The increase in vaccine hesitancy threatens advances in public health and causes vaccine-preventable diseases outbreaks in infra-vaccinated communities. This study aims to determine and compare the perception and attitudes towards vaccination among pharmacy users, pharmacy students and community pharmacists.
MethodsA cross-sectional observational study was conducted during March and April 2020, surveying perceptions and attitudes towards vaccination in Barcelona (Spain). Statistical analysis was assessed by chi2 test and multivariate regression. Statistical significance when P<.05. The association measure of Odds Ratio and its 95% confidence interval (CI) were estimated.
ResultsA high percentage of hesitant opinions (44%) among pharmacy users was observed, despite high vaccine coverage (80%). Some showed mistrust in the health system (23.3%) and a statistically significant association was found between previous negative experiences with vaccination and hesitant attitudes (OR: 3.04; 95%CI 1.16 to 7.93; P=.02). Of all surveyed pharmacy users, those over 44 years old showed a stronger hesitant attitude towards vaccines (OR: 2.63; 95%CI 1.11 to 6.19; P=.03), and 40% undervalued influenza vaccine, including risk groups. Both pharmacy students and community pharmacists had a positive attitude towards vaccination. While only 16% of surveyed pharmacists vaccinated against influenza during the 2019/2020 influenza seasonal campaign, most of them considered their vaccination important to the profession (61%).
ConclusionsActive promotion and education of the population and reliable communication on vaccines are some of the needs that community pharmacists can solve, claiming their role as highly qualified health professionals in daily contact with the population.
El aumento de la reticencia vacunal amenaza los avances logrados en salud pública y causa brotes de enfermedades inmunoprevenibles en comunidades infra vacunadas. El objetivo de este estudio es explorar y comparar las actitudes y percepciones hacia la vacunación de los usuarios de farmacia, los estudiantes de farmacia y los farmacéuticos comunitarios.
MétodosSe realizó un estudio observacional transversal mediante encuestas sobre las actitudes hacia la vacunación en la provincia de Barcelona (España) durante marzo-abril de 2020. El análisis estadístico se llevó a cabo mediante la prueba χ2 y una regresión multivariable. El nivel de significación estadística se consideró cuando P<0,05. Como medida de asociación se estimó la Odds Ratio con sus intervalos de confianza al 95%.
ResultadosLos resultados obtenidos muestran un 44% de reticencia en la población a pesar de tener una cobertura vacunal del 80%. Se observó desconfianza en el Sistema de Salud (23,3%) y se asoció experiencia negativa previa con la vacunación y reticencia (OR: 3,04; IC 95% de 1,16 a 7,93; P=0,02). Del total de encuestados, los mayores de 44 años mostraron una principal reticencia a las vacunas (OR: 2,63; IC 95% de 1,11 a 6,19; P=0,03). Un 40% de los encuestados infravaloraron la vacuna antigripal. Los estudiantes de farmacia y los farmacéuticos comunitarios mostraron una actitud positiva hacia la vacunación. Aunque sólo el 14% estaban vacunados contra la gripe, la mayoría consideró que su vacunación es importante.
ConclusionesUna promoción activa, educación poblacional y comunicación especializada sobre vacunas son algunas de las necesidades que el farmacéutico comunitario puede resolver, reafirmado así su papel como profesional de la salud altamente calificado en contacto constante con la población.
In 2019 global vaccine coverage, that is, the proportion of children around the world who had received the recommended vaccines, remained at 85%.1 This great progress, however, has been threatened recently by the increase in vaccine hesitancy (VH), defined by World Health Organization (WHO), as the “delay in the acceptance or refusal of vaccination despite the availability of vaccination services”.2–4 Outbreaks of vaccine preventable diseases have recently been reported in under-vaccinated communities mainly due to this phenomenon.5–9
Hesitant individuals may refuse some vaccines but accept others, delay vaccination, or get vaccinated, even though not being confident. According to the WHO Group of Strategic Advisors (SAGE), VH is characterized by being “complex and context-specific; which varies according to time, place and vaccines. It is influenced by factors such as complacency, convenience and trust”.2
Betsch et al. defined in 2018 two additional factors.10 The calculation, referring to intensive research about vaccines, that may lead an individual to poorly contrasted sources and/or an increased perception of risk. And collective responsibility, defined as the desire to protect other people through their own vaccination. Many interrelated factors at different levels may come also into play as noted by Dubé et al.11
VH has also affected the usually low influenza vaccination coverage.9,10 Due to the possible role as transmitters of the disease, influenza vaccination is recommended not only for people at risk of developing complications from it, but also for individuals in contact with this group, such as health personnel. However, in Catalonia, during the 2018/2019 influenza immunization campaign, only 30% of healthcare professionals (HCPs) got vaccinated.12
HCPs may expose themselves and patients to several vaccine preventable diseases especially during outbreaks or at peak epidemic activity. Furthermore, it is important to reduce absenteeism among HCPs, which can be a threat when there is a high burden of patients needing care.13
Community pharmacists are healthcare personnel in daily contact with their users and thus can also be a two-way transmitter as attending physicians and nurses.14
HCPs influence over their patients could affect vaccination uptake, as reported by Napolitano et al. and Bianco et al.15,16 Therefore, as highly qualified health professionals, community pharmacists could act as an advisor or firewall on those questions or misconceptions about vaccination that may otherwise be neglected and could lead to the omission of vaccination by the patient.16,17
In this study pharmacy students, community pharmacists and their users were surveyed via three questionnaires. The objective was to examine and compare the perception and attitudes towards vaccination among those groups to provide recommendations for vaccine promotion and to evaluate influenza vaccine coverage among community pharmacists.
MethodsA cross-sectional study was conducted between March and April 2020 at the province of Barcelona, Spain. Pharmacy users from this region were invited to participate in the survey, initially, within the facilities collaborating on the study by answering the questionnaire in person, and later, due to mobility restrictions caused by the COVID-19 pandemic, an online questionnaire was spread via a cross-platform messaging application.
The questionnaire was developed following available literature18–22 and translated into Spanish and Catalan. Respondents answered questions about general knowledge and attitudes towards vaccination, beliefs on vaccine safety and efficacy, collective responsibility, risk of newer vaccines, vaccination schedule, sources of information, health system and provider's trust, personal experience, and immunization behaviors.
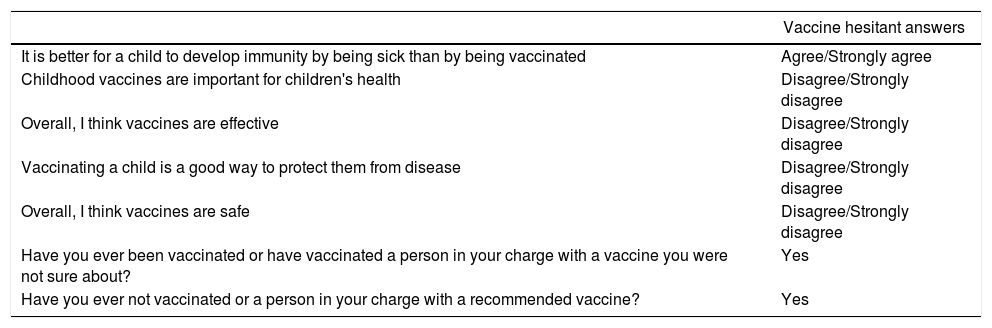
To categorize VH attitudes among pharmacy users and considering WHO definition of VH described above, a set of answers to the questionnaire were considered hesitant (Table 1).
