSM-5. Los cambios encontrados son discutidos en base a la bibliografía científica publicada en Medline, Scopus y Scielo hasta julio del 2019 y la información de las páginas web de la OMS y la APA. Dado que el diagnóstico de la esquizofrenia se basa en los criterios diagnósticos de los sistemas de clasificación diagnóstica, resulta importante conocer los cambios hechos en su conceptualización y la evidencia que sustenta tales modificaciones.
The diagnostic classification systems, International Classification of Diseases (ICD) developed by the World Health Organisation (WHO) and the Diagnostic Statistical Manual (DSM) developed by the American Psychiatric Association (APA), conceptualise mental psychopathology in mental disorders.1–4 This process defines the set of clinical manifestations specific to each disorder through consensus reached by its developers.5 The ICD and DSM have enabled diagnoses to be made, treatments to be applied and prognoses to be postulated in psychiatry,6,7 but they have not exposed the underlying roots of mental psychopathology.8,9 As a way of addressing this limitation, the National Institute of Mental Health of the United States has proposed the Research Domain Criteria project, which seeks to construct a classification system based on the direct correlation between observed behaviours and findings in neurosciences.10,11 The project classifies mental psychopathology into 5 constructs, which should be studied in 7 units of analysis (e.g., genes, molecules, etc.). Although the primary objective is to provide a framework for research in psychiatry, in the future it is expected that its results will enable the diagnosis and treatment of mental symptoms.12 Therefore, as long as there are no bases for constructing a classification system based on neurobiological findings, the ICD and DSM conceptualisation of mental disorders will remain the classification procedure in psychiatry.13
The conceptualisation of mental disorders specifies the limits, characteristics and content of these clinical entities for use in research, the clinic, statistics and public health.14,15 Conceptualisation is a continuous process carried out with each publication of the diagnostic classification systems based on the available scientific evidence,16 assessment of the classification systems in force17,18 and consensus reached by those responsible for their development.19 Thus, the conceptualisation of mental disorders has varied through the 5 versions of the ICD and the 6 versions of the DSM in seeking an adequate description of these clinical entities.20,21 In the different versions of the diagnostic classification system, schizophrenia has been a main diagnostic category22 and its conceptualisation, started even before the publication of the first versions of these classification systems, has seen conceptual changes over time and between both classification systems.
The notion of schizophrenia started to be forged at the end of the 19th century by distinguished European psychiatrists.16 However, its current concept was developed by Emil Kraepelin, who formulated the concept of early dementia and highlighted as characteristics of the disorder onset in youth, progressive course and poor clinical outcome.16,23 Eugen Bleuler called Kraepelin’s early dementia schizophrenia, under the assumption that this disorder was due to a split in the psyche of a person, and indicated that the most important characteristic was the fundamental symptoms (negative symptoms).16,24 Kurt Schneider, for his part, indicated that the main defect in the disorder was due to impaired empathic communication and considered the first-rank symptoms (positive symptoms) the most relevant manifestations.3,25,26 Based on these concepts, the different versions of the classification systems have incorporated, to a greater or lesser extent, Kraepelin’s chronicity, Bleuler’s negative symptoms and Schneider’s first rank symptoms with the construct of schizophrenia.3,22,25,27
The conceptualisation of schizophrenia has also varied between the ICD and the DSM. The initial versions of both systems conceptualised schizophrenia under a clinical description of psychodynamic approach.28 Then, while the DSM-II (1968) conceptualised schizophrenia as the "loss of ego boundaries" based on the dominant Bleuler approach in the United States,16 the ICD-8 (1967) conceptualised the disorder based on positive symptoms, chronicity and poor clinical outcomes supported by the perspective of Schneider and Kraepelin that prevailed in the rest of the world.16 Differences in the conceptualisation of the disease led to problems in diagnosis, which was evidenced in a study that showed that patients in the United States were twice as likely to be diagnosed with schizophrenia as in London.29 The DSM-III (1980) then introduced a diagnostic system based on explicit criteria, which facilitated diagnosis and brought about the widespread use of classification systems in clinical practice and research.16,30 The latest versions of the ICD (ICD-10) and the DSM (DSM-IV and DSM-5) share greater similarity in the conceptualisation of schizophrenia.3,16
ICD-11, published in June 2018, has introduced a series of changes in the conceptualisation of schizophrenia with respect to those of ICD-10 and DSM-5.1,2,31 The changes were made in order to improve the clinical utility of the disorder,17,32,33 or to make the ICD-11 criteria similar to those of DSM-5.34 The changes have an empirical basis or, by contrast, the criteria have been maintained because no reason has been found to justify their being modified. The aim of the paper is to describe the changes made in the conceptualisation of schizophrenia in ICD-11 in relation to that of ICD-10 and DSM-5, and to show the evidence that supports these modifications.
