In 2008, the Otoneurology committee of the SEORL-PCF published a classification of peripheral vertigo, based on clinical criteria. The objective of this study was to validate this classification through analysing the diagnostic agreement among several medical assessors.
MethodsSeven medical assessors, all with clinical experience, from 6 different hospitals, participated in the study. One of them selected the clinical histories of 50 consecutive patients who had consulted as a result of balance disorders (24 men and 26 women) with an average age of 53.5 years. These clinical histories – without any information that would identify the patient, the diagnosis established and the treatment – were sent to another 6 assessors. Each of these investigators established their own diagnosis, trying to adjust it to the epigraphs of the classification.
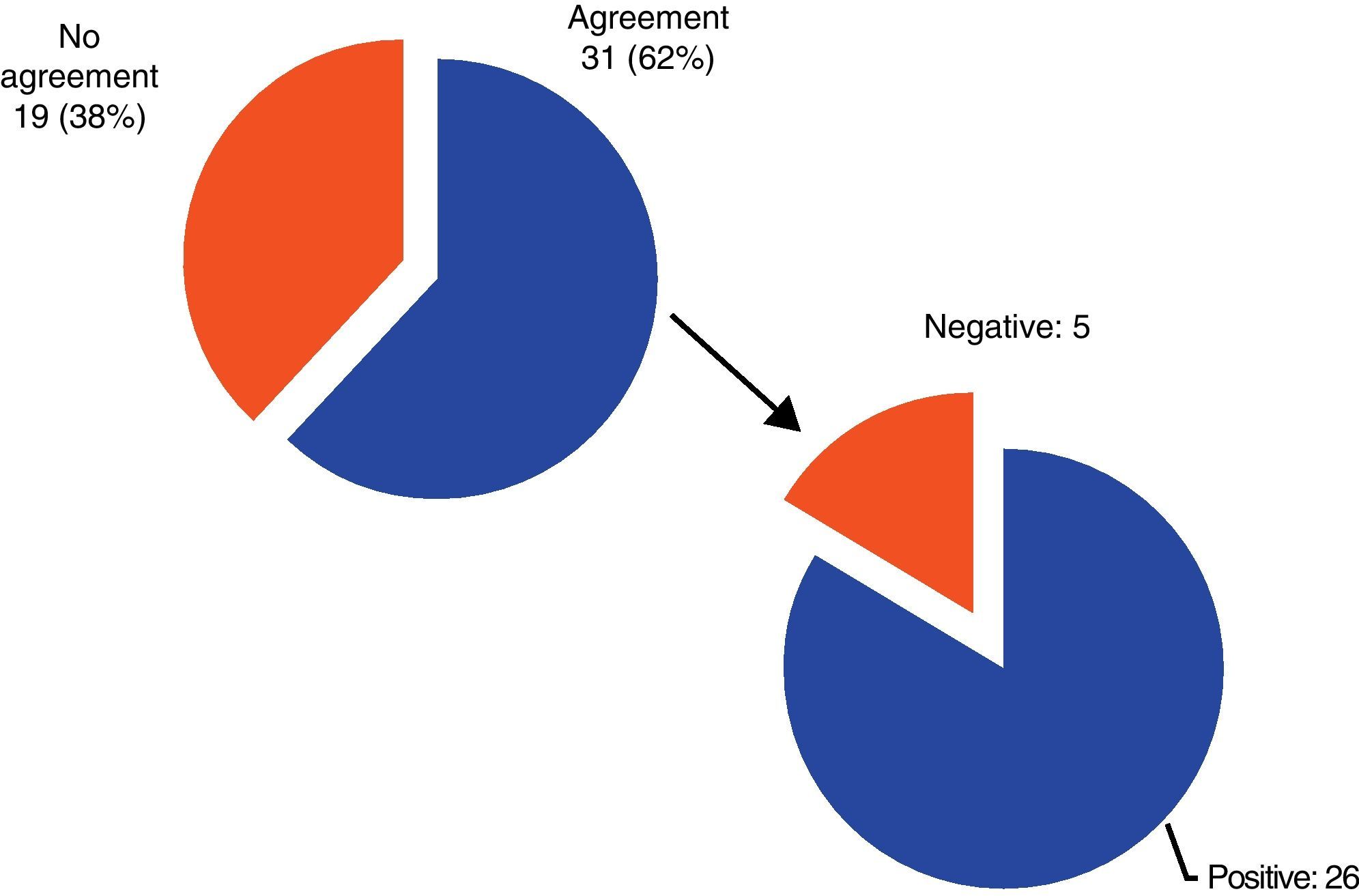
ResultsOf the 50 patients, there was substantial agreement in the diagnosis (4 or more evaluators indicated the same one) in 31 cases (26 with a positive diagnosis and 5 with a negative one, which could not be included in any epigraph). The kappa index, which measures the level of accordance between 2 or more assessors, was 0.4198 (moderate level of agreement). Unanimity was achieved in only 7 cases (4 BPPV, 2 Ménière's disease and 1 vertigo associated with migraine).
ConclusionsThe current classification, with the included criteria it includes, allows labelling with an acceptable consensus to only 62% of the patients. Therefore, a modification in the classification is proposed in relation with the probable BPPV epigraph, as well as a revision of the entries for vertigo-migraine and vertigo associated with migraine.
La Comisión de Otoneurología de la SEORL-PCF publicó en 2008 una clasificación de los vértigos periféricos, basada en criterios clínicos. El objetivo de este estudio es validar esta clasificación mediante el análisis de la concordancia diagnóstica entre múltiples evaluadores.
MétodosParticiparon 7 evaluadores con experiencia clínica en el diagnóstico de afección vestibular, pertenecientes a 6 centros diferentes. Uno de ellos seleccionó las historias clínicas de 50 pacientes consecutivos que consultaron por alteraciones del equilibrio (24 varones y 26 mujeres; edad media: 53,5 años). Estas historias, suprimidos los datos que permitiesen identificar a los pacientes, el diagnóstico establecido y el tratamiento pautado, fueron remitidas a los otros 6 investigadores. Cada uno de ellos estableció un diagnóstico, intentando ajustarlo a los epígrafes de la clasificación.