Calculation of VH attitudes among pharmacy users according to their questionnaire answers.
| Vaccine hesitant answers | |
|---|---|
| It is better for a child to develop immunity by being sick than by being vaccinated | Agree/Strongly agree |
| Childhood vaccines are important for children's health | Disagree/Strongly disagree |
| Overall, I think vaccines are effective | Disagree/Strongly disagree |
| Vaccinating a child is a good way to protect them from disease | Disagree/Strongly disagree |
| Overall, I think vaccines are safe | Disagree/Strongly disagree |
| Have you ever been vaccinated or have vaccinated a person in your charge with a vaccine you were not sure about? | Yes |
| Have you ever not vaccinated or a person in your charge with a recommended vaccine? | Yes |
Ninety-one students from the Public Health subject of the pharmacy degree at the University of Barcelona were also surveyed using paper questionnaires. The questionnaire was based on the one created by La Cátedra Balmis de Vacunología at the Universidad de Alicante in 2018, and used by Laguna et al.23 Students answered questions about knowledge on vaccines and which community pharmacists should be vaccinated from, immunization beliefs, sources of information, and perceptions on their current vaccine education.
Another survey was conducted during the same period and in the same location among community pharmacists. They were invited to participate in the survey by sending an explanatory note and the online questionnaire to their corresponding email obtained at their pharmacy's web site. They were also encouraged to spread the questionnaire to other colleagues of Barcelona province to increase the sample.
The questionnaire was developed following available literature24,25 and translated into Catalan. Respondents answered questions about disease susceptibility and severity, vaccine effectiveness and safety, immunization behaviors, sources of information, influenza vaccination coverage and preparedness to give an adequately vaccination advice.
All three surveys were anonymous and written consent was obtained through the online questionnaires and verbal consent before giving the paper questionnaires. No incentive was used to promote any participation. All participants were assured that all information collected would be kept confidential and analyzed anonymously at the start of the questionnaires. In the online questionnaires, participants were not able to continue to the next question if they failed to provide response to an item. No pilot studies were conducted due to time constraints.
A 5% precision and 95% confidence were used on an online-based sample size estimator (https://www.checkmarket.com/sample-size-calculator). For the pharmacy users survey, a sample size of 385 was calculated considering population over 18 years old in the province of Barcelona in 2018. For the community pharmacist survey, it was calculated based on the number of registered pharmacists according to the Official Professional Pharmacists Association of Barcelona in 2018. A sample size of 369 was computed.
Variables studied were gender, age (“a”: <45 years of age and “b”: ≥45 years of age), educational level (“a”: lower than undergraduate studies and “b”: undergraduate or higher studies), and vaccination uptake for influenza during the 2019/2020 season. Attitude replies were distributed into two categories (“a”: Strongly Agree and Agree and “b”: Strongly Disagree and Disagree). Variable of years of experience as community pharmacists was also studied (“a”: 1–14 years and “b”: more than 14 years).
The collected data were processed using the Excel® Microsoft program and the MedCalc® statistical program. Bivariate (chi-square test) and multivariate (multiple logistic regression) analyses were performed based on two-sided P values with statistically significance if P<.05. The association measure of Odds Ratio (OR) and its 95% confidence intervals (CI) were also estimated.
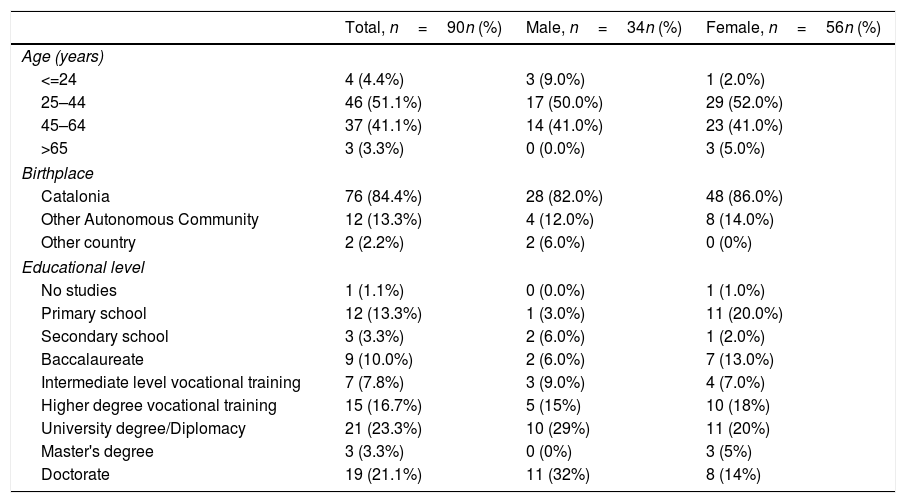
ResultsPharmacy users surveyA total of 90 surveys were collected among pharmacy users between March and April 2020. All of them accepted to participate and all were selected for the study. The respondent's sociodemographic characteristics are shown in Table 2. The majority of the study participants were females (62%), aged between 25 and 44 years old (51%), born in Catalonia (84%), and had achieved more than a high school diploma (65%). Fourteen percent suffered from chronic diseases, and only 3% were pregnant women.
Characteristics of pharmacy users.
| Total, n=90n (%) | Male, n=34n (%) | Female, n=56n (%) | |
|---|---|---|---|
| Age (years) | |||
| <=24 | 4 (4.4%) | 3 (9.0%) | 1 (2.0%) |
| 25–44 | 46 (51.1%) | 17 (50.0%) | 29 (52.0%) |
| 45–64 | 37 (41.1%) | 14 (41.0%) | 23 (41.0%) |
| >65 | 3 (3.3%) | 0 (0.0%) | 3 (5.0%) |
| Birthplace | |||
| Catalonia | 76 (84.4%) | 28 (82.0%) | 48 (86.0%) |
| Other Autonomous Community | 12 (13.3%) | 4 (12.0%) | 8 (14.0%) |
| Other country | 2 (2.2%) | 2 (6.0%) | 0 (0%) |
| Educational level | |||
| No studies | 1 (1.1%) | 0 (0.0%) | 1 (1.0%) |
| Primary school | 12 (13.3%) | 1 (3.0%) | 11 (20.0%) |
| Secondary school | 3 (3.3%) | 2 (6.0%) | 1 (2.0%) |
| Baccalaureate | 9 (10.0%) | 2 (6.0%) | 7 (13.0%) |
| Intermediate level vocational training | 7 (7.8%) | 3 (9.0%) | 4 (7.0%) |
| Higher degree vocational training | 15 (16.7%) | 5 (15%) | 10 (18%) |
| University degree/Diplomacy | 21 (23.3%) | 10 (29%) | 11 (20%) |
| Master's degree | 3 (3.3%) | 0 (0%) | 3 (5%) |
| Doctorate | 19 (21.1%) | 11 (32%) | 8 (14%) |
Of those surveyed, 40 (44%) showed some degree of VH according to the criteria set out in Table 1. There was no statistical association found between VH and gender (OR: 0.54; 95%CI 0.23 to 1.31; P=.17), nor the low level of studies (OR: 1.47; 95%CI 0.63 to 3.38; P=.37). When comparing age groups of vaccine hesitant respondents, a significant association was found for the older group (OR: 2.63; 95%CI 1.11 to 6.19; P=.03).
A significant regression equation was found (F(3,86)=2,346, P<.078), R2 of 0.043. Participants’ predicted VH is equal to 0.360+0.226 (Age)+0.109 (Gender)+0.06 (Education), where age is coded as 1=≥45 years, and 0=<45 years, gender is coded as 1=Male, 0=Female, and education is coded as 1=lower than undergraduate studies and 0=undergraduate or higher studies. Participant's VH increased 0.226 for the older group and 0.057 for the lower studies; and decreased 0.122 for males. Age was a significant predictor of VH (P=.03).
