Orchalgia is a common andrological disorder and usually results from pathognomonic change of testes and regional structures. However, responsible cause is still unknown in more than one-fourth of patients.
MethodsWe report two men who initially suffered an acute, isolated orchalgia and posteriorly complicated with paraparesis. They had previous history of prostate cancer and cervical myelitis. The urological examination was negative in both of them. Finally, prostate cancer metastasis and recurrent myelitis at T2/3 level was identified, respectively. Although their orchalgia progressively subsided, their urological, sexual and neurological dysfunction persisted.
ConclusionsIn the literature, the responsible pathology of spinal orchalgia was exclusively found below T10 level, frequently delaying affirmative diagnosis. Therefore, a thorough evaluation of spinal cord above T10 level should be alerted for idiopathic orchalgia with a pre-existing history or risk of spinal cord disorder and a negative urological examination.
La orquialgia es un trastorno andrológico frecuente y suele darse como resultado de un cambio patognomónico en los testículos y estructuras adyacentes. Sin embargo, su causa sigue siendo desconocida en más de una cuarta parte de los pacientes.
MétodosInformamos de dos varones que sufrieron inicialmente una orquialgia aguda y aislada, que se complicó conduciendo posteriormente a una paraparesia. Los dos tenían antecedentes de cáncer de próstata y mielitis cervical. El examen urológico fue negativo en ambos. Finalmente, se identificó metástasis del cáncer de próstata y mielitis recurrente a nivel de T2 y T3, respectivamente. Aunque la orquialgia cedió progresivamente, las disfunciones urológicas, sexuales y neurológicas persistieron en los dos pacientes.
ConclusionesSegún la literatura existente, la patología responsable de la orquialgia espinal se hallaba exclusivamente por debajo del nivel T10, lo que solía demorar el diagnóstico confirmatorio. Por lo tanto, en el caso de la orquialgia idiopática con una historia preexistente o riesgo de trastorno de la médula espinal y un estudio urológico negativo, se debe recomendar la evaluación exhaustiva de la médula espinal por encima del nivel T10.
Acute non-traumatic orchalgia mostly results from testicular torsion in children and adolescence whereas testicular torsion, ischemia or infection in adult men.1 However, idiopathicity is still reported in 25% of pediatric patients2 whereas 25.2%–51.22% of adult patients2–4 after extensive survey, and that renders a high risk of underdiagnosis, an exposure to unnecessary examinations, and legal disputes. A few abdominal pathologies, such as pancreatitis,5 aortic dissection,6 aortic aneurysm or adrenal pheochromocytoma, provoked referred pain in scrotum mimicking acute orchalgia through the sensory interconnections below the lower thoracic spinal cord. Herein, we firstly report two men who suffered an acute, isolated orchalgia was found to have upper thoracic spinal cord disorders later.