ResultadosDe los 50 pacientes, existió una coincidencia sustancial en el diagnóstico (4 o más evaluadores alcanzaron el mismo) en 31 (26 con diagnóstico positivo y 5 negativo: no podía ser incluido en ningún epígrafe). El índice kappa, que mide el nivel de concordancia entre tres o más observadores, fue de 0,4198 (lo que indica un grado de acuerdo moderado). La unanimidad solo se alcanzó en 7 pacientes (4 VPPB, dos enfermedades de Ménière y un vértigo asociado a migraña).
ConclusionesLa actual clasificación, con los criterios que incluye, solo permite etiquetar con un consenso aceptable al 62% de los pacientes. Se propone una modificación de la clasificación, incluyendo el epígrafe de VPPB probable, y revisando los de vértigo-migraña y vértigo asociado a migraña.
Patients with vertigo are often particularly a diagnostic chanllenge for otolaryngologists. Vagueness in the explanation of their symptoms and difficulty to interpret them are often worsened by variability in the naming of clinical symptoms. Despite various attempts to classify vertigo (or the entities which cause it),1 reality has shown that, even among otolaryngologists with specific experience in Otoneurology, there is no common language enabling simple communication when establishing diagnoses and treatment protocols. This fact has also been noted internationally by the Bárány Society.2,3
With this reality in mind, and as an attempt to establish a simple nomenclature accepted by all, the Otoneurology Commission of SEORL-PCF developed a proposal for the classification of peripheral vertigo between 2003 and 2006. After being reviewed and evaluated by various Spanish otoneurologists, it was published as a consensus document in Acta Otorrinolaringológica Española in the year 2008,4 and later quoted in a publication by the Bárány Society in 2009.3
In the same year 2009, the Otoneurology Commission of SEORL-PCF proposed a validation of this classification, in order to test its usefulness in clinical practice. The aim was threefold:
- –
To determine the percentage of patients attending consultation due to vertigo and balance disorders who could be included within each section of the classification.