In this study, 18 (20%) respondents had stopped vaccinating themselves or their dependents; and 17% were unsure of the nature of a vaccine they had taken. The most-reported doubt was regarding influenza virus, meningococcus B, and papillomavirus vaccines (47%, 20%, and 13%, respectively).
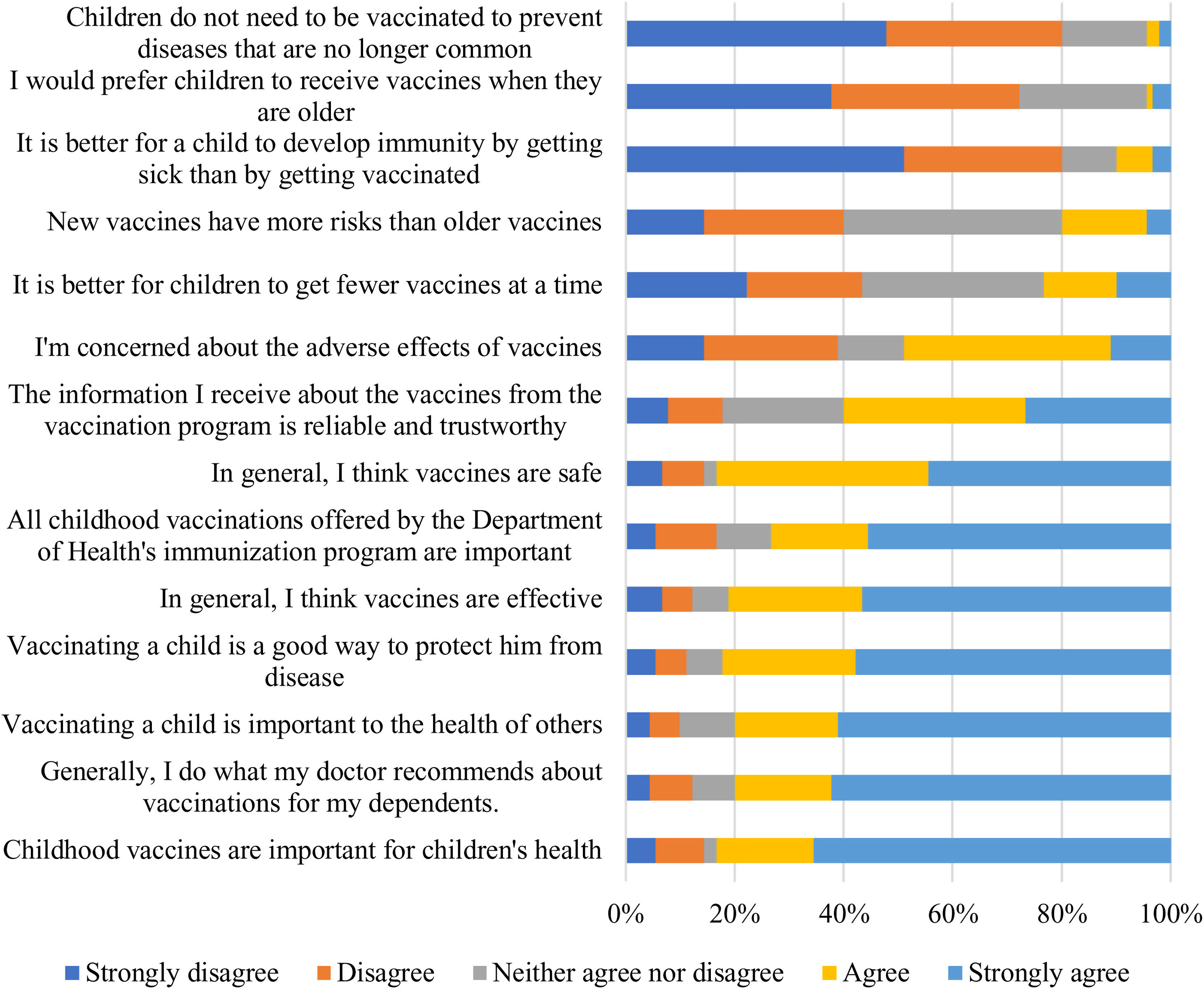
Of the 90 who participated, 75 (83%) regarded vaccines as safe and 73 (81%) as effective. Forty-four (49%) respondents were concerned about the adverse effects of vaccines. Nine respondents (10%) believed a child should develop immunity by natural infection rather than by the vaccine.
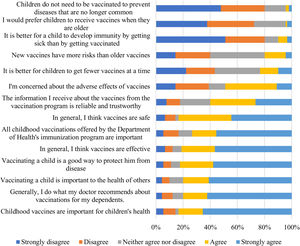
Of those surveyed, 46 (40%) considered the information received about vaccines from the vaccination program not reliable or trustworthy, and 15 (17%) had doubts about the importance of some of the childhood vaccinations included in the immunization program offered by the Department of Health (Fig. 1).
Twenty-five (28%) respondents knew someone that had suffered adverse effects due to a vaccine. This negative experience was associated with high vaccine-hesitant answers to the questionnaire (OR: 3.03; 95%CI 1.16 to 7.93; P=.02).
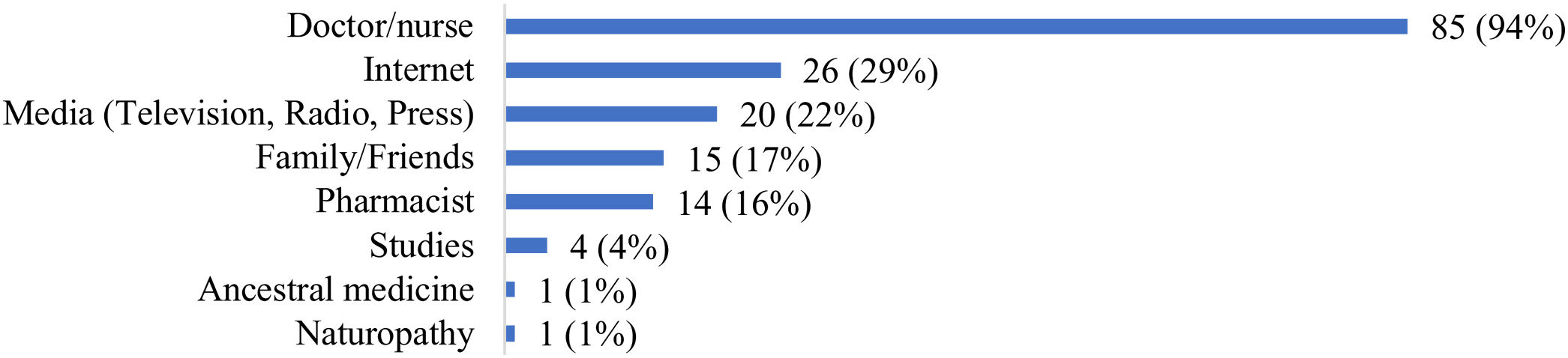
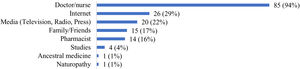
Eighty-one (90%) respondents of our study considered themselves capable of explaining what a vaccine is and what it does to our body. The majority of respondents’ principal sources of information on vaccines were doctors and nurses (94%), while pharmacists were considered only by 14 (16%) of them (Fig. 2).
