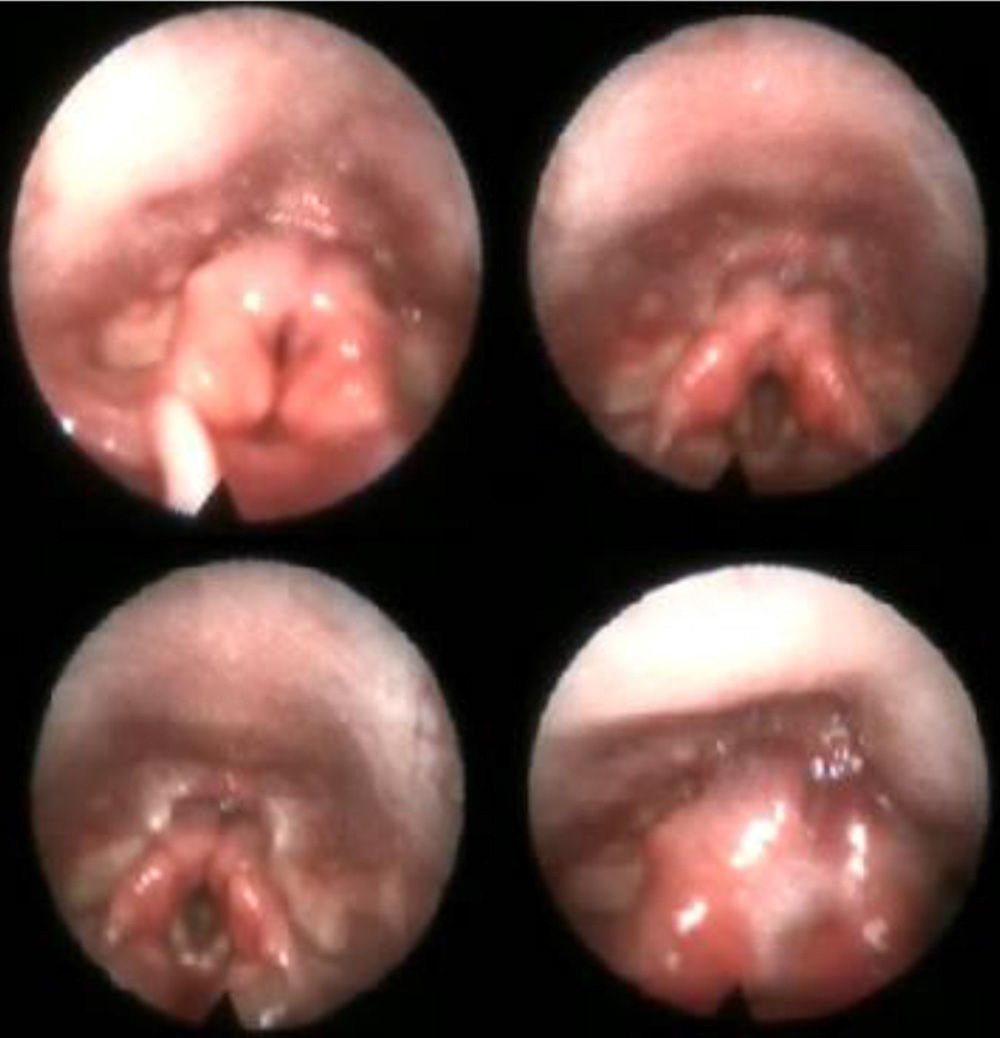
A 14 month male patient with a background of unilateral right canal stenosis, enteral nutrition through percutaneous endoscopic gastrostomy (PEG) due to dysphagia from weaning, hospital admittance for bronchopneumonia, dysphoric crying, coughing after swallowing, and asphyctic episodes was referred to our hospital for study and treatment. Examination revealed small low inward facing auricles, a narrow auditory canal, a palmiped uvula and wide nasal bridge. A nasopharynx and laryngeal tracheoscopy and rigid laryngoscopy were performed to examine the aerodigestive tract and these revealed an excess of protruding mucosa (Fig. 1) in both arytenoids which deposited an interarytenoid solution that impeded posterior laryngeal closure without cutting across the glottis plane. Evaluation was completed with a video fluoroscopic swallowing study and an isotopic swallowing study using Tc99 gamma graphics. Endoscopic surgical closure using CO2 laser and microsutures was indicated for the diagnosis of secondary dysphagia to type II laryngeal diastema in the patient with a polymalformative condition compatible with OpitzG/BBB syndrome. The postoperative video fluoroscopic study confirmed safety in swallowing.