- –
To establish the level of agreement between different clinical evaluators in the diagnoses of these same patients, using the criteria described in this classification.
- –
To conduct, if appropriate, a modification in the classification whenever limitations were detected and there was a consensus on how to address them.
A multicentre study was designed, involving 1 coordinator and 6 different evaluators, all of them otolaryngologists specifically involved with Otoneurology and from 6 different centres.
The coordinator selected the clinical records of 50 consecutive patients who attended the otoneurology clinic at Hospital Universitario de Santiago due to vertigo and balance disorders and for whom, in his judgement, it was possible to obtain a diagnosis. The patients were 24 males and 26 females, with a mean age of 53.5 years (with a minimum of 8 and a maximum of 89 years). The following information was excluded from these histories:
- –
Name and identification details of the patients, in order to preserve their privacy.
- –
Diagnosis proposed by the study coordinator.
- –
Treatment indicated (since it could be indicative of the diagnosis).
Consequently, the medical records included:
- –
Demographic data of patients: age, gender, marital status, occupation and toxic habits (alcohol, tobacco and/or caffeine consumption and exposure to noise).
- –
Clinical data: personal and family medical history, current use of medication, reason for consultation and detailed otoneurological history.
- –
Exploration data:
- •
General otolaryngology clinical examination.
- •
Neurological examination (cranial nerves, strength, sensitivity and coordination tests).
- •
- –
Clinical, otoneurological and balance examination:
- •
Exploration of spontaneous nystagmus (with naked eye and with Frenzel goggles).
- •
Halmagyi and head shaking tests.
- •
Unteberger and Romberg tests.
- •
Positional tests (whenever listed): Dix and Hallpike, McClure and/or cephalic hyperextension tests.
- •
Tone threshold audiometry.
- •
Instrumental balance tests (as indicated for each patient): videonystagmography (caloric and/or rotating tests), dynamic posturography, craniocorpography and/or vestibular evoked myogenic potentials.
- •
Other tests, including analytical, audiological (otoacoustic emissions and/or auditory evoked potentials) and/or imaging tests (brain MRI scan and/or petrosal CT scan).
These 50 clinical histories were simultaneously referred to the 6 reviewers. All were asked for:
- –
A diagnosis of each patient, attempting to follow the sections in the consensus classification.
- –
A personal diagnosis for each patient.
- –
Comments on the difficulties encountered to match each patient to a section in the classification.
The diagnoses and comments from each of the evaluators were collected in an Excel spreadsheet. Statistical analysis of the results was performed using SPSS 15.0 for Windows. The kappa index was used to analyse diagnostic agreement.
ResultsFirst, we analysed the percentage of patients whom the assessors found it possible to define a diagnostic category included in the consensus classification. We considered 3 possibilities:
- –
A diagnosis was established and it formed part of the classification.
- –
A diagnosis was established, but it was not contemplated by the classification.
- –
It was not possible to establish a diagnosis with the information available.
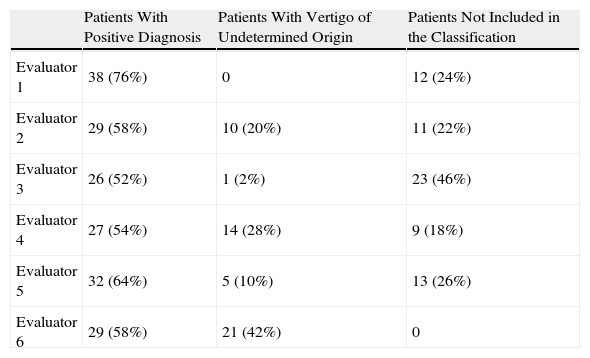
The percentage of patients included by each of the evaluators is shown in Table 1. According to reviewers, the percentage of patients for whom it was not possible to establish a diagnosis described in the consensus classification ranged between 24% and 48% of the total.