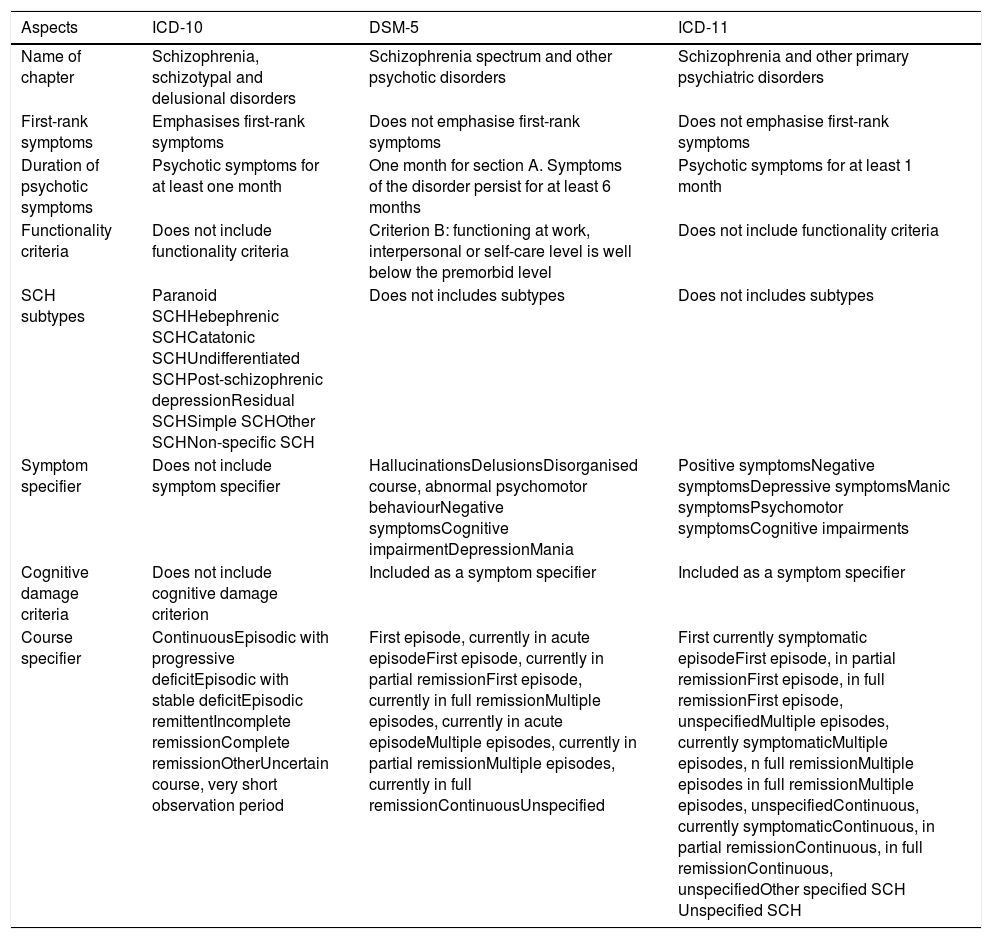
MethodologyWe reviewed the diagnostic classification systems: ICD-11, ICD-10 and DSM-5,1,2,31 and compared the conceptualisation (diagnostic criteria and specifiers) of schizophrenia of ICD-11 (2018) with that of ICD-10 (1992) and that of DSM-5 (2013). The diagnostic criteria define and delimit the disorder, while the specifiers characterise it according to its course, severity and form of presentation. The differences found between the diagnostic classification systems are discussed based on the scientific evidence available in Medline, Scopus and Scielo published up to July 2019. This data was collected through search strategies using a combination of the terms: International Classification of Diseases, ICD, ICD-11, ICD-10, Diagnostic Statistical Manual, DSM, DSM-5, psychiatric nosology, schizophrenia and psychosis, that were entered into the search engine of each of these virtual libraries. The Scielo search was performed with the same terms translated into Spanish. In addition, the WHO and APA web pages were reviewed to collect information on the development of ICD-11 and DSM-5, respectively.35,36 The differences found between ICD-11, ICD-10 and DSM-5 are shown in Table 1.