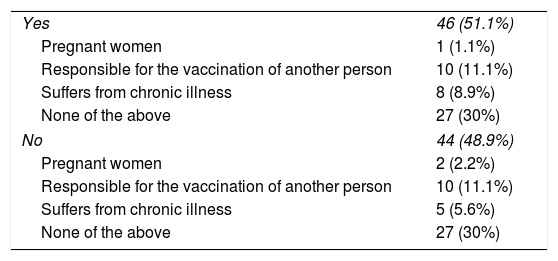
Forty-eight respondents (53%) considered insufficient the information received about vaccines and their safety, and 44 (49%) considered influenza vaccination to be unimportant (Table 3).
Answers to the question: Do you think influenza vaccination is important?
| Yes | 46 (51.1%) |
| Pregnant women | 1 (1.1%) |
| Responsible for the vaccination of another person | 10 (11.1%) |
| Suffers from chronic illness | 8 (8.9%) |
| None of the above | 27 (30%) |
| No | 44 (48.9%) |
| Pregnant women | 2 (2.2%) |
| Responsible for the vaccination of another person | 10 (11.1%) |
| Suffers from chronic illness | 5 (5.6%) |
| None of the above | 27 (30%) |
A total of 91 students from the fourth-year undergraduate pharmacy degree were surveyed during a public health course. The average age of the respondents was 22 years. Eighty-two percent of respondents were female, and 71 (78%) had Catalonia as their birthplace. All of them accepted to participate and all were selected for the study.
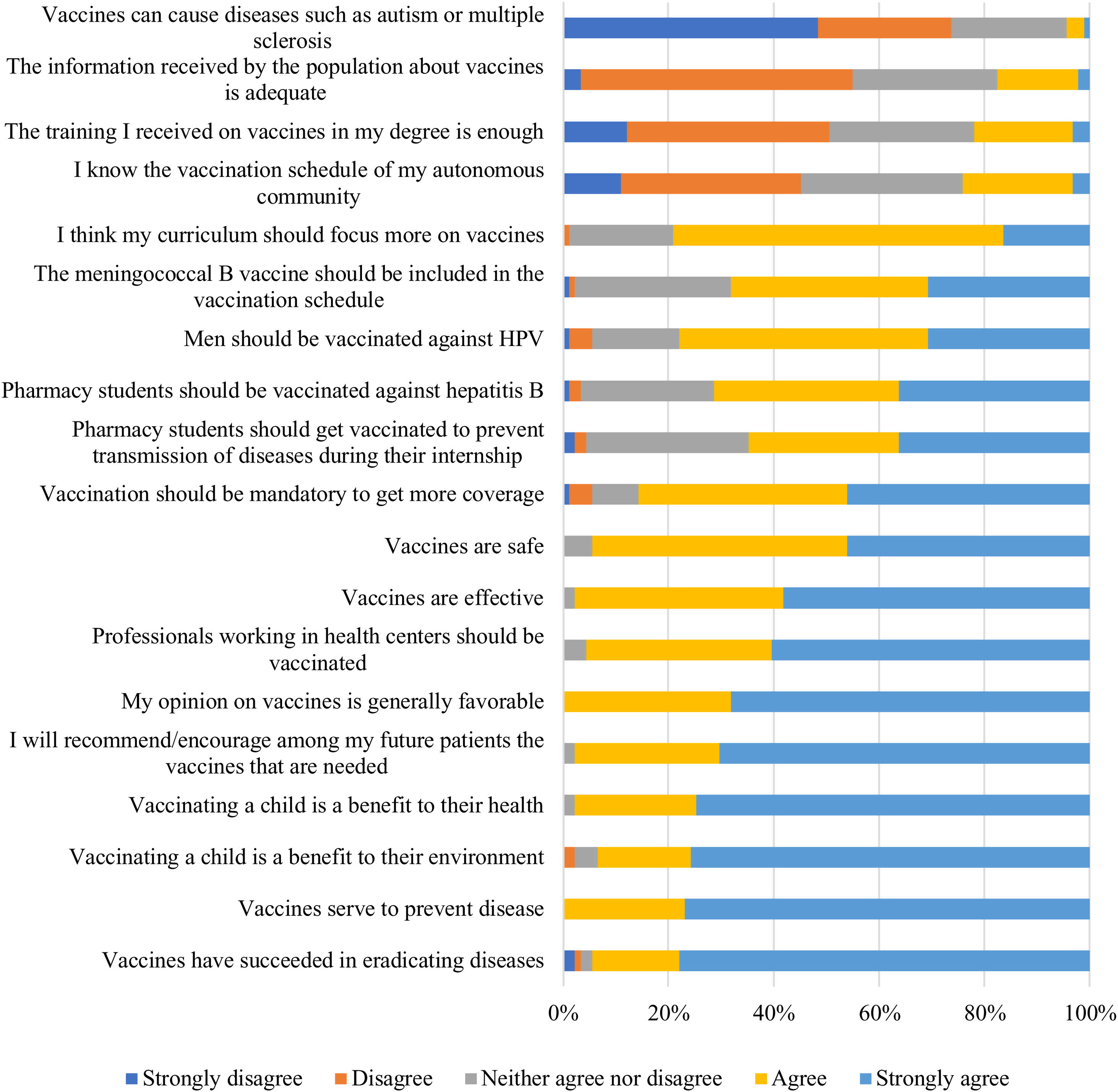
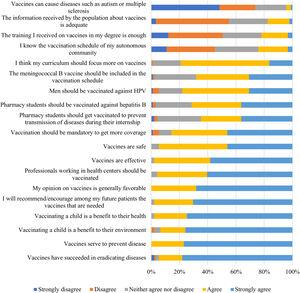
All surveyed students had a favorable attitude towards vaccination, and 89 (98%) agreed or strongly agreed that they would recommend and encourage the required vaccinations among their future patients/users. However, when asked if vaccines could cause diseases such as autism or multiple sclerosis, 20 respondents (22%) answered they neither agree or disagree with the statement, and 4 agree or strongly agree (Fig. 3).
Half of the respondents considered vaccine training in the pharmacy degree insufficient, and 72 surveyed students (79%) pondered the study program should devote more teaching hours to vaccines. University, family doctor, and pediatrician were the principal sources of information about vaccines among surveyed students.