Patients Who Could or Could Not Be Included in the Classification.
| Patients With Positive Diagnosis | Patients With Vertigo of Undetermined Origin | Patients Not Included in the Classification | |
| Evaluator 1 | 38 (76%) | 0 | 12 (24%) |
| Evaluator 2 | 29 (58%) | 10 (20%) | 11 (22%) |
| Evaluator 3 | 26 (52%) | 1 (2%) | 23 (46%) |
| Evaluator 4 | 27 (54%) | 14 (28%) | 9 (18%) |
| Evaluator 5 | 32 (64%) | 5 (10%) | 13 (26%) |
| Evaluator 6 | 29 (58%) | 21 (42%) | 0 |
Next, we proceeded to analyse the level of diagnostic agreement between the evaluators. We considered 2 options:
- –
Patients in whom there was unanimity in diagnosis among the 6 evaluators: 7 patients (14% of total). These were 4 patients with benign paroxysmal positional vertigo, 2 with Meniere's disease and 1 with migraine-associated vertigo.
- –
Patients with majority agreement (at least 4 of the evaluators agreed on the diagnosis based on the classification): 31 patients (62%). Of these, the agreement was positive (there was agreement that it was possible to establish a diagnosis included in the classification) in 26 patients (52% of total) and negative (it was agreed that it was not possible to include the patient in any of the sections of the classification) in 5 cases (10% of total). This agreement is shown as a graph in Fig. 1.
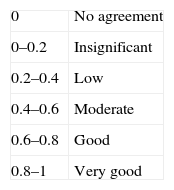
We used the kappa index for the statistical analysis of agreement between evaluators, measuring the agreement between 3 or more observers with 2 categories. In this case the 2 categories were the following:
- –
A diagnosis was established.
- –
A diagnosis was not established (“vertigo of unknown origin” or “cannot be included in the classification”).
The level of agreement indicated by the result of the kappa index is shown in Table 2. Under the above conditions, in our series of patients the kappa index value was 0.4198, with a 95% confidence interval and a value of P<.00001. This indicates a moderate level of agreement.
Finally, we collected the comments of various evaluators on the difficulties encountered to include patients in each section of the classification. These comments were summarised as follows:
- –
Some patients did not report vertigo crises, but rather instability or imbalance, so they could not be included in any of the sections of the classification.
- –
The diagnosis of benign paroxysmal positional vertigo requires positive evidence at the time of diagnosis. Thus, it was not possible to include those patients who reported compatible clinical symptoms which had been resolved at the time of consultation.
- –
Some evaluators reported that there were some diagnostic possibilities missing:
- •
Vestibulotoxicity.
- •
Presbyvertigo/presbyastasia.
- •
Intoxication/drug side effects.
- •
Acute vestibular episode lasting hours (duration not specified in neuritis).
- •
Recurrent peripheral vertigo.
- •
Phobic postural vertigo and anxiety.
- •
The existence of a consensus nomenclature which enabled the categorisation of patients with vertigo based on clinical data and ease of use was a common demand of otolaryngologists involved in Otoneurology. The consensus classification proposed by the Otoneurology Commission of SEORL-PCF was developed in an attempt to respond to this demand.
The current validation was conducted in an attempt to adapt to the clinical reality of patients with vertigo and balance disorders. To this end, a group of patients who consulted consecutively due to vertigo or balance disorders at a specialised Otoneurology unit were collected without applying selection or exclusion criteria. This was simultaneously an advantage (it adjusted to the reality of consultation) and a limitation (not all patients referred to Otoneurology units were adequately pre-screened, so there could be many patients who did not really suffer vertigo or instability).