Comparison between diagnostic classification systems.
| Aspects | ICD-10 | DSM-5 | ICD-11 |
|---|---|---|---|
| Name of chapter | Schizophrenia, schizotypal and delusional disorders | Schizophrenia spectrum and other psychotic disorders | Schizophrenia and other primary psychiatric disorders |
| First-rank symptoms | Emphasises first-rank symptoms | Does not emphasise first-rank symptoms | Does not emphasise first-rank symptoms |
| Duration of psychotic symptoms | Psychotic symptoms for at least one month | One month for section A. Symptoms of the disorder persist for at least 6 months | Psychotic symptoms for at least 1 month |
| Functionality criteria | Does not include functionality criteria | Criterion B: functioning at work, interpersonal or self-care level is well below the premorbid level | Does not include functionality criteria |
| SCH subtypes | Paranoid SCHHebephrenic SCHCatatonic SCHUndifferentiated SCHPost-schizophrenic depressionResidual SCHSimple SCHOther SCHNon-specific SCH | Does not includes subtypes | Does not includes subtypes |
| Symptom specifier | Does not include symptom specifier | HallucinationsDelusionsDisorganised course, abnormal psychomotor behaviourNegative symptomsCognitive impairmentDepressionMania | Positive symptomsNegative symptomsDepressive symptomsManic symptomsPsychomotor symptomsCognitive impairments |
| Cognitive damage criteria | Does not include cognitive damage criterion | Included as a symptom specifier | Included as a symptom specifier |
| Course specifier | ContinuousEpisodic with progressive deficitEpisodic with stable deficitEpisodic remittentIncomplete remissionComplete remissionOtherUncertain course, very short observation period | First episode, currently in acute episodeFirst episode, currently in partial remissionFirst episode, currently in full remissionMultiple episodes, currently in acute episodeMultiple episodes, currently in partial remissionMultiple episodes, currently in full remissionContinuousUnspecified | First currently symptomatic episodeFirst episode, in partial remissionFirst episode, in full remissionFirst episode, unspecifiedMultiple episodes, currently symptomaticMultiple episodes, n full remissionMultiple episodes in full remissionMultiple episodes, unspecifiedContinuous, currently symptomaticContinuous, in partial remissionContinuous, in full remissionContinuous, unspecifiedOther specified SCH Unspecified SCH |
SCH: schizophrenia.