Patients and methodsTwo men who initially suffered an acute, isolated orchalgia, following by an exacerbation of urological, sexual and neurological dysfunction due to upper thoracic cord lesion, were reported. A literature review of spinal orchalgia from PUBMED was also completed. This study has been approved by the Chang Gung Medical Foundation Institutional Review Board (file number: 201701510B0).
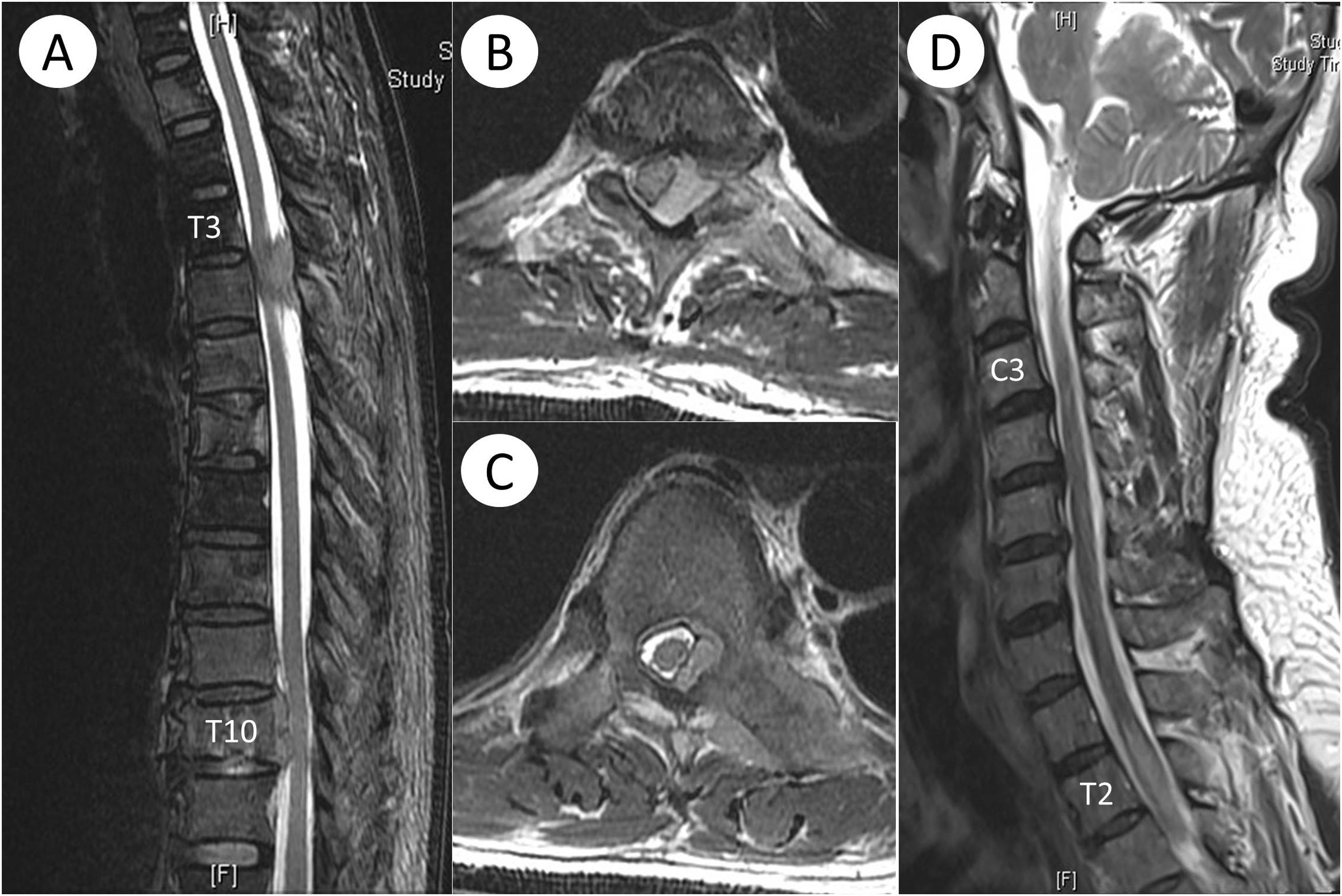
Case 1. A 63-year-old man had had prostate cancer 3 years ago and completed surgical ablation and radiotherapy. Patient remained well until when a sudden onset of pain at testes occurred without antecedent trauma, infection or exercise. Erectile function was preserved. Testes did not enlarge. Pain was not provoked by palpation of testis. Cremasteric and anal reflex were preserved. Prostate cancer metastasis to testes was initially considered. A detailed urological survey, including doppler sonography, urinalysis and prostate specific antigen, did not reveal abnormal finding. Abdominal aneurysm, dissection or urolithiases was not found. While the intensity of orchalgia progressively decreased, numbness below umbilical region, weakness of both legs, urine retention and erectile dysfunction rapidly occurred at one week later. Lumbar spine radiography showed osteolytic foci suspecting for metastases. Incomplete transverse myelopathy below T7 level and anal and cremasteric areflexia were found. Spinal magnetic resonance imaging (MRI) disclosed multiple vertebral metastases and two extradural masses at T3-T4 level and T10-T11 level, respectively (Fig. 1A to 1C). Histopathological study of the masses was compatible with adenocarcinoma of prostate. Although orchalgia subsided within 2 days and numbness gradually improved after emergent surgical measure, dysuria, erectile dysfunction and paraparesis persisted. On a follow-up of 1 year, there was no recurrence of orchalgia.
In Case 1, spinal magnetic resonance imaging showed extradural masses at T3-T4 and T10-T11 and multiple vertebral metastases (A). The thoracic cord was compressed and displaced at T3-T4 (B) and T10-T11 level (C). In Case 2, acute edema was seen at T2-T3 level (D). T2-weighted intensity at C3-C4 level was considered residual change in previous myelitis.