A second limitation was due to the methodological design of the study. The evaluators only had access to the information which the study coordinator sent them and which he considered sufficient to establish a diagnosis. However, this may not have been the same for the evaluators. Moreover, a diagnosis established from a clinical history written by a third person has limitations with respect to a diagnosis “in person”, due to the additional information that can be obtained in the latter case (possibility of delving deeper during questioning, information provided by body language, etc.).
Once these considerations were taken into account, the level of agreement achieved (measured as the kappa index value) showed the need for improvements in the classification in order to obtain a substantially higher level of agreement. The results of this assessment were discussed, not only between the coordinator and evaluators, but also among a larger group of otoneurologists in September 2010 in Madrid and subsequently via email, so that the classification modification was obtained by consensus. Two modifications were proposed. The first was the inclusion of a new section under the heading “recurrent vertigo crises without hypoacusis, caused by posture”, dividing it into 2 sections:
- –
Definitive BPPV: according to the prior definition of the classification: “brief vertigo (usually lasting seconds), caused by positional triggering tests (Dix and Hallpike test, lateral position test, rotation test or cephalic hyperextension test) which is finite and reproducible”.
- –
Probable BPPV: clinical manifestations suggestive of BPPV, but with negative positional tests at the time of consultation (due to spontaneous resolution of symptoms).
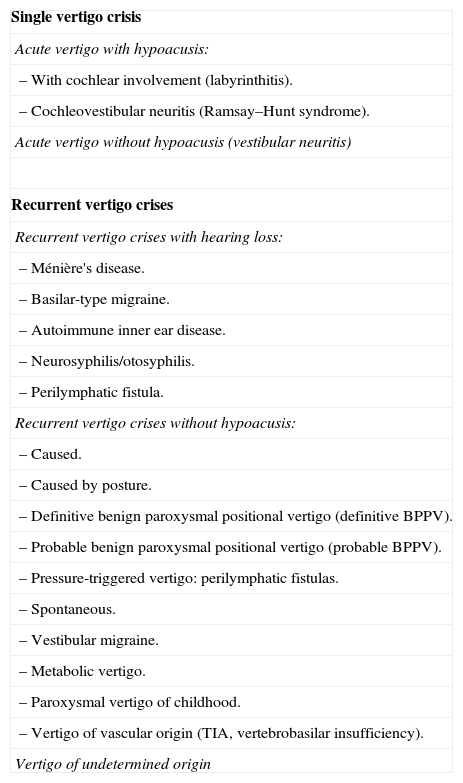
The second change was the review and update of the diagnoses of “vertigo-migraine” and “migraine-associated vertigo”, which were replaced by “basilar-type migraine” and “vestibular migraine”, respectively, based on bibliographic information subsequent to the publication of the first classification. With these modifications, the consensus classification of vertigo by the Otoneurology Commission of SEORL-PCF would be as reflected in Table 3. The definition of each section, including the modifications already described for BPPV, vertigo-migraine and migraine-associated vertigo, are transcribed as an annex from the initial publication.4
Diagnostic Categories for Peripheral Vestibular Disorder (SEORL-PCF 2011, Version 2).