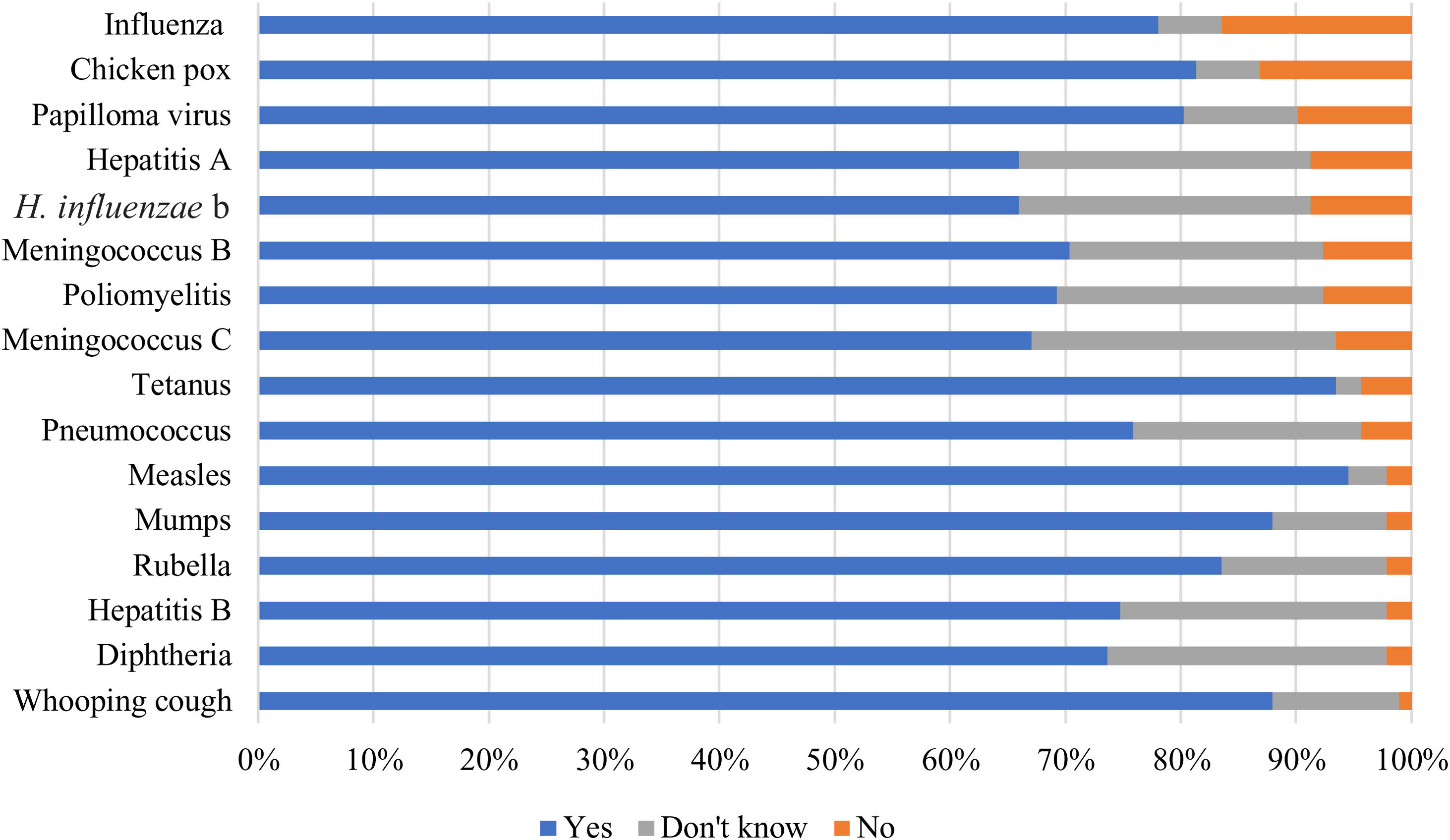
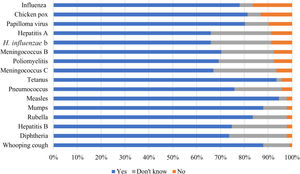
When asked: Which vaccines do you think are needed for a health care provider?, all the proposed vaccines were considered relevant (>67% answered yes). Fifteen respondents considered the influenza vaccine the least important (16% answered no), while 86 pondered measles the most (95% answered yes) (Fig. 4).
Official Professional Associations were considered, by most respondents, to be the bodies that should offer follow-up courses on vaccines (84, 92%).
Community pharmacists surveySixty-four surveys were collected among community pharmacists, of which 51 (80%) were answered by women. More than half of respondents (36; 56%) were aged between 25 and 44 years old, and 55 (86%) were born in Catalonia. The mean years of experience as community pharmacists were 14,25 (SD 10.488). All of them accepted to participate and all were selected for the study.
Fifty-seven (89%) pharmacists considered vaccination the most important measure to prevent infectious diseases.
Only 10 (16%) respondents received influenza vaccination during the 2019/2020 influenza seasonal campaign, while 39 (61%) agreed that pharmacists, being health professionals, should receive influenza vaccine annually. No significant bivariate or multivariate association was observed between omission of influenza vaccine and gender (OR: 0.98; 95%CI 0.18 to 5.27; P=.98) nor with years of professional experience (OR: 0.77; 95%CI 0.19 to 3.05; P=.71).
Twenty (31%) pharmacists admitted not having been vaccinated at some point in their lives, of these 16 (80%) referred to H. influenza. Low benefit/risk and lack of time were some of the reasons given by respondents.
The Official Professional Pharmacists Association of Barcelona was the main source of vaccine information among 34 (53%) respondents followed by the Department of Health in Catalonia and the European Medicines Agency (EMA) in 11 (17%) respondents, respectively.