Case 2. A 59-year-old man had had hypertension and prostate hyperplasia for 3 years and received transurethral ablation before. Patient remained well until when a sudden onset of weakness of both legs occurred due to C3/4 myelitis. Residual weakness was complicated after corticosteroid pulse therapy. Two months later, a sudden onset of orchalgia of both testes occurred without antecedent trauma, infection or exercise. Erectile function was preserved. Testes did not enlarge. Pain was not provoked by palpation of testes. Cremasteric and anal reflex were preserved. Prostate cancer metastasis to testes was initially considered. A detailed urological survey, including doppler sonography, urinalysis and prostate specific antigen, did not reveal abnormal finding. Abdominal aneurysm, dissection or urolithiases was not found. Two days later, urine retention, exacerbation of previous weakness and erectile dysfunction rapidly occurred. Incomplete transverse myelopathy below T5 level and anal and cremasteric areflexia were found. Spinal MRI disclosed acute edema of thoracic spinal cord at T2-T4 level (Fig. 1D). Laboratory tests disclosed moderate lymphocytic pleocytosis. Neuromyelitis optica was finally diagnosed. Although orchalgia and numbness subsided whereas dysuria improved after corticosteroid pulse therapy, erectile dysfunction and paraparesis persisted. On a follow-up of 2 years, there was no recurrence of orchalgia.
DiscussionThe responsible lesions were identified at T2/3 level of spinal cord in our two patients. Neurogenic orchalgia has occasionally reported to arise from an involvement of peripheral nerves, lumbar plexuses, or lumbosacral nerve roots that innervate the testes. On the other hand, spinal orchalgia was reported in only four patients after a literature review of PUBMED (Table 1),7–10 including primary tumor at T10 and T11 level, conus medullaris tumor, and T11-L5 spinal stenosis, in that the sensory innervations of testes are affected. Therefore, the results of our patients extend the pathognomonic sensory level from T10/11 upwards to T2/3 for orchalgia. A careful evaluation of spinal cord at upper thoracic cord is suggested for acute or chronic orchalgia, in especially without determined cause.
Summary of spinal orchalgia in PUBMED.
| Author, year | Age (Year) | Etiology and location | Intervala | Associated symptom(s) | Outcome |
|---|---|---|---|---|---|
| Chen & Yin, Present series | 63 | Prostate cancer intradural metastasis at T3−5 | 7 days | Initially only acute orchalgia for 1 week, following by dysuria, erectile dysfunction, paraparesis and numbness below T9 level; no vertebral symptom | Surgical removal relieved scrotal pain. Dysuria and numbness improved but paraparesis and erectile dysfunction persisted |
| Kao et al., Present series | 59 | Postinfectious myelitis at T3 level | 2 days | Initially only acute orchalgia for 2 days, following by dysuria, erectile dysfunction, paraparesis and numbness below T5 level; no vertebral symptom | Pulse therapy abolished scrotal pain and numbness. Dysuria improved. Erectile dysfunction and paraparesis persisted |
| Dawson et al., 2014 | 42 | Ependymoma at T11-L2 | NR | Lumbago, scrotal pain | Pain was relieved by palliative gabapentin, amitriptyline and morphine |
| Doubleday et al., 2003 | 36 | Central disc herniation at T12-L1 | 1 month | Vertebral symptom for 5 years; acute orchalgia, buttock pain, paresthesia and weakness of leg at right side | Physical therapy relieved deficits |
| Kawsar & Goh, 2002 | 38 | Spinal schwannoma at T10-L2 level | 6 weeks | Erectile dysfunction, dysuria, groin pain, orchalgia, gait instability | Surgical removal improved paraparesis partially but no benefit for other deficits |
| Kosar et al., 1999 | 31 | Conus medullaris meningioma | 1 year | Initially only orchalgia of both testes; lumbago and leg pain occurred at 9 months later | Surgical removal abolished pain within 1 month |
DOP: diagnosis of underlying cause under first presentation; NR: Not reported.
A rapid and accurate diagnosis was greatly challenged in our patients by an absence of antecedent or concomitant neurological, sexual or vertebral symptom at initial until when their paraparesis abruptly occurred at 2–7 days later. Interestingly, the time interval between orchalgic onset and final diagnosis ranged from 6 weeks to 1 year in previously reported patients of spinal orchalgia,8–10 suggesting that spinal orchalgia is seriously neglected even ancillary symptom was present. Although a restricted somatosensory deficit is not rare for remote spinal cord disorder,11 we strive to search if the experiences in our patients can fill the gap of difficult diagnosis under similar situations. Reviewing the clinical course, our patients have had have a history of antecedent malignancy or myelitis that risks for metastasis or recurrent myelitis, and also a negative physical and sonographic result on presentation. Accordingly, a negative urological survey, together with a previous history of pathogenicity with a high risk of spinal cord involvement, should consider the possibility of spinal orchalgia.
A poor prognosis of urological and sexual ability is common in our and previous patients.7–10 Indeed, erectile and fertile dysfunction prevalently complicate and poorly improve than motor component in spinal cord disorder in men.12 Accordingly, a rapid and accurate diagnosis is necessary for minimizing urological and sexual dysfunction and preventing legal dispute in spinal orchalgia.
Conflict of interestThe authors declare that they have no conflict of interest.