The ICD, the standard health information system for mortality and morbidity statistics worldwide, defines the universe of diseases, disorders, injuries and other health-related conditions. The ICD is used in clinical and research settings to define diseases and study their patterns, as well as in health service management to monitor outcomes and allocate resources.35 ICD-11 was published after 25 years, which is the longest time for a version of the ICD to be developed.37,38 The project started in 1999 and for 14 years hundreds of experts around the world contributed to creating a new version through an electronic review process that received over 10,000 review proposals.39–41 ICD-11 was designed to be used in different areas of health and related fields, and therefore it is easy to use, uses clear language and allows for decision-making.42 WHO member states meeting at the World Health Assembly adopted ICD-11 in May 2019, and therefore this new ICD version will come into effect in January 2022.43
The chapter on mental and behavioural disorders of ICD-11 was developed by the WHO Department of Mental Health and Substance Abuse.17,37,44 The department oversaw that changes to the diagnostic criteria were made through a multidisciplinary, transparent and multilingual process, while remaining as free as possible from conflict of interest.37 The department conducted a comprehensive and systematic programme of field studies in clinical settings and via the Internet, which evaluated the diagnostic criteria for mental disorders (Clinical description and diagnostic guidelines).17,41,44 These studies were conducted in countries with different languages and different income levels to extensively investigate the reliability and clinical utility of the diagnostic criteria.18,44–46 The chapter on psychotic disorders in ICD-11 was developed by the Working group on the Classification of Psychotic Disorders, in charge of reviewing the scientific evidence and developing the diagnostic proposals that were finally included in ICD-11.37
ICD-11 describes psychotic disorders in the block "Schizophrenia spectrum and other primary psychiatric disorders". The block includes schizophrenia, schizoaffective disorder, schizotypal disorder, acute and transient psychotic disorder, delusional disorder and other specified schizophrenias or other primary psychotic disorders. These disorders are characterised by impaired assessment of reality and behaviour, and by the presence of positive symptoms (delusions, hallucinations, disorganised thinking and behaviour, and experiences of passivity and control), negative symptoms (flattened or suppressed affect) and psychomotor disturbances.31 The diagnosis of schizophrenia, in particular, is based on the presence of disorders in thought, perception, experience of self, cognition, volition, affect and behaviour, which must have persisted for at least one month. Psychomotor disturbances such as catatonia may also be present. Symptoms must not be a manifestation of another health condition or of substance or medication use.31
Comparison between the ICD-11 and the ICD-10Conceptual comparisonThe ICD-11 made a change to the ICD-10 diagnostic criteria for schizophrenia. The change involved removing the preponderance of Schneider's first-rank symptoms from ICD-10 (bizarre delusion or first-rank hallucination). Kurt Schneider considered the first-rank symptoms important for the diagnosis of schizophrenia, therefore he termed them "first-rank", but he never considered them sufficient or necessary.47 ICD-10 gave almost pathognomonic value to these clinical manifestations,47,48 in considering that the presence of a single symptom was sufficient to make a diagnosis of schizophrenia.1 The decision to remove the preponderance of first-rank symptoms was made fundamentally because of the evidence showing their low specificity in differentiating schizophrenia from other non-affective psychoses48,49 and from affective psychoses.47,50 With this change, ICD-11 values first-rank symptoms equally with hallucinations and delusions of any kind as diagnostic criteria for schizophrenia.31
Comparison in descriptionICD-11 made 3 changes in the characterisation of schizophrenia from ICD-10. ICD-11 removed the subtypes of schizophrenia from ICD-10 that had been proposed as a way of capturing the clinical heterogeneity of the disorder.31 These categories, created based on the combination of symptoms, were not natural clinical entities, just symptomatic constructs that provided some information on the clinical picture.51 In clinical practice, the subtypes of schizophrenia had low diagnostic stability in longitudinal assessments52,53 and the overlap of symptoms between the different subtypes of schizophrenia (symptoms of disorganisation in catatonic schizophrenia) and with mood disorders and other medical conditions (catatonia).51,54 In addition, these categories did not allow for a description of the different and independent clinical presentation of psychotic and mood components of the disorder.22 In this regard, removing the subtypes of schizophrenia in ICD-11 could result in a simplified clinical description of the disorder.22