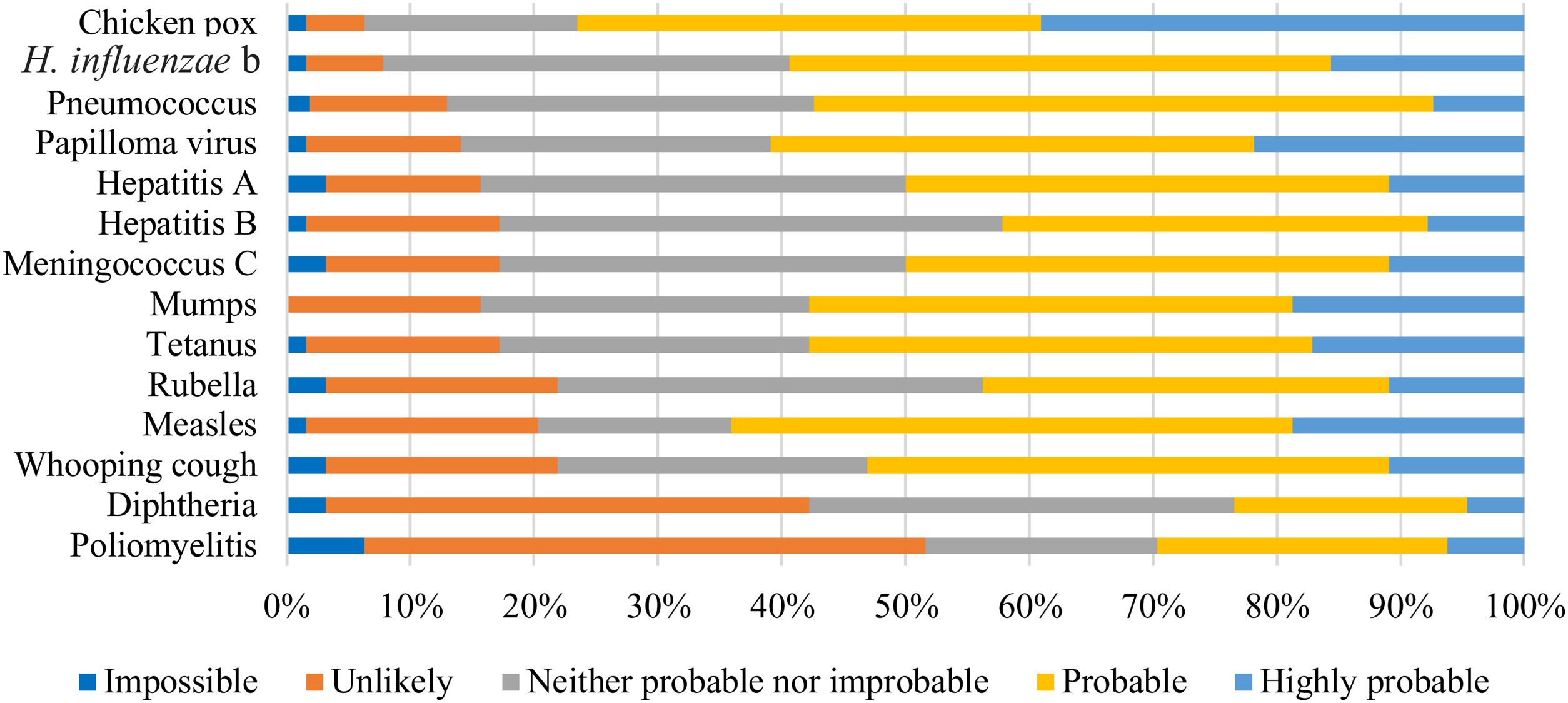
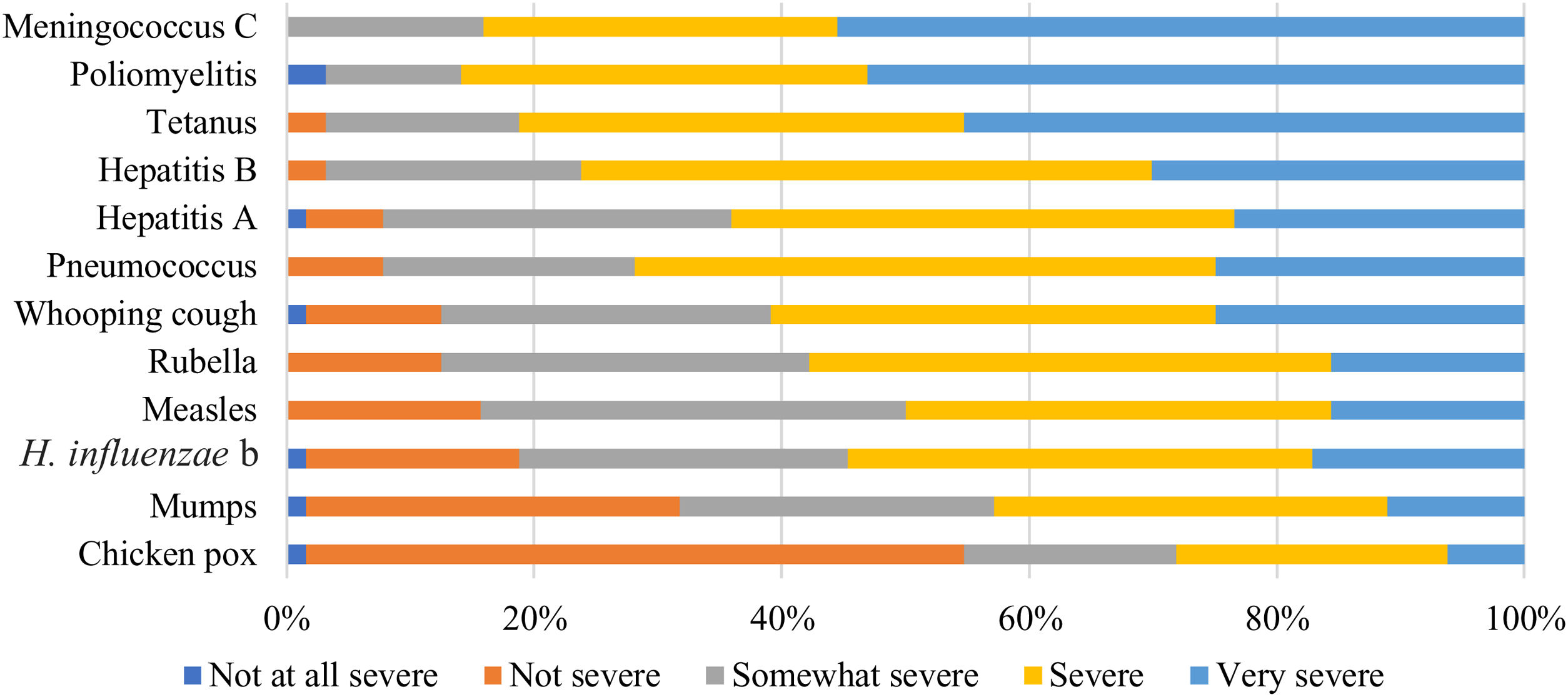
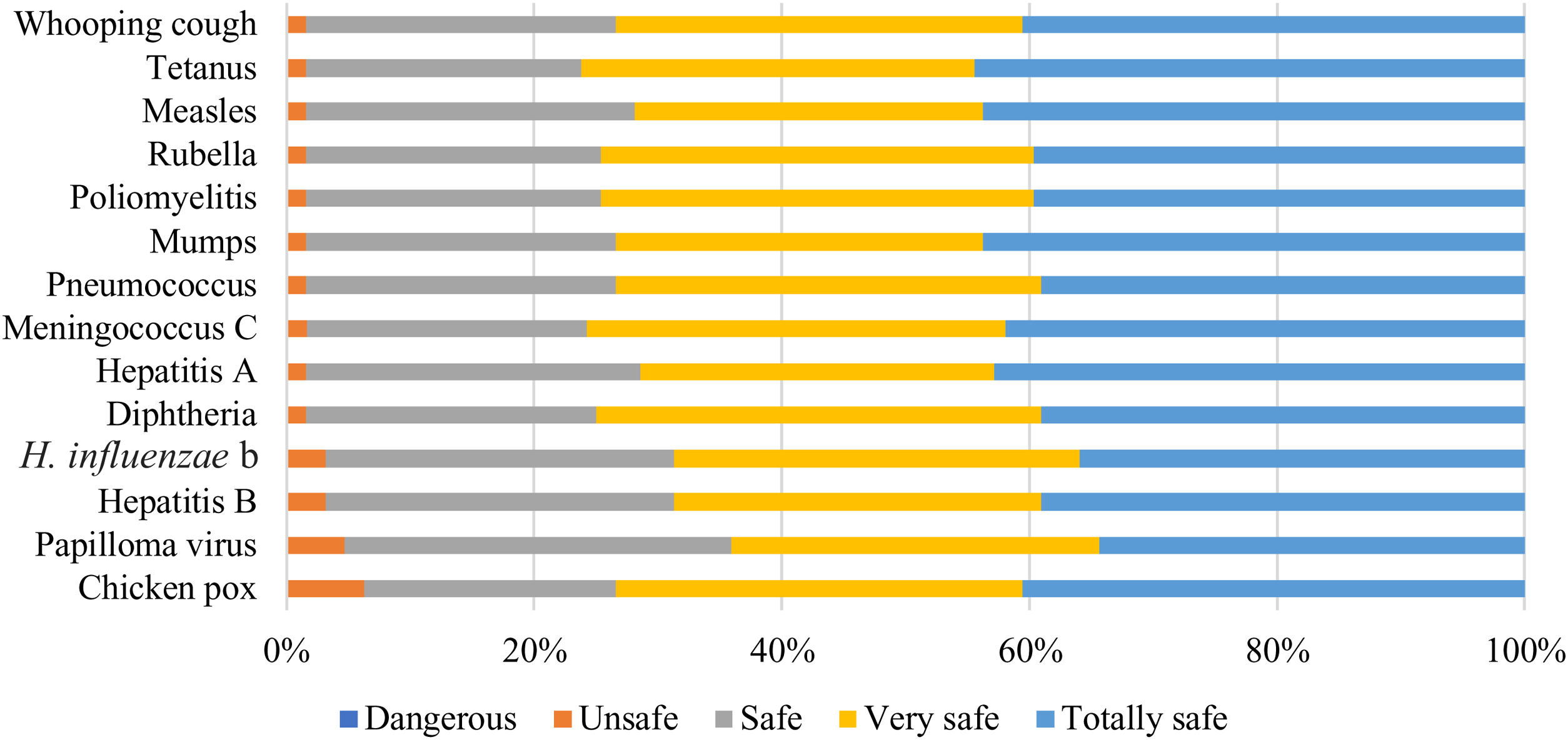
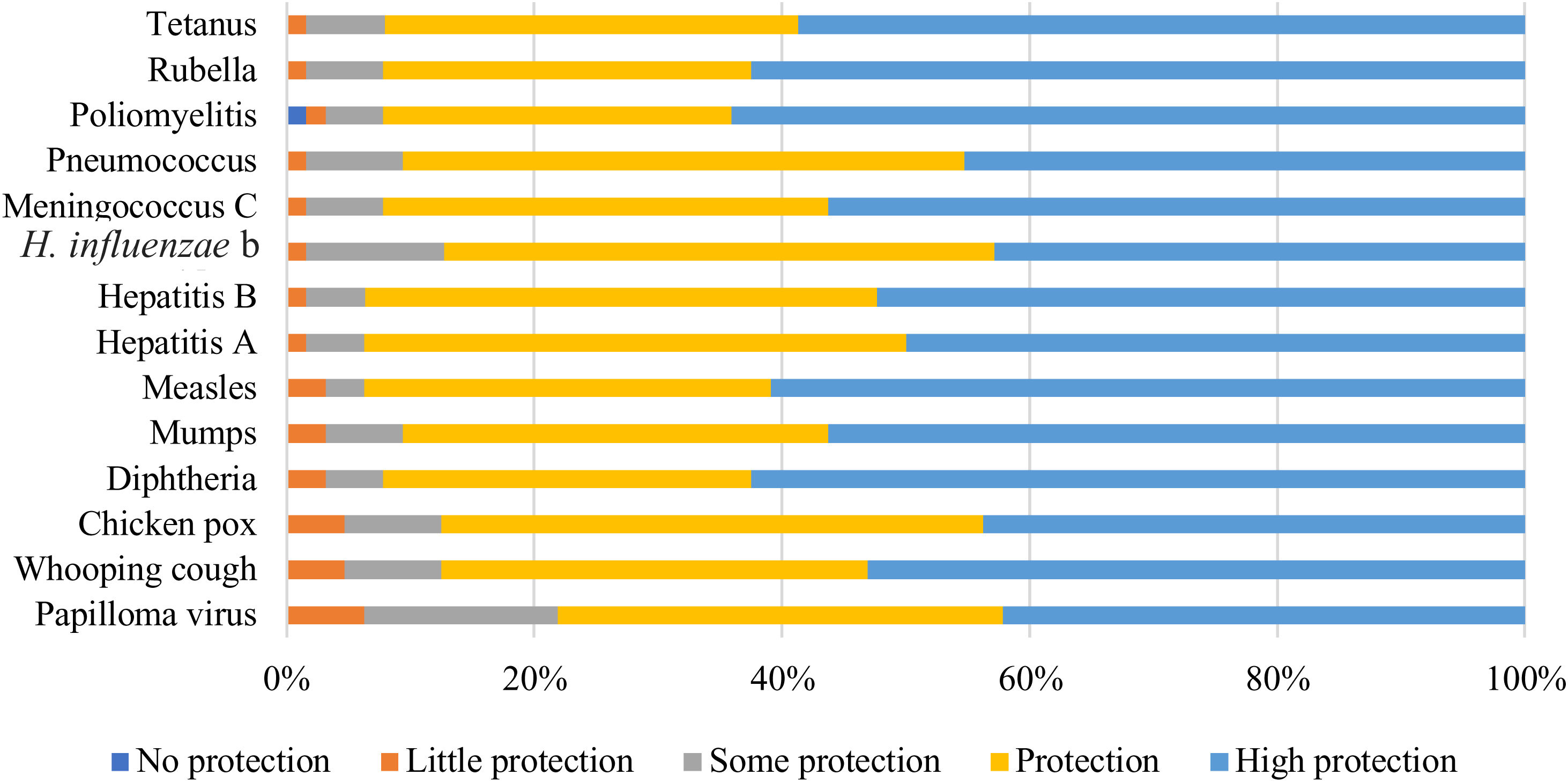
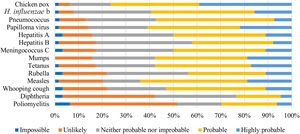
Answers to the questions on the perception of susceptibility and severity of a serial of vaccine-preventable diseases are shown in Figs. 5–8.
Four (6%) respondents considered impossible for an unvaccinated child to contract the poliomyelitis, while 39 (61%) considered it probable or highly probable that they would contract human papillomavirus (Fig. 5).
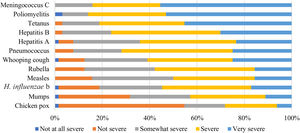
Respondents considered meningococcus C and poliomyelitis the most severe disease that an unvaccinated 8-year-old child can contract, while chickenpox was the least severe (Fig. 6).
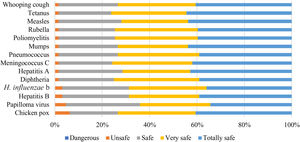
All vaccines were considered safe by most respondents (89%). The chickenpox vaccine was considered the least safe of all, followed by the human papillomavirus (HPV) vaccine (Fig. 7).
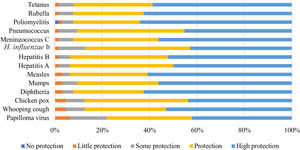
According to the pharmacists surveyed, 69% considered all vaccines offered protection. Papillomavirus vaccine obtained the lowest percentage of perception of protection (22% answered it provided some or little protection) (Fig. 8). One respondent considered the poliomyelitis vaccine gave no protection.
All surveyed pharmacists promoted vaccination while 52 (81%) responders considered they did not have the needed support educational material to properly promote vaccination and 13 (20%) responders did not considered themselves able to discuss questions from people for and against vaccination.
DiscussionThe present study aimed to investigate the perception and attitudes towards vaccination of pharmacy users, pharmacy students and community pharmacists.