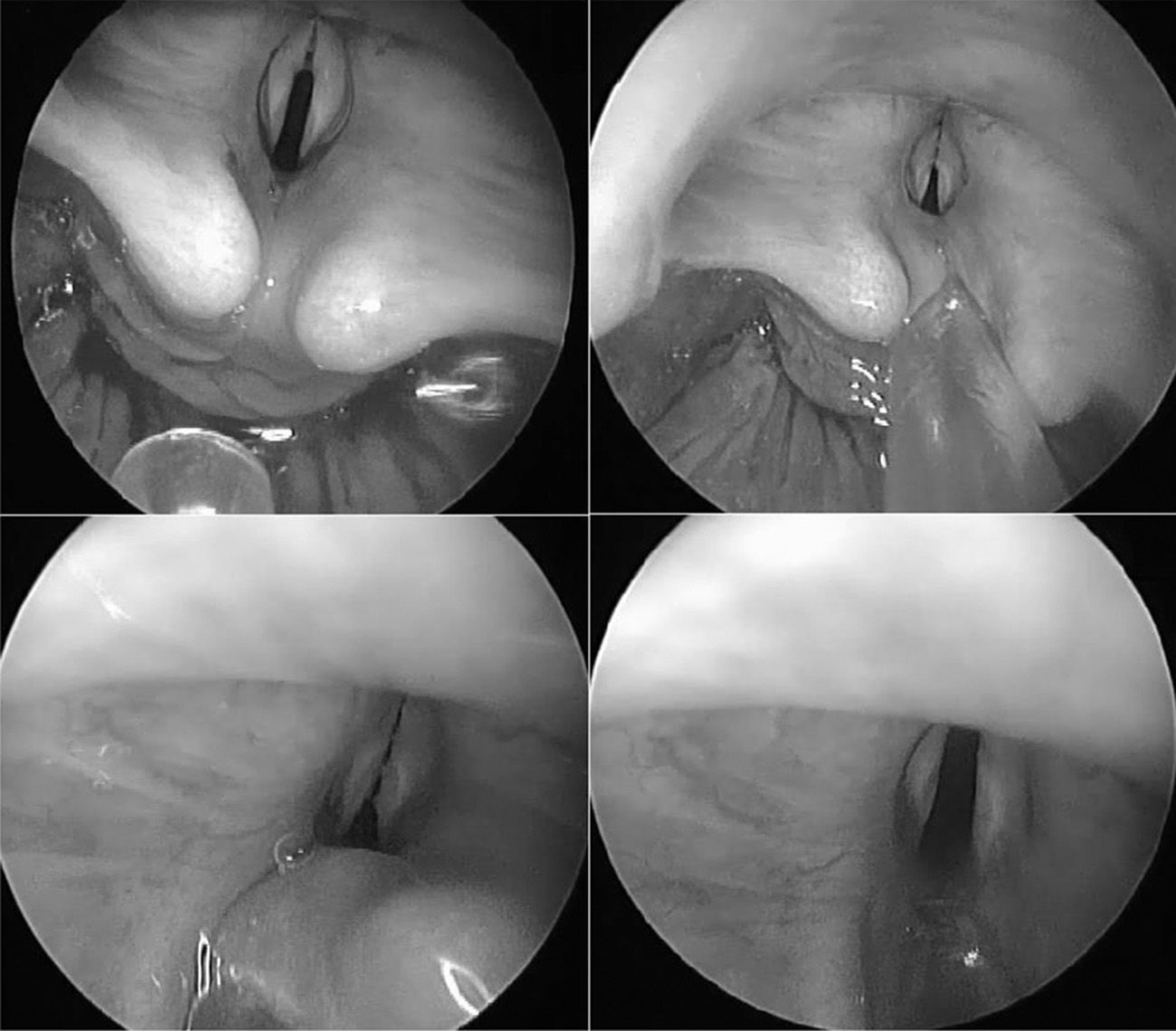
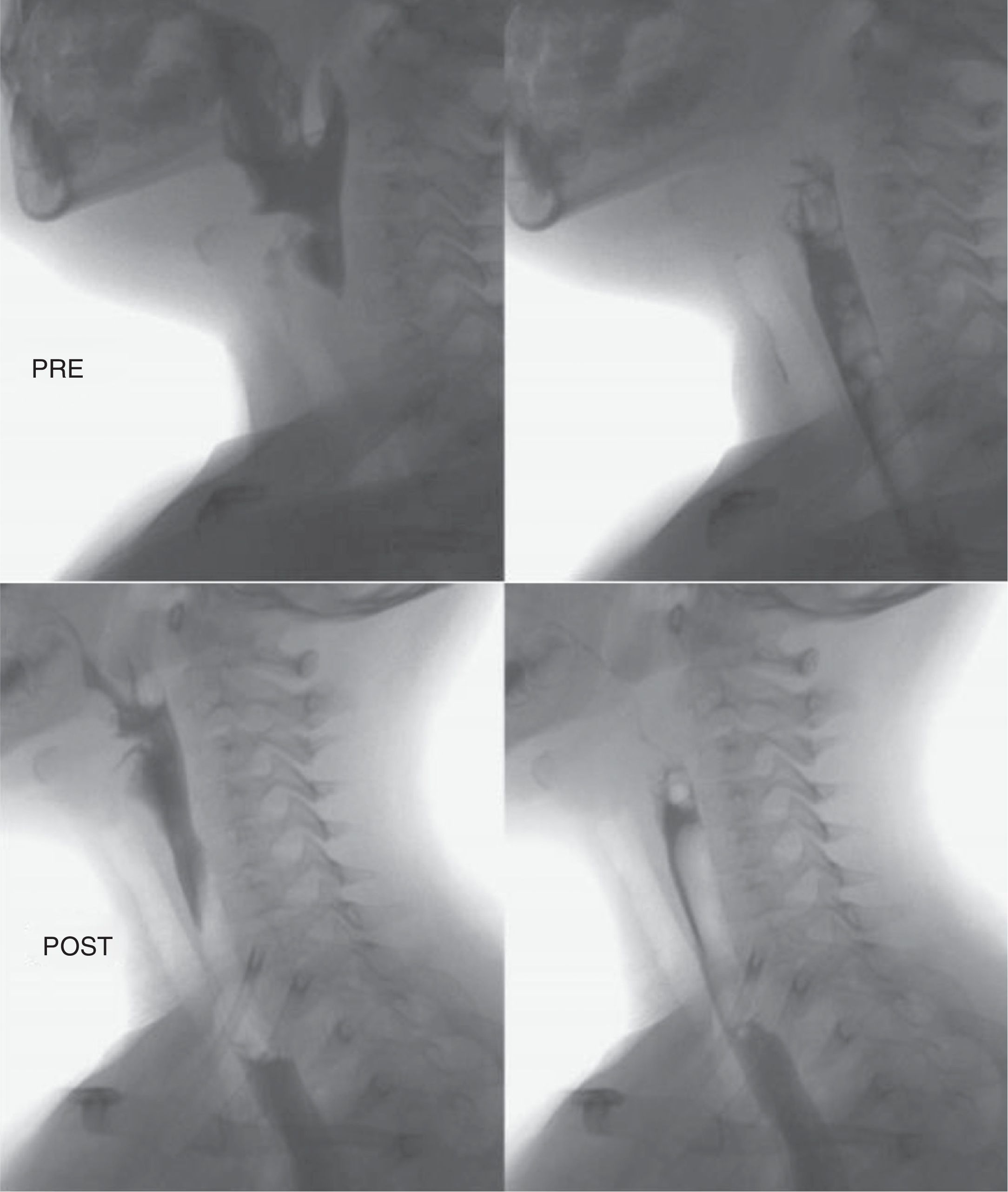
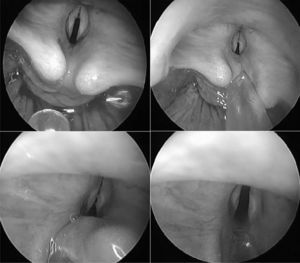
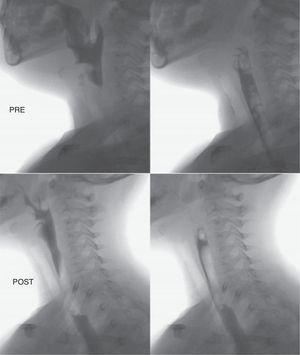
Case 2A 4-year-old female patient with a medical history of repeated pneumonia with several hospital admittances to the Paediatric Intermediate Care Unit (PIMC) from the age of 2, presented with a single clinical swallowing condition of a productive cough, which was on occasion related to ingestion of liquids. Aerodigestive airway examination was performed under sedation using a nasopharynx and laryngeal tracheoscopy procedure, which established the diagnosis of bronchiectasis and the suspicion of type I laryngeal cleft. The video fluoroscopic swallowing study confirmed the presence of tracheal aspiration with small volumes of 5cc liquid density (Fig. 1). Instrumental examination during direct laryngoscopy in suspension under anaesthesia with spontaneous ventilation confirmed the diagnosis, whilst (Fig. 2) we proceeded simultaneously to closure, using the CO2 laser and microsuture. The patient was extubated during the initial 24h, with continued respiratory monitoring in the PIMC. A video fluoroscopy of swallowing was subsequently programmed which confirmed the absence of aspiration (Fig. 3).