ICD-11 has introduced a symptom specifier to replace the subtypes of schizophrenia.31 The specifier records information on the presence or absence of symptoms, their longitudinal course, response to treatment and prognosis in the disorder.22 The specifier must be constantly assessed throughout the course of the disease as the severity of clinical manifestations varies between patients and in the same patient at different times.22 The specifier categories include positive, negative, depressive, manic, psychomotor and cognitive deficits.34,55,56 Although cognitive deficit was not considered a core symptom of schizophrenia, its inclusion as a specifier was based on its role in the psychosocial and functional recovery of patients.34 These symptoms are assessed individually on a scale from zero (absent) to 4 (severe).55 The symptom specifier, compared to the subtypes of schizophrenia, could allow for more accurate and dynamic capture of the different symptoms of schizophrenia.22
ICD-11 modified the ICD-10 schizophrenia course specifier. The course of the disorder in ICD-10 was divided into continuous, episodic (with progressive or stable deficit and remitting), remission (complete and incomplete), other and uncertain course.1 These specifiers were changed in ICD-11 to the following categories: first episode, multiple episodes, continuous course and unspecified, where the first 3 categories allow for specifying whether the patient is presenting with an acute episode, partial or total remission of symptoms of whether it is unspecified.31 The most relevant innovation of the course specifier is the incorporation of the “first episode” category, which will enable better registration in health systems of patients who started with psychotic symptoms and better longitudinal study of the disorder from its initial stages. The introduction of this category in ICD-11 is related to the global interest in the study of psychotic disorders from their early stages in recent decades.57–59 Thus, the ICD-11 course specifier offers a more complete system for describing the different courses that schizophrenia can take.
Comparison between ICD-11 and DSM-5Conceptual comparisonICD-11 and DSM-5 made a similar change in the diagnostic criteria for schizophrenia. The change consisted of the removal of Schneider's first-rank symptoms from the diagnostic criteria of schizophrenia by both systems.3,34 DSM-IV required only one bizarre delusion or first-rank auditory hallucination to meet criterion A of the diagnostic criteria. 60 DSM-5 eliminated this criterion and therefore, in this version of the DSM, any type of delusion or hallucination has the same diagnostic value.3 This decision was based on the studies that showed the low specificity of bizarre delusions and the difficulty in distinguishing between bizarre and non-bizarre delusions,61,62 and on the papers that showed that first-rank auditory hallucinations were of variable reliability, poor prognostic value, low specificity and inconsistent frequency.62 Given that less than 2% of patients were diagnosed with schizophrenia based on first-rank symptoms, this change is not expected to have a major impact on diagnosis.62
ICD-11 presents 2 differences in the diagnostic criteria of schizophrenia with DSM-5. Although ICD-11 and DSM-5 require that psychotic symptoms last at least one month to make the diagnosis of schizophrenia,2,31 DSM-5 additionally requires that these symptoms along with prodromal or residual symptoms be present for 6 months.2,42 It has been pointed out that there are few studies that have directly investigated the criterion of one month’s duration of psychotic symptoms,63 but that this criterion is maintained in ICD-11 given the high stability of the schizophrenia construct taking this period into account.64 On the other hand, while impaired function is a diagnostic criterion of schizophrenia in DSM-5, it is not considered in ICD-11. The ICD argues that functional deficits do not occur in all people with schizophrenia and are therefore not specific to the disorder.42 In addition, it points out that mental disorders should be defined based on their symptoms and not in relation to activity limitations.17 For its part, the DSM uses a criterion of "clinical significance of damage" as a threshold to identify mental disorders. Therefore, in line with this approach, DSM-5 maintains functional impairment as a diagnostic criterion.37
Comparison in descriptionICD-11 and DSM-5 have made similar changes in the description of schizophrenia. Both systems removed the subtypes of the disorder as they had little clinical utility, low diagnostic stability, no heritability and little influence on treatment.3,42 Similarly, cluster analysis studies have shown that the symptoms of schizophrenia were grouped differently from the subtypes proposed in the DSM.65,66 In clinical practice, only the undifferentiated and paranoid subtypes were used with some frequency, while the other subtypes were rarely used.22 For example, in the United States, the catatonic subtype was only used in diagnosing 1% of Medicaid patients and in 2% of those treated as outpatients.27 These categories were little used in research, noting that only 9.8% of studies published in 1990 and 6.5% in 2010 considered schizophrenia subtypes.67 These findings served to support the removal of the subtypes of schizophrenia from both classification systems.