The results indicate that although most of the surveyed pharmacy users (80%) vaccinated from all recommended vaccines including influenza vaccine, almost half of them (44%) showed some degree of VH. Similarly Della Polla et al. found that 33.3% of parents of teenagers in the Campània region of Italy, had hesitant attitudes towards HPV vaccine, while 88% consider it useful to prevent the disease.26 Dubé et al. also noted this phenomenon in Canada, where according to the Childhood National Immunization Coverage Survey in 2013, only 1.5% of children had never received vaccines, while 70% of the parents indicated they were concerned about potential side effects from vaccines, and 37% believed that a vaccine could cause the same disease it was meant to prevent.27,28
This suggests that the percentage of vaccine coverage in a country is not entirely indicative of the degree of its VH, as there may be a large portion of the population with serious doubts and worries about vaccines, who still vaccinate. These people are at risk to reject the vaccination but are also more receptive to vaccination promotion interventions, as stated by Leask et al.29
Although a high percentage of respondents considered themselves able to explain what a vaccine is and what it does to our body (90%), 11% within that group said they disagreed or strongly disagreed with the following statement: “Vaccinating a child is important to the health of others in my community.” In Eurobarometer 488 it was found that for the same statement there was a high correlation between the “strongly disagreed” response and a low level of knowledge about vaccines.21
This suggests that the perception of knowledge about vaccination cannot be diagnostic of the actual knowledge of people and therefore all information about vaccines prepared for the population should not be provided exclusively on demand but to the population as a whole, and thus be able to correct misconceptions.