| Single vertigo crisis |
| Acute vertigo with hypoacusis: |
| – With cochlear involvement (labyrinthitis). |
| – Cochleovestibular neuritis (Ramsay–Hunt syndrome). |
| Acute vertigo without hypoacusis (vestibular neuritis) |
| Recurrent vertigo crises |
| Recurrent vertigo crises with hearing loss: |
| – Ménière's disease. |
| – Basilar-type migraine. |
| – Autoimmune inner ear disease. |
| – Neurosyphilis/otosyphilis. |
| – Perilymphatic fistula. |
| Recurrent vertigo crises without hypoacusis: |
| – Caused. |
| – Caused by posture. |
| – Definitive benign paroxysmal positional vertigo (definitive BPPV). |
| – Probable benign paroxysmal positional vertigo (probable BPPV). |
| – Pressure-triggered vertigo: perilymphatic fistulas. |
| – Spontaneous. |
| – Vestibular migraine. |
| – Metabolic vertigo. |
| – Paroxysmal vertigo of childhood. |
| – Vertigo of vascular origin (TIA, vertebrobasilar insufficiency). |
| Vertigo of undetermined origin |
TIA: transient ischemic attack; BPPV: benign paroxysmal positional vertigo.
Patients with persistent or recurrent instability were not included in this classification.
Another result of the reflections and consultations conducted for this assessment was a commitment by the Otoneurology Commission of SEORL-PCF to reassess the classification in a dynamic manner. This will enable its effectiveness to be determined and aid in reaching new agreements over entities for which a definitive consensus could not be reached at the time (presbyvertigo, ototoxicity, etc.).
Conflicts of InterestThe authors have no conflicts of interest to declare.
Acute vertigo with hearing loss. Clinical syndrome characterised by hearing loss with a sudden vertigo crisis, diaphoresis, spontaneous nystagmus and postural imbalance. It may also appear with: (a) cochlear involvement (labyrinthitis) with an otogenous, vascular, tumoural or degenerative cause, and (b) cochleovestibular neuritis: otic herpes zoster (Ramsay–Hunt syndrome).
Acute vertigo without hearing loss: vestibular neuritis. Clinical syndrome characterised by the sudden onset of a prolonged vertigo crisis, with nausea and vomiting, spontaneous nystagmus and postural imbalance, without neurological or hearing symptoms.
Ménière's disease. In order to be included in this group, the patient must have suffered at least 2 episodes typical of vertigo (of at least 20min duration, accompanied by imbalance and often nausea and sweating, requiring rest, and always presenting horizontal or horizontal-rotary nystagmus). Hearing loss must be of perceptive type, verified at least once through audiometric tests (it is common for hearing to fluctuate, but it is not essential for diagnosis). The affected ear must present tinnitus, aural fullness or both. This would correspond to what the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) defined as “definite MD”.1 It would also include other clinical forms such as familial Meniere's vertigo (MV), due to a likely genetic alteration, and bilateral MV (synchronous and asynchronous).
Basilar-type migraine (code 1.2.6. of the ICHD-II).5 Vertigo is present in 60% of patients with basilar-type migraine.6 It is defined as a migraine headache with aura which presents at least 2 of the following, fully reversible, neurological symptoms:
- –
Dysarthria.
- –
Vertigo.
- –
Tinnitus.
- –
Hearing loss.
- –
Diplopia.
- –
Simultaneous visual symptoms in both eyes and both nasal and temporal visual fields.
- –
Ataxia.
- –
Decreased level of consciousness.
- –
Simultaneous bilateral paresthesias.
The presence of motor impairment excludes this diagnosis. The symptoms associated by basilar-type migraine are typically associated with those of the posterior fossa and are usually bilateral. It is necessary for one of the aura symptoms to develop gradually over 5min or for various aura symptoms to occur in succession for over 5min. In addition, each aura symptom must last for at least 5min and up to a maximum 60min.
It was previously classified as basilar migraine. The terminology has been modified because there is little evidence that the basilar artery or its territory are involved. ICHD-II recognises vertigo as an aura of basilar-type migraine.
Autoimmune inner ear disease. Clinical symptoms characterised by vertigo and sudden sensorineural hearing loss, rapidly progressive and/or episodic, with good response to treatment with corticosteroids and immunosuppressors, in the context of a systemic autoimmune disease and/or alterations in any of the following laboratory tests: elevated sedimentation rate, positive rheumatoid factor, positive antinuclear antibodies, positive antineutrophil cytoplasmic antibodies, elevated circulating immune complexes, positive Western blot and T16 cell immunophenotype.