Laryngeal cleft or diastema (LD) is a rare congenital condition with a classically reported incidence of one case per 10,000–20,000 live newborns.1 Greater awareness and a higher index of suspicion has increased the incidence of its diagnosis.2,3 It may present in conjunction with complex syndromes (Opitz–Frias and Pallister–Hall) or nonsyndromic anomalies of other systems.3 LD is a fissure arising between the larynx and/or the trachea and the pharynx and oesophagus system, due to a fault in the separation of the laryngo tracheal groove and the oesophagus.4 Many classifications have been used to describe it, the most frequent currently being the modified version made by Sandu and Monnier5 of the classical Benjamin and Inglis classification6: type 0: submucosa cleft; type I: supraglottic, interarytenoid cleft type II: the defect compromises the vocal cords and in part the cricoid cartilage; type IIIa: compromise of all cricoid cartilage up to the trachea with no compromise of the later; type IIIb: compromise of the cricoid cartilage and cervical trachea; type IV: compromise of the thoracic trachea and may descend to the carina. Clinical manifestations are correlated with its extension and may vary from asymptomatic patients (21% in several series)7 to moderate symptoms including stridor, a hoarse cry, pharyngeal hypersecretion, problems swallowing and slight pulmonary repercussion for type I. In types II and III the most marked symptoms are pulmonary aspiration and infection. Finally, in type IV there is almost immediate respiratory distress, massive aspiration with difficulty in ventilation.4
The low incidence of LD makes it a diagnostic challenge, with a need for high clinical suspicion and a systematic instrumental examination to include probing of the posterior laryngeal wall. As a result the lesion may be classified and the appropriate treatment indicated.4,5 In the first case, our patient received multiple treatments in different institutions without a definitive diagnosis, and in the second case different entities suspected it to be cystic fibrosis and/or pulmonary tuberculosis which resulted in antibiotic treatments being indicated. It is of note that there was low suspicion of aspiration until examination in the second case. For this reason we affirm the need to consider this type of suspicion in the presence of aerodigestive conditions and all the more so if they are associated with other midline malformation defects.4 With respect to treatment, for types I, II and in some cases type III, endoscopic surgery is indicated as it is minimally invasive, easy to perform, and does not present aesthetic cervical sequelae.4,8 For types III and IV an external surgical approach is necessary, due to respiratory instability.9 The anaesthetic considerations in the different studies reviewed suggested maintaining the patient with spontaneous ventilation without endotracheal intubation or the use of small calibre tubes.3,10 In our 2 cases, depending on the extent of the defect, an endoscopic closure was performed under general anaesthesia with intubation, with removal of the mucosa margins and the vertex aided by the CO2 laser superpulsed mode at output of 3–5W and suturing the laryngeal tracheal and pharyngoesophageal walls with non-absorbent 5–0 monofilament aided by a microsurgical needle holder. The video fluoroscopy of postoperative swallowing confirmed the absence of aspiration with both patients was able to receive complete oral and asymptomatic nutrition.
Conflict of InterestsThe authors have no conflicts of interest to declare.
Please cite this article as: Macías-Rodríguez DH, Martín-Hernández R, Muñoz-Herrera ÁM, Benito-González F. Hendidura laríngea: diagnóstico y tratamiento quirúrgico endoscópico. Presentación de 2 casos. Acta Otorrinolaringol Esp. 2015;66:237–240.