DSM-5, like ICD-11, incorporated a symptom specifier in the assessment of the clinical manifestations of schizophrenia (delusions, hallucinations, abnormal psychomotor behaviour, disorganised speech and negative symptoms.2 Symptoms have been divided into 8 specifiers: hallucinations, delusions, disorganised speech, abnormal psychomotor behaviour, negative symptoms, cognitive impairment, depression and mania,68 which must be assessed on a scale from 0 (absent) to 4 (severe), described in the chapter “Assessment measures” of section iii of DSM-5.2 The incorporation of the symptom specifier enables the clinical heterogeneity of schizophrenia to be assessed in a valid and clinically useful way.27 In addition, it provides information on the nature of the disease in a particular patient and enables an assessment of the impact of treatment in different aspects of the disorder.69 The incorporation of a symptom specifier common to both DSM-5 and ICD-11 will allow clinical information to be compared between the two classification systems.6
Catatonia, having been removed as a subtype of schizophrenia, was handled similarly by ICD-11 and DSM-5.70 ICD-11 considers that catatonia can be caused by mental disorders (e.g. schizophrenia), psychoactive substances (including medication) and by medical conditions.71 In the first case, catatonia is assessed with the symptom specifier under the category “psychomotor symptoms”37,72 and in the other 2 cases as a secondary presentation.71 DSM-5 considers that catatonia could be due to mental disorders, medical conditions and have an unspecified form.70 Catatonia in schizophrenia is assessed with an independent specifier (“with catatonia”), like the course and symptom specifier.2,27 Catatonia due to medical conditions is a form secondary to a particular health condition and unspecified catatonia is reserved for cases where the underlying cause of the condition is not known.70 The classification of catatonia is not supported by empirical data, therefore it is assigned as a category of the symptom specifier, a symptom specifier or a separate clinical entity by the consensus reached by the ICD and DSM developers.72,73
ICD-11 and DSM-5 have modified the schizophrenia course specifier. DSM-IV included the categories: episodic (with and without residual inter-episodic symptoms), continuous, single episode (partial and complete remission), other unspecified pattern, and less than one year from onset of the first active phase symptoms.60 DSM-5 modified these categories and instead sought to highlight current state and the longitudinal pattern that the disorder could follow. 27 Current state assesses whether the patient is experiencing active symptoms or is in partial or complete remission of symptoms. The longitudinal pattern characterises the disorder as first-episode, multiple-episode, continuous or non-specific.27 The combination of these categories provides a set of different course specifiers that allow clinicians and researchers to document the current state and overall course of a patient's disorder in a given assessment.27 Similar current course specifiers between ICD-11 and DSM-5 will enable a comparison of the different course patterns that schizophrenia could follow between the two classification systems.
DiscussionThe conceptualisation of schizophrenia has evolved from its initial conception in the late 19th century to the recent publication of ICD-11 in 2018. Throughout this period, the definition of the disorder has varied, its boundaries have expanded or narrowed and its diagnostic criteria have been modified.3,16,19 The changes in its conceptualisation are due to the fact that its nature has been little clarified (genetic abnormalities, deregulation of neurotransmitters, anatomical alterations),74,75 which means that to date there is no biological marker that allows an empirical diagnosis.76 This means that the diagnosis of schizophrenia continues to be based on data obtained through clinical observation rather than on biological markers related to brain function or disease.77 In this sense, the conceptualisation of schizophrenia by the ICD and the DSM is of vital importance for study, diagnosis and treatment of the disorder.