Neurosyphilis-otosyphilis. Includes patients with episodic vertigo with unilateral or bilateral, progressive, perceptive hearing loss. Patients present unilateral or bilateral vestibular hypofunction and analytical studies are positive for syphilis.
Perilymphatic fistula. Characterised by vertigo with progressive sensorineural hearing loss, with stepwise evolution and history of middle-internal ear malformations, (observed by CT and MRI scan), head injury or surgery with manipulation of oval or round window and/or visualisation of the fistula during surgery. Fistula test should be positive (although not in all cases). Most cases present labyrinth hypoexcitability in the thermal test.
Caused
By posture. BPPV, with 2 possibilities:
- –
Definitive BPPV, according to the prior definition of the classification: “known as benign paroxysmal positional vertigo and defined as a brief vertigo (usually lasting seconds), caused by positional triggering tests (Dix and Hallpike test, lateral position test, rotation test or cephalic hyperextension test) which is finite and reproducible”.
- –
Probable BPPV: clinical manifestations suggestive of BPPV, but with negative positional tests at the time of consultation (due to spontaneous resolution of symptoms).
Pressure-induced vertigo: perilymphatic fistula. Vertigo triggered by mechanical pressure generated by the patient (Valsalva manoeuvre), by the explorer (pressure generated in the external ear canal) or by sounds (Tullio phenomenon). Generally, perilymphatic fistulas appear with hearing loss; however, in superior semicircular canal dehiscence there may not be hearing loss.
Spontaneous
Vestibular migraine.7 Defined by 4 criteria:
- –
Episodic vestibular symptoms of moderate intensity.
- –
Current or previous history of migraine according to ICHD-II criteria.
- –
One of the following migraine symptoms must occur during at least 2 vertigo crises: migrainous headache, photophobia, phonophobia, visual symptoms or other auras.
- –
Other causes must be ruled out by appropriate laboratory tests.
Vestibular symptoms include rotatory vertigo or another illusion of bodily or object movement, which can be spontaneous or positional. Vestibular symptoms are “moderate” if they interfere with, but do not prevent daily activities.8 The diagnosis of vestibular migraine does not require consistent association between vertigo and headache. In fact, this systematic association only occurs in 5%–10% of patients who meet the criteria for vestibular migraine. Typically, migraine headaches often precede the vertigo crises by several years.
In any case, although widely used and studied, the term vestibular migraine is not included in ICHD.
Metabolic vertigo. Balance disorder (instability and/or episodes of movement sensation) in patients with known metabolic and unbalanced diseases (diabetes, kidney disease, etc.). The symptoms should be reversed once the metabolic symptoms are balanced.
Paroxysmal vertigo of childhood. Brief and recurrent episodes (less than 15 min) of loss of balance which appear during the first years of life (usually before the age of 6 years). It can be accompanied by vegetative symptoms and tend to disappear spontaneously (usually before the age of 10 years). It is often associated with migraine.
Vertigo of vascular origin (TIA, vertebrobasilar insufficiency). Repeated episodes of vertigo or imbalance in elderly patients and/or those with cardiovascular risk factors, sometimes triggered by sudden movements of the cervical region. Accompanied by transient symptoms of posterior fossa ischemia (blurred vision and/or photopsia, occipital headache, loss of strength and/or paresthesias in upper limbs, etc.) with complete recovery after the crises.
Vertigo of unknown origin. Referring to vertigos which could not be included in any of the above sections.
Member of the Otoneurology Commission of SEORL-PCF.
Please cite this article as: Soto-Varela A, et al. Clasificación de los vértigos periféricos de la Comisión de Otoneurología de la Sociedad Española de Otorrinolaringología: concordancia diagnóstica y actualización (versión 2, año 2011). Acta Otorrinolaringol Esp. 2012;63:125–31.