The only two respondents who indicated that “ancestral medicine” and “naturopathy” were one of their main sources of information gave a high vaccine-hesitant answers to the questionnaire. Despite having an insufficient sample, these results would match those of other authors who suggest a correlation between the use of complementary medicines and low vaccine coverage.22,30,31
The lack of trust in the National Health System observed in this study (23%) is consistent with that obtained in a cohort study conducted in Japan in 2015, which showed 28.4% distrust.32 This value may be related to the perception of lack of information received about vaccines and their safety presented by 53% of respondents in the present study.
A significant association between the vaccine hesitant answers to the overall questionnaire, and previous negative experiences with vaccination, was observed in this study. However, most of the side effects described by the respondents were the most common after the administration of any vaccine: mild fever, feeling tired, muscle aches, swelling or redness where the shot was given, etc.
Higher age (>44 years) was also found to be significantly associated with stronger vaccine hesitant answers. However, in literature this has been shown to be a barrier to vaccine uptake, as well as a promotor, thus not being a conclusive predictor of vaccination.33
Almost half of respondents (49%) considered unimportant to get vaccinated against the influenza vaccine, and the same was observed by those who reported being pregnant or suffering from a serious chronic illness (40%). These results are consistent with the study presented by the WHO in 2016, and indicate a high level of complacency, i.e., a low perception of risk of influenza.33
Pharmacy students had a similar positive attitude towards vaccination as medical students from La Laguna University (Tenerife) surveyed by Lebrero et al. and from other European countries reported by Rostkowska et al.23,34 However, only 50% of surveyed medical students by Lebrero et al. considered that the curriculum should devote more teaching hours to vaccines compared to 79% acknowledged by students in the present study.
This perceived lack of training could be the cause of the high number of respondents (74.7%) without knowledge about the vaccination schedule of their autonomous community, for which medical students of Lebrero et al. obtained a significantly lower percentage (58%).23
Similar beliefs between our study and Lebrero et al. were found when asked if vaccines could cause diseases such as autism or multiple sclerosis. Although in our study only 3 respondents agreed or strongly agreed with this statement, these beliefs should be addressed in the university setting.
Most surveyed pharmacy students considered all the proposed vaccines relevant for a health care provider. Similar results were obtained by Lebrero et al., however, in our study slightly lower percentages were observed for influenza and hepatitis B vaccines, and higher for mumps and papilloma virus vaccines. In both studies, tetanus and measles vaccines showed high acceptance among respondents.23 Contrastingly, Rostkowska at al. reported a high number of respondents (86%) that considered vaccination against seasonal influenza and Hepatitis B should be mandatory for medical staff.34
In both our study and Lebrero et al., the main source of information for the respondents was the university. However pharmacy students give more importance to friends and family; to nurses and midwives; and informative leaflets and posters, than medical students.23
Seasonal influenza vaccination coverage among community pharmacists in our study was 16%, lower than other studies conducted in Catalonia, and even lower than in other western countries, which in this last case could be explained by compensations or requirement to be vaccinated by their employers.35–40
According to the literature, the main causes for the omission of this vaccine are lack of time, low perception of risk of contracting the disease, consideration that they have no medical indication to get the vaccine or concerns about vaccine safety and efficacy.17,36,39,41,42 In our study, lack of time and low benefit/risk were some of the justifications given by respondents.
The high importance that surveyed pharmacists gave to vaccinating against influenza and the high number of respondents that considered not missed any vaccines for themselves contrast with the low influenza vaccination rate observed, and indicate that pharmacists, despite finding vaccination necessary, do not consider it an omission not to get this vaccine.
Both surveyed pharmacy students and community pharmacists considered Professional Associations a source of reliable vaccine information. This agrees with Andrés-Rodríguez et al., who found that community pharmacist in Pontevedra consider the Professional Associations should be responsible for training and provide support for the implementation of any new care service provided to patients, clearly over the University as an institution.43 In Italy, however, sources of information of community pharmacists surveyed by Della Polla et al. were scientific journals (69.6%), followed by mass-media and internet (41.3%).44
Perceptions of disease severity and probability of infection in our study was similar to those reported by Picchio et al.24 While a very low percentage of respondents considered impossible or improbable for an unvaccinated child to contract several diseases (4%), this overconfidence attitude may prevent pharmacists from recommending their vaccines to the pharmacy users coming for advise on them.24
The chickenpox vaccine was considered the least safe of all, followed by the human papillomavirus (HPV) vaccine. In the study by Picchio et al. the human papilloma virus vaccine was considered the most unsafe, being the only one described as “dangerous” by one respondent. This may be due to the fact that this study was carried out between 2016 and 2017 in Barcelona, when the HPV vaccine had been less time in the vaccination schedule.24
The biggest barrier encountered for the promotion of vaccination provided by community pharmacists was the lack of support material noted by 81% of respondents, which could be resolved by proportioning educational brochures to the pharmacies.
According to Pullagura et al. surveyed pharmacists in Canada reported the most effective strategies to address VH at the community pharmacy were provision of information on safety and efficacy and educating patients on the risks of non-vaccination and the benefits of vaccination.17 This strategies should be implemented as promoting vaccination through community pharmacists offers many advantages (location, no need to prebook appointments, long opening hours and the high quality and trustworthiness of pharmacy-based services) according to Sepp et al.45
Our results must be interpreted taking into account several limitations. There may be a sample selection bias as respondents volunteered to participate in the surveys, and a recall bias as several questions required remembrance of previous events. The size of the sample was also restricted, specially among community pharmacists. According to literature, surveys with this group often have lower response rates than those made with other HCPs.24,46,47 However, in this study, context played the highest role. The COVID-19 pandemic during the months of data collection, difficulted reaching reaching a wider population, especially the community pharmacists, who were overwhelmed with work.
Changes on the method of disseminating the questionnaires also prevented to track how many individuals declined to participate, and if they held more vaccine doubts or not.
Besides, the perception towards vaccination may have varied after the public attention the vaccines have received recently, and social desirability bias may have affected our study. Therefore, further research on VH is needed to draw robust conclusions.
However, the findings of this study may be helpful to increase awareness and importance of the influenza vaccine among community pharmacists, as first line health care professionals. The study shows a clear need for information and appropriate tools to better target hesitant attitudes on the pharmacy context and promote vaccine uptake, which would reduce the burden in primary health care.
ConclusionsThe results obtained in this study indicate the need for the promotion and active education of the population on vaccines, the improvement of the information provided, and reliable communication between health professionals and patients. Community pharmacists, as health professionals in daily contact with the population, have the opportunity to offer this service in pharmacy offices, establishing them as the point of reference for the citizens to resolve all minor issues about vaccination that would otherwise be neglected and could lead to its omission.
Having educational material about vaccines in the pharmacy office is therefore vital to resolve doubts and lead to sources of proven and reliable information.
Likewise, the low coverage of the influenza vaccine among community pharmacists should be addressed too. Professional associations should promote vaccination campaigns, as this was the principal source of information on vaccines among pharmacists in our study.
FundingThe authors declare that the current study was not funded.
Conflict of interestsThe authors declare no conflict of interests.
The authors thank the community pharmacists and their users, the pharmacy students, and their professors at the University of Barcelona for participating in this study, as well as the pharmacies that contributed by diffusing the questionnaires. MSc Joan Feliu Calafat Pla is also thanked for his writing assistance.
All authors attest they meet the ICMJE criteria for authorship.