ICD-11, like its predecessors, has conceptualised schizophrenia from a categorical approach, following the principles of the biomedical model.6,78,79 The application of this model has enabled the diagnosis and clinical management of chronic psychotic conditions 7; however, it has also shown that conditions of psychosis, included under the construct of schizophrenia, do not present the characteristics of a categorical entity.9,80,81 This is evidenced by the diagnostic problems that arise when assessing cases that jointly present symptoms of psychosis and mood,82 the high comorbidity presented by schizophrenia with other mental disorders83,84 and the difficulties in the diagnosis of sub-threshold psychotic pictures.82 Thus, although schizophrenia is conceptualised as a categorical entity in current diagnostic classification systems, psychotic illness does not appear to possess such a characteristic.82 This has called into question the strict separations between mental disorders (zone of rarity) assumed by the categorical approach9,85 and, therefore, the suitability of this approach for the study of psychotic illness.86
The dimensional approach is an alternative model for the study of schizophrenia.87–89 This approach considers the existence of a quantitative and gradual variation between the different mental disorders and between “normality” and disease.81 The dimensional approach places schizophrenia together with schizoaffective disorder and bipolar disorder with psychotic symptoms within the psychotic spectrum.88,90 Thus, it considers that disorders within this spectrum share several aetiological factors (genetic and environmental)91–93 and that while shared factors explain the development of psychosis, non-shared factors explain the specific symptoms of each disease.87,93 The influence of the dimensional approach on ICD-11 and DSM-5 is observed in the symptom specifier assessment system (severity grading) and in the name of the block on psychotic disorders of DSM-5 (“Schizophrenia spectrum and other primary psychiatric disorders”).22,73 The dimensional approach does not exclude the categorical approach; therefore, the study of schizophrenia is being considered with a hybrid model that combines the categorical and the dimensional approach.81,94 An example of this lies in the clinical staging of schizophrenia that seeks to prevent progression of the disorder to advanced stages or to promote a return to less severe stages or even complete remission.95 To that end, it studies the psychotic illness in a continuum of severity in its different stages (e.g., prodromal phase, first psychotic episode and chronic phase) and proposes specific therapeutic strategies in each.96
The proposed changes in schizophrenia not only relate to its conceptualisation, but also to its name. Different movements made up of health professionals, patients and families have called for a change in the name of the disorder.97,98 These movements argue that the term “schizophrenia” is highly stigmatising and is associated with hopelessness, violence and discrimination.97,99 Therefore, they argue that this name impacts negatively on patients who not only have to live with the symptoms of the disorder, but also with the social pressure caused by the disease.100,101 In this regard, new names have been proposed to replace the name schizophrenia,97 such as “Kraepelin-Bleuler disease”,102 “psychosis susceptibility syndrome”103 and “Bleuler’s disease”.104 These ideas have taken hold in Asian countries that have changed the name of schizophrenia to “integration disorder” (Japan), “attunement disorder” and “dysfunction of thought and perception” (Hong Kong and Taiwan).105 The proposed changes in the approach to the study and naming of schizophrenia are on the agenda for future versions of the ICD and DSM.
In conclusion, ICD-11 conceptualised schizophrenia from a categorical approach and made a change in the diagnostic criteria (removal of Schneider's first-rank symptoms) and 3 changes in the specifiers (removal of schizophrenia subtypes, changes in symptom and course specifiers) with respect to the schizophrenia of ICD-10. Therefore, the nuclear definition of schizophrenia of ICD-10 is maintained in ICD-11, but its description is changed. Furthermore, the ICD-11 definition of schizophrenia was harmonised with that of DSM-5 with the removal of first-rank symptoms,62 but differences remain with regard to duration of symptoms and impaired function. The changes in the specifiers of schizophrenia in ICD-11 are similar to those made by DSM-5 to DSM-IV. One difference in the specifiers is the different management of catatonia, with ICD-11 considering it a symptom specifier category and DSM-5 evaluating it as an independent specifier.72 In general, the changes incorporated in the conceptualisation of schizophrenia of ICD-11 have made it more similar to that of DSM-5.
FundingNo funding has been received for this research from any public agency, commercial or non-profit institution.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Valle R. La esquizofrenia en la CIE-11: comparación con la CIE-10 y el DSM-5. Rev Psiquiatr Salud Ment (Barc.). 2020. https://doi.org/10.1016/j.rpsm.2020